Benefits of Menopausal Hormone Therapy
Menopause affects approximately 75% of women by age 51, with an estimated 40-60% experiencing moderate to severe symptoms. Despite this prevalence, only about 6% of women use menopausal hormone therapy (MHT). The endocrine and reproductive systems are primarily involved, leading to symptoms that are often underrecognized or misattributed. This underrecognition poses significant challenges for effective management and quality of life. For more on symptom prevalence, visit the NIH resource.
1. Symptom Relief for Hot Flashes

One of the most significant benefits of menopausal hormone therapy (MHT) is its effectiveness in relieving vasomotor symptoms, particularly hot flashes and night sweats. These symptoms occur in up to 75% of menopausal women and are primarily caused by declining and fluctuating estrogen levels. MHT works by stabilizing these hormone levels, directly targeting the root cause of hot flashes, and often providing rapid relief within weeks of starting treatment.
Compared to non-hormonal interventions, such as lifestyle modifications, cognitive behavioral therapy, or medications like selective serotonin reuptake inhibitors (SSRIs), hormone therapy remains the most effective therapy for moderate to severe hot flashes. While non-hormonal options can be beneficial for some women, studies consistently show that MHT offers greater and more consistent symptom improvement (BMJ, 2020).
If hot flashes become frequent, severe, disrupt daily activities, or negatively impact sleep, it is advisable to seek medical evaluation. Persistent symptoms may indicate the need for targeted therapy, and a healthcare provider can help determine whether MHT or an alternative approach is most appropriate for your situation.
2. Reduction of Night Sweats

Night sweats are a common and distressing symptom for many women during menopause, often resulting from hormonal changes that disrupt the body’s normal temperature regulation. Menopausal hormone therapy (MHT) helps by restoring estrogen levels, which play a crucial role in the hypothalamus—the part of the brain responsible for regulating body temperature. This stabilization minimizes the erratic signals that trigger sudden sweating episodes at night, leading to a more comfortable sleep environment (NCBI).
The impact of hormone therapy on sleep quality can be profound. Before starting therapy, women often report frequent awakenings, soaked bedclothes, and persistent fatigue due to disrupted sleep. After initiating MHT, studies show significant reductions in the frequency and severity of night sweats, contributing to longer periods of uninterrupted sleep and improved overall well-being (NIH Study).
To track improvements, consider monitoring sleep disturbances by keeping a nightly journal: note the number of awakenings, episodes of sweating, and overall sleep quality. Sharing this information with your healthcare provider can help tailor your treatment and maximize symptom relief.
3. Improved Sleep Quality

Stabilized hormone levels provided by menopausal hormone therapy (MHT) can have a substantial impact on reducing insomnia and restless sleep in menopausal women. Estrogen and progesterone play important roles in sleep regulation by influencing the brain’s sleep centers and circadian rhythms. When these hormones decline, sleep fragmentation and difficulty falling or staying asleep become common. MHT helps to restore hormonal balance, leading to fewer nighttime awakenings and more restorative sleep (Sleep Foundation).
Research consistently shows a positive effect of hormone therapy on sleep duration and quality. A randomized controlled trial found that women using MHT reported significantly longer sleep durations and fewer episodes of wakefulness compared to non-users. Additionally, improvements were noted in both subjective sleep quality and objective sleep measures, such as time spent in deep sleep stages.
If sleep difficulties persist for more than a few weeks, or if daytime fatigue and impaired functioning continue despite lifestyle adjustments, it is important to consult a healthcare provider. Persistent sleep issues may require further evaluation and targeted treatment options.
4. Prevention of Osteoporosis
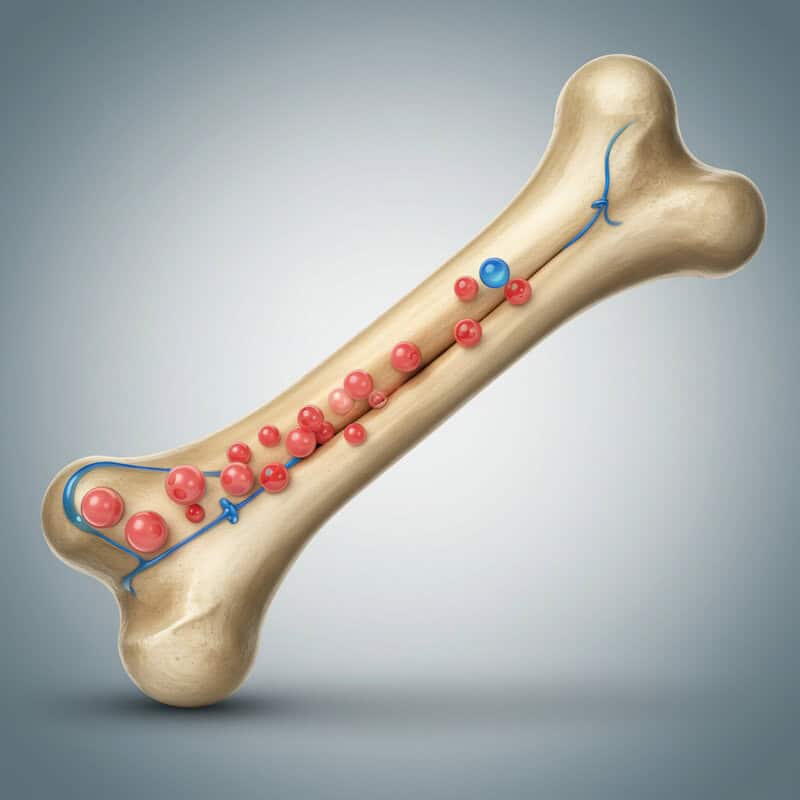
Estrogen is a key hormone in the maintenance of bone density throughout a woman’s life. During menopause, the natural decline in estrogen production accelerates bone loss, leading to an increased risk of osteoporosis and related fractures. Menopausal hormone therapy (MHT) helps slow bone resorption and supports the formation of new bone, thereby maintaining stronger and healthier bones (NIH Osteoporosis & Menopause).
Numerous studies have shown that women who use hormone therapy during and after menopause have a lower risk of both osteoporotic fractures and hip fractures compared to those who do not use MHT. A meta-analysis published by The Lancet concluded that MHT reduced fracture risk by up to 34% in postmenopausal women, making it one of the most effective interventions for osteoporosis prevention in this population.
Bone density screening, typically performed using a DEXA scan, is generally recommended for women over age 65 or for younger postmenopausal women with additional risk factors such as a history of fractures, family history of osteoporosis, or early menopause.
5. Support for Vaginal Health

Menopausal hormone therapy (MHT) plays a crucial role in alleviating vaginal dryness and atrophy, which are common symptoms resulting from declining estrogen levels during menopause. Lower estrogen leads to thinning of the vaginal walls, decreased elasticity, and reduced natural lubrication, often causing discomfort, itching, and pain during intercourse. By replenishing estrogen, hormone therapy helps restore vaginal tissue thickness, moisture, and pH balance, thereby improving overall vaginal health (Mayo Clinic).
There are two main approaches to treating these symptoms: systemic and topical hormone therapy. Systemic therapy (pills, patches) improves both vaginal and whole-body symptoms, while topical therapy (creams, tablets, rings) delivers low-dose estrogen directly to the vaginal tissues. For women experiencing only vaginal symptoms, topical estrogen is often preferred due to its effectiveness and lower risk of systemic side effects (ACOG).
Women should seek gynecological consultation if vaginal discomfort persists, if there is bleeding after intercourse, or if over-the-counter lubricants do not provide relief. Prompt evaluation ensures appropriate diagnosis and treatment tailored to individual needs.
6. Enhanced Sexual Function

Menopausal hormone therapy (MHT) can significantly improve libido and sexual comfort for many women during and after menopause. The drop in estrogen levels often leads to vaginal dryness, decreased blood flow, and thinning of vaginal tissues, all of which can make sexual activity uncomfortable or even painful. By restoring estrogen, MHT enhances vaginal lubrication, elasticity, and sensitivity, contributing to a more pleasurable and satisfying sexual experience (NIH Study).
Clinical studies have shown that women using hormone therapy report increased sexual desire and reduced pain during intercourse compared to those who do not use MHT. For example, research published in the journal Menopause found that both systemic and local estrogen therapy led to significant improvements in sexual function scores, including arousal, lubrication, and satisfaction.
Open communication is essential for addressing sexual health concerns. Women are encouraged to discuss changes in libido or sexual comfort with their partners and healthcare providers. Such conversations help identify the most appropriate therapies and foster emotional intimacy and support during the menopausal transition.
7. Mood Stabilization

