Nutritional Support for Autoimmune Conditions
Autoimmune diseases affect over 50 million people in the United States alone and are estimated to impact 5-10% of the global population, according to the National Institute of Allergy and Infectious Diseases and the World Health Organization. These conditions result from the immune system mistakenly attacking the body’s own tissues. A major challenge is the frequent late detection or diagnosis, often due to overlapping symptoms with other illnesses, complicating effective intervention.
1. Omega-3 Fatty Acids

Omega-3 fatty acids, particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are renowned for their potent anti-inflammatory properties. Research has shown that omega-3s can help modulate immune system activity and reduce inflammation, which is especially beneficial for individuals with autoimmune conditions. For example, studies have demonstrated that supplementation with fish oil, a rich source of EPA and DHA, can decrease joint pain and stiffness in patients with rheumatoid arthritis (source). These fatty acids work by inhibiting the production of pro-inflammatory cytokines and eicosanoids, thereby dampening the excessive immune response often seen in autoimmune disorders.
Increasing omega-3 intake can be achieved through dietary sources such as fatty fish (salmon, sardines, mackerel, and trout), flaxseeds, chia seeds, and walnuts. For those who do not consume enough omega-3-rich foods, high-quality fish oil supplements are widely available and can be used to bridge nutritional gaps. It is recommended to consult with a healthcare provider before starting supplementation to determine appropriate dosing and ensure safety, especially for individuals taking medications that affect blood clotting (source).
2. Vitamin D
Vitamin D plays a critical role in immune system regulation by modulating both innate and adaptive immune responses. It enhances the pathogen-fighting effects of monocytes and macrophages and helps prevent the immune system from attacking the body’s own tissues. Deficiency in vitamin D has been strongly associated with the development and progression of several autoimmune diseases, notably multiple sclerosis (MS). Epidemiological studies indicate that individuals with low vitamin D levels have a higher risk of developing MS, and supplementation may offer protective benefits (source).
Safe supplementation involves first assessing vitamin D status through a blood test, as excessive intake can lead to toxicity. For most adults, the recommended dietary allowance ranges from 600 to 800 IU daily, though higher dosages may be required to correct deficiencies. Vitamin D can be obtained from sunlight exposure, fortified foods, fatty fish, and supplements. It is important to consult a healthcare provider for personalized dosage recommendations and to monitor blood levels periodically. Combining vitamin D supplements with meals containing healthy fats can improve absorption (source).
3. Probiotics

Probiotics are beneficial live microorganisms that help maintain a balanced gut microbiome, which plays a pivotal role in immune system function. Disruptions in the composition of gut bacteria have been linked to the onset and exacerbation of autoimmune diseases. In conditions like ulcerative colitis, studies have shown that probiotics can help reduce inflammation and promote remission. For instance, a clinical trial demonstrated that certain probiotic strains, such as Escherichia coli Nissle 1917, were as effective as standard medication in maintaining remission in patients with ulcerative colitis (source).
To support a healthy gut microbiome, individuals can incorporate probiotic-rich foods into their diets, such as yogurt with live cultures, kefir, sauerkraut, kimchi, miso, and tempeh. For those who may not consume these foods regularly, high-quality probiotic supplements are available and provide a convenient alternative. When choosing a supplement, it is important to look for products that contain well-researched strains and list viable colony-forming units (CFUs). Consulting a healthcare professional can help tailor probiotic use to individual needs, especially for those with compromised immune systems (source).
4. Fermented Foods

Fermented foods are rich in naturally occurring probiotics, which can enhance immune function by supporting a healthy and diverse gut microbiome. The fermentation process promotes the growth of beneficial bacteria, which in turn helps regulate immune responses and reduces inflammation—an important factor in managing autoimmune conditions. Kimchi, a traditional Korean fermented vegetable dish, and sauerkraut, a type of fermented cabbage, are both excellent sources of probiotics and have been shown to positively impact immune health. Research has demonstrated that regular consumption of kimchi can modulate immune activity and improve gut barrier function (source).
Including fermented foods in the daily diet is a practical way to support immune health. It is generally recommended to start with small amounts, such as 1-2 tablespoons per day, and gradually increase intake as tolerated. Other options include yogurt with live cultures, kefir, tempeh, and miso. Individuals should look for unpasteurized or raw versions, as heat-treated products may not contain viable probiotics. As with all dietary changes, it is wise to monitor for individual tolerance and consult a healthcare provider if there are concerns about introducing new foods (source).
5. Antioxidant-Rich Berries

Berries are among the most potent sources of dietary antioxidants, which help combat oxidative stress and inflammation—key contributors to autoimmune disease progression. Blueberries, in particular, are renowned for their high levels of anthocyanins, a class of flavonoids with strong antioxidative and anti-inflammatory effects. Studies have shown that blueberries possess greater antioxidant capacity compared to many other fruits, including apples and bananas (source). Regular consumption of antioxidant-rich berries can support the immune system by neutralizing free radicals and reducing the risk of cellular damage.
For optimal immune support, incorporating a variety of berries such as strawberries, raspberries, blackberries, and blueberries into the daily diet is recommended. A typical serving size is about one cup (approximately 150 grams) of fresh or frozen berries per day. This amount provides a substantial dose of vitamins, minerals, and phytochemicals that promote overall health. Berries can be enjoyed on their own, added to smoothies, yogurt, or oatmeal, and even incorporated into salads for a nutritious boost. Choosing organic options when possible may help reduce exposure to pesticides (source).
6. Selenium

Selenium is an essential trace mineral that plays a crucial role in maintaining both thyroid function and immune health. It is a vital component of selenoproteins, which help regulate immune responses and protect cells from oxidative damage. Adequate selenium intake is particularly important for individuals with autoimmune thyroid diseases, such as Hashimoto’s thyroiditis and Graves’ disease, as it supports thyroid hormone synthesis and may help modulate inflammation (source).
Brazil nuts are recognized as one of the richest natural sources of selenium; just one or two nuts can provide the recommended daily allowance for most adults. Other dietary sources include seafood, poultry, eggs, and whole grains. While selenium is essential, it is important to exercise caution with supplementation, as excessive intake can lead to toxicity and adverse health effects such as gastrointestinal disturbances, hair loss, and nerve damage. The upper intake level for adults is 400 micrograms per day (source). To avoid over-supplementation, it is generally advised to meet selenium needs through food sources and consult a healthcare professional before considering supplements.
7. Zinc
Zinc is a vital mineral that plays a key role in the development and function of immune cells, including T lymphocytes, neutrophils, and natural killer cells. Adequate zinc levels help maintain the integrity of the immune system, supporting the body’s ability to defend against pathogens and regulate inflammatory responses. Deficiency in zinc has been linked with impaired immune function and increased susceptibility to infections, which can further complicate autoimmune conditions (source).
Oysters are the most concentrated dietary source of zinc, providing significantly more of the mineral per serving than other foods. A single medium oyster contains up to 5.5 mg of zinc, which is about half of the recommended daily allowance for adults. Other good sources include beef, poultry, beans, nuts, and whole grains. The recommended dietary allowance for zinc is 8 mg per day for adult women and 11 mg per day for adult men. It is important not to exceed the upper intake level of 40 mg per day, as excessive zinc intake can suppress immune function, interfere with copper absorption, and cause gastrointestinal symptoms (source).
8. Gluten-Free Diet

