Signs Your Blood Pressure Is Climbing
Hypertension affects nearly 1.28 billion adults worldwide, according to the World Health Organization. The cardiovascular system, responsible for circulating blood and nutrients, relies on stable blood pressure to function properly. Unfortunately, high blood pressure often develops without obvious symptoms, earning it the nickname “silent killer.” Many individuals remain undiagnosed until complications arise, making late detection a widespread and dangerous issue. Recognizing early signs is crucial to preventing serious health consequences and improving long-term outcomes.
1. Persistent Headaches
Persistent headaches are a commonly reported symptom in individuals with elevated blood pressure, though not everyone will experience them. High blood pressure can increase the pressure inside the skull, affecting blood vessels and surrounding tissues. This heightened pressure may result in a sensation of dull, throbbing pain, often felt at the back of the head or in the mornings. For example, someone who rarely suffers from headaches might suddenly notice ongoing discomfort, especially when waking up, that doesn’t respond to over-the-counter medications.
It’s important to note that while headaches are not always present with hypertension, their occurrence—especially if new, severe, or different from usual—can be a warning sign. According to the Centers for Disease Control and Prevention (CDC), sudden or severe headaches could indicate dangerously high blood pressure, also known as a hypertensive crisis. This situation requires immediate medical attention. If you experience headaches that are persistent, worsening over time, or accompanied by other symptoms such as vision changes or confusion, you should contact a healthcare provider as soon as possible to rule out serious complications.
2. Dizziness or Lightheadedness

Dizziness or lightheadedness can occur when high blood pressure disrupts the normal flow of blood to the brain. Elevated pressure places extra strain on blood vessels, sometimes causing them to narrow or stiffen. This can momentarily reduce the brain’s oxygen supply, leading to sensations of unsteadiness, faintness, or feeling as if the room is spinning. For instance, a middle-aged person might notice sudden bouts of dizziness when standing up quickly or during mild physical activity, despite previously feeling fine in those situations.
While occasional lightheadedness can be attributed to dehydration or standing up too fast, persistent or unexplained episodes may signal an underlying problem such as hypertension. According to the American Heart Association, these symptoms should not be ignored, especially if they are recurrent, severe, or occur alongside chest pain, blurred vision, or shortness of breath. If you experience frequent dizziness, fainting, or feel unable to maintain your balance, it is important to seek prompt medical evaluation to rule out complications like stroke or hypertensive crisis, both of which require immediate attention.
3. Blurred or Double Vision