Menopausal hormone therapy (MHT) can play a valuable role in stabilizing mood during the menopausal transition. Estrogen influences the production and activity of key neurotransmitters in the brain, such as serotonin, dopamine, and norepinephrine, which are directly involved in regulating mood, emotional responses, and stress levels. When estrogen levels decline, women may experience increased irritability, mood swings, anxiety, or depressive symptoms. MHT helps to restore hormonal balance, thereby supporting healthier neurotransmitter activity and more stable moods (NIH Review).
Studies have shown that women using hormone therapy often report fewer mood disturbances and improved emotional well-being compared to non-users. For instance, research published in JAMA Psychiatry demonstrated reduced depressive symptoms and improved overall quality of life among perimenopausal and early postmenopausal women receiving estrogen therapy.
It’s important to monitor for persistent anxiety or depression despite hormone therapy, as these conditions may require additional support or treatment. If mood symptoms are severe, long-lasting, or interfere with daily functioning, seeking evaluation from a healthcare provider or mental health specialist is strongly recommended.
8. Lower Risk of Colorectal Cancer
Emerging research suggests that menopausal hormone therapy (MHT), particularly estrogen therapy, may be associated with a reduced risk of colorectal cancer in postmenopausal women. Large-scale studies, such as the Women’s Health Initiative, have found that women who used combined estrogen and progestin therapy had a statistically significant lower incidence of colorectal cancer compared to non-users (National Cancer Institute).
Population data indicate that postmenopausal women on hormone therapy experienced up to a 40% reduction in colorectal cancer risk compared to those who never used MHT (JAMA). The mechanisms are not fully understood but may relate to estrogen’s influence on cell growth and apoptosis within the colon. While this benefit is promising, hormone therapy is not prescribed solely for cancer prevention, as its use must be carefully weighed against other health risks.
Regardless of hormone therapy use, timely colorectal cancer screening remains essential for all women over 45 or earlier if risk factors exist. Regular screenings help catch colorectal cancer early, when it is most treatable.
9. Bladder Health Improvement
Menopausal hormone therapy (MHT) can provide notable benefits for bladder and urinary tract health in postmenopausal women. Estrogen is vital for maintaining the strength, elasticity, and moisture of the urethral and bladder tissues. When estrogen levels drop during menopause, the tissues of the lower urinary tract may become thinner and less resilient, increasing the risk of urinary symptoms like urgency, frequency, and incontinence. Hormone therapy, especially topical estrogen, helps restore tissue integrity and improves blood flow, thereby reducing discomfort and urinary problems (Urology Care Foundation).
Studies have shown that women using estrogen therapy, particularly in topical form, experience lower rates of urinary incontinence and fewer episodes of urinary tract infections compared to those who do not use MHT (NIH Study). While systemic hormone therapy may have a less pronounced effect, topical estrogen is often recommended for women whose primary menopausal symptoms are urogenital.
It is important to monitor for early signs of bladder changes, such as increased urgency, pain, or new incontinence. Women experiencing persistent urinary symptoms should discuss them with their healthcare provider to determine if hormone therapy or other treatments may be appropriate.
10. Reduced Risk of Type 2 Diabetes
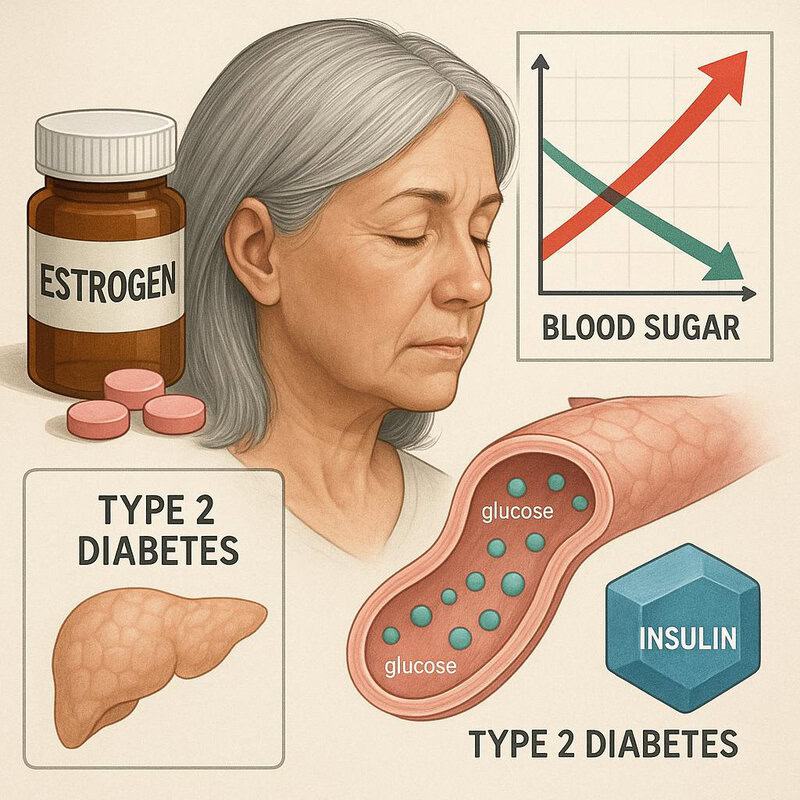
Estrogen has important metabolic effects that influence glucose regulation and insulin sensitivity. During menopause, declining estrogen levels can contribute to increased insulin resistance, higher blood sugar levels, and a greater risk of developing type 2 diabetes. Menopausal hormone therapy (MHT) helps counteract these metabolic changes by improving insulin sensitivity and supporting healthy glucose metabolism (NCBI Study).
Population-based studies have shown that women using hormone therapy have a lower incidence of type 2 diabetes compared to non-users. For example, the BMJ published a comprehensive review indicating that MHT reduced the risk of developing diabetes by up to 30% in postmenopausal women. These benefits appear most pronounced with combined estrogen-progestin therapy and when initiated near the onset of menopause.
Despite these findings, hormone therapy is not recommended solely for diabetes prevention. Women using MHT should have regular monitoring of blood sugar levels and metabolic health, especially if they have other risk factors for diabetes. Early detection and management are key to maintaining long-term health.
11. Lowered Risk of Osteoporotic Fractures

Menopausal hormone therapy (MHT) is well-established for its role in reducing the risk of osteoporotic fractures by enhancing bone strength and density. Estrogen helps regulate the balance between bone formation and resorption, and its reduction after menopause accelerates bone loss, making bones more fragile and prone to fractures. By replenishing estrogen, MHT slows bone breakdown, resulting in improved bone structure and a significant reduction in fracture rates (NIH Study).
International studies highlight the impact of hormone therapy on fracture prevention. According to research published in the Lancet Diabetes & Endocrinology, postmenopausal women using MHT were found to have a 20-34% lower risk of hip and vertebral fractures compared to non-users, a trend consistent across both the United States and Europe. This reduction translates into fewer hospitalizations, improved mobility, and better quality of life for aging women.
Preventive screening, such as bone mineral density (BMD) tests and regular assessments of fracture risk, are recommended for women at menopause and beyond. Early screening enables timely intervention with therapies like MHT to help maintain strong, healthy bones.
12. Support for Cognitive Function
Emerging research suggests that estrogen may play a neuroprotective role in the brain, supporting memory, attention, and other cognitive functions. During menopause, declining estrogen levels have been linked to increased episodes of forgetfulness, trouble concentrating, and mental fog. Menopausal hormone therapy (MHT) may help counteract these changes by promoting blood flow in the brain, supporting synaptic health, and reducing inflammation (NIH Review).
Several studies have compared cognitive outcomes in women using MHT to those who do not. For example, a review published in Frontiers in Aging Neuroscience found that women who initiated hormone therapy around the onset of menopause demonstrated better verbal memory and executive function than non-users. However, the benefits appear most significant when therapy is started early in the menopausal transition, rather than many years later.
Women experiencing persistent memory lapses or difficulty concentrating should consider early cognitive assessments. These evaluations, performed by healthcare providers, can help identify changes that may be addressed with lifestyle modification, hormone therapy, or other targeted interventions.
13. Reduction in Joint Pain