Gluten, a protein found in wheat, barley, and rye, is well-known for triggering autoimmune responses in individuals with celiac disease, leading to intestinal damage and systemic inflammation. Emerging research also suggests that gluten may exacerbate symptoms in some people with non-celiac autoimmune conditions, such as Hashimoto’s thyroiditis and rheumatoid arthritis, though the evidence is less definitive (source). For those affected, adopting a gluten-free diet can help reduce inflammation and improve symptoms.
Real-life dietary swaps to avoid gluten include replacing wheat-based bread and pasta with gluten-free alternatives made from rice, quinoa, or corn. Oats are naturally gluten-free but should be labeled as such to avoid cross-contamination. Other gluten-free options include potatoes, legumes, fruits, and vegetables. Caution is necessary, as gluten can be hidden in sauces, salad dressings, processed meats, and even some supplements. Reading ingredient labels carefully and choosing certified gluten-free products can help minimize accidental exposure (source). Consulting with a registered dietitian can provide further guidance on balanced gluten-free meal planning and help address any nutritional gaps.
9. Mediterranean Diet

The Mediterranean diet is renowned for its anti-inflammatory properties, primarily due to its emphasis on plant-based foods, healthy fats, and lean proteins. This dietary pattern includes abundant fruits, vegetables, whole grains, nuts, seeds, legumes, olive oil, moderate fish and poultry, and minimal red meat and processed foods. The combination of antioxidants, fiber, and omega-3 fatty acids helps reduce systemic inflammation, which is beneficial for individuals with autoimmune conditions. Studies have shown that adherence to the Mediterranean diet is associated with lower disease activity and improved quality of life in people with systemic lupus erythematosus (SLE) (source).
To get started with this dietary approach, begin by incorporating more fruits and vegetables into daily meals, replacing butter and margarine with extra-virgin olive oil, and choosing whole grains over refined grains. Add fish, especially oily varieties like salmon and sardines, a few times per week, and include nuts and seeds as snacks. Limit processed foods, sugary drinks, and red meat. Herbs and spices can be used for flavor instead of salt. For more detailed guidance and recipes, resources like the Oldways Mediterranean Diet can be helpful.
10. Turmeric (Curcumin)

Turmeric is a yellow spice widely used in Asian cuisine and traditional medicine, prized for its active compound curcumin. Curcumin exhibits powerful antioxidant and anti-inflammatory effects by modulating various molecular pathways that drive inflammation and oxidative stress. It inhibits pro-inflammatory cytokines and enzymes such as COX-2, making it particularly helpful for managing autoimmune conditions characterized by chronic inflammation (source).
In autoimmune diseases like rheumatoid arthritis, curcumin supplementation has been shown to reduce joint swelling, pain, and stiffness, with some studies suggesting effects comparable to nonsteroidal anti-inflammatory drugs (NSAIDs) but with fewer side effects. To enhance curcumin’s absorption, it is commonly recommended to pair turmeric with black pepper, which contains piperine—a compound that can increase curcumin’s bioavailability by up to 2,000% (source).
Turmeric can be added to curries, soups, smoothies, or taken as a supplement. For supplements, look for products that include black pepper extract (piperine) or consult a healthcare provider for personalized advice on dosing and safety, especially if you are taking medications or have gallbladder issues.
11. Leafy Greens

Leafy greens are nutritional powerhouses packed with vitamins, minerals, antioxidants, and fiber that support immune health and help manage inflammation. They are excellent sources of vitamins A, C, K, folate, magnesium, and phytonutrients that protect against cellular damage and promote optimal immune function. Spinach and kale are two of the most popular leafy greens, each offering a unique nutrient profile. Spinach is particularly high in folate and iron, supporting red blood cell production and DNA synthesis, while kale offers more vitamin C, vitamin K, and calcium per serving, which are vital for immune response and bone health (source).
Adding leafy greens to your diet is simple and versatile. Incorporate fresh spinach or kale into salads, blend them into smoothies, or sauté them with garlic as a nutrient-rich side dish. Add chopped greens to soups, stews, omelets, or pasta dishes for extra flavor and nutrition. For convenience, frozen greens can be used in cooked dishes without sacrificing nutritional value. Aim to include at least one to two cups of leafy greens daily to maximize their health benefits and support immune function (source).
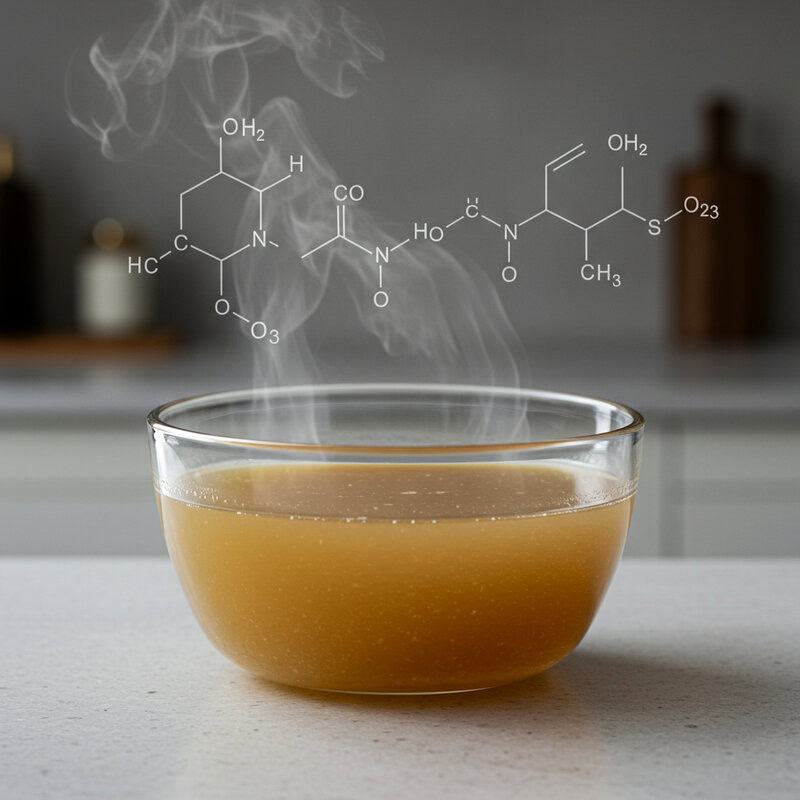
12. Bone Broth

Bone broth is a nutrient-dense liquid made by simmering animal bones and connective tissue, resulting in a rich source of minerals, amino acids, and collagen. Its gut-soothing properties are especially valuable for individuals with autoimmune conditions, as a healthy gut lining is vital for balanced immune function. Collagen and the amino acids glycine and glutamine found in bone broth have been shown to support the integrity of the gut barrier, reduce inflammation, and promote healing of the intestinal tract (source).
Homemade bone broth allows for complete control over ingredients, avoiding additives and excessive sodium commonly found in some store-bought versions. Simmering beef, chicken, or fish bones with vegetables and herbs for 12-24 hours extracts the maximum nutrients. Store-bought bone broths can be a convenient alternative, but it’s important to choose brands that are labeled as “organic,” “grass-fed,” or “free-range” and to check for minimal ingredients and sodium content. Bone broth can be consumed on its own, used as a base for soups and stews, or added to grains for extra flavor and nutrition (source).
13. Garlic

Garlic has a long history as a medicinal food, valued for its immune-modulating and anti-inflammatory properties. Its active compound, allicin, has been shown to enhance the activity of immune cells such as macrophages and natural killer cells, supporting the body’s defense against infections and potentially modulating autoimmune activity (source). Research indicates that regular garlic consumption may reduce the severity and frequency of common infections, including colds and flu, by stimulating the immune response.
For best results, garlic should be prepared properly to maximize its health benefits. Crushing or chopping fresh garlic cloves activates the enzyme alliinase, which converts alliin to allicin—the key bioactive compound. Allowing crushed or chopped garlic to sit for 5-10 minutes before cooking or eating helps enhance its beneficial properties. Raw garlic offers the most potent effects, but it can also be added toward the end of cooking to preserve its active compounds. Incorporate garlic into salad dressings, dips, stir-fries, and roasted vegetables for both flavor and immune support. Those sensitive to raw garlic may start with small amounts and gradually increase intake (source).
14. Green Tea

