Foods Endocrinologists Avoid for High Blood Sugar
High blood sugar and diabetes rates have surged globally, with over 38 million Americans and 537 million adults worldwide affected in 2023, according to the CDC and International Diabetes Federation. The pancreas and its hormone insulin are central in regulating blood sugar, but many cases go undetected until complications arise. Identifying problematic foods is crucial, as early intervention helps prevent severe health outcomes and supports better long-term management.
1. Sugary Sodas

Sugar-sweetened beverages, such as regular cola, fruit punch, and lemonade, are among the leading contributors to rapid spikes in blood glucose levels. These drinks contain high amounts of added sugars that are quickly absorbed into the bloodstream, causing an immediate rise in blood sugar and prompting the pancreas to release large amounts of insulin. Over time, this repeated stress can lead to insulin resistance, a key factor in the development of type 2 diabetes. A single 12-ounce can of soda can contain upwards of 39 grams of sugar, far exceeding the daily recommended limit for most adults.
Even diet sodas, which are sweetened with artificial sweeteners like aspartame or sucralose, are not considered a healthy alternative by many endocrinologists. Studies suggest that these artificial sweeteners may disrupt the gut microbiome and influence insulin sensitivity, potentially increasing the risk of metabolic disorders (source). For those looking to manage high blood sugar, water, unsweetened tea, or sparkling water with a splash of lemon are much better choices. Avoiding sugary and diet sodas is a crucial step in maintaining healthy blood glucose and supporting overall metabolic health.
2. White Bread

White bread is made from refined grains that have been stripped of their fiber, vitamins, and minerals during processing. This results in a high glycemic index (GI), meaning white bread is rapidly digested and absorbed, causing quick spikes in blood glucose levels. Such rapid increases can challenge insulin production and contribute to insulin resistance over time. In contrast, whole grain breads contain more fiber, which slows down carbohydrate absorption and helps stabilize blood sugar. According to the Harvard T.H. Chan School of Public Health, choosing whole grains over refined grains is associated with a lower risk of type 2 diabetes.
Reading nutrition labels is essential when shopping for bread, as many varieties marketed as “wheat” or “multigrain” may still contain mostly refined flour and added sugars. Look for “100% whole grain” or “100% whole wheat” as the first ingredient, and check for hidden sugars under names like high fructose corn syrup, dextrose, or maltose. By choosing whole grain options and being mindful of added sugars, individuals can better manage their blood sugar and reduce their risk of diabetes-related complications.
3. Breakfast Cereals

Many popular breakfast cereals, especially those marketed to children, contain alarmingly high amounts of added sugars. Cereals like frosted flakes, chocolate puffs, and honey-coated clusters can deliver 10-20 grams of sugar or more per serving, causing rapid increases in blood glucose and placing extra demand on insulin production. In addition to their sugar content, most of these cereals are made from refined grains, which further exacerbate their impact on blood sugar regulation. Research from the Centers for Disease Control and Prevention (CDC) highlights the need to reduce added sugars as a key strategy for diabetes prevention.
In stark contrast, steel-cut oats are a much healthier breakfast choice. They are minimally processed, high in fiber, and have a low glycemic index, meaning they release glucose slowly into the bloodstream and help sustain energy levels. When choosing cereals, look for options with at least 3-5 grams of fiber per serving and less than 5 grams of sugar. Reading ingredient lists and nutrition labels carefully is crucial to avoid hidden sugars like cane syrup or maltodextrin. Adding fresh fruit, nuts, or seeds to plain oats provides natural sweetness and extra nutrients without spiking blood sugar.
4. Packaged Snack Cakes

Ultra-processed snack cakes, such as cream-filled cupcakes, brownies, and mini-donuts, are notorious for their high sugar and refined carbohydrate content. These treats are designed to be hyper-palatable, often containing a combination of sugar, white flour, and unhealthy fats, which leads to rapid blood sugar spikes and increased insulin demand. The frequent consumption of such foods has been linked to a greater risk of developing type 2 diabetes and other metabolic disorders, as reported by the Harvard T.H. Chan School of Public Health.
Another concern is portion distortion: snack cakes are often sold in multi-packs or large sizes, making it easy to consume far more sugar and calories than intended. This excessive intake can overwhelm the body’s ability to manage blood glucose, especially for those already at risk. For healthier snacking, endocrinologists recommend options such as fresh fruit, plain Greek yogurt, or a small handful of nuts. These alternatives provide fiber, protein, and healthy fats, which help slow sugar absorption and keep blood sugar stable. Making mindful swaps can satisfy sweet cravings while promoting better metabolic health.
5. Flavored Yogurts

Flavored yogurts, especially those labeled as “fruit on the bottom” or “blended,” often contain significant amounts of added sugars that can rapidly elevate blood glucose. Some single-serving containers can have as much as 20 grams of sugar, much of which is added rather than naturally occurring from milk. These hidden sugars are a concern for people managing high blood sugar, as they can undermine efforts to maintain stable glucose levels. According to the Harvard Health Blog, many flavored yogurts rival the sugar content of a dessert rather than a healthy snack.
In contrast, plain Greek yogurt is a much better option. It is higher in protein, lower in sugar, and its thicker texture makes it more filling. Plain Greek yogurt also contains beneficial probiotics that support gut health. For those who prefer a sweeter taste, it’s healthier to add natural flavorings at home. Mixing in fresh berries, a sprinkle of cinnamon, or a few chopped nuts can provide sweetness and texture without causing blood sugar spikes. Reading nutrition labels and opting for unsweetened varieties empowers individuals to enjoy yogurt as a nourishing, blood sugar-friendly snack.
6. Fruit Juices

Even when labeled as “100% fruit juice,” beverages like orange juice, apple juice, and grape juice can cause rapid spikes in blood sugar. This is because juicing removes most of the fruit’s fiber, which is essential for slowing sugar absorption and moderating post-meal glucose levels. Without this fiber, the natural sugars in juice are absorbed quickly, leading to sharp increases in blood glucose and a greater demand for insulin. The Harvard T.H. Chan School of Public Health points out that fruit juice, even with no added sugar, behaves much like soda in the body and is associated with a higher risk of type 2 diabetes.
Whole fruits, on the other hand, supply not only fiber but also important vitamins, minerals, and antioxidants. Eating an orange or apple is far less likely to cause blood sugar spikes than drinking a glass of juice from the same fruit. For those who enjoy juice, endocrinologists suggest diluting it with water or sparkling water to lower the sugar concentration. Alternatively, choosing fiber-rich smoothies made with whole fruits and vegetables is a healthier option, as these retain the beneficial fiber that supports blood sugar control.
7. Sweetened Coffee Drinks