Estrogen has an important anti-inflammatory effect that extends to joint tissues, helping to maintain joint lubrication and reduce swelling and stiffness. During menopause, the natural decline in estrogen can lead to increased inflammation, which may contribute to joint pain and discomfort. Menopausal hormone therapy (MHT) has been shown to alleviate these symptoms by decreasing inflammatory mediators and improving the health of synovial membranes within the joints (NIH Review).
Clinical studies support these benefits; women who use hormone therapy during menopause often report lower pain scores and fewer physical limitations compared to those who do not use MHT. For example, research in the Journal of Women’s Health found that MHT users experienced significant reductions in joint pain and stiffness, leading to improved overall mobility and quality of life.
Despite these potential improvements, persistent or severe joint pain should not be ignored. If joint discomfort is accompanied by swelling, redness, or loss of function, a rheumatological evaluation may be warranted to rule out underlying conditions such as arthritis or autoimmune disorders and to guide further treatment.
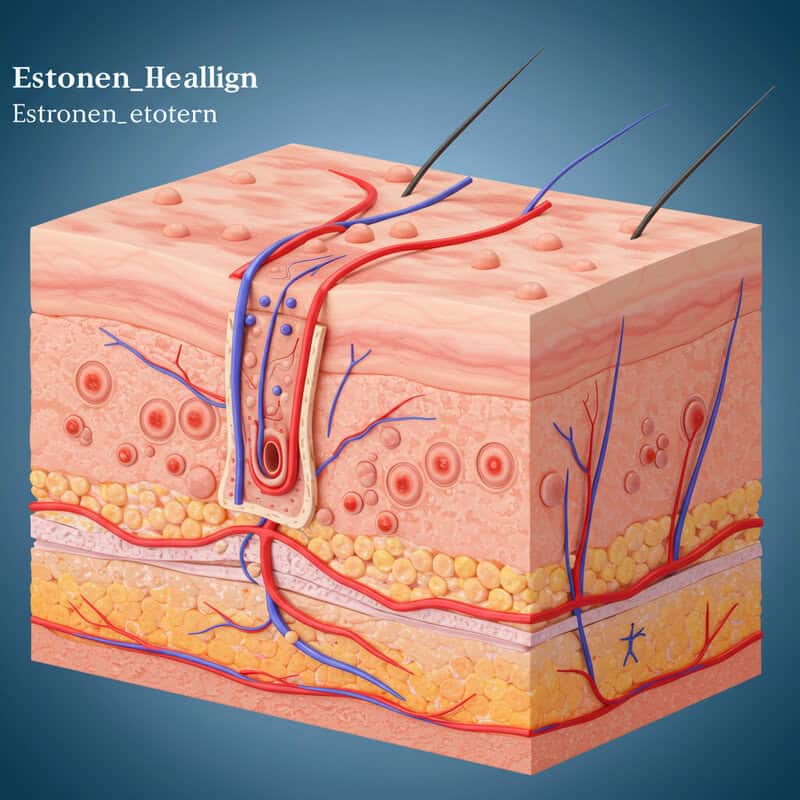
14. Maintenance of Skin Elasticity
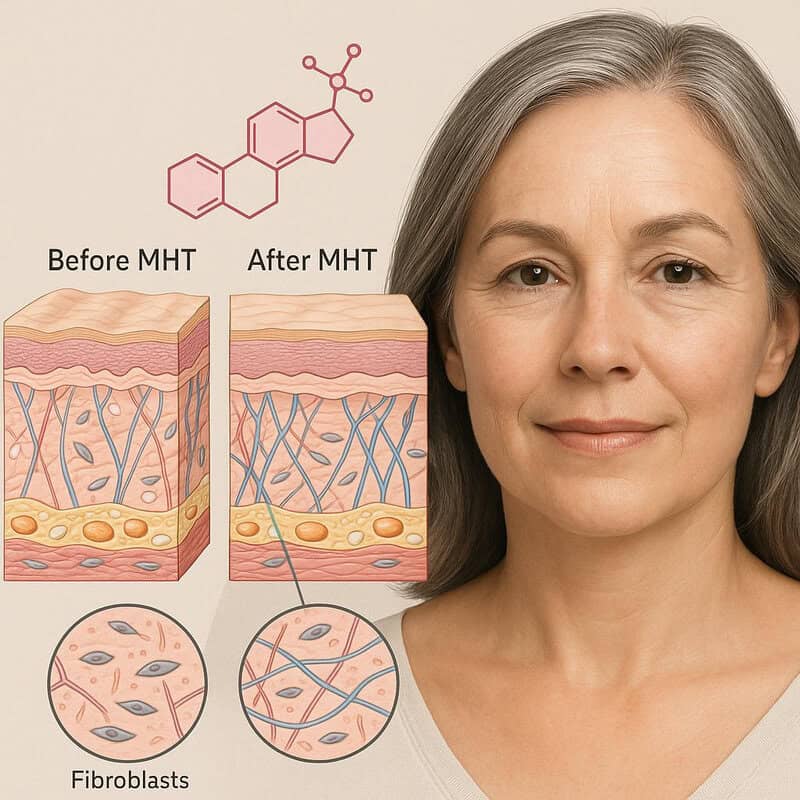
Estrogen plays a vital role in supporting collagen production and maintaining skin thickness and elasticity. During menopause, declining estrogen levels contribute to a reduction in collagen, leading to thinner, drier skin, increased wrinkling, and a loss of firmness. Menopausal hormone therapy (MHT) has been shown to slow these skin changes by replenishing estrogen, which in turn stimulates fibroblast activity and collagen synthesis (NIH Review).
Comparative studies reveal that women using hormone therapy tend to have improved skin hydration, elasticity, and fewer fine lines than those who do not use MHT. For example, a study published in Skin Pharmacology and Physiology demonstrated increased skin elasticity and thickness in postmenopausal women on estrogen therapy.
To maximize the benefits of MHT for skin health, it is recommended to follow a comprehensive skin care regimen that includes daily moisturizers, broad-spectrum sunscreen, and gentle cleansers. Consulting with a dermatologist can help tailor skin care routines and identify additional treatments, such as retinoids or antioxidants, to complement hormone therapy.
15. Potential Cardiovascular Benefits (Younger Women)
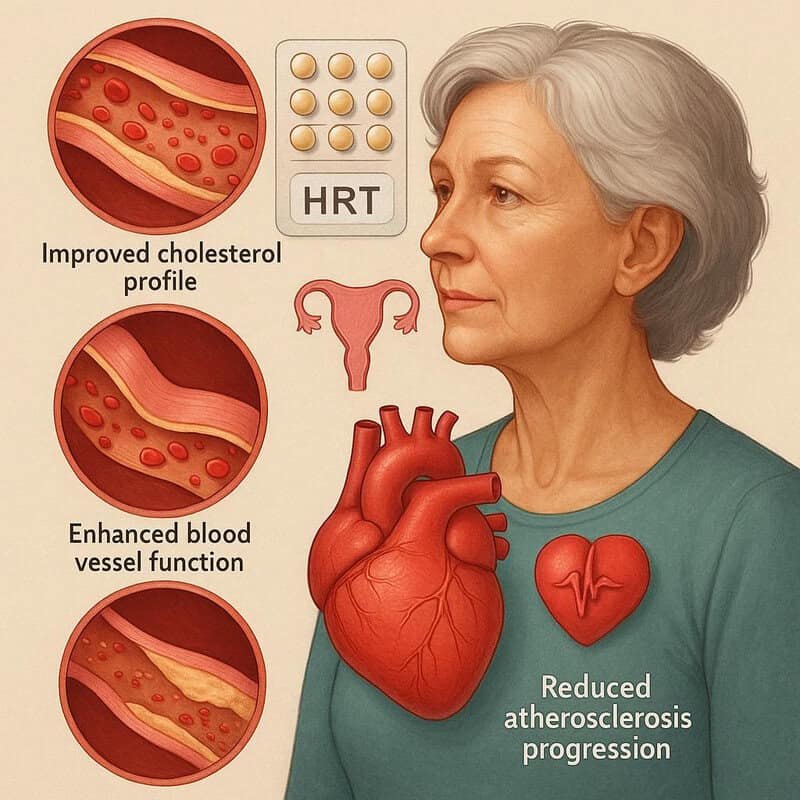
The effects of menopausal hormone therapy (MHT) on cardiovascular health are nuanced and depend greatly on the timing and age at initiation. Research suggests that starting hormone therapy in younger postmenopausal women—typically within 10 years of menopause onset or before age 60—may offer protective cardiovascular effects, such as improved cholesterol profiles, enhanced blood vessel function, and reduced atherosclerosis progression (Circulation, American Heart Association).
For instance, the KEEPS trial and other randomized studies have shown that women who began MHT near menopause had a lower risk of coronary heart disease compared to those who started therapy later or not at all. However, this benefit is not seen in women who initiate therapy many years after menopause, and risks may outweigh benefits in older populations.
It is crucial to emphasize individualized risk assessment when considering MHT for heart health. Each woman’s age, medical history, and cardiovascular risk factors must be carefully evaluated with a healthcare provider to determine whether hormone therapy is appropriate and safe for her specific situation.
16. Improved Quality of Life

Menopausal hormone therapy (MHT) is associated with significant improvements in overall wellbeing for many women navigating the menopausal transition. By alleviating distressing symptoms such as hot flashes, night sweats, sleep disturbances, vaginal discomfort, and mood changes, hormone therapy can help women regain a sense of normalcy and comfort. These improvements translate into a greater ability to engage in daily activities, maintain social relationships, and sustain productivity at work or home (NIH Review).
Studies comparing quality of life indices—such as the Menopause-Specific Quality of Life (MENQOL) questionnaire—have consistently found that women using MHT report better scores in physical, psychological, and sexual wellbeing compared to non-users. For example, clinical trials have demonstrated substantial reductions in symptom severity and improvements in self-reported life satisfaction among hormone therapy users.
To track personal health improvements, women can keep a symptom diary or use digital health apps to monitor changes in sleep, mood, energy, and discomfort. Regularly reviewing these records with a healthcare provider helps tailor treatment and celebrate progress in overall quality of life.
17. Enhanced Work Productivity

Menopausal hormone therapy (MHT) can have a positive impact on work productivity by relieving disruptive symptoms such as hot flashes, night sweats, sleep disturbances, and mood swings. These symptoms often interfere with focus, memory, and concentration, leading to reduced efficiency and increased absenteeism in the workplace. By stabilizing hormone levels and improving overall wellbeing, MHT enables women to maintain better attention to tasks and manage daily responsibilities more effectively (NIH Study).
Workplace examples include fewer missed days due to severe menopausal symptoms and improved performance in meetings or projects that require sustained mental effort. Research from the BMJ highlights that women experiencing untreated menopausal symptoms were more likely to report presenteeism (being at work but less productive) and increased use of sick leave, while those using MHT showed reduced symptom-related work impairment.
Employers are increasingly recognizing the importance of workplace support resources, such as flexible scheduling, private rest areas, and access to occupational health services. Women are encouraged to seek information about available resources and have open conversations with their managers or HR departments to create a supportive work environment.
18. Reduced Risk of Tooth Loss