Green tea is celebrated for its high content of polyphenols, particularly epigallocatechin gallate (EGCG), which exhibit powerful antioxidant and anti-inflammatory effects. These polyphenols help modulate immune function by reducing the production of pro-inflammatory cytokines and protecting cells from oxidative stress. Research suggests that green tea’s bioactive compounds may support immune balance and offer protective effects against autoimmune inflammation (source).
Compared to black tea, green tea is less oxidized during processing, preserving a higher concentration of beneficial polyphenols. While both teas provide antioxidants, green tea generally contains more EGCG, which is thought to be particularly effective in immune modulation and inflammation reduction. Green tea also contains less caffeine than black tea, making it suitable for multiple daily servings without excessive stimulation.
To reap the immune-supportive benefits, it is recommended to consume 2-3 cups of green tea daily. Steeping the tea in hot (not boiling) water for 2-3 minutes helps preserve its delicate polyphenols. Green tea can be enjoyed plain or with a squeeze of lemon, and should be consumed without excessive sugar to maximize health benefits (source).
15. Flaxseeds

Flaxseeds are an excellent plant-based source of alpha-linolenic acid (ALA), a type of omega-3 fatty acid known for its anti-inflammatory properties. Consuming omega-3s can help modulate immune responses and may be beneficial for individuals with autoimmune conditions by reducing the production of inflammatory molecules. In addition to their omega-3 content, flaxseeds are rich in dietary fiber and lignans, which further support gut health and immune function (source).
When compared to chia seeds, flaxseeds provide similar amounts of ALA and fiber, but flaxseeds are particularly noted for their high lignan content, which offers additional antioxidant benefits. Both seeds can be valuable additions to an anti-inflammatory diet, but flaxseeds may offer a slight advantage for those seeking to boost their intake of lignans.
To maximize absorption of nutrients, flaxseeds should be consumed ground rather than whole, as whole seeds often pass through the digestive tract undigested. Add ground flaxseeds to smoothies, oatmeal, yogurt, or baked goods for a nutritional boost. Store ground flaxseeds in the refrigerator to prevent oxidation and preserve their beneficial oils (source).
16. Water Intake

Proper hydration is essential for maintaining cellular function, supporting detoxification, and regulating inflammation—all of which are crucial for individuals with autoimmune conditions. Water helps transport nutrients, flush out toxins, and ensures that immune cells operate efficiently throughout the body. When hydration is inadequate, inflammation can worsen, and normal physiological processes may be disrupted, increasing the risk of symptom flare-ups and delayed recovery (source).
Symptoms of dehydration can include fatigue, headaches, dry mouth, dizziness, poor concentration, and even joint pain or muscle cramps. Chronic low-level dehydration may also contribute to increased inflammation and impaired immune response. Therefore, maintaining optimal hydration is a simple yet effective strategy for supporting overall health and immune function.
General guidelines recommend aiming for about 8 cups (64 ounces) of water per day for most adults, but individual needs may vary based on activity level, climate, and health status. Those with autoimmune conditions may need to adjust their intake during periods of illness, fever, or increased physical activity. Carrying a reusable water bottle and setting regular reminders can help ensure adequate daily water consumption (source).
17. Whole Grains

Whole grains are an important source of dietary fiber, vitamins, minerals, and antioxidants that support digestive and immune health. Unlike refined grains, whole grains retain their bran and germ, providing higher levels of nutrients such as B vitamins, magnesium, iron, selenium, and phytonutrients. Fiber in whole grains promotes healthy gut bacteria, which can help modulate immune responses and reduce inflammation—key factors in managing autoimmune conditions (source).
Quinoa, a naturally gluten-free whole grain, is a nutritional standout compared to white rice. It contains more protein, fiber, and micronutrients such as magnesium and iron, making it a superior option for supporting energy, muscle function, and immune health. Additionally, quinoa is a complete protein, providing all nine essential amino acids, which is rare among plant foods.
For those needing gluten-free options, there are several whole grains to consider, including brown rice, millet, buckwheat, amaranth, and certified gluten-free oats. Incorporating a variety of these grains into meals helps ensure a balanced intake of nutrients and supports digestive health. Swap refined grains for whole grains in salads, stir-fries, and breakfast bowls for optimal benefits (source).
18. Monounsaturated Fats

Monounsaturated fats are heart-healthy fats that have demonstrated anti-inflammatory effects, making them valuable in the dietary management of autoimmune conditions. These fats can help reduce levels of inflammatory markers in the body and support healthy cholesterol levels. Olive oil is a prime example, rich in oleic acid and polyphenols, which work together to suppress inflammation and oxidative stress (source). Studies have shown that regular consumption of extra-virgin olive oil is associated with a lower risk of developing chronic inflammatory diseases and improved immune function.
To incorporate more monounsaturated fats into your diet, swap saturated fats such as butter, margarine, and lard for healthier alternatives like olive oil, avocado oil, and canola oil. Use extra-virgin olive oil for salad dressings, drizzling over vegetables, or low to medium-heat cooking. Avocados, nuts (such as almonds and cashews), and seeds are also excellent sources of monounsaturated fats. For high-heat cooking, avocado oil is a suitable option due to its higher smoke point. Making these simple swaps can support a more anti-inflammatory dietary pattern and benefit those managing autoimmune symptoms (source).
19. Vitamin B12

Vitamin B12 is a water-soluble vitamin essential for nerve health, red blood cell formation, and DNA synthesis. Its importance is especially pronounced in autoimmune conditions such as pernicious anemia, where the immune system attacks cells in the stomach that produce intrinsic factor, a protein required for B12 absorption. Without sufficient B12, individuals can experience neurological symptoms, fatigue, and cognitive disturbances (source).
Dietary sources of vitamin B12 are primarily animal-based and include beef, poultry, fish, eggs, and dairy products. For individuals following a plant-based diet or those with absorption issues, fortified plant milks, breakfast cereals, and nutritional yeast provide alternative sources. In cases of deficiency or malabsorption—such as with pernicious anemia—oral B12 supplements or intramuscular injections may be necessary to restore adequate levels. The recommended dietary allowance for adults is approximately 2.4 micrograms per day, though those with diagnosed deficiency may require higher doses under medical supervision (source).
Monitoring B12 status through regular blood tests is important for individuals at risk, and consulting with a healthcare professional can guide appropriate dietary or supplemental strategies to maintain nerve health and overall wellbeing.
20. Low Glycemic Index Foods

Choosing foods with a low glycemic index (GI) plays a significant role in maintaining stable blood sugar levels and reducing systemic inflammation—both important considerations for managing autoimmune conditions. High-GI foods cause rapid spikes and crashes in blood glucose, which can trigger inflammatory responses and worsen autoimmune symptoms. In contrast, low-GI foods release glucose more gradually, supporting sustained energy and minimizing inflammatory cascades (source).
For example, lentils have a much lower GI compared to white bread. Lentils provide complex carbohydrates, fiber, and protein, resulting in slower digestion and absorption, while white bread leads to a rapid increase in blood sugar and insulin levels. Regular consumption of low-GI foods like lentils, beans, quinoa, sweet potatoes, and non-starchy vegetables can support blood sugar stability and help reduce inflammation.
Simple low-GI swaps include replacing white bread with whole grain bread, choosing brown rice over white rice, and opting for steel-cut oats instead of instant oatmeal. Incorporating more legumes, nuts, seeds, and a variety of colorful vegetables into meals can further promote a low-GI dietary pattern and support immune health (source).
21. Cruciferous Vegetables