Popular coffeehouse beverages such as flavored lattes, frappuccinos, and caramel macchiatos can contain as much or even more sugar than a can of soda. Many medium-sized (16-ounce) sweetened coffee drinks pack 30-50 grams of sugar, rapidly increasing blood glucose and overwhelming the body’s insulin response. These sugar-laden beverages are often topped with whipped cream and flavored syrups, further amplifying their glycemic impact. According to the Centers for Disease Control and Prevention (CDC), excessive added sugar intake from beverages is a significant contributor to poor metabolic health and increased diabetes risk.
In contrast, black coffee contains virtually no sugar or calories and has been associated with a lower risk of type 2 diabetes when consumed in moderation. For those who prefer their coffee with some flavor, endocrinologists recommend customizing drinks with small amounts of unsweetened plant-based milk, a dash of cinnamon, or a sprinkle of cocoa powder. Opting for sugar-free syrups or simply reducing the amount of added sugar step-by-step can help gradually adjust taste preferences. Reading nutrition information before ordering and requesting less syrup or whipped cream are practical strategies for making coffee drinks more blood sugar-friendly.
8. Energy Drinks

Energy drinks are often marketed as performance boosters, but their high sugar and caffeine content make them a risky choice for people concerned about blood sugar. Brands such as Red Bull, Monster, and Rockstar frequently contain 25-30 grams of sugar per can, rivaling the sugar load found in regular sodas. This large amount of sugar can prompt rapid spikes in blood glucose and put extra strain on the pancreas to produce enough insulin. Additionally, the high caffeine content can sometimes mask feelings of fatigue caused by fluctuating blood sugar, potentially encouraging overconsumption. According to the CDC, energy drinks have been linked to negative health outcomes, including increased risk for metabolic syndrome and type 2 diabetes.
Hidden sugars are also a concern, as some energy drinks use multiple sweeteners, including glucose, sucrose, and high fructose corn syrup, which can be difficult to spot on ingredient lists. For those seeking a healthier energy boost, water and unsweetened teas are far better options. Herbal teas, green tea, or simply staying hydrated with water can support energy levels without disrupting blood sugar. Avoiding energy drinks is especially important for individuals at risk for diabetes or those managing high blood sugar.
9. Pre-Made Smoothies

Store-bought or pre-made smoothies are often promoted as healthy choices, but they can contain surprisingly high levels of added sugars and hidden ingredients that spike blood glucose. Many commercial smoothies use sweetened fruit puree, fruit juice concentrates, flavored syrups, or even ice cream and frozen yogurt as bases—all of which significantly increase sugar content. Some large smoothies from popular chains can contain more than 50 grams of sugar in a single serving, rivaling or exceeding the sugar found in a can of soda. According to the CDC, consuming too much added sugar is a major risk factor for developing type 2 diabetes.
Homemade smoothies, by contrast, allow for better control over ingredients and portion sizes. For blood sugar-friendly options, endocrinologists recommend starting with non-starchy vegetables (such as spinach or kale), unsweetened plant-based milk or water, and a controlled portion of whole fruit. Adding healthy fats like avocado, chia seeds, or a small handful of nuts provides satiety and helps slow sugar absorption. Avoiding fruit juices and sweetened yogurts as smoothie bases is key. By making smoothies at home, you can enjoy a nutrient-dense, personalized beverage without the blood sugar spikes associated with many pre-made options.
10. Canned Fruit in Syrup

Canned fruit is a convenient option, but when packed in heavy or light syrup, it often delivers a hefty dose of added sugars. Syrups are essentially sugar solutions that soak into the fruit, significantly increasing its total sugar content and leading to faster, higher blood glucose spikes when consumed. For example, a single half-cup serving of peaches in heavy syrup can contain nearly double the sugar of the same amount packed in juice or water. According to the Centers for Disease Control and Prevention (CDC), reducing added sugars is crucial for blood sugar management and diabetes prevention.
Choosing fruit canned in its own juice or water is a much better choice, as these options contain only the natural sugars found in fruit, without the additional sugar load from syrup. If syrup-packed fruit is the only option, draining and thoroughly rinsing the fruit under water can help remove some of the excess sugar. However, the best approach is to look for cans labeled “no sugar added” or “packed in water/juice,” and to read ingredient lists carefully. These small adjustments can have a significant impact on blood glucose control, making canned fruit a safer addition to a balanced diet.
11. White Rice
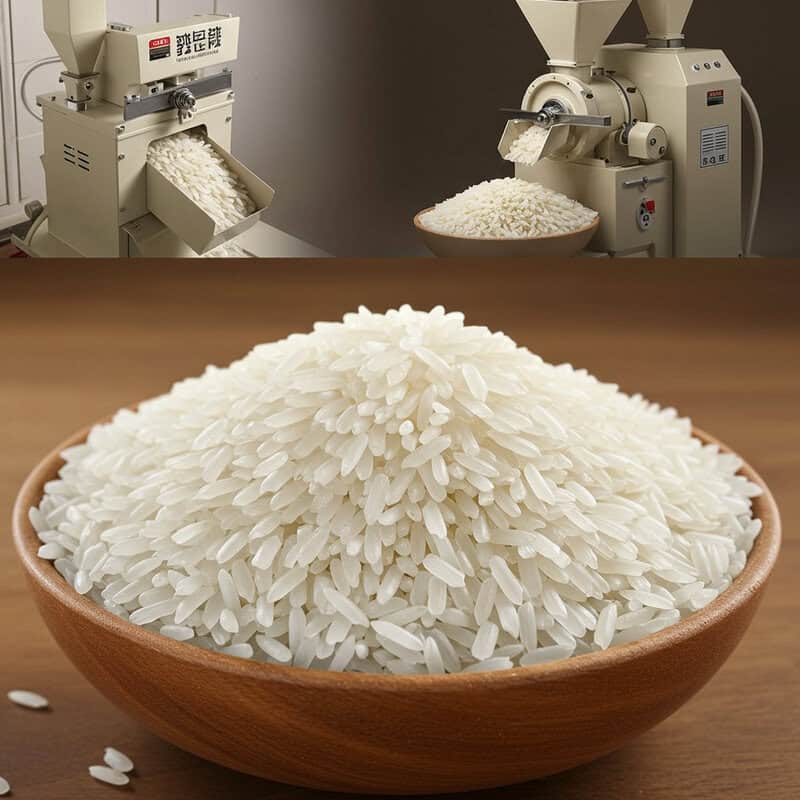
White rice is a staple in many cuisines, but it is highly processed, with the bran and germ layers removed during milling. This lack of fiber and nutrients means white rice is rapidly digested, resulting in a swift rise in blood glucose levels after eating. According to the Harvard T.H. Chan School of Public Health, frequent consumption of white rice is associated with an increased risk of type 2 diabetes, especially in populations that rely heavily on it as a dietary staple.
In contrast, brown rice and wild rice retain their fiber-rich outer layers, which slow digestion and help moderate post-meal glucose spikes. These whole grain alternatives also provide more vitamins, minerals, and antioxidants, supporting better overall metabolic health. For those managing high blood sugar, portion control is key—consider measuring out servings (about 1/2 cup cooked) and balancing rice with plenty of non-starchy vegetables and protein. Swapping white rice for brown, wild, or even cauliflower rice can make a significant difference in stabilizing blood sugar. Gradually transitioning to whole grains and mindful portion sizes supports healthier eating habits and improved glucose control.
12. Instant Noodles