Estrogen plays a crucial role in maintaining oral health by supporting the strength and integrity of gum tissues and the alveolar bone that anchors teeth. During menopause, decreased estrogen levels can accelerate bone loss in the jaw and increase the risk of periodontal disease, both of which are major contributors to tooth loss in older women. Menopausal hormone therapy (MHT) has been shown to help preserve oral bone density and support healthy gum tissues, thereby reducing the likelihood of tooth loss (NIH Review).
Comparative studies indicate that women who use hormone therapy during menopause have better dental outcomes than those who do not. For example, research published in the Journal of Dentistry found that postmenopausal women on MHT experienced less bone loss in the jaw and a lower rate of tooth extraction. This evidence highlights the value of hormone therapy not only for skeletal health but also for maintaining a healthy smile.
Regular dental checkups are vital for early detection and management of gum disease and bone loss. Women should inform their dentist about menopausal status and any hormone therapy use to ensure comprehensive oral care and optimal long-term dental health.
19. Protection Against Macular Degeneration
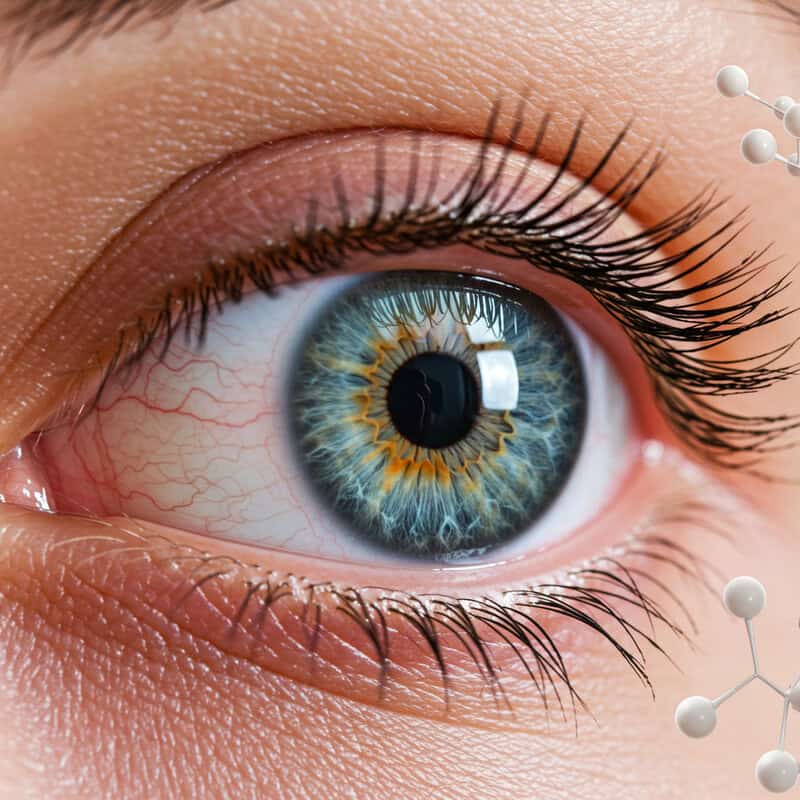
Emerging research suggests that estrogen may have a protective effect on eye health, particularly in reducing the risk of age-related macular degeneration (AMD)—a leading cause of vision loss in older adults. Estrogen is thought to support retinal blood flow and limit oxidative stress, both of which help maintain healthy retinal cells. During menopause, reduced estrogen levels could contribute to increased vulnerability to retinal damage and faster progression of AMD (NIH Review).
Population studies indicate that postmenopausal women who use hormone therapy may have a lower incidence of AMD compared to non-users. For instance, a study published in JAMA Ophthalmology found that women receiving estrogen therapy had a reduced risk of developing early-stage macular degeneration. While the exact magnitude of this benefit varies, the trend suggests a possible link between hormone therapy and preserved vision.
To optimize eye health during and after menopause, it is important to schedule regular eye screenings with an ophthalmologist. Early detection of retinal changes can help initiate timely interventions and protect against significant vision loss as women age.
20. Support for Healthy Hair
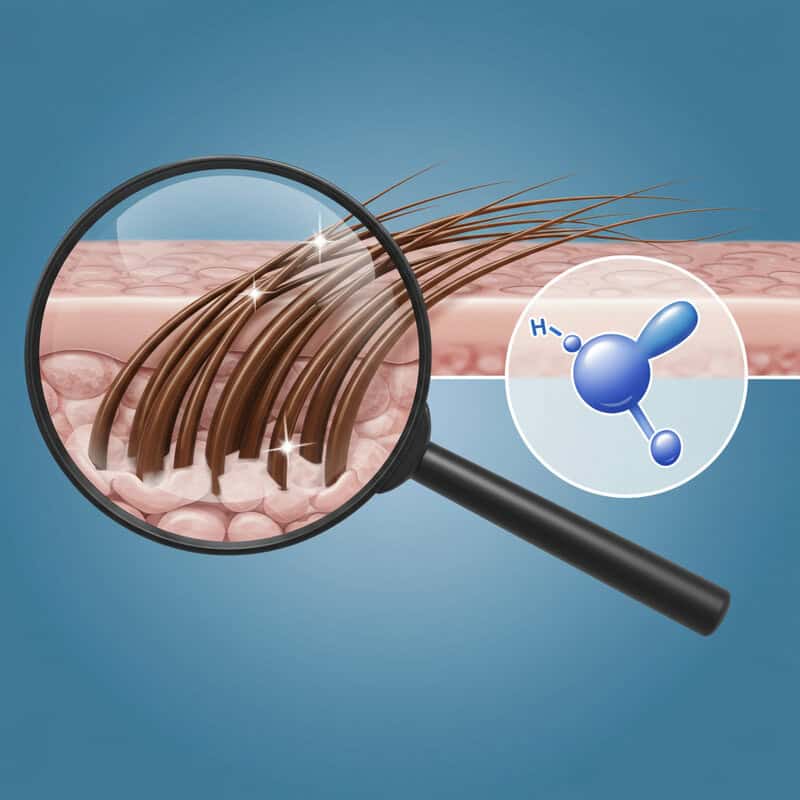
Estrogen plays an important role in maintaining hair growth and density by prolonging the growth phase of hair follicles and supporting scalp health. During menopause, declining estrogen levels often lead to hair thinning, increased shedding, and changes in hair texture. Menopausal hormone therapy (MHT) may help reduce these effects by stabilizing hormone levels, which in turn can promote healthier, fuller hair (NIH Review).
Comparative studies have shown that women who use hormone therapy are less likely to experience significant menopausal hair loss than non-users. A review in the Journal of Cosmetic Dermatology found that MHT users reported less diffuse thinning and slower progression of hair loss patterns typical of menopause, such as widened part lines and overall scalp visibility.
To complement hormone therapy, women should adopt gentle hair care practices during menopause—using mild shampoos, avoiding excessive heat styling, and maintaining a balanced diet rich in vitamins and minerals. Consulting with a dermatologist or trichologist can provide personalized strategies to address hair changes and maintain scalp health throughout the menopausal transition.
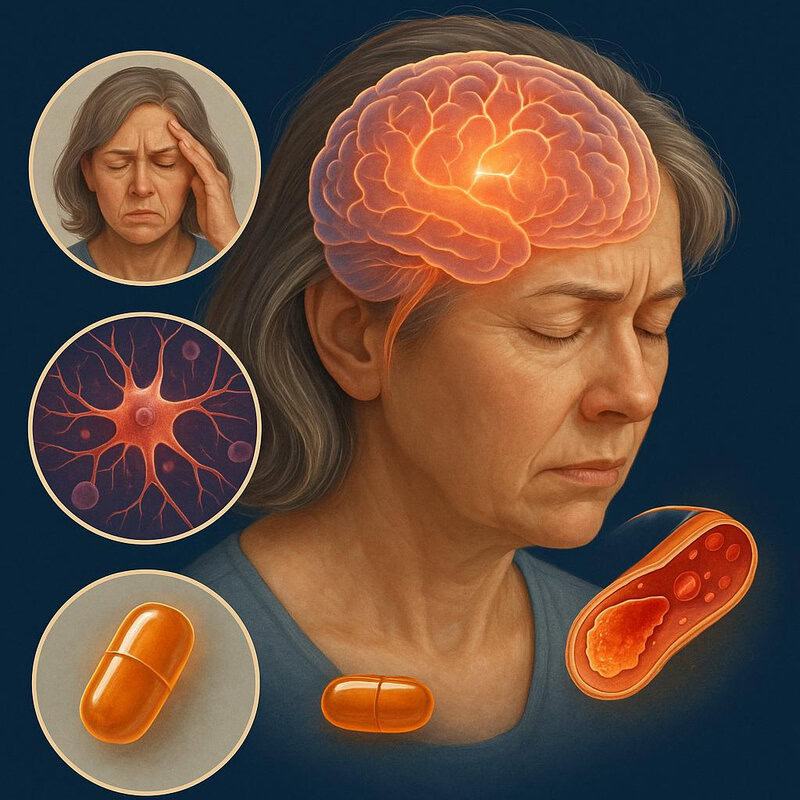
21. Decreased Severity of Migraines

Hormonal fluctuations, particularly in estrogen levels, are a well-known trigger for migraines in many women. During menopause, abrupt drops or irregularities in estrogen can lead to increased migraine frequency and severity. Menopausal hormone therapy (MHT) seeks to stabilize these hormonal shifts, which may help reduce the occurrence and intensity of migraine attacks. By providing consistent estrogen levels, MHT can lessen the hormonal volatility that often exacerbates migraines (NIH Review).
Clinical observations and studies indicate that women who experience migraines related to hormonal changes often notice a decline in migraine frequency and severity after starting hormone therapy. For example, research published in the journal Neurology found that postmenopausal women using transdermal estrogen had fewer and less intense migraines compared to those not receiving therapy. However, the response can vary, and some forms of hormone therapy may not be suitable for all migraine sufferers.
If migraines persist, worsen, or are accompanied by neurological symptoms, it is important to consult a headache specialist or neurologist. Specialist input can guide individualized treatment, including possible adjustments to hormone therapy or alternative migraine management strategies.
22. Reduced Urinary Tract Infections
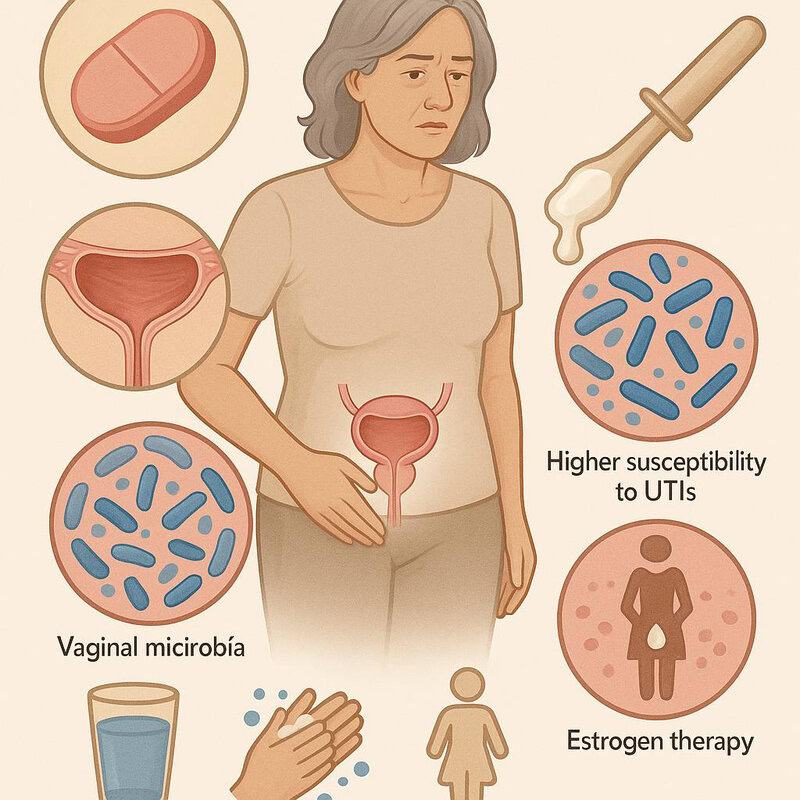
Estrogen is essential for maintaining the health of the urinary tract lining and supporting the body’s natural defenses against infection. During menopause, decreased estrogen levels lead to thinning of the urethral and bladder walls, reduced vaginal lactobacilli, and higher vaginal pH, all of which can increase susceptibility to urinary tract infections (UTIs). Menopausal hormone therapy (MHT), particularly topical estrogen, helps restore the mucosal barrier, promotes a healthy vaginal microbiome, and enhances resistance to uropathogens (NIH Study).
Comparative research shows that postmenopausal women using topical vaginal estrogen have a significantly lower rate of recurrent UTIs than those who do not use hormone therapy. For example, a study published in the Obstetrics & Gynecology journal demonstrated a marked reduction in infection recurrence among estrogen users, suggesting that hormone therapy can be a valuable adjunct in UTI prevention.
Prevention strategies include staying well-hydrated, practicing proper hygiene, urinating after intercourse, and considering topical estrogen if recurrent UTIs become problematic. Women should discuss persistent urinary symptoms or frequent infections with their healthcare provider for individualized management.
23. Enhanced Social Engagement