Cruciferous vegetables—such as broccoli, cauliflower, and cabbage—are packed with nutrients and phytochemicals that offer robust immune support and anti-inflammatory benefits. These vegetables are rich in vitamins C, K, and folate, and contain unique sulfur-containing compounds called glucosinolates. When consumed, glucosinolates are converted into biologically active compounds like sulforaphane, which has been shown to modulate immune cell activity and protect against oxidative stress (source).
Broccoli, in particular, stands out for its high content of vitamin C and sulforaphane, which can help reduce inflammation and support detoxification pathways. Cauliflower and cabbage also contribute fiber and additional antioxidants, making them excellent choices for individuals with autoimmune conditions seeking to optimize immune defenses.
To maximize nutrient retention, it’s best to lightly steam or sauté cruciferous vegetables rather than boiling them, as extended heat and water exposure can lead to significant nutrient loss. Chopping or shredding these vegetables and allowing them to sit for a few minutes before cooking can also enhance the formation of beneficial compounds. Incorporate cruciferous veggies into salads, stir-fries, soups, or as crunchy snacks for a daily immune boost (source).
22. Magnesium

Magnesium is an essential mineral involved in more than 300 biochemical reactions in the body, including the regulation of nerve and muscle activity, immune system balance, and inflammation control. Its calming effect on nerves and muscles can help reduce symptoms such as muscle cramps, spasms, and irritability, which are sometimes experienced by individuals with autoimmune and inflammatory disorders. Magnesium has also been shown to support stress resilience and promote healthy sleep patterns, further benefiting immune health (source).
Nuts and seeds are excellent dietary sources of magnesium. For example, pumpkin seeds, almonds, cashews, and sunflower seeds all offer significant amounts of this vital mineral. Other magnesium-rich foods include leafy greens, whole grains, legumes, and dark chocolate. The recommended daily intake for magnesium is about 310-320 mg for adult women and 400-420 mg for adult men. Consuming a variety of magnesium-rich foods can help meet daily needs and support overall health.
If dietary intake is insufficient, magnesium supplements are available, but excessive supplementation can cause digestive upset or interact with certain medications. It’s best to consult with a healthcare provider before starting any new supplement (source).
23. Elimination Diets
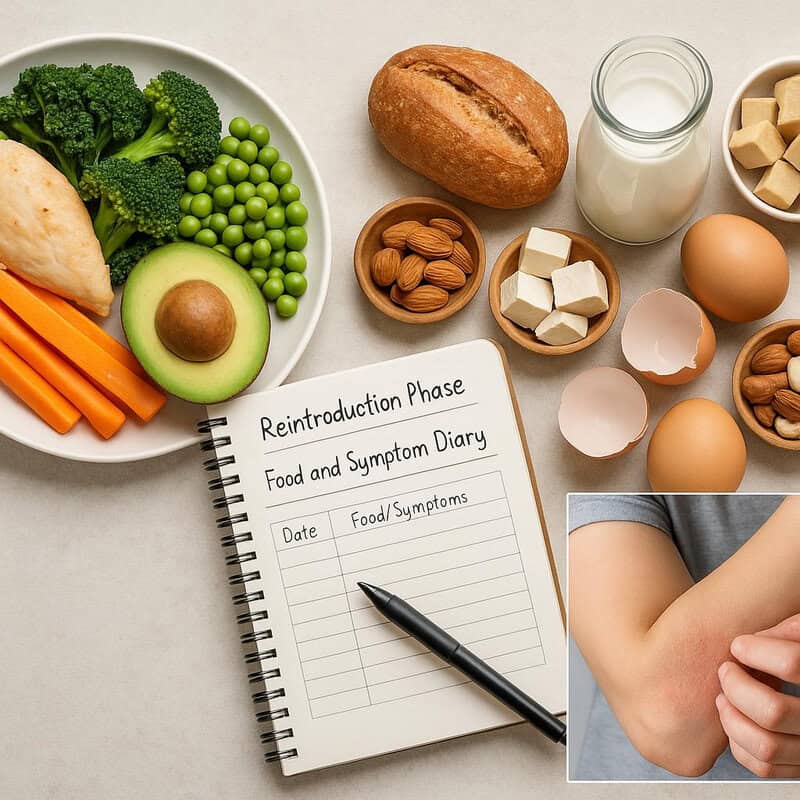
Elimination diets are structured eating plans designed to help individuals identify foods that may trigger or worsen autoimmune symptoms. By systematically removing and then reintroducing specific foods, these diets can reveal sensitivities or intolerances that contribute to inflammation and immune system overactivity. For example, in individuals with eczema—a condition often linked to immune dysfunction—elimination diets have been used to pinpoint triggers such as dairy, eggs, or soy, resulting in improved skin symptoms and reduced flare-ups (source).
A safe elimination diet protocol typically starts with the removal of common allergens and inflammatory foods, such as gluten, dairy, soy, eggs, nuts, and processed foods, for a period of two to six weeks. During this phase, individuals focus on eating whole, minimally processed foods. After the elimination phase, foods are reintroduced one at a time, usually every three to five days, while monitoring for adverse symptoms. It’s important to keep a detailed food and symptom diary throughout the process. Elimination diets should be conducted under the guidance of a healthcare professional or registered dietitian to ensure balanced nutrition and prevent deficiencies (source).
24. Plant-Based Proteins
Plant-based proteins offer several advantages over red meats, particularly for individuals managing autoimmune conditions. Diets high in red and processed meats have been associated with increased inflammation and a higher risk of chronic disease, while plant-based protein sources provide essential amino acids along with beneficial fiber, antioxidants, and phytonutrients. These components help reduce inflammation and support a balanced gut microbiome, both crucial for immune regulation (source).
Lentils exemplify the power of plant-based proteins. Compared to beef, lentils are lower in saturated fat and calories but high in protein, iron, magnesium, and folate. While beef is a complete protein, lentils can be combined with whole grains, such as brown rice or quinoa, to provide all essential amino acids. Additionally, lentils supply dietary fiber—which beef lacks—supporting digestive health and stable blood sugar.
For meal planning, include a variety of plant proteins such as beans, chickpeas, lentils, tofu, tempeh, quinoa, and edamame. Experiment with hearty salads, stews, curries, and stir-fries. Gradually replacing some or all red meat with plant-based proteins can be a sustainable and nutritious strategy for supporting both immune and overall health (source).
25. Quercetin
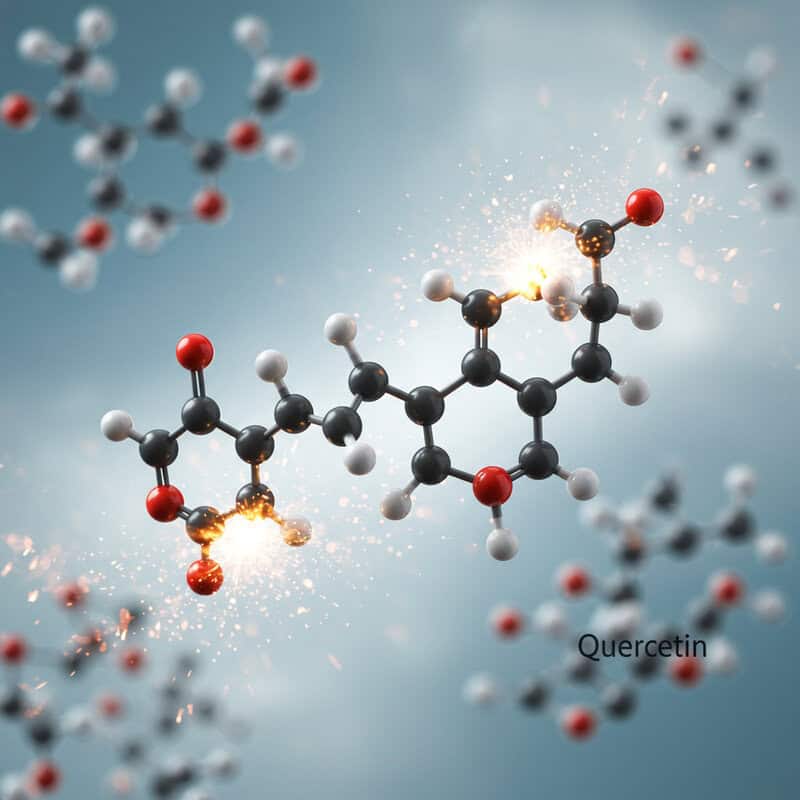
Quercetin is a powerful flavonoid with notable antioxidant and anti-inflammatory effects, making it a valuable nutrient for those with autoimmune conditions. Quercetin works by scavenging free radicals, reducing oxidative stress, and inhibiting the production of pro-inflammatory cytokines, which can help modulate immune responses and decrease inflammation within the body (source). Its ability to stabilize mast cells and reduce histamine release further supports its use in managing allergic and inflammatory symptoms.
Natural food sources rich in quercetin include apples, onions (especially red and yellow varieties), berries, capers, kale, and broccoli. Regularly incorporating these foods into your diet can help support antioxidant defenses and promote immune balance. For example, adding sliced apples and onions to salads, or including kale and broccoli in stir-fries, can boost daily quercetin intake.
While there is no official recommended daily allowance for quercetin, studies suggest that a daily intake of 500 mg from food and supplements combined may confer health benefits. Most people can reach beneficial levels through a varied diet rich in fruits and vegetables. For higher supplemental doses, consult with a healthcare provider (source).
26. Vitamin C