Instant noodles are a popular convenience food, but their nutritional profile poses challenges for blood sugar and heart health. Made primarily from refined wheat flour, instant noodles are quickly digested, leading to rapid elevations in blood glucose. This effect is compounded by their low fiber content, which fails to slow carbohydrate absorption. Additionally, instant noodles are typically very high in sodium—one serving can contain more than half the recommended daily intake—contributing to elevated blood pressure and increased cardiovascular risk. The National Institutes of Health (NIH) highlights the association between instant noodle consumption and higher risk for metabolic syndrome and heart-related complications.
Whole grain noodles, such as those made from buckwheat (soba), brown rice, or quinoa, offer more fiber and nutrients and result in a slower, more gradual increase in blood sugar. For better blood glucose management, endocrinologists recommend eating instant noodles only occasionally and pairing them with vegetables, lean protein, and reduced-sodium seasoning packets. Limiting portion sizes and using half the flavor packet can also help decrease sodium intake. By favoring whole grain options and practicing moderation, individuals can enjoy noodle dishes with less impact on their blood sugar and cardiovascular health.
13. French Fries

French fries, a beloved fast-food item, are made from deep-fried potatoes and have a high glycemic load, meaning they can cause substantial and rapid increases in blood sugar. The process of frying also adds unhealthy fats and extra calories, contributing to weight gain and increasing insulin resistance over time. According to the Harvard T.H. Chan School of Public Health, frequent consumption of fried potatoes, such as french fries, is linked to a higher risk of type 2 diabetes and cardiovascular disease.
Baked or boiled potatoes, while still considered high-glycemic foods, have a lower fat content and fewer calories compared to fried versions. Choosing these cooking methods, and consuming potatoes with the skin for added fiber, can help lessen the blood sugar impact. However, even with healthier preparations, portions matter—large servings can still lead to significant glucose spikes. Endocrinologists recommend limiting portion sizes (about half a medium potato) and pairing potatoes with non-starchy vegetables and lean proteins to slow carbohydrate absorption. By choosing healthier preparation methods and being mindful of quantity, individuals can enjoy potatoes with less risk to blood sugar control.
14. Potato Chips

Potato chips are a highly processed snack made from thinly sliced potatoes that are deep-fried or baked and heavily salted. Their combination of refined carbohydrates, unhealthy fats, and sodium creates a food that is quickly digested, causing blood sugar to rise rapidly. These spikes may be followed by crashes, which can trigger cravings for more high-carb snacks, setting up a cycle that undermines blood sugar management. Research published by the Harvard T.H. Chan School of Public Health links frequent consumption of potato chips with increased risk of weight gain and type 2 diabetes.
Air-popped alternatives, such as homemade popcorn or baked vegetable chips, offer a healthier way to satisfy savory snack cravings. These options are typically higher in fiber and lower in unhealthy fats and calories. Practical snack tips include portioning out servings to avoid mindless eating, pairing snacks with a protein source (such as a small handful of nuts), and choosing snacks with simple, whole-food ingredients. Reading labels for sodium and added fats is also important. By replacing potato chips with more nutritious, fiber-rich snacks, individuals can enjoy crunch and flavor without destabilizing their blood sugar or increasing diabetes risk.
15. Frozen Pizza

Frozen pizza is a convenient meal choice but is often loaded with simple carbohydrates and added sugars, both of which contribute to rapid blood sugar spikes. The crust is typically made from refined white flour, which lacks fiber and is quickly digested, while many brands add sugar to enhance flavor and browning. Additionally, frozen pizzas are usually high in sodium and saturated fats, factors that can worsen metabolic health and increase the risk of insulin resistance. According to the Centers for Disease Control and Prevention (CDC), limiting added sugars and refined grains is important for blood sugar management and overall wellness.
Homemade pizza offers a healthier alternative, as it allows for the use of whole grain or cauliflower crusts, reduced-fat cheese, and plenty of vegetable toppings. By controlling the ingredients, you can significantly reduce the glycemic load and sodium content of the meal. When purchasing frozen pizza, endocrinologists recommend reading nutrition labels carefully—look for whole grain options, check for hidden sugars (such as dextrose or corn syrup), and avoid varieties with excessive sodium or saturated fats. Smart choices and homemade options make it possible to enjoy pizza while supporting blood sugar control.
16. Barbecue Sauce

Barbecue sauce is a flavorful condiment, but it is often packed with sugar and high-fructose corn syrup to deliver its signature sweetness and sticky texture. A typical two-tablespoon serving can contain 8-12 grams of sugar, which can quickly add up and cause unintended blood sugar spikes, especially when used generously on grilled meats or as a dip. The primary sources of sugar in many commercial barbecue sauces are high-fructose corn syrup and molasses, both of which rapidly elevate glucose levels. According to the Centers for Disease Control and Prevention (CDC), reducing added sugars in sauces and condiments is an important step in managing blood sugar and preventing diabetes.
Homemade barbecue sauces offer more control over sugar content, allowing the use of natural sweeteners in moderation or sugar substitutes. There are also reduced-sugar and no added sugar varieties available in stores, which can be a better choice for those watching their glucose levels. As alternatives, consider using spices, vinegar-based hot sauces, mustard, or salsa to add flavor without extra sugar. Reading labels and experimenting with homemade recipes can help you enjoy bold flavors while keeping blood sugar in check.
17. Ketchup

Ketchup is a staple condiment in many households, but it’s often overlooked as a source of added sugars. A single tablespoon of standard ketchup can contain about 4 grams of sugar, primarily from added sweeteners like high-fructose corn syrup or cane sugar. Because ketchup is commonly used in generous portions and paired with foods already high in refined carbohydrates—such as fries or burgers—the sugar content can quickly accumulate and contribute to blood sugar spikes. Research from the Centers for Disease Control and Prevention (CDC) highlights how added sugars in condiments significantly impact total daily intake.
Sugar-free or reduced-sugar ketchup varieties are now widely available and can be a better choice for those managing high blood sugar. These versions use alternative sweeteners or simply reduce the overall sugar content, offering the familiar flavor with less metabolic impact. Regardless of the type chosen, portion control is key—measuring out servings rather than pouring directly from the bottle helps reduce consumption. As an alternative, try using tomato paste with herbs or fresh salsa for a tangy, low-sugar topping. Being mindful of condiments is a simple strategy to support healthy blood sugar levels.
18. Honey

While honey is often perceived as a healthier alternative to refined sugar due to its natural origins and trace nutrients, it still has a significant impact on blood sugar. Like table sugar, honey is primarily composed of glucose and fructose, both of which are rapidly absorbed and can cause spikes in blood glucose levels. Just one tablespoon of honey contains about 17 grams of sugar, similar to the amount found in agave syrup or maple syrup. According to the Centers for Disease Control and Prevention (CDC), all forms of added sugar—regardless of their source—can negatively affect blood sugar regulation when consumed in excess.
Agave and maple syrup are also marketed as natural sweeteners, but their sugar content and effects on glucose are comparable to that of honey. While they may contain some antioxidants or minerals, these benefits do not outweigh the risks for those managing high blood sugar. Endocrinologists recommend using any sweetener, natural or otherwise, with caution and moderation. To reduce sugar intake, consider flavoring foods with spices such as cinnamon or nutmeg, or using fresh fruit as a sweetener. Awareness and moderation are key to enjoying sweetness without compromising blood sugar control.
19. Granola Bars