Relief from menopausal symptoms through hormone therapy can lead to greater confidence and willingness to participate in social activities. Symptoms such as hot flashes, sleep disturbances, mood swings, and urinary discomfort often contribute to self-consciousness, fatigue, and withdrawal from social events. By alleviating these issues, menopausal hormone therapy (MHT) helps women feel more comfortable and energetic, enabling them to engage more fully with friends, family, and community groups (NIH Review).
Studies indicate that untreated menopausal symptoms are associated with higher rates of social isolation and reduced life satisfaction. For example, research in the journal Ageing & Society found that women experiencing severe symptoms were more likely to avoid social situations, whereas those with effective symptom management, including MHT users, reported better social functioning and emotional wellbeing.
To maintain an active lifestyle, women are encouraged to join exercise classes, volunteer organizations, or hobby groups. Staying socially connected not only enriches daily life but also supports mental and physical health. Discussing symptom management with a healthcare provider can further facilitate ongoing participation in meaningful social activities.
24. Reduction in Anxiety Symptoms
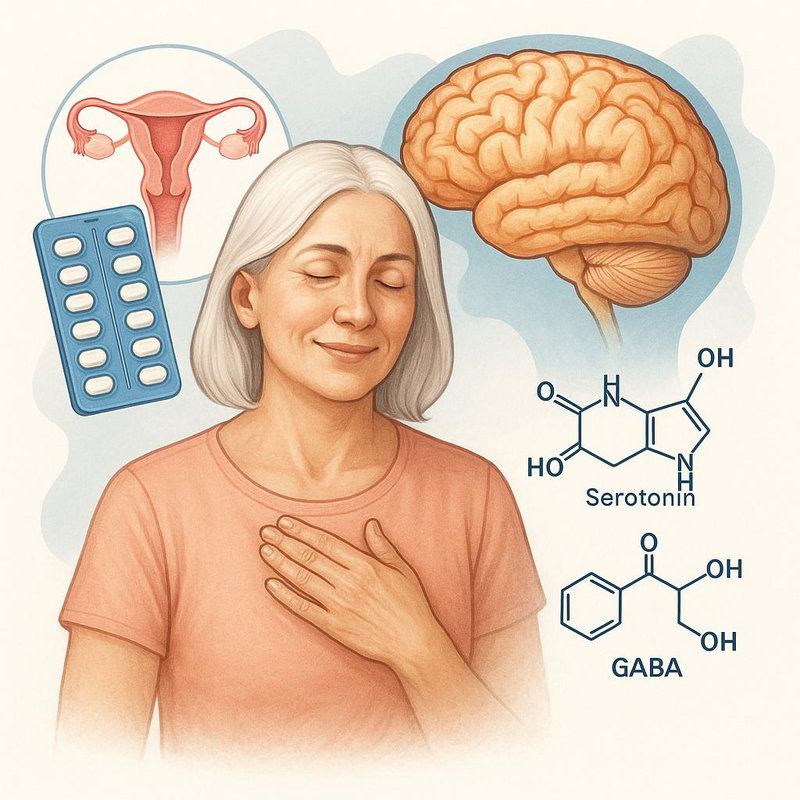
Menopausal hormone therapy (MHT) is recognized for its calming effect on mood and emotional wellbeing, including a reduction in anxiety symptoms. During menopause, declining estrogen levels can disrupt neurotransmitter balance in the brain, leading to increased anxiety, irritability, and nervousness. By replenishing estrogen, MHT helps restore balance to neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), both of which play key roles in regulating anxiety and stress responses (NIH Review).
Clinical studies show that women using hormone therapy often report lower anxiety scores compared to non-users. For example, research in the Current Psychiatry Reports found that MHT users experienced significant decreases in anxiety and panic symptoms over time, resulting in improved overall mental health and quality of life. These benefits are especially notable for women whose anxiety is closely linked to menopausal hormonal fluctuations.
Regular mental health check-ins are recommended during menopause, whether self-assessed or with a healthcare provider. Early recognition and management of anxiety symptoms can help prevent escalation and ensure that women receive the support and treatment they need for emotional wellbeing.
25. Better Weight Management

Estrogen plays a significant role in regulating metabolism, fat distribution, and appetite. During menopause, declining estrogen levels can slow metabolic rate, increase central fat accumulation, and alter how the body stores and utilizes energy. These changes often lead to weight gain, particularly around the abdomen. Menopausal hormone therapy (MHT) may help counteract some of these effects by stabilizing hormone levels and supporting a healthier metabolic profile (NIH Review).
Comparative studies indicate that women using MHT tend to experience less weight gain and a lower increase in abdominal fat than non-users. For example, research published in the Journal of Clinical Endocrinology & Metabolism found that MHT users had more favorable changes in body composition, including reduced waist circumference and lower body fat percentage over time.
For optimal weight management during menopause, it is important to combine hormone therapy with healthy diet and exercise strategies. Emphasize nutrient-dense foods, regular aerobic and strength-training exercises, and mindful eating habits. Consulting with a registered dietitian or fitness professional can help personalize an effective plan to support weight and overall health.
26. Improved Mobility

Menopausal hormone therapy (MHT) contributes to improved mobility by enhancing both bone density and joint health. Estrogen’s protective effects help maintain bone strength and reduce the risk of fractures, while its anti-inflammatory properties support healthier, more flexible joints. Together, these benefits make it easier for postmenopausal women to stay active and maintain independence as they age (NIH Review).
Comparative studies show that women using hormone therapy score better on mobility measures such as walking speed, balance, and lower body strength. For instance, research published in the Journal of Gerontology found that MHT users had a lower risk of mobility limitations and were more likely to maintain their ability to perform daily activities compared to non-users, even into older age.
If mobility issues such as persistent pain, stiffness, or difficulty with movement arise, physical therapy can be a valuable resource. Physical therapists can design individualized programs to improve strength, flexibility, and balance, complementing the benefits of MHT and helping women retain functional independence.
27. Enhanced Self-Esteem

Menopausal hormone therapy (MHT) can offer significant psychological benefits by effectively controlling distressing menopausal symptoms such as hot flashes, night sweats, mood swings, and vaginal discomfort. The alleviation of these symptoms can lead to improved confidence, positive body image, and greater satisfaction with personal health. Feeling comfortable and in control of one’s body helps many women navigate the menopausal transition with enhanced self-assurance (NIH Review).
Studies using self-esteem surveys, such as the Rosenberg Self-Esteem Scale, have shown that women who receive MHT report higher self-esteem scores compared to those who do not use hormone therapy. Research published in the Sex Roles Journal suggests that successful symptom control is closely linked to increased feelings of self-worth and overall life satisfaction during midlife and beyond.
To further support self-esteem during menopause, women are encouraged to practice regular self-care activities—such as mindfulness, physical activity, nurturing hobbies, and social engagement. Open communication with healthcare providers ensures that symptoms are managed effectively, promoting both mental and physical wellbeing.
28. Reduced Risk of Depression
Menopausal hormone therapy (MHT) has demonstrated a stabilizing effect on mood, which may help reduce the risk of developing depression during and after the menopausal transition. The hormonal fluctuations of menopause can disrupt neurotransmitter function, increasing vulnerability to depressive symptoms. MHT, by providing consistent estrogen levels, supports neurotransmitters such as serotonin and dopamine, which play critical roles in mood regulation (NIH Review).
Comparative data show that women using hormone therapy experience lower rates of depression than non-users, especially when MHT is started early in the menopausal transition. For example, a study published in JAMA Psychiatry found that perimenopausal and early postmenopausal women on estrogen therapy had significantly fewer depressive episodes and improved emotional wellbeing compared to those not using MHT.
Regular mental health screenings are important for women in midlife, as early detection of depressive symptoms allows for timely intervention. Open discussions with healthcare providers about mood changes, combined with appropriate therapy, can ensure optimal mental health throughout the menopausal years.
29. Prevention of Genital Atrophy
Estrogen is crucial for maintaining the health and integrity of genital tissues, including the vulva and vagina. During menopause, declining estrogen levels can lead to genital atrophy—characterized by thinning, dryness, and decreased elasticity of the vaginal and vulvar tissues. These changes can cause symptoms such as itching, burning, pain during intercourse (dyspareunia), and an increased risk of infections. Menopausal hormone therapy (MHT), especially in the form of local or topical estrogen, helps restore moisture, thickness, and elasticity to genital tissues, alleviating discomfort and promoting overall genital health (Mayo Clinic).
Women who use hormone therapy generally report fewer and less severe symptoms of genital atrophy compared to those who do not use MHT. Studies, such as those referenced by the American College of Obstetricians and Gynecologists (ACOG), highlight the effectiveness of both systemic and local estrogen therapies in reversing atrophic changes and improving quality of life.
Women experiencing persistent vaginal dryness, pain, or recurrent urinary or genital infections should seek gynecological care. Early intervention can prevent complications, ensure proper diagnosis, and guide individualized treatment for optimal comfort and sexual health.
30. Reduced Risk of Atrial Fibrillation

Menopausal hormone therapy (MHT) may have a protective effect on heart rhythm, particularly regarding the risk of atrial fibrillation (AF)—a common cardiac arrhythmia that increases with age and is more prevalent in postmenopausal women. Estrogen is believed to influence cardiac electrical activity and vascular health, potentially reducing the susceptibility to abnormal heart rhythms. Recent studies have suggested that women who use hormone therapy, especially when initiated near menopause, exhibit a lower incidence of atrial fibrillation compared to non-users (Circulation: Cardiovascular Outcomes).
A large cohort study published in European Heart Journal found that recent users of hormone therapy had a significantly reduced risk of developing AF, with the benefit most pronounced among younger postmenopausal women. However, the effects may vary based on the type and timing of hormone therapy, and individual cardiovascular risk profiles must always be considered.
Regular heart monitoring—including check-ups, blood pressure measurement, and, if indicated, electrocardiograms—is advisable for women using MHT, particularly those with a history of cardiovascular issues. Early detection of rhythm changes can help prevent complications and ensure optimal heart health.
31. Lowered Risk of Hip Fractures