Vitamin C is a crucial nutrient that boosts immune cell activity, enhances the production and function of white blood cells, and acts as a potent antioxidant to protect against cellular damage. It also supports the skin’s barrier function and promotes the repair of tissues, making it an important nutrient for individuals managing autoimmune and inflammatory conditions. Vitamin C can help shorten the duration of infections and support overall immune resilience (source).
Citrus fruits—such as oranges, grapefruits, lemons, and limes—are well-known sources of vitamin C. Other excellent food sources include kiwi, strawberries, bell peppers, and broccoli. Consuming vitamin C from whole foods not only provides this vital nutrient but also delivers additional phytochemicals and fiber that work synergistically to support health. While supplements are widely available, evidence suggests that the body absorbs and utilizes vitamin C from foods more effectively than from synthetic supplements (source).
The recommended dietary allowance for adults ranges from 75 mg (women) to 90 mg (men) per day. Higher doses may be used short-term, but excessive intake (over 2,000 mg daily) can cause digestive upset. It’s best to prioritize fruits and vegetables for daily vitamin C needs.
27. Iron

Iron is an essential mineral critical for the production of hemoglobin, which allows red blood cells to transport oxygen throughout the body. Anemia is a common complication in several autoimmune conditions, such as lupus and rheumatoid arthritis, due to chronic inflammation or blood loss. Adequate iron status is vital for maintaining energy, cognitive function, and a robust immune response (source).
Iron is available in two forms: heme and non-heme. Heme iron, found in animal products like red meat, poultry, and fish, is more readily absorbed by the body. Non-heme iron, present in plant foods such as lentils, beans, spinach, and fortified cereals, is absorbed less efficiently but can be enhanced with vitamin C-rich foods. For example, adding bell peppers or citrus fruits to meals with beans can improve non-heme iron absorption.
Signs of iron deficiency include fatigue, weakness, shortness of breath, pale skin, and difficulty concentrating. Individuals with autoimmune diseases are at increased risk and should monitor their iron status regularly. Supplementation may be necessary in cases of diagnosed deficiency, but it should be managed with medical supervision to avoid excess iron (source).
28. Low Histamine Diet

Histamine intolerance occurs when the body cannot effectively break down histamine, a compound involved in immune responses and inflammation. This intolerance can lead to symptoms such as headaches, hives, digestive issues, and flushing, and it may overlap with or exacerbate autoimmune conditions by increasing inflammatory responses. Some individuals with autoimmune diseases find that reducing dietary histamine helps alleviate flares or unexplained symptoms (source).
High-histamine foods include aged cheeses, smoked meats, fermented foods (such as sauerkraut and kimchi), alcohol, vinegar, and certain fish like tuna and mackerel. In contrast, low-histamine foods include fresh meats and fish, eggs, non-citrus fruits (such as apples and pears), rice, and most fresh vegetables. Since histamine levels in foods can increase with storage and fermentation, eating freshly prepared meals is often recommended.
Tracking symptoms in a food diary can be helpful in identifying potential triggers and monitoring the effects of dietary changes. Individuals considering a low histamine diet should work with a healthcare professional or registered dietitian to ensure nutritional adequacy and to interpret symptoms accurately (source).
29. Soy Products

Soy products, such as tofu, tempeh, and edamame, are well-known for their high-quality plant protein and unique content of isoflavones—plant compounds that have mild estrogen-like effects in the body. These isoflavones can interact with estrogen receptors and may influence hormone-related autoimmune diseases, such as Hashimoto’s thyroiditis and certain forms of lupus. Research is mixed: some studies suggest that moderate soy intake does not adversely affect thyroid function in healthy individuals or those with adequately treated thyroid disease, while others recommend caution in those with active thyroid dysfunction (source).
Compared to animal protein, tofu and other soy foods provide a complete protein source but with less saturated fat and cholesterol, supporting heart and immune health. Soy also contains fiber and antioxidants, which contribute to its anti-inflammatory profile. However, highly processed soy products and soy supplements may not offer the same benefits as whole or minimally processed options.
For most individuals, enjoying moderate amounts of whole soy foods—such as 1-2 servings per day—is considered safe and may support a balanced diet. Those with hormone-sensitive autoimmune conditions should consult their healthcare provider for personalized recommendations on soy intake (source).
30. Polyphenols

Polyphenols are a diverse group of plant compounds known for their potent antioxidant and immune-modulating properties. They help reduce inflammation, scavenge free radicals, and regulate immune cell activity, making them highly beneficial for individuals with autoimmune conditions. Polyphenols like flavonoids, phenolic acids, and lignans have been shown to suppress pro-inflammatory signaling pathways and support a balanced immune response (source).
Berries—such as blueberries, raspberries, and strawberries—are among the richest sources of polyphenols. Dark chocolate (with a cocoa content of at least 70%) is also notable for its high levels of flavonoids, which contribute to its anti-inflammatory effects. Other sources include grapes, cherries, plums, black and green tea, and a variety of colorful fruits and vegetables.
Practical serving ideas for increasing polyphenol intake include adding a handful of mixed berries to breakfast oatmeal or yogurt, enjoying a few squares of dark chocolate as an afternoon snack, or sipping a cup of green or black tea. Incorporating a rainbow of plant-based foods into each meal helps ensure a diverse intake of polyphenols, supporting immune health and overall wellbeing (source).
31. Nightshade Vegetables

Nightshade vegetables, which include tomatoes, eggplants, bell peppers, and potatoes, are a topic of debate in autoimmune nutrition. These vegetables contain compounds such as alkaloids and lectins, which some believe may trigger inflammation or exacerbate symptoms in sensitive individuals with autoimmune conditions, particularly in those with rheumatoid arthritis or inflammatory bowel diseases. However, scientific evidence supporting a universal need to avoid nightshades is limited, and most people tolerate them well (source).
Nightshades are rich in vitamins, minerals, antioxidants, and fiber, contributing to overall health and immune support. Tomatoes, for example, are an excellent source of vitamin C, potassium, and lycopene, a powerful antioxidant. For many, including nightshades as part of a balanced diet can offer nutritional benefits without adverse effects.
Because reactions to nightshades are highly individualized, personalized monitoring is recommended. If you suspect nightshade sensitivity, consider keeping a food and symptom diary or conducting a trial elimination under the guidance of a healthcare provider or dietitian. After a few weeks, reintroduce nightshades one at a time and observe for any symptoms. This approach helps determine individual tolerance while maintaining dietary variety (source).
32. Alcohol Moderation