Granola bars are often marketed as a healthy, on-the-go snack, but many commercial varieties are high in added sugars and low in fiber. Common ingredients include sugar, honey, corn syrup, and chocolate chips, which can cause quick blood glucose spikes and undermine energy levels. Some granola bars contain as much as 15-20 grams of sugar per serving—rivaling the sugar content of many candy bars. The CDC warns that products labeled as “natural” or “healthy” are not always low in sugar or beneficial for blood sugar management.
Homemade granola bars provide more control over ingredients, allowing you to use rolled oats, nuts, seeds, and dried fruit in moderation. By omitting or severely limiting sweeteners, you can create a snack that is higher in fiber and protein, both of which help slow sugar absorption and promote satiety. When buying packaged granola bars, scrutinize nutrition labels—look for bars with at least 3 grams of fiber, less than 5 grams of sugar, and whole food ingredients. Avoid bars that list sugar, corn syrup, or other sweeteners among the first few ingredients. Smart choices and homemade alternatives can help support stable blood sugar levels.
20. Dried Fruit

Dried fruit, such as raisins, dates, apricots, and cranberries, is often considered a healthy snack due to its vitamins and fiber. However, the drying process removes water, greatly concentrating the fruit’s natural sugars. This means that just a small handful of dried fruit can deliver a sugar load equivalent to multiple servings of fresh fruit, quickly raising blood glucose levels. Moreover, many commercial dried fruits are sweetened with additional sugar or syrups, further increasing their glycemic impact. The CDC emphasizes the importance of monitoring both natural and added sugars for optimal blood sugar management.
Fresh fruit, by comparison, contains more water and fiber, which help slow sugar absorption and promote fullness. Choosing whole, fresh fruit over dried versions is a better strategy for those aiming to keep blood sugar stable. If dried fruit is consumed, it is crucial to watch portion sizes—just one or two tablespoons is often plenty—and to select unsweetened varieties. Combining a small amount of dried fruit with nuts or seeds can also help moderate glucose spikes. Careful portion control and label reading are key to enjoying the benefits of fruit without compromising blood sugar control.
21. Sweetened Nut Butters

Nut butters like peanut butter, almond butter, and hazelnut spreads are popular for their creamy texture and healthy fats. However, many conventional varieties are sweetened with added sugars, honey, or syrups to enhance flavor and appeal. This added sugar can quickly increase the glycemic load of a meal or snack, leading to blood sugar spikes that are especially problematic for individuals managing high blood sugar. According to the Centers for Disease Control and Prevention (CDC), even condiments and spreads can significantly contribute to daily sugar intake when not chosen carefully.
Natural nut butters, on the other hand, contain only nuts and sometimes a pinch of salt, offering more protein, fiber, and healthy fats without the sugar. These options help slow digestion and support more stable blood glucose levels. When shopping for nut butters, endocrinologists recommend reading ingredient lists and avoiding products that list sugar, honey, molasses, or syrups among the first ingredients. Look for spreads labeled “no added sugar” or “natural,” and stir before use if separation occurs. Opting for these unsweetened varieties makes it possible to enjoy the nutritional benefits of nut butters without unwanted effects on blood sugar.
22. Flavored Oatmeal Packets

Flavored instant oatmeal packets are a convenient breakfast option, but they often contain significant amounts of added sugar, artificial flavors, and sodium. Popular varieties like “maple and brown sugar” or “apple cinnamon” may have 10-15 grams of sugar per serving, which can cause blood glucose to spike soon after eating. The quick-cooking oats used in these packets are also more processed, resulting in a higher glycemic index and faster digestion compared to less processed oats. The Centers for Disease Control and Prevention (CDC) cautions that even seemingly wholesome foods like instant oatmeal can undermine blood sugar control if they contain excess added sugar.
In contrast, unflavored old-fashioned or steel-cut oats offer more fiber, a lower glycemic index, and no added sugars, making them a better choice for those managing high blood sugar. To naturally enhance flavor, try adding fresh or frozen berries, a dash of cinnamon, vanilla extract, or a small handful of chopped nuts. These additions boost nutritional value without causing large glucose spikes. Preparing oats from scratch and flavoring them naturally empowers individuals to enjoy a warm, satisfying breakfast while keeping blood sugar stable and energy levels steady throughout the morning.
23. Biscuits and Pastries

Biscuits, pastries, and other baked goods are often loaded with refined flour, added sugars, and unhealthy fats, making them particularly problematic for blood sugar control. Items like croissants, danishes, cinnamon rolls, and scones are quickly digested, causing rapid spikes in blood glucose and increased insulin demand. These foods are also typically high in saturated fats, which can further contribute to insulin resistance and cardiovascular risk. According to the Centers for Disease Control and Prevention (CDC), reducing intake of foods high in both sugar and saturated fat is essential for managing diabetes and overall metabolic health.
Whole grain alternatives, such as whole wheat muffins or oat-based breakfast bars with minimal added sugar, offer more fiber and nutrients, helping to slow digestion and moderate glucose response. Still, even healthier baked goods should be enjoyed in moderation, as large portions can quickly add up in carbohydrates and calories. Endocrinologists advise saving pastries and biscuits for special occasions and focusing on nutrient-dense breakfasts and snacks most of the time. Practicing portion control and choosing whole grain options can help satisfy cravings without significantly disrupting blood sugar balance.
24. Ice Cream

Ice cream is a classic dessert, but its high sugar and saturated fat content make it a challenging choice for those managing high blood sugar. A typical half-cup serving can contain 15-20 grams of added sugar, and the creamy texture is achieved with substantial amounts of cream and sometimes butterfat, contributing to high calorie and fat content. These components can rapidly elevate blood glucose while also increasing the risk of weight gain and insulin resistance. The Centers for Disease Control and Prevention (CDC) recommends minimizing intake of high-sugar desserts to reduce diabetes risk and better manage blood sugar.
Frozen yogurt and fruit-based desserts, such as blended frozen bananas or homemade fruit sorbet, can offer lighter alternatives. However, it’s important to read nutrition labels carefully, as many commercial frozen yogurts are also high in added sugars. For any frozen dessert, portion control is key—opt for a small scoop and savor it slowly, or share a serving with someone else. Choosing options with less added sugar, incorporating fruit, and enjoying ice cream only occasionally can help satisfy sweet cravings without causing drastic spikes in blood glucose.
25. Candy Bars