Bone density is a crucial factor in the prevention of hip fractures, which are among the most serious and debilitating injuries for postmenopausal women. The decline in estrogen during menopause accelerates bone loss, weakening the hip and increasing the risk of fractures even with minor falls. Menopausal hormone therapy (MHT) helps maintain bone mineral density, thereby strengthening the hip and reducing fracture susceptibility (NIH Review).
Comparative studies have shown that women using hormone therapy experience significantly lower rates of hip fractures compared to non-users. For example, data from the Lancet Diabetes & Endocrinology and the Women’s Health Initiative demonstrated reductions in hip fracture risk by as much as 34% among MHT users. These findings underscore the beneficial effect of hormone therapy on skeletal health, particularly for women at higher risk of osteoporosis.
To optimize bone health, screening intervals for bone mineral density (BMD) are generally recommended every 1-2 years for women with risk factors or those over age 65. Early and regular screening enables timely intervention to prevent hip fractures and maintain mobility and independence.
32. Improved Blood Lipid Profiles
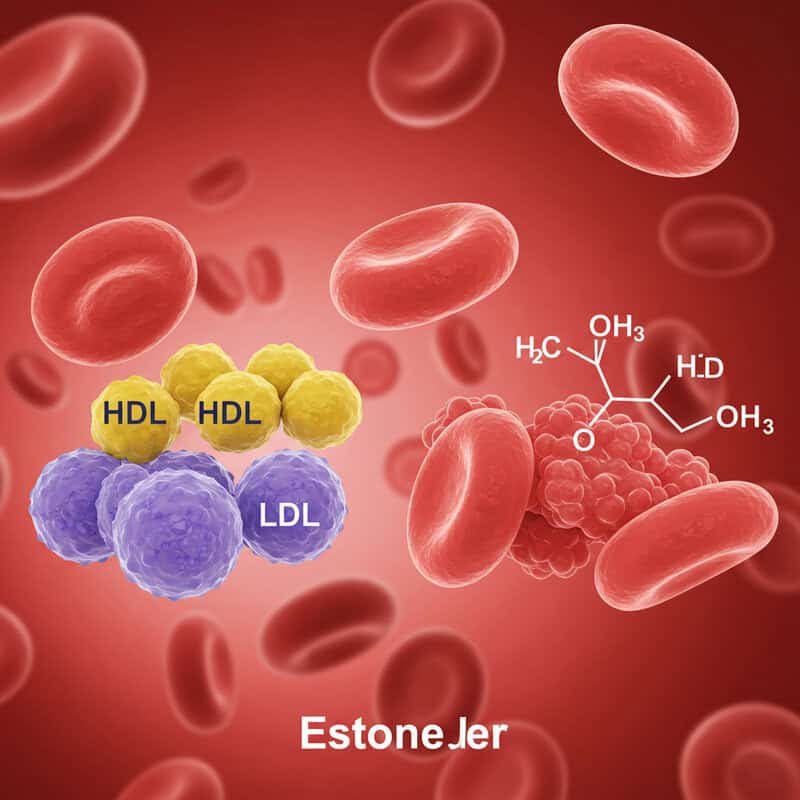
Estrogen plays a significant role in regulating blood lipid levels, which are vital for cardiovascular health. During menopause, declining estrogen levels can lead to unfavorable changes in cholesterol, including higher low-density lipoprotein (LDL or “bad” cholesterol) and lower high-density lipoprotein (HDL or “good” cholesterol). Menopausal hormone therapy (MHT) helps counteract these changes by raising HDL and lowering LDL levels, thereby contributing to a healthier lipid profile and potentially reducing cardiovascular risk (NIH Review).
Comparative clinical studies reveal that women using MHT have improved cholesterol and triglyceride levels compared to non-users. A meta-analysis in the journal Circulation found that oral estrogen therapy increased HDL, reduced LDL, and lowered total cholesterol. These favorable changes are most notable when hormone therapy is started during early menopause, although individual responses may vary depending on the type and route of therapy.
Women using hormone therapy or concerned about cardiovascular health should have regular blood tests to monitor cholesterol and triglyceride levels. Ongoing assessment helps tailor therapy, guide lifestyle modifications, and support long-term heart health.
33. Enhanced Wound Healing
Estrogen has a notable influence on the body’s wound healing processes, particularly through its effect on skin repair and regeneration. Estrogen stimulates the production of collagen and promotes angiogenesis (the formation of new blood vessels), both of which are essential for tissue recovery after injury. During menopause, reduced estrogen can slow these processes, often leading to delayed or impaired healing of cuts, scrapes, or surgical wounds. Menopausal hormone therapy (MHT) may help restore these healing mechanisms, resulting in faster and more effective wound repair (NIH Review).
Comparative studies indicate that postmenopausal women using hormone therapy tend to experience shorter wound healing times and improved skin integrity compared to non-users. For instance, research published in the Journal of Investigative Dermatology has shown enhanced recovery rates and less scarring among MHT users, further emphasizing estrogen’s reparative benefits.
If wounds are slow to heal, become infected, or show signs of poor recovery, it is important to seek medical attention. Proper wound care, combined with hormone therapy if indicated, can help optimize healing and prevent complications during and after menopause.
34. Less Frequent Mood Swings
One of the notable benefits of menopausal hormone therapy (MHT) is the stabilization of hormone levels, which directly influences emotional regulation. Fluctuating estrogen during menopause can disrupt neurotransmitter activity in the brain, often resulting in sudden mood changes, irritability, or emotional lability. By providing consistent hormone levels, MHT helps reduce the frequency and intensity of mood swings, allowing for a smoother emotional experience throughout the menopausal transition (NIH Review).
Comparative studies have shown that women using hormone therapy report fewer and less severe mood swings compared to non-users. For example, research in the journal Menopause found that MHT users experienced significant improvements in emotional stability and overall psychological wellbeing. This improvement is particularly helpful for women who experienced pronounced mood fluctuations prior to therapy.
To monitor progress, women are encouraged to use mood-tracking strategies such as journaling, mood-tracking apps, or regular self-assessment scales. Sharing these records with a healthcare provider can help tailor therapy and provide additional support for emotional health during menopause.
35. Improved Bone Healing
Estrogen is essential not just for maintaining bone density but also for supporting bone repair and regeneration after injury. It enhances the activity of osteoblasts (cells responsible for bone formation) and helps regulate bone remodeling. During menopause, the decline in estrogen levels can impair the healing process, resulting in slower or less effective recovery from fractures and bone injuries. Menopausal hormone therapy (MHT) has been shown to accelerate bone repair by restoring hormonal balance and promoting the cellular mechanisms necessary for healing (NIH Review).
Comparative studies have found that postmenopausal women receiving hormone therapy experience faster and more complete bone healing than those who do not use MHT. For example, research in the Journal of Orthopaedic Trauma noted shorter healing times and better bone quality in MHT users following fractures.
For optimal bone injury recovery, women should follow medical advice, maintain a balanced diet rich in calcium and vitamin D, avoid smoking and excessive alcohol, and engage in safe, weight-bearing exercises as healing allows. Prompt rehabilitation and regular follow-up with healthcare providers can further enhance recovery outcomes.
36. Lowered Risk of Dental Disease

Estrogen plays a vital role in maintaining oral and dental health by supporting the strength of gum tissue, promoting blood flow, and preserving bone density in the jaw. During menopause, declining estrogen levels can lead to increased susceptibility to periodontal (gum) disease, tooth decay, and bone loss, all of which heighten the risk for dental disease. Menopausal hormone therapy (MHT) helps counter these changes by improving oral tissue resilience and supporting healthy bone around the teeth (NIH Review).
Comparative research shows that postmenopausal women using hormone therapy have lower rates of dental disease than non-users. For example, a study in the Journal of the American Dental Association found that MHT users experienced less gum recession, reduced pocket depth, and lower rates of tooth loss. This evidence highlights the oral health benefits of maintaining hormonal balance throughout the menopausal transition.
Regular dental visits—including professional cleanings and oral exams—are crucial for early detection and management of dental issues. Women should inform their dentist about menopause status and any hormone therapy use to ensure comprehensive, personalized care for lifelong oral health.
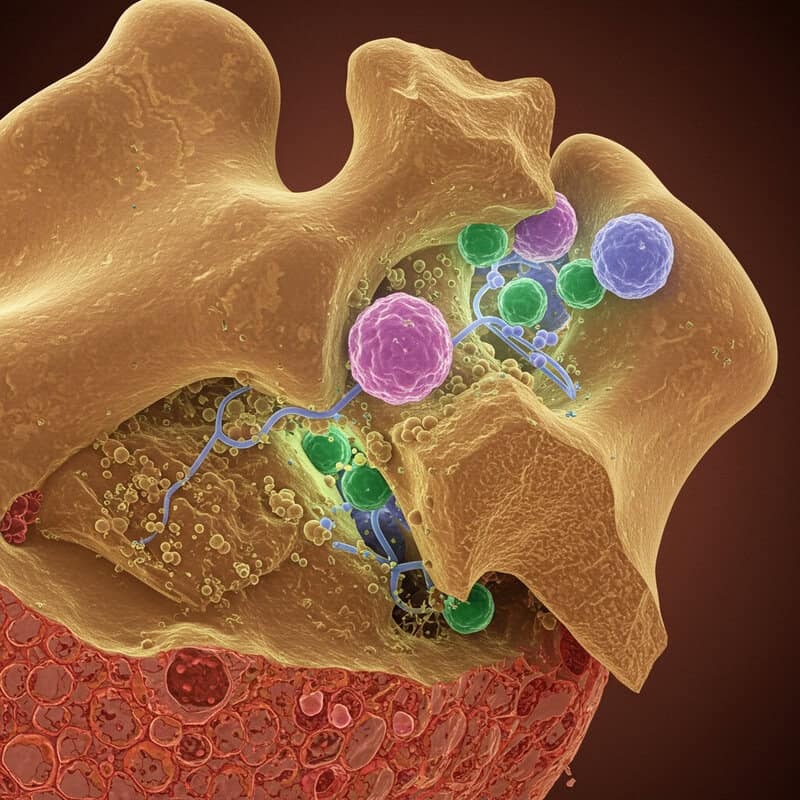
37. Support for Immune Function