Alcohol consumption can significantly affect immune function, with both short-term and long-term consequences for individuals managing autoimmune conditions. Alcohol impairs the activity of immune cells, increases inflammation, and disrupts the gut barrier, which can exacerbate autoimmune symptoms and increase susceptibility to infections (source). Excessive or chronic alcohol intake is particularly harmful, as it can lead to immune suppression, liver damage, nutrient deficiencies, and worsened disease outcomes.
In contrast, moderate alcohol consumption—generally defined as up to one standard drink per day for women and up to two for men—may have less pronounced effects on immune health. Some studies suggest that moderate intake of certain alcoholic beverages, such as red wine, may confer antioxidant benefits due to polyphenols, though these potential benefits do not outweigh the risks for many people with autoimmune diseases (source).
For those with autoimmune conditions, it is wise to limit or avoid alcohol to reduce the risk of flares and complications. If choosing to drink, stay within recommended safe limits, drink water alongside alcohol, and avoid drinking on an empty stomach. Always consult your healthcare provider regarding alcohol use and medication interactions.
33. Dairy Alternatives

Dairy products can trigger inflammation and digestive discomfort in some individuals with autoimmune conditions, particularly those with lactose intolerance or sensitivity to milk proteins such as casein and whey. In certain autoimmune diseases, such as rheumatoid arthritis or multiple sclerosis, some people report symptom improvement after reducing or eliminating dairy from their diets (source). However, the evidence is mixed, and tolerance can be highly individual.
Plant-based milk alternatives—such as almond, soy, oat, coconut, and rice milk—offer options for those avoiding dairy. Among these, soy milk is closest to cow’s milk in protein content, while almond and oat milks are typically lower in protein but can be fortified with calcium and vitamin D. It’s important to choose unsweetened and fortified varieties to avoid excess added sugars and to ensure adequate nutrient intake.
Alternative sources of calcium for those who avoid dairy include leafy greens (like kale and bok choy), fortified plant milks and juices, tofu made with calcium sulfate, canned fish with bones (such as sardines), and almonds. Reading labels and varying food choices can help support bone health and overall nutrition while minimizing potential inflammatory triggers (source).
34. Intermittent Fasting

Intermittent fasting (IF) involves alternating periods of eating and fasting, and emerging research suggests it may help regulate immune responses and reduce inflammation, factors that are particularly important in autoimmune conditions. Animal studies have shown that IF can promote the regeneration of immune cells, decrease the production of pro-inflammatory cytokines, and improve outcomes in models of autoimmune diseases such as multiple sclerosis and rheumatoid arthritis (source). IF may also support gut health by giving the digestive system time to rest and repair.
Common IF methods include the 16:8 approach (16 hours fasting, 8 hours eating window) or alternate-day fasting. While some people report improvements in energy, inflammation, and symptom severity, intermittent fasting is not suitable for everyone. Individuals with certain medical conditions, those taking medications, or those at risk for nutrient deficiencies should exercise caution.
Practical safety tips include starting with shorter fasting periods, staying well hydrated, listening to your body’s signals, and ensuring nutrient-dense meals during eating windows. It’s wise to consult with a healthcare provider or registered dietitian before beginning intermittent fasting, especially if you have an autoimmune disease or other chronic health conditions (source).
35. Herbal Teas

Herbal teas such as ginger and chamomile have a long history of use for their immune-supporting and anti-inflammatory properties, making them beneficial additions to an autoimmune-friendly diet. Ginger tea is well-known for its ability to reduce inflammation and oxidative stress. Its active compounds, including gingerol and shogaol, have been shown to suppress pro-inflammatory cytokines and may help alleviate symptoms associated with autoimmune conditions (source).
Chamomile tea, on the other hand, is prized for its calming effects on the nervous system and its potential to modulate immune function. Apigenin, a compound in chamomile, has mild anti-inflammatory and antioxidant activities that may help reduce anxiety, promote restful sleep, and soothe digestive discomfort, all of which are relevant for those with autoimmune disorders (source).
To integrate herbal teas into your daily routine, enjoy a cup of ginger tea in the morning to support digestion and immune health, and sip chamomile tea in the evening to promote relaxation and sleep. Herbal teas can be consumed alone or blended with other calming or anti-inflammatory herbs for added benefit. Always check for allergies or interactions with medications.
36. Fiber

Dietary fiber plays a pivotal role in supporting gut health and modulating inflammation, both of which are crucial in managing autoimmune conditions. Fiber helps nourish beneficial gut bacteria, leading to the production of short-chain fatty acids like butyrate, which have anti-inflammatory effects and help maintain the integrity of the gut barrier (source). A healthy gut environment is linked to improved immune regulation and reduced risk of autoimmune flare-ups.
There are two main types of fiber: soluble and insoluble. Soluble fiber dissolves in water to form a gel-like substance, slowing digestion and helping regulate blood sugar. It is found in foods like oats, beans, lentils, apples, and citrus fruits. Insoluble fiber adds bulk to stool and promotes regular bowel movements, supporting digestive health. It is abundant in whole grains, nuts, seeds, and the skins of fruits and vegetables. Both types are important for overall gut health and immune function.
To boost fiber intake, gradually add more fruits, vegetables, legumes, nuts, seeds, and whole grains to your meals. Aim for at least 25-30 grams of fiber per day for adults. Increase fiber slowly and drink plenty of water to minimize digestive discomfort (source).
37. Personalized Nutrition Plans
Developing a personalized nutrition plan is essential for effectively managing autoimmune conditions, as dietary triggers, nutrient needs, and individual tolerances can vary widely. Tailored diets consider a person’s medical history, specific autoimmune diagnosis, symptoms, allergies, and lifestyle factors. Personalized plans not only help reduce inflammation and manage symptoms but also support long-term health and nutritional adequacy (source).
Working with a registered dietitian (RD) or nutritionist is a highly effective way to create a plan that meets individual needs. An RD can help identify trigger foods through elimination diets, address nutrient deficiencies, and design meal plans that accommodate preferences and cultural traditions. For example, a dietitian may assist someone with lupus in managing photosensitivity with antioxidant-rich foods or help a person with celiac disease navigate gluten-free nutrition safely.
Next steps for assessment include keeping a detailed food and symptom diary, obtaining relevant laboratory tests (such as vitamin D, iron, or B12 levels), and scheduling a consultation with a qualified nutrition professional. This collaborative approach ensures ongoing support, timely adjustments, and the best possible outcomes for autoimmune management (source).
38. Low Sodium Intake

Limiting sodium intake is important for individuals with autoimmune conditions, as excess sodium has been linked to increased inflammation and can worsen symptoms in some diseases. High sodium levels can stimulate the production of pro-inflammatory immune cells, potentially aggravating autoimmune responses. Additionally, excessive sodium contributes to elevated blood pressure and increases the risk of cardiovascular complications, which are more common in those with chronic inflammation (source).
Processed and packaged foods are the primary sources of dietary sodium, often containing significantly higher levels than their fresh counterparts. Examples include canned soups, deli meats, frozen meals, snack foods, and restaurant fare. In contrast, fresh fruits, vegetables, whole grains, and unprocessed meats typically have much lower sodium content and offer greater nutritional value.
To reduce sodium intake, opt for fresh or minimally processed foods, cook meals at home, and flavor dishes with herbs, spices, citrus, or vinegar instead of salt. Reading nutrition labels and choosing products labeled “low sodium” or “no added salt” can also help. The American Heart Association recommends consuming less than 2,300 mg of sodium per day, aiming for an ideal limit of 1,500 mg (source).
39. Mushrooms