Candy bars are notorious for their high sugar content, refined carbohydrates, and unhealthy fats, making them one of the quickest ways to spike blood glucose. A typical candy bar can contain 20-30 grams of sugar, which is rapidly absorbed, causing a sharp rise in blood sugar and a subsequent insulin surge. In addition to sugar, candy bars often contain ingredients like high-fructose corn syrup, caramel, nougat, and milk chocolate, all of which contribute to their glycemic impact. The Centers for Disease Control and Prevention (CDC) warns that frequent consumption of sugary snacks is associated with higher risk of type 2 diabetes and poor blood sugar control.
As a more blood sugar-friendly treat, small amounts of dark chocolate (70% cacao or higher) contain less sugar and more antioxidants compared to standard candy bars. When choosing a snack, opt for a piece or two of dark chocolate, and pair it with a handful of nuts to slow sugar absorption and promote satiety. Practicing mindful snacking, reading labels, and reserving candy bars for rare occasions can help minimize blood sugar spikes while still allowing for occasional sweet enjoyment.
26. Sweetened Condensed Milk

Sweetened condensed milk is a thick, syrupy dairy product made by removing most of the water from milk and adding large quantities of sugar. Just two tablespoons can contain over 20 grams of sugar, making it a concentrated source of rapidly absorbed carbohydrates that can cause significant spikes in blood glucose. This ingredient is commonly used in desserts, coffee drinks, and baked goods, often going unnoticed as a major contributor to daily sugar intake. According to the Centers for Disease Control and Prevention (CDC), minimizing added sugars from such sources is crucial for effective blood sugar management and diabetes prevention.
Evaporated milk, by contrast, is unsweetened and contains only the natural sugars found in milk, making it a better option for those watching their glucose levels. While still concentrated, evaporated milk can be used in recipes to add creaminess without the intense glycemic impact of sweetened condensed milk. When recipes call for condensed milk, consider reducing the amount or substituting with evaporated milk plus a non-caloric sweetener if needed. Practicing mindful usage and being aware of hidden sugars in recipes and beverages can help keep blood sugar stable and support healthier dietary habits.
27. Sweetened Almond/Cashew Milk

Plant-based milks, such as almond and cashew milk, have become popular alternatives to cow’s milk, but many commercial varieties are sweetened with added sugars. Sweetened almond or cashew milk can contain 7-15 grams of sugar per cup, which can have a notable impact on blood glucose, especially when used in cereals, smoothies, or coffee drinks. The added sugar in these beverages often comes in the form of cane sugar or syrups, which are rapidly absorbed and can contribute to insulin resistance over time. The Centers for Disease Control and Prevention (CDC) highlights the importance of minimizing added sugars in all beverages, including plant-based milks, for optimal blood sugar management.
Unsweetened almond or cashew milk, on the other hand, contains little to no sugar and is a better choice for people looking to control their blood sugar. These varieties offer the same creamy texture without the added glycemic load. To ensure you’re making the healthiest option, always read nutrition labels and ingredient lists—look for products labeled “unsweetened” and check for hidden sugars listed under names like evaporated cane juice or agave. Making this simple swap can significantly reduce daily sugar intake and support stable blood glucose levels.
28. Flavored Rice Cakes

Flavored rice cakes, such as those coated in caramel, chocolate, or apple cinnamon, may seem like a light snack, but they can be surprisingly high in added sugars. These sweet coatings increase the glycemic index and can cause rapid spikes in blood glucose, especially when consumed in multiples. The combination of refined rice and sugary toppings means these snacks are quickly digested and absorbed, providing little satiety and often leading to cravings for more. According to the Centers for Disease Control and Prevention (CDC), reducing added sugars—even in snacks—plays an important role in blood sugar management and diabetes prevention.
Plain rice cakes, while still made from refined rice, do not contain added sugars and can be a better alternative when enjoyed occasionally and paired with protein or healthy fats (such as a thin spread of natural nut butter). When shopping, it’s important to check ingredient lists carefully for hidden sugars, which may appear as cane sugar, brown rice syrup, or honey. Opting for plain, unflavored rice cakes and adding your own nutritious toppings can help limit sugar intake, promote satiety, and better support stable blood glucose levels.
29. Syrupy Pancakes/Waffles

Pancakes and waffles are breakfast favorites, but when made from refined flour and drenched in syrup, they deliver a double blow to blood sugar control. The simple carbohydrates in traditional pancake and waffle mixes are rapidly digested, causing blood glucose to rise quickly. Adding a generous pour of maple syrup or pancake syrup—both of which are concentrated sources of sugar—can easily add 20-30 grams of sugar to a single meal, compounding the glycemic impact. The Centers for Disease Control and Prevention (CDC) emphasizes the need to minimize both refined grains and added sugars to promote healthy blood sugar levels.
Whole grain pancakes or waffles made with oats, whole wheat, or almond flour offer more fiber and nutrients, resulting in a slower, steadier glucose rise. Swapping out traditional syrup for lower-sugar toppings can also make a big difference. Try using fresh berries, a dollop of plain Greek yogurt, or a light sprinkle of cinnamon for flavor without the sugar spike. Practicing portion control and reserving syrupy breakfasts for special occasions, rather than daily meals, helps support more stable blood glucose and better long-term metabolic health.
30. Sweet-and-Sour Sauces

Sweet-and-sour sauces are popular accompaniments for takeout dishes like chicken, shrimp, and stir-fried vegetables, but they are often loaded with sugar and corn syrup. Just two tablespoons of commercial sweet-and-sour sauce can contain 10-15 grams of sugar, which is quickly absorbed and can contribute to significant blood sugar spikes—especially when paired with white rice or fried foods. According to the Centers for Disease Control and Prevention (CDC), reducing added sugars in restaurant and takeout foods is crucial for maintaining healthy blood sugar levels and reducing diabetes risk.
Homemade versions of sweet-and-sour sauce allow for better control of sugar content. By using ingredients like vinegar, a small amount of fresh fruit juice, and natural sweeteners in moderation, you can create a flavorful sauce with far less sugar. Other alternatives include using low-sugar or sugar-free sauces, or simply flavoring dishes with herbs, citrus, and spices. When eating out or ordering takeout, ask for sauces on the side and use them sparingly. Practicing moderation and seeking lower-sugar options can help you enjoy flavorful meals without compromising your blood glucose control.
31. Chocolate Spreads

Chocolate-hazelnut spreads, such as Nutella and similar products, are widely enjoyed for their creamy texture and sweet, chocolaty flavor. However, these spreads are typically high in added sugars—often containing over 20 grams of sugar in just two tablespoons—which can lead to rapid blood glucose spikes. The first ingredient in many chocolate spreads is sugar, followed by palm oil and only a small proportion of nuts. Regular consumption can contribute to excess calorie intake, weight gain, and increased risk of insulin resistance. The Centers for Disease Control and Prevention (CDC) notes that spreads and toppings are common hidden sources of sugar in the diet.
In contrast, natural nut butters made from peanuts, almonds, or cashews offer more protein, fiber, and heart-healthy fats, with little or no added sugar. When selecting a spread, read ingredient labels carefully to identify added sugars, syrups, or oils, and opt for products where nuts are the primary ingredient. For a chocolaty treat without the sugar spike, try mixing unsweetened cocoa powder into natural nut butter and adding a non-nutritive sweetener if desired. These small changes can help satisfy sweet cravings while supporting more stable blood sugar levels.
32. Jams and Jellies