Estrogen plays a significant role in modulating immune system function, influencing both innate and adaptive immune responses. During menopause, declining estrogen levels can lead to alterations in immune cell activity, potentially increasing susceptibility to infections and reducing the body’s ability to mount effective immune responses. Menopausal hormone therapy (MHT) may help restore some of this immune balance by supporting the production and function of immune cells such as lymphocytes and macrophages (NIH Review).
Comparative studies suggest that postmenopausal women using hormone therapy may experience lower rates of certain infections and improved immune markers compared to non-users. For example, research in the journal Frontiers in Immunology found that estrogen supplementation supports better regulation of inflammatory responses, which can help protect against both chronic and acute illnesses.
To further bolster immune health, women are encouraged to maintain up-to-date vaccinations, such as annual influenza and recommended adult boosters. A healthy lifestyle—including balanced nutrition, regular exercise, and adequate sleep—also plays a key role in supporting optimal immune function throughout menopause and beyond.
38. Improved Concentration

Menopausal hormone therapy (MHT) has been shown to provide cognitive benefits, particularly in the areas of focus and attention. Declining estrogen levels during menopause can impact neurotransmitter function in brain regions responsible for concentration and working memory, leading many women to experience “brain fog” or trouble maintaining attention. MHT may help counteract these effects by supporting synaptic plasticity and enhancing blood flow to the brain, leading to clearer thinking and improved ability to concentrate (NIH Review).
Comparative studies indicate that women using hormone therapy report better focus and cognitive performance than non-users. For example, research published in Frontiers in Aging Neuroscience found that MHT users demonstrated higher scores on cognitive tests involving sustained attention and executive function, especially when therapy began near the onset of menopause.
To further support mental clarity, women are encouraged to incorporate mental exercises into their daily routines. Activities such as puzzles, memory games, learning new skills, and regular reading can help maintain cognitive sharpness and reinforce the benefits of hormone therapy for concentration and brain health.
39. Reduced Risk of Metabolic Syndrome
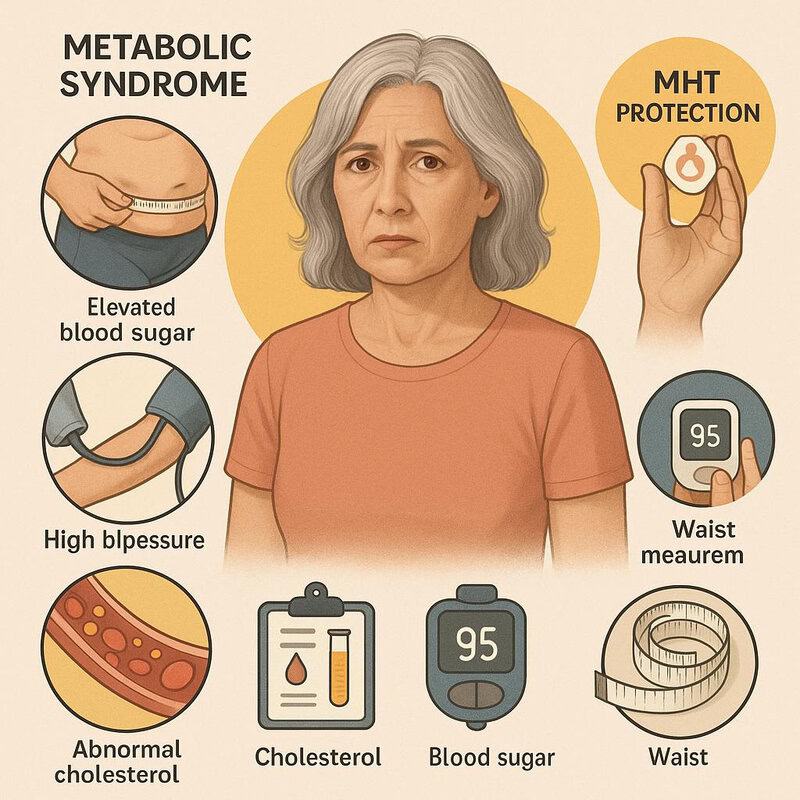
Metabolic syndrome is a cluster of conditions—including increased waist circumference, high blood pressure, elevated blood sugar, and abnormal cholesterol levels—that together raise the risk for cardiovascular disease and type 2 diabetes. During menopause, declining estrogen levels can contribute to the development of these risk factors, making postmenopausal women more susceptible to metabolic syndrome. Menopausal hormone therapy (MHT) offers protective effects by improving insulin sensitivity, supporting healthier lipid profiles, and helping to regulate fat distribution (NIH Review).
Comparative studies demonstrate that women using hormone therapy have lower prevalence of metabolic syndrome and its individual risk factors compared to non-users. For example, research published in the Journal of Clinical Endocrinology & Metabolism found that MHT users experienced improvements in waist circumference, blood pressure, triglycerides, and fasting glucose levels.
To monitor and reduce the risk of metabolic syndrome, women are encouraged to have regular health checks that include blood pressure, cholesterol, blood sugar, and waist measurements. Early detection and comprehensive management, including lifestyle modifications and appropriate therapy, are key to maintaining metabolic health through menopause and beyond.
40. Support for Blood Vessel Health
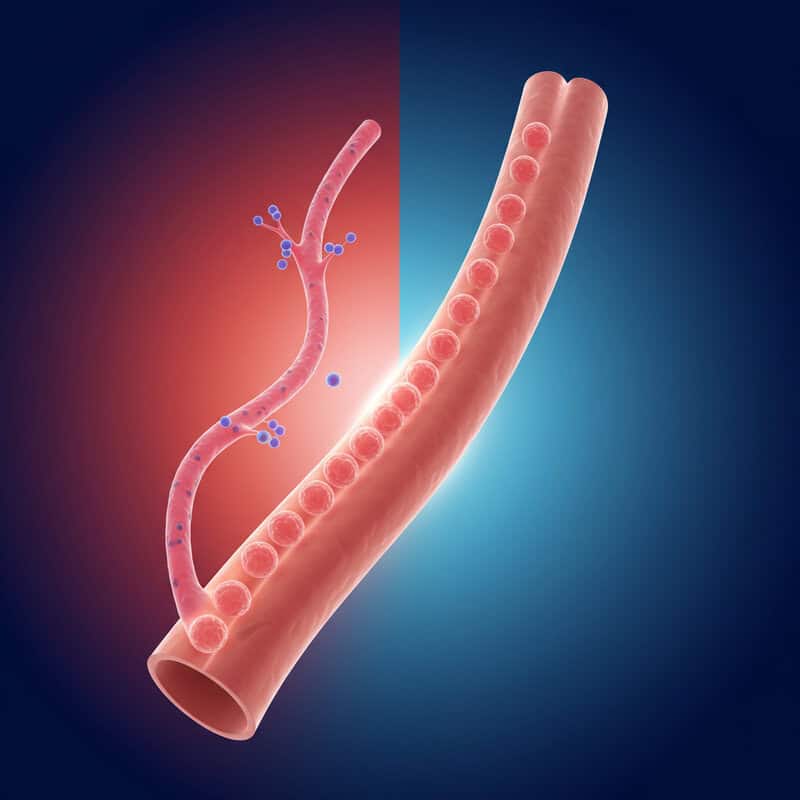
Estrogen plays a crucial role in maintaining vascular health by promoting blood vessel elasticity, reducing inflammation, and supporting healthy endothelial function. During menopause, the decline in estrogen levels can lead to stiffer arteries and increased vascular resistance, which in turn elevate the risk of hypertension and cardiovascular disease. Menopausal hormone therapy (MHT) may help preserve vascular function by enhancing the production of nitric oxide, a molecule that relaxes blood vessels and improves circulation (AHA Circulation).
Comparative studies have found that women using hormone therapy exhibit greater blood vessel elasticity and lower measures of arterial stiffness than non-users. For example, research published in the European Heart Journal reported improved vascular compliance and reduced progression of arterial aging among MHT users, particularly when therapy was initiated early in the postmenopausal period.
It is important for women—especially those on hormone therapy—to monitor blood pressure regularly and report any significant changes to their healthcare provider. Routine monitoring helps detect early signs of vascular issues and ensures that both therapy and lifestyle interventions optimally support long-term heart and vessel health.
41. Reduction of Palpitations

Many women experience heart palpitations—the sensation of a racing, fluttering, or irregular heartbeat—during menopause due to fluctuating hormone levels, particularly estrogen. These hormonal changes can disrupt the autonomic nervous system’s regulation of heart rhythm, leading to uncomfortable or anxiety-provoking episodes. Menopausal hormone therapy (MHT) helps stabilize estrogen levels, which can have a calming effect on the cardiovascular system and reduce the frequency and severity of palpitations (NIH Review).
Women who use MHT often report fewer or milder palpitations compared to those who do not receive treatment. A study published in the journal Menopause found that untreated menopausal symptoms were associated with a higher incidence and greater distress from palpitations, while those on hormone therapy experienced significant relief. This effect can contribute to improved comfort, reduced anxiety, and a greater sense of cardiac stability during menopause.
If new or persistent palpitations occur, especially if accompanied by chest pain, dizziness, or shortness of breath, it is important to seek medical evaluation. Early assessment helps rule out underlying cardiovascular conditions and ensures appropriate management and peace of mind.
42. Reduced Incidence of Breast Pain
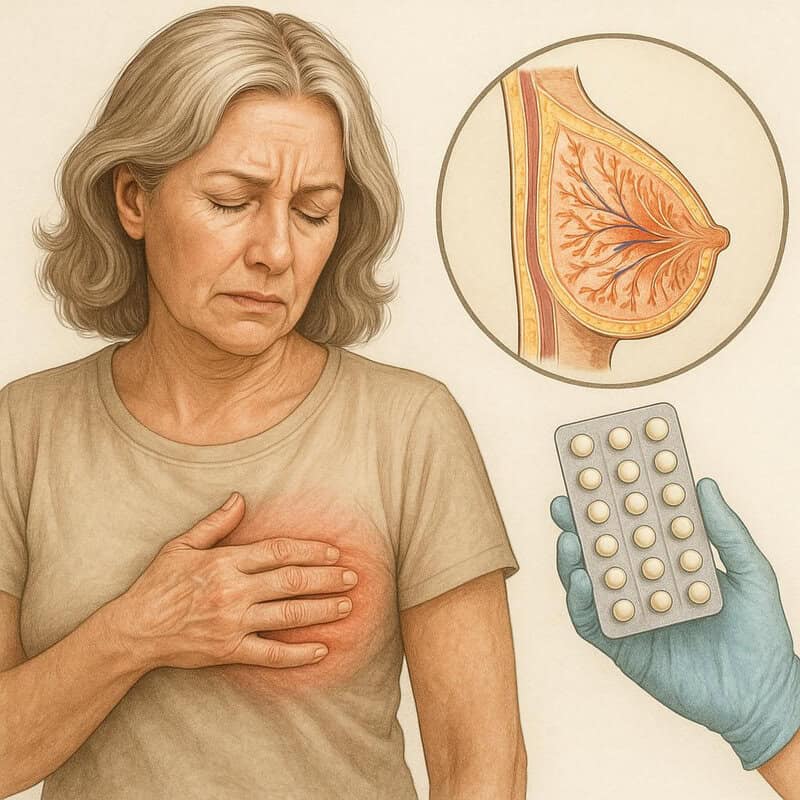
Estrogen significantly influences breast tissue health, and fluctuations in hormone levels during menopause can lead to changes in breast structure and sensitivity. Many women experience cyclical or persistent breast pain (mastalgia) as estrogen levels vary. Menopausal hormone therapy (MHT), when appropriately dosed, can help stabilize hormonal fluctuations, reducing the occurrence, duration, and intensity of breast pain in many postmenopausal women (NIH Review).
Comparative studies have shown that women using MHT—especially those on lower, steady doses—tend to report fewer and less severe episodes of breast pain than women with untreated menopausal symptoms or those using high-dose regimens. For example, research in the journal Menopause found that consistent hormone therapy use was associated with a reduction in pain frequency and severity, contributing to improved comfort and quality of life.
Regardless of pain severity, routine breast self-exams and regular clinical breast screenings remain essential for all women during and after menopause. These practices ensure early detection of any changes and provide reassurance about breast health while using hormone therapy.
43. Improved Hand and Grip Strength