Mushrooms are rich in bioactive compounds, including beta-glucans, polysaccharides, and antioxidants, which have been shown to modulate immune function and support the body’s defense mechanisms. Beta-glucans, in particular, stimulate the activity of macrophages, natural killer cells, and other immune cells, enhancing immune surveillance and helping to regulate inflammatory responses (source).
Shiitake and maitake mushrooms are especially notable for their immune-supporting properties. Shiitake mushrooms contain lentinan, a polysaccharide studied for its ability to boost immune cell production and protect against infections. Maitake mushrooms provide D-fraction, another potent beta-glucan with demonstrated immunomodulatory and anti-inflammatory effects. Both varieties are also good sources of B vitamins, copper, and selenium, all of which are important for immune health.
To incorporate mushrooms into your diet, add sliced shiitake or maitake mushrooms to stir-fries, soups, stews, or grain bowls. Roasting mushrooms with olive oil and herbs, or sautéing them with garlic and greens, can enhance their flavor and nutritional value. Using mushrooms as a meat substitute in burgers or tacos is another creative way to enjoy their benefits (source).
40. Cooking Methods

The way foods are cooked can significantly influence both their nutrient content and their impact on inflammation, which is especially important for individuals with autoimmune conditions. Grilling, steaming, and frying each affect nutrients differently. Grilling, while flavorful, can produce harmful compounds called advanced glycation end products (AGEs) and polycyclic aromatic hydrocarbons (PAHs), which are linked to increased inflammation and oxidative stress (source). Frying, particularly deep-frying, often adds unhealthy fats and further generates inflammatory compounds while reducing vitamins sensitive to heat.
In contrast, steaming is one of the best methods for preserving vitamins and minerals—especially water-soluble nutrients like vitamin C and B vitamins—without producing harmful byproducts. Sautéing with a small amount of healthy fat (like olive oil) at moderate temperatures can also help retain nutrients and add flavor.
For nutrient-preserving and anti-inflammatory cooking, prioritize steaming, roasting, and gentle sautéing. Avoid charring foods and limit frying, especially in unhealthy oils. Use herbs, spices, and citrus to enhance flavor without excessive heat. Cutting vegetables just before cooking and using minimal water also helps retain nutrients. These methods support both nutritional quality and immune health (source).
41. Meal Timing
Meal timing and frequency play an emerging role in immune balance and the management of autoimmune conditions. Research suggests that when you eat can affect circadian rhythms, hormone regulation, and inflammatory processes. Time-restricted eating (TRE), a form of intermittent fasting where all meals are consumed within a limited daily window (such as 8-10 hours), has shown promise in supporting immune function and reducing inflammation. Animal and human studies indicate TRE can lower markers of oxidative stress, improve metabolic health, and positively influence gut microbiota—all factors relevant to autoimmune health (source).
Practical scheduling might include eating breakfast later (e.g., at 9 a.m.) and finishing dinner earlier (e.g., by 7 p.m.), which aligns food intake with natural circadian rhythms. Fewer, larger meals may help some people control appetite and energy levels, while others may benefit from smaller, more frequent meals to prevent fatigue and blood sugar dips. The optimal schedule is highly individualized and should be based on symptom patterns, medications, and lifestyle needs.
Start by tracking your energy, digestion, and symptom patterns with different meal timings. Gradually adjust your schedule and consult with a healthcare professional to find a routine that best supports your immune balance and overall wellbeing (source).
42. Food Additives

Food additives and preservatives are commonly found in processed foods and can have potential inflammatory effects, particularly for individuals with autoimmune conditions. Certain additives, including artificial colors, flavors, emulsifiers, and preservatives such as sodium benzoate and monosodium glutamate (MSG), have been linked to increased gut permeability, altered gut microbiota, and heightened immune responses (source). These changes may exacerbate inflammation and autoimmune symptoms, especially in those who are sensitive to these compounds.
Processed snacks, convenience meals, and packaged baked goods often contain a variety of food additives, in contrast to whole foods such as fruits, vegetables, legumes, nuts, and fresh meats, which are naturally free from these substances. Whole foods are generally more nutrient-dense and less likely to provoke inflammatory reactions, making them a better choice for supporting immune health and reducing symptom flares.
To minimize additive intake, become a diligent label reader. Look for products with short ingredient lists and avoid those with unfamiliar or unpronounceable additives. Opt for “additive-free,” “preservative-free,” or “organic” labels when possible. Preparing meals at home using whole, minimally processed ingredients is one of the most effective strategies for reducing exposure to potentially inflammatory food additives (source).
43. Sulforaphane

Sulforaphane is a potent phytochemical found in cruciferous vegetables, especially broccoli sprouts, and is widely recognized for its immune-modulating and anti-inflammatory properties. This compound activates the body’s antioxidant defense system, promotes detoxification, and helps regulate immune cell activity. Research indicates that sulforaphane can reduce the production of pro-inflammatory cytokines and protect against oxidative stress, making it particularly beneficial for those with autoimmune conditions (source).
While mature broccoli is a good source of sulforaphane, broccoli sprouts contain concentrations up to 100 times higher, making them one of the most effective foods for obtaining this nutrient. Consuming even a small amount of broccoli sprouts can provide significant immune benefits compared to larger servings of mature broccoli.
For optimal sulforaphane availability, broccoli sprouts are best eaten raw or only lightly steamed, as excessive heat can destroy the enzyme myrosinase necessary for sulforaphane formation. Adding fresh broccoli sprouts to salads, sandwiches, or smoothies is an easy way to incorporate them into the diet. If using mature broccoli, chopping it and letting it sit before cooking can help boost sulforaphane content (source).
44. Mindful Eating

Mindful eating is a practice that involves paying full attention to the experience of eating and drinking, which can reduce stress and, in turn, lower inflammation—an important consideration for people with autoimmune conditions. Stress is known to exacerbate immune dysregulation and trigger inflammatory responses, making stress reduction strategies, including mindful eating, beneficial for symptom management (source).
Practical mindful eating exercises include eating slowly, chewing thoroughly, and focusing on the flavors, textures, and aromas of each bite. Try putting down utensils between bites, taking deep breaths before and during meals, and eliminating distractions such as screens or multitasking. Notice feelings of hunger and fullness to help regulate portion sizes and prevent overeating, which can also reduce digestive discomfort and inflammation.
If you find it challenging to eat mindfully or notice persistent emotional eating, anxiety, or stress-related flares, consider seeking support from a registered dietitian, therapist, or a mindfulness coach. Professional guidance can help tailor mindfulness strategies to your needs and address underlying issues contributing to disordered eating patterns or stress, ultimately supporting both immune health and well-being (source).
45. Avoiding Ultra-Processed Foods