Jams and jellies are traditional spreads made by preserving fruit with sugar, resulting in a product that is often more sugar than fruit by weight. A single tablespoon of standard jam or jelly can contain up to 13 grams of sugar, much of which is added during processing to achieve the desired sweetness and texture. These concentrated sugars are rapidly absorbed, leading to quick rises in blood glucose levels—especially when jams and jellies are used on bread, toast, or pastries made from refined grains. The Centers for Disease Control and Prevention (CDC) highlights that reducing added sugars, even in small amounts, is vital for blood sugar management.
Fresh fruit, by comparison, contains natural sugars along with fiber, water, and nutrients that help slow the absorption of glucose and make it a better choice for those with high blood sugar. For those who enjoy fruit spreads, reduced-sugar or “no sugar added” jams are available and typically use fruit concentrates or non-nutritive sweeteners. These options can provide fruity flavor with less glycemic impact. Spreading a thin layer or pairing with whole grain bread can further help moderate blood sugar response while still allowing for a touch of sweetness.
33. Sports Drinks

Sports drinks, such as Gatorade and Powerade, are formulated to replenish fluids and electrolytes lost during intense physical activity. However, they often contain high amounts of added sugars—typically 20-34 grams per 20-ounce bottle—which can cause significant blood glucose spikes. While these beverages provide sodium, potassium, and other electrolytes, their sugar content makes them unsuitable for routine hydration, particularly for individuals managing high blood sugar. According to the Centers for Disease Control and Prevention (CDC), water is the best choice for hydration in most situations, as it contains no calories or sugars.
Sports drinks may be appropriate for athletes or individuals engaging in prolonged, vigorous exercise (exceeding one hour), where rapid replenishment of electrolytes and carbohydrates is necessary. For the general population and those with high blood sugar, these drinks are not needed and can inadvertently contribute to excessive sugar intake and poor glucose control. Reading labels is important, as some “low-calorie” options still contain added sugars. For everyday hydration, choose water, unsweetened tea, or add a slice of lemon or cucumber for flavor. Reserve sports drinks for specific, high-intensity needs under medical or athletic guidance.
34. Muffins

Bakery and café muffins are often much larger than standard homemade muffins, with some varieties containing upwards of 30-40 grams of sugar and 400-600 calories each. These oversized portions are made with refined flour, significant amounts of oil or butter, and sweetened with sugar, honey, or syrups. As a result, they deliver a hefty glycemic load that can cause rapid blood sugar surges and contribute to excess calorie intake. According to the Centers for Disease Control and Prevention (CDC), reducing portion sizes and added sugars in baked goods is important for blood sugar management and diabetes prevention.
Homemade muffins offer greater control over ingredients and portion size. Using whole grain flours, adding nuts or seeds, and limiting sweeteners can make muffins more blood sugar-friendly. Opting for mini muffins or baking in smaller molds helps keep serving sizes reasonable. When purchasing muffins, split one with a friend or save half for later to avoid overconsumption. Reading nutrition information in stores and choosing options labeled “whole grain” and “low sugar” can further support healthier choices. Moderation, mindful portions, and DIY baking are key to enjoying muffins without risking blood sugar spikes.
35. Sweetened Applesauce

Flavored or sweetened applesauce is commonly marketed as a healthy snack, especially for children, but many commercial varieties contain significant amounts of added sugars. A single-serving cup can have up to 20 grams of sugar, much of which is not naturally present in the fruit but added during processing. These added sugars can cause rapid blood glucose elevations, particularly when applesauce is eaten alone without accompanying fiber or protein. The Centers for Disease Control and Prevention (CDC) emphasizes the importance of reducing added sugars in snacks to support healthy blood sugar management.
Unsweetened applesauce, in contrast, contains only the natural sugars found in apples and no added sweeteners, making it a much better choice for those concerned about glucose control. For added nutrition and flavor, consider stirring in cinnamon or mixing unsweetened applesauce with a small handful of nuts or a spoonful of plain Greek yogurt. Alternatively, enjoying whole apples provides more fiber and a lower glycemic impact. Always check ingredient labels to ensure products are truly unsweetened, and opt for fruit snacks that retain their natural fiber to help slow sugar absorption and promote fullness.
36. Milkshakes

Milkshakes are indulgent beverages made from ice cream, milk, and often flavored syrups or added sugar, resulting in a dessert that is extremely high in both sugar and calories. A typical fast-food milkshake can contain 50-80 grams of sugar and 400-800 calories per serving, making it a major source of rapidly absorbed carbohydrates that can spike blood glucose levels dramatically. Regular consumption of such high-sugar drinks is linked to increased risk of obesity, insulin resistance, and type 2 diabetes. According to the Centers for Disease Control and Prevention (CDC), beverages with added sugar should be limited or avoided for optimal blood sugar management.
Smoothies, when made at home with whole fruits, leafy greens, and unsweetened yogurt or plant-based milk, can be a healthier alternative, providing fiber and nutrients that help slow sugar absorption. However, even smoothies should be consumed in moderation and without added sweeteners. For those craving a milkshake-like treat, try blending frozen bananas with a splash of unsweetened milk and a touch of vanilla extract for a creamy, lower-sugar dessert. Practicing moderation, reading nutrition information, and reserving milkshakes for rare treats can help maintain more stable blood glucose levels.
37. Sweet Liqueurs

Sweet liqueurs, such as Baileys Irish Cream, Kahlua, and Amaretto, are popular alcoholic beverages that contain significant amounts of hidden sugars. These liqueurs are often crafted with added syrups, cream, or chocolate and can contain 10-20 grams of sugar per standard serving (about 1.5 ounces). When consumed in cocktails or combined with mixers, the sugar content can escalate even further, leading to rapid spikes in blood glucose. According to the Centers for Disease Control and Prevention (CDC), alcohol itself can impact blood sugar regulation, and the addition of sugars in sweet liqueurs compounds the risk for people with diabetes or high blood sugar.
Dry wines and clear spirits, such as vodka, gin, or whiskey, contain little to no added sugar and are less likely to cause abrupt changes in blood glucose when consumed in moderation. If choosing to drink, opt for these lower-sugar options and avoid sugary mixers. Always practice moderation—limit intake to one drink per day for women and two for men, as recommended by health authorities. Reading ingredient labels and being mindful of serving sizes can help reduce the risk of blood sugar swings and support more balanced drinking habits.
38. Glazed Meats