Estrogen supports musculoskeletal health by maintaining muscle mass, tendon elasticity, and bone density—all essential for hand function and grip strength. During menopause, declining estrogen levels can accelerate muscle loss and reduce neuromuscular efficiency, leading to weaker hand strength and diminished dexterity. Menopausal hormone therapy (MHT) helps to mitigate these changes by preserving muscle fibers and supporting the connective tissue structure, which translates to improved grip and hand function (NIH Review).
Comparative research demonstrates that women using MHT tend to have better grip strength and slower decline in hand function than non-users. A study published in the Age and Ageing journal found that postmenopausal women on hormone therapy maintained higher hand grip strength, which is a key indicator of overall musculoskeletal health and functional independence.
To further support hand and grip strength, aging women are encouraged to engage in regular strength training exercises that target the hands, wrists, and forearms, such as squeezing stress balls, using grip trainers, or resistance band routines. Incorporating these activities into a broader fitness program can help sustain function and quality of life with age.
44. Lowered Risk of Cataracts

Estrogen has been shown to have a protective effect on the eye lens, supporting antioxidant defenses and reducing the risk of oxidative damage that can lead to cataract formation. As estrogen levels decline during menopause, the eye lens becomes more susceptible to clouding and protein aggregation, which are hallmarks of cataracts. Menopausal hormone therapy (MHT) may help maintain lens clarity and delay cataract development by supporting ocular metabolism and reducing inflammation within eye tissues (NIH Review).
Comparative studies have reported that women who use hormone therapy have lower rates of cataracts and delayed onset of lens opacity compared to non-users. A large cohort study published in JAMA Ophthalmology found a statistically significant reduction in cataract risk among postmenopausal women receiving MHT, suggesting a link between hormone balance and eye health.
To support lifelong vision health and detect any changes early, women are encouraged to have regular eye exams with an ophthalmologist. Eye screenings help monitor lens clarity, identify cataracts in their earliest stages, and guide timely interventions as needed.
45. Support for Thyroid Function
Emerging research suggests that there is cross-talk between estrogen and thyroid hormones, both of which are vital for regulating metabolism, energy levels, and overall endocrine health. Estrogen may influence thyroid hormone production, conversion, and action at cellular receptors, while thyroid hormones can impact estrogen metabolism. During menopause, fluctuating or declining estrogen levels can unmask or exacerbate underlying thyroid dysfunction, leading to symptoms such as fatigue, weight changes, and mood disturbances. Menopausal hormone therapy (MHT) may help stabilize this delicate hormonal interplay, potentially supporting more balanced thyroid function (NIH Review).
Comparative studies have shown that women on hormone therapy often experience more stable thyroid hormone levels and report fewer thyroid-related symptoms than non-users. For example, research in the journal Menopause found that MHT can influence thyroid function tests and may offer a protective effect against certain thyroid disorders in postmenopausal women.
Given the overlapping symptoms of menopause and thyroid dysfunction, it is essential for women to have regular thyroid screening during midlife. Early identification and management of thyroid imbalances can optimize energy, mood, and metabolic health throughout menopause.
46. Improved Gut Health
Emerging research highlights a fascinating connection between estrogen and gut microbiota, the diverse community of microorganisms living in the digestive tract. Estrogen influences the composition and diversity of gut bacteria, which in turn can impact nutrient absorption, immune function, and inflammation. During menopause, declining estrogen levels may disrupt this balance, potentially leading to increased digestive symptoms such as bloating, irregular bowel movements, or discomfort. Menopausal hormone therapy (MHT) may help support a healthier gut microbiome, thereby improving overall digestive health (NIH Review).
Comparative studies suggest that women using hormone therapy experience fewer gastrointestinal complaints and better gut function than non-users. For instance, research published in Frontiers in Microbiology found that MHT users had greater microbial diversity and reduced inflammation, correlating with improved digestion and less abdominal discomfort.
To further support gut health during menopause, women should consider dietary modifications such as increasing fiber intake, consuming probiotic-rich foods (like yogurt and kefir), and staying well-hydrated. Consulting a healthcare provider or dietitian can help tailor dietary strategies to complement the benefits of hormone therapy for digestive wellbeing.
47. Enhanced Pain Tolerance
Estrogen has a significant impact on pain perception and tolerance by modulating neurotransmitters and inflammatory pathways in the central nervous system. During menopause, declining estrogen levels can heighten pain sensitivity, making women more prone to chronic pain conditions such as headaches, joint pain, and muscle aches. Menopausal hormone therapy (MHT) may help increase pain thresholds and reduce the intensity of both acute and chronic pain by restoring hormonal balance and dampening inflammatory responses (NIH Review).
Comparative studies indicate that women using hormone therapy generally demonstrate higher pain tolerance and report less frequent or severe pain than those not on MHT. Research published in The Clinical Journal of Pain has shown that estrogen supplementation may reduce pain sensitivity and improve quality of life for postmenopausal women with pain-related complaints.
For optimal pain management, women are encouraged to combine hormone therapy with holistic pain strategies such as regular physical activity, stress reduction techniques, physical therapy, and the use of over-the-counter or prescribed pain relief when necessary. Consulting a healthcare provider ensures individualized and effective pain control.
48. Reduced Incidence of Dry Eyes

Menopause is commonly associated with an increased risk of dry eye syndrome, a condition characterized by insufficient tear production and discomfort. Estrogen helps regulate the function of the lacrimal glands, which are responsible for producing tears and maintaining proper eye lubrication. With declining estrogen levels during menopause, these glands may become less efficient, resulting in dryness, irritation, and blurred vision. Menopausal hormone therapy (MHT) can help restore hormonal balance and support healthier tear production, thereby reducing the prevalence and severity of dry eye symptoms (NIH Review).
Comparative studies show that women using hormone therapy tend to report fewer complaints of dry eyes than those who are not on MHT. Research published in the journal Cornea found improved tear film stability and decreased incidence of dry eye symptoms among MHT users.
Women experiencing persistent eye dryness are encouraged to use eye care strategies such as artificial tears, humidifiers, and avoiding irritants (like wind or smoke). For ongoing discomfort, an eye care professional can recommend tailored treatments and assess for other underlying eye conditions.
49. Improved Sense of Wellbeing

Menopausal hormone therapy (MHT) is associated with a holistic enhancement of overall wellbeing for many women experiencing menopause. By alleviating a wide array of symptoms—ranging from hot flashes and night sweats to mood swings, sleep disturbances, and joint pain—MHT allows women to regain vitality, energy, and emotional balance. This comprehensive symptom relief fosters a more positive outlook and a greater sense of control over one’s health during the menopausal transition (NIH Review).
Studies comparing wellbeing scores, such as those using the Menopause-Specific Quality of Life (MENQOL) questionnaire, consistently show that women on hormone therapy report higher levels of overall satisfaction, self-confidence, and daily functioning than non-users. For example, research published in the International Journal of Women’s Health found significant improvements in physical, emotional, and social wellbeing among MHT users.
To sustain and monitor this improved sense of wellbeing, women should engage in ongoing health monitoring with regular check-ups, symptom tracking, and open communication with healthcare providers. This proactive approach ensures that therapy remains effective and that health and happiness are prioritized throughout menopause and beyond.
50. Greater Autonomy in Health Decisions

Access to accurate information and education about menopausal hormone therapy (MHT) empowers women to make informed decisions about their health. Understanding the benefits, risks, and alternatives allows women to actively participate in choosing the treatment plan that best fits their needs, values, and lifestyle. This sense of autonomy has been linked to greater confidence, reduced decisional regret, and improved satisfaction with healthcare outcomes (NIH Review).
Comparative studies have shown that women who are well-informed and engage in shared decision-making with their healthcare providers report higher satisfaction with their health choices and better adherence to therapy. For example, research published in BMJ highlights that shared decision-making leads to increased patient empowerment and trust in clinical care, particularly in complex areas like menopause management.
Women are encouraged to seek open, collaborative discussions with their healthcare providers, ask questions, and express their goals and concerns. This shared decision-making approach ensures that treatment decisions are truly personalized, enhancing both health outcomes and the confidence to navigate menopause on one’s own terms.
Conclusion

Understanding the broad range of benefits associated with menopausal hormone therapy (MHT) is essential for informed, proactive health management during the menopausal transition. Timely evaluation of menopausal symptoms can lead to effective intervention, improve quality of life, and reduce the risk of long-term complications. Women are encouraged to maintain open communication with their healthcare providers, discuss personal goals and concerns, and undergo recommended screenings to ensure safe and optimal therapy outcomes. Utilizing reputable resources, such as the NIAMS Menopause Resource, can further support well-informed decisions. With collaborative care and regular monitoring, women can confidently navigate menopause and embrace this new stage of life.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