Ultra-processed foods, characterized by high levels of additives, preservatives, sugars, unhealthy fats, and low nutrient density, have been linked to immune dysregulation and increased inflammation. Regular consumption of these foods can disrupt gut microbiota, promote metabolic disturbances, and exacerbate symptoms in individuals with autoimmune diseases (source). In contrast, home-cooked meals made from whole or minimally processed ingredients provide more vitamins, minerals, fiber, and antioxidants, all of which support balanced immune function and overall health.
Preparing meals at home allows greater control over ingredients, portion sizes, and cooking methods, reducing exposure to inflammatory compounds often present in ultra-processed foods. Studies show that people who eat home-cooked meals regularly tend to have healthier dietary patterns and lower risks of chronic disease.
Effective shopping strategies include sticking to the perimeter of the grocery store, where fresh produce, meats, and dairy are typically found, and minimizing purchases from the center aisles, which often stock processed snacks and packaged foods. Reading ingredient lists and choosing products with short, recognizable ingredients can also help. Planning meals in advance and preparing larger batches for leftovers further encourages healthy eating habits (source).
46. Vitamin E
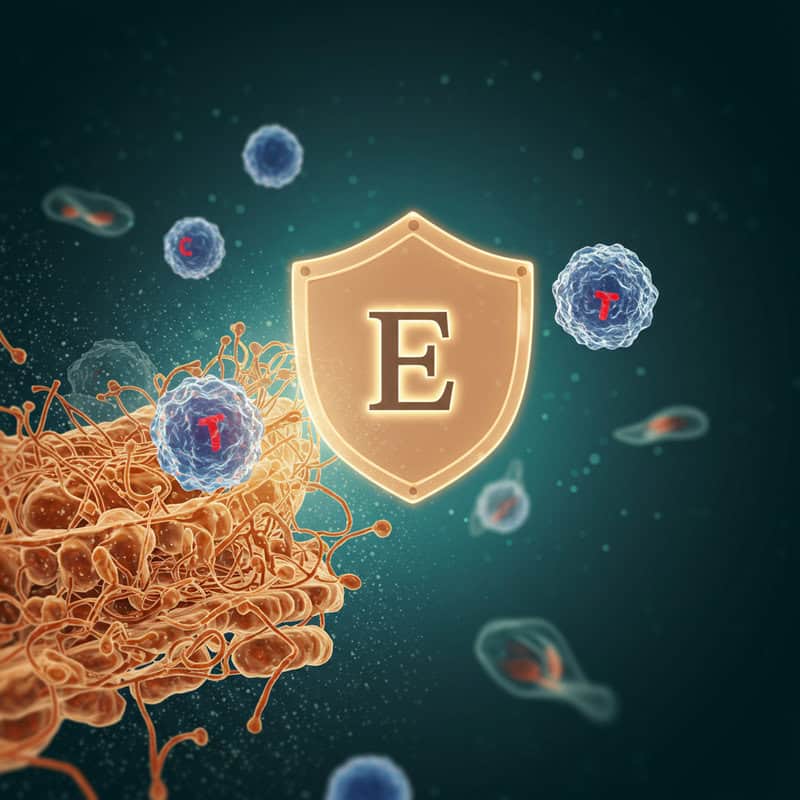
Vitamin E is a fat-soluble antioxidant that plays a vital role in protecting immune cells from oxidative damage. It helps stabilize cell membranes and enhances the function of T cells and other immune components, which are crucial for mounting an effective defense against pathogens and regulating inflammation. Adequate vitamin E intake may help reduce the risk of infections and support overall immune balance, making it especially important for individuals with autoimmune conditions (source).
Almonds are one of the best dietary sources of vitamin E, providing about 7 mg per ounce (23 nuts), which is nearly half the recommended daily allowance for adults. Other good sources include sunflower seeds, hazelnuts, peanuts, spinach, and avocado. Incorporating a variety of these foods into meals and snacks can help maintain sufficient vitamin E levels and support immune health.
The recommended dietary allowance for vitamin E is 15 mg (22.4 IU) per day for adults. Most people can meet their needs through a balanced diet rich in nuts, seeds, and leafy greens. Excessive supplementation is not recommended, as very high doses can interfere with blood clotting and cause other adverse effects (source).
47. Glycine
Glycine is a non-essential amino acid with notable anti-inflammatory and immunomodulatory properties, making it an important nutrient for individuals with autoimmune conditions. Glycine helps regulate immune responses, inhibit the production of pro-inflammatory cytokines, and protect tissues from oxidative stress. Research suggests that adequate glycine intake may help reduce inflammation, support healthy gut lining, and enhance overall immune function (source).
Bone broth is a particularly rich source of glycine, as the slow simmering process extracts this amino acid from animal bones and connective tissue. A cup of homemade or high-quality store-bought bone broth can provide a meaningful amount of glycine along with other amino acids beneficial for joint and gut health. Legumes, such as beans and lentils, also contain glycine and offer a plant-based option for supporting intake. Additionally, glycine is present in fish, poultry, and gelatin.
To include more glycine in your daily routine, enjoy bone broth as a warm beverage, use it as a base for soups or stews, or add cooked legumes to salads, grain bowls, or side dishes. Incorporating a variety of glycine-rich foods supports immune balance and may help reduce inflammation (source).
48. Allergen Label Reading

For individuals with autoimmune conditions, especially those prone to food sensitivities or allergies, reading ingredient labels is critical to avoid hidden allergens that could trigger immune reactions or worsen symptoms. Many packaged foods contain ingredients derived from common allergens—such as gluten, dairy, soy, nuts, or eggs—that may not be obvious from the product name or front-of-package claims (source).
Real-world examples of hidden allergens include wheat starch in processed meats, casein in non-dairy creamers, soy lecithin in chocolate, and egg proteins in salad dressings. Even foods labeled as “gluten-free” may be processed in facilities that handle wheat, posing a risk of cross-contamination. Additionally, ingredients like “natural flavors” or “spices” may sometimes contain allergenic substances, making detailed label examination essential.
Tips for safer shopping include familiarizing yourself with alternative names for allergens, scanning ingredient lists on every purchase (even trusted brands can change recipes), and choosing certified allergen-free or single-ingredient products when possible. Utilize mobile apps or lists from reputable organizations to identify hidden sources. When in doubt, contact manufacturers directly for clarification on ingredients (source).
49. Food Sensitivity Testing

Food sensitivity testing is increasingly popular among individuals with autoimmune conditions seeking to identify dietary triggers for inflammation or symptom flares. Various tests are available, including blood tests that measure IgG antibodies to specific foods. However, the accuracy and clinical relevance of these tests are debated, as IgG responses may simply reflect exposure rather than true intolerance or sensitivity (source).
In contrast, elimination diets—where suspected foods are removed for several weeks and then systematically reintroduced—are considered the gold standard for identifying food sensitivities. This approach allows individuals to observe symptom changes directly and can provide more reliable results than many commercial blood tests. While blood tests may be convenient, they are best used as a preliminary guide rather than a definitive diagnosis.
It is important to consult a healthcare professional, such as a registered dietitian or an allergist, before making significant dietary changes or interpreting test results. A professional can help design a safe and effective elimination protocol, interpret laboratory findings, and ensure nutritional adequacy throughout the process. Self-diagnosis and unsupervised restriction can lead to nutrient deficiencies and unnecessary dietary limitations (source).
50. Consistent Monitoring and Journaling
Consistently tracking symptoms and food intake is a powerful strategy for personalizing nutrition and managing autoimmune conditions. By monitoring what you eat and how you feel each day, patterns often emerge that can help identify trigger foods, track progress with dietary changes, and optimize overall health. This self-awareness enables individuals to make informed decisions and collaborate more effectively with healthcare providers (source).
Journaling can be done with a simple notebook or through digital tools and apps. Popular options include MyFitnessPal for tracking food intake, Cara Care for symptom and digestive health tracking, and specialized symptom tracker apps designed for chronic illness management. Entries might include meals, snacks, beverages, symptoms, medications, sleep quality, and stress levels.
Regularly reviewing your journal—weekly or monthly—with the help of a healthcare provider or dietitian can reveal trends and inform adjustments to your diet or lifestyle. This proactive approach fosters greater control, improved symptom management, and a more customized nutrition plan for long-term autoimmune wellness (source).
Conclusion

Nutritional support is a vital and urgent component in the management of autoimmune conditions, offering the potential to reduce inflammation, support immune balance, and improve quality of life. By taking proactive steps—such as adopting anti-inflammatory diets, monitoring triggers, and staying well-informed—individuals can positively influence their health outcomes. Early screening for nutrient deficiencies and food sensitivities, combined with personalized guidance from healthcare professionals, ensures safer and more effective interventions. Collaborative care with a registered dietitian or specialist can help tailor strategies to each individual’s unique needs (source). Embracing a comprehensive, nutrition-focused approach empowers those with autoimmune diseases to better manage symptoms and pursue long-term wellness.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