Glazed meats, such as honey-glazed ham, teriyaki chicken, or barbecue-glazed ribs, are popular for their sweet, sticky coatings. However, these glazes are often made with sugar, honey, molasses, or syrups, which can deliver 10-20 grams or more of added sugar per serving. When these sugars caramelize in the oven or on the grill, they create appealing flavor and texture—but also contribute to rapid blood sugar elevations when consumed. According to the Centers for Disease Control and Prevention (CDC), hidden sugars in savory dishes, including meat glazes, are a significant contributor to excessive daily sugar intake and can undermine efforts to manage high blood sugar.
As a healthier alternative, dry rubs made with herbs, spices, and a small amount of salt provide bold flavor without adding sugar. Ingredients like smoked paprika, garlic powder, cumin, and black pepper can enhance meats naturally. When preparing or purchasing glazed meats, read ingredient lists carefully or ask about preparation methods to identify added sugars. Opting for dry-rubbed or simply seasoned meats, and using sweet glazes sparingly, helps reduce sugar consumption while still enjoying flavorful, satisfying dishes.
39. Instant Puddings

Boxed instant puddings are a popular dessert choice due to their convenience and creamy texture, but they are typically high in added sugars and artificial additives. A single serving of prepared instant pudding can contain 15-20 grams of sugar, along with ingredients like artificial flavors, colors, and preservatives. These sugars are rapidly absorbed and can cause swift spikes in blood glucose levels, while the additives offer little nutritional value. According to the Centers for Disease Control and Prevention (CDC), reducing intake of processed desserts high in sugar and artificial ingredients is important for blood sugar management and overall health.
Homemade puddings made with natural ingredients, such as chia seeds, unsweetened cocoa powder, and a non-nutritive sweetener, can provide a healthier, lower-sugar alternative. Using unsweetened plant-based milk or low-fat dairy, and incorporating fiber-rich add-ins, helps slow sugar absorption and support more stable glucose levels. Other alternatives include Greek yogurt with berries or a small serving of fruit compote. When craving something sweet and creamy, opt for homemade versions where you can control sweetness and ingredient quality. These swaps allow for occasional indulgence without the glycemic impact of instant pudding mixes.
40. Popcorn with Caramel or Sugar

Flavored popcorn varieties, such as caramel corn, kettle corn, or chocolate-drizzled popcorn, are popular snacks but come with a significant sugar load. The sugar coating used in these products can add 10-15 grams of sugar or more per serving, quickly turning a whole-grain snack into a dessert that can spike blood glucose levels. The sweet glaze is rapidly absorbed by the body, especially when combined with the fast-digesting carbohydrates in popcorn itself. According to the Centers for Disease Control and Prevention (CDC), even snacks that appear healthy can contribute to excessive sugar intake when sweetened or coated.
Air-popped popcorn, without added sugar or butter, is a much healthier choice for those concerned about blood sugar. It is naturally low in calories and contains fiber, which can help with satiety and slow glucose absorption. For an extra flavor boost, try seasoning air-popped popcorn with herbs, spices, or a light sprinkle of nutritional yeast. When choosing packaged popcorn, check ingredient labels for added sugars and opt for unsweetened varieties. Practicing portion control—measuring out a serving rather than eating from the bag—can also help keep snacking in check and support blood sugar stability.
41. Sweet Bread (Challah, Brioche)

Sweet breads such as challah and brioche are enriched with sugar, eggs, and butter, giving them a soft texture and subtly sweet flavor. While delicious, these breads can contain 5-10 grams of sugar per slice, in addition to refined flour and saturated fats. This combination causes these breads to be rapidly digested, resulting in quick spikes in blood glucose. When used in recipes like French toast or bread pudding, additional sugar is often added, compounding the glycemic load. The Centers for Disease Control and Prevention (CDC) advises that even seemingly modest sources of added sugar can impact blood sugar management, especially when eaten regularly.
Whole grain breads provide more fiber, vitamins, and minerals, and their slower digestion leads to a steadier rise in blood glucose. When choosing bread, opt for options labeled “100% whole grain” or “whole wheat” and check for minimal added sugars in the ingredients. Enjoying sweet breads like challah or brioche in moderation—such as on special occasions or as a small treat—can help keep overall sugar and refined carbohydrate intake within healthy limits while still allowing for culinary enjoyment.
42. Sweet and Salty Snack Mixes

Sweet and salty snack mixes, such as trail mixes containing chocolate candies, yogurt-covered raisins, candied nuts, or sweetened dried fruit, can be deceptively high in added sugars. While marketed as energy-boosting or healthy, many commercial varieties contain 10-20 grams of sugar per small handful, quickly raising blood glucose and adding unnecessary calories. These mixes often pair refined carbohydrates with salty, roasted nuts, making them highly palatable and easy to overeat. The Centers for Disease Control and Prevention (CDC) notes that even “healthy” snacks can contribute to excessive sugar intake if not chosen carefully.
Unsweetened nut and seed mixes, free from added sugars or candy pieces, provide a more blood sugar-friendly alternative. These mixes deliver healthy fats, protein, and fiber, which help promote satiety and slow glucose absorption. When purchasing snack mixes, read ingredient lists closely and avoid those with added sweeteners, syrups, or chocolate. For a DIY approach, combine raw or roasted nuts and seeds with a small amount of unsweetened dried fruit for a balanced, satisfying snack. Practicing portion control and focusing on whole-food ingredients can help manage cravings and support healthier blood sugar levels.
43. Sweet Pickles

Sweet pickles, such as bread-and-butter pickles, are cucumbers preserved in a brine made with sugar and vinegar. A single serving can contain up to 8 grams of added sugar, which contributes to their distinctive sweet flavor but also makes them a hidden source of sugar in the diet. Consuming sweet pickles regularly or in large quantities can quickly add up, leading to unintended blood sugar spikes—especially when paired with other carbohydrate-rich foods. According to the Centers for Disease Control and Prevention (CDC), being mindful of added sugars in condiments and preserved foods is essential for effective blood sugar management.
Dill pickles, on the other hand, are made without added sugar, relying on vinegar, salt, and spices for flavor. These are a better choice for those aiming to reduce sugar intake. If you enjoy sweet pickles, look for brands that offer “no sugar added” or “reduced sugar” varieties, or try making your own at home with alternative sweeteners. Always check ingredient labels for sugar content and serving size to make informed choices. Opting for lower-sugar pickles can help keep snacks and meals flavorful while supporting more stable blood glucose levels.
44. Tonic Water

Tonic water is a common mixer for cocktails and a refreshing beverage on its own, but it is often overlooked as a source of added sugar. A standard 12-ounce serving of tonic water contains about 30 grams of sugar—comparable to many regular sodas. This high sugar content can cause rapid increases in blood glucose, making tonic water a less-than-ideal choice for individuals concerned about blood sugar control. According to the Centers for Disease Control and Prevention (CDC), even beverages that are not perceived as sweet can contribute significantly to daily sugar intake.
In contrast, club soda and sparkling water are sugar-free and provide the same fizzy sensation without impacting blood sugar. For those who enjoy cocktails or need a mixer, opting for club soda, seltzer, or sparkling water with a squeeze of lime or lemon is a healthier alternative. When shopping, always read the nutrition label to distinguish between regular and “diet” or “zero sugar” tonic waters, as these may use non-nutritive sweeteners instead. Small changes in mixer choices can help reduce sugar intake and support more stable blood glucose levels, whether you’re enjoying a drink at home or out with friends.
45. Sweetened Iced Tea

Bottled sweetened iced teas are widely available and often marketed as a refreshing, healthier alternative to soda. However, these beverages can contain as much as 30-40 grams of added sugar per 16-ounce bottle, which is about the same as or even more than many sodas. This high sugar content is rapidly absorbed and can cause substantial spikes in blood glucose, making sweetened iced tea a risky choice for those seeking to manage their blood sugar. The Centers for Disease Control and Prevention (CDC) recommends reducing consumption of all sugar-sweetened beverages, including iced tea, to support better metabolic health.
Unsweetened iced tea—whether black, green, or herbal—contains no added sugar and is a far better option for hydration and refreshment. Homemade iced teas offer even greater control, allowing you to add natural flavors such as fresh mint, lemon, or a few berries for a subtle sweetness without the glycemic impact. If you prefer a bit of sweetness, consider using a non-nutritive sweetener or infusing tea with naturally sweet spices like cinnamon. Making or choosing unsweetened teas can help significantly reduce daily sugar intake and support more stable blood glucose levels.
46. Sweetened Canned Baked Beans

Sweetened canned baked beans are a convenient side dish, but many commercial varieties contain significant amounts of added sugars such as brown sugar, molasses, or high-fructose corn syrup. A typical half-cup serving can contain 10-15 grams of sugar, which quickly adds up, especially when baked beans are served in large portions. This added sugar can elevate blood glucose, offsetting the benefits of the beans’ natural fiber and protein. According to the Centers for Disease Control and Prevention (CDC), monitoring sources of hidden sugars, including in savory foods like canned beans, is essential for blood sugar management.
Homemade baked beans offer greater control over the amount and type of sweetener used—or allow you to omit it entirely. Alternatively, plain canned beans such as kidney, navy, or black beans contain only the natural sugars found in the beans themselves and are a better choice for those watching their blood sugar. When shopping for canned beans, read ingredient lists carefully and choose products labeled “no added sugar” or “low sugar.” Rinsing canned beans can also help reduce sodium content. Opting for unsweetened varieties supports better blood glucose control while still providing the nutritional benefits of beans.
47. Sweetened Popcorn Toppings

Popcorn is often thought of as a healthy whole-grain snack, but sweetened varieties like kettle corn and popcorn with caramel, chocolate, or other sugary toppings can dramatically increase sugar intake. Kettle corn, for example, combines sugar with oil and salt, resulting in a snack that can contain 8-12 grams of sugar per serving. Flavored popcorn toppings, such as cinnamon sugar, caramel drizzle, or chocolate coatings, also add rapidly absorbed sugars that can spike blood glucose levels. The Centers for Disease Control and Prevention (CDC) advises that even snacks marketed as “light” or “all-natural” can be significant sources of hidden sugars.
Savory popcorn options—seasoned with herbs, spices, nutritional yeast, or a light sprinkle of parmesan—are far better choices for individuals managing blood sugar. Air-popped popcorn without added sugar or butter is low in calories and provides fiber for better satiety and slower glucose absorption. For healthier snacking, portion out servings rather than eating straight from the bag, and check ingredient labels for hidden sugars in flavored varieties. Making popcorn at home allows full control over toppings, ensuring your snack remains blood sugar-friendly and satisfying.
48. Sweetened Protein Shakes

Commercial protein shakes are often marketed as healthy meal replacements or workout recovery drinks, but many contain significant amounts of added sugars to improve taste and texture. It’s not uncommon to find 15-25 grams of sugar per serving, especially in chocolate, vanilla, or “fruit” flavored varieties. These sugars, frequently listed as cane sugar, maltodextrin, or corn syrup, can lead to rapid blood glucose surges and undermine the benefits of consuming a protein-rich beverage. The Centers for Disease Control and Prevention (CDC) warns that added sugars in drinks, even those considered “health foods,” can contribute to poor blood sugar control and increased risk of metabolic disease.
Homemade protein shakes offer better control over ingredients and sugar content. Using unsweetened protein powders, plain Greek yogurt, a handful of spinach, and a small portion of whole fruit allows you to create a nutrient-dense beverage without excess sugar. When purchasing ready-to-drink shakes, scrutinize nutrition labels for sugar content and opt for varieties labeled “unsweetened” or “no added sugar.” Making your own shakes or carefully selecting commercial options supports stable blood glucose while still providing convenient, high-protein nutrition.
49. Sweetened Coconut Water

Coconut water is often marketed as a natural, hydrating beverage due to its electrolyte content, but flavored or sweetened varieties can contain substantial added sugars. Many commercial coconut waters include fruit flavors or added cane sugar, with some bottles containing 15-25 grams of sugar per serving—comparable to many sports drinks or sodas. This added sugar can lead to rapid blood glucose spikes, making sweetened coconut water a risky choice for those managing high blood sugar. According to the Centers for Disease Control and Prevention (CDC), hidden sugars in beverages are a leading contributor to excessive daily sugar intake.
Plain, unsweetened coconut water contains only the natural sugars found in the coconut and is lower in total sugar than flavored varieties. For most people, water remains the best option for daily hydration, as it contains no calories or sugars. If choosing coconut water for its minerals and electrolytes, select the unsweetened kind and consume it in moderation. Always read nutrition labels to check for added sugars or syrups, and avoid products marketed as “flavored” or “with a splash of fruit.” Prioritizing plain water or unsweetened beverages can help support stable blood glucose and overall health.
50. Sweetened Fruit-Flavored Gelatin

Fruit-flavored gelatin desserts, such as those found in single-serve cups or boxed mixes, are typically made with added sugars and artificial sweeteners to enhance taste and texture. A single serving can contain 15-20 grams of sugar, which is quickly absorbed and can cause spikes in blood glucose. Additionally, many commercial gelatins rely on artificial colors and flavors, offering little to no nutritional value. The Centers for Disease Control and Prevention (CDC) cautions that even small, seemingly innocent desserts can contribute to excessive sugar intake and make blood sugar management more challenging.
Homemade gelatin made with 100% fruit juice (diluted to reduce sugar content) and plain, unflavored gelatin can be a healthier option. To further lower sugar, use unsweetened juice and add fresh fruit chunks for natural sweetness and extra fiber. Alternatively, simple fruit-based desserts like fresh berries with a dollop of plain Greek yogurt provide satisfying sweetness, beneficial nutrients, and a lower glycemic impact. For anyone trying to manage high blood sugar, reading labels, choosing unsweetened or homemade options, and focusing on whole fruit for desserts are practical strategies to enjoy a sweet treat without destabilizing glucose levels.
Conclusion

Understanding and identifying foods high in added sugars and refined carbohydrates is essential for preventing and managing high blood sugar and related complications. Regularly reading labels, making mindful food choices, and favoring whole, minimally processed options can support stable glucose levels and long-term health. Routine screening for elevated blood sugar is also vital, as early detection allows for timely intervention and better outcomes (CDC). For personalized guidance, consult an endocrinologist or registered dietitian who can tailor dietary and lifestyle recommendations to your unique needs. Prioritizing awareness and professional advice empowers you to make informed decisions and maintain optimal metabolic health.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