High blood pressure can adversely affect the delicate blood vessels in the eyes, leading to vision disturbances such as blurred or double vision. When blood pressure is elevated, it can cause damage or leakage in the tiny vessels supplying the retina, a condition known as hypertensive retinopathy. Over time, this interference with blood flow may result in swelling, bleeding, or even detachment of the retina, all of which can impact how clearly you see. For example, someone who suddenly finds it difficult to read road signs or experiences episodes where their vision seems split may be experiencing these effects.
According to the American Academy of Ophthalmology, vision changes like blurriness, double vision, or seeing spots should never be dismissed, especially if they develop rapidly or are accompanied by other symptoms such as headache or dizziness. Such changes may signal that your blood pressure is dangerously high and harming your eyesight. If you notice any persistent or sudden alterations in your vision, it is critical to consult an eye doctor or healthcare provider immediately to prevent permanent damage and address the underlying cause.
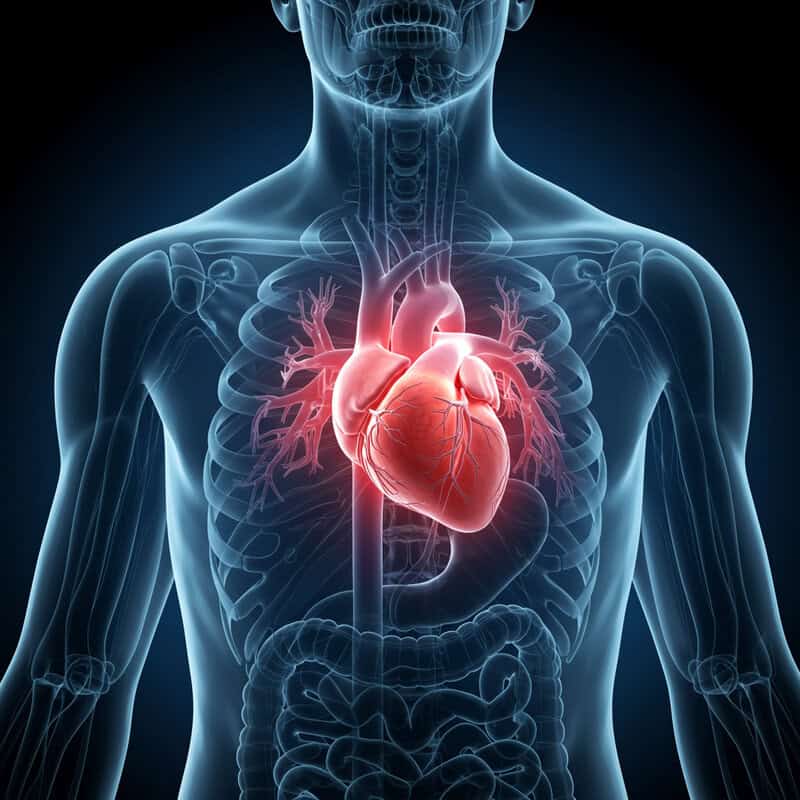
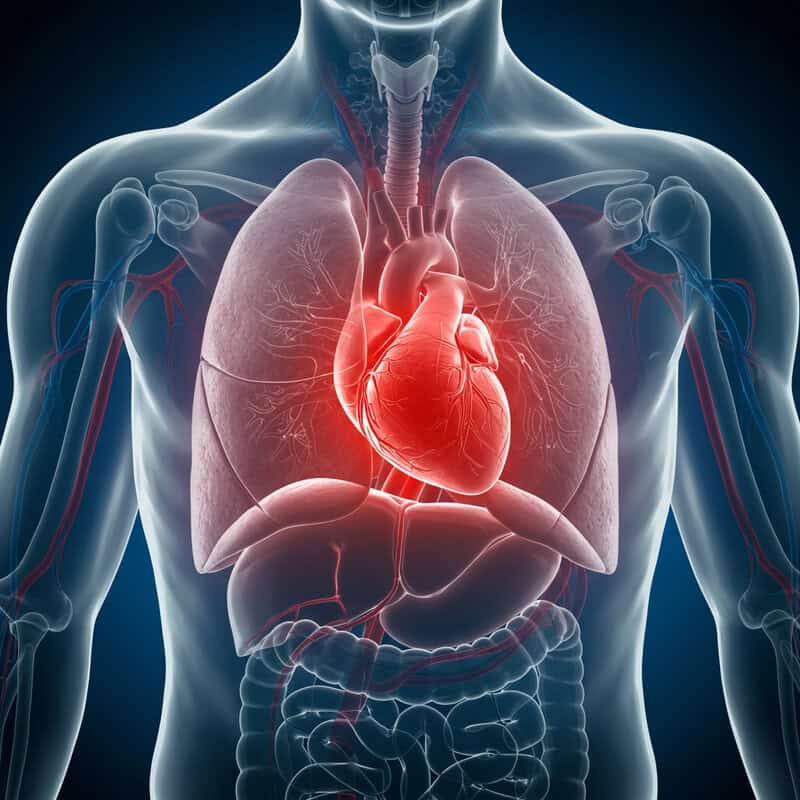
4. Shortness of Breath

Shortness of breath is a significant symptom that may indicate rising blood pressure is putting excess strain on the heart and lungs. Elevated blood pressure forces the heart to work harder to pump blood throughout the body, which can lead to left ventricular hypertrophy (thickening of the heart muscle) and eventually heart failure. As the heart’s efficiency decreases, fluid can accumulate in the lungs, making it difficult to breathe comfortably. Unlike the breathlessness experienced after intense exercise, hypertension-related shortness of breath can occur during everyday activities or even while at rest.
For example, someone who once climbed stairs with ease might suddenly find themselves pausing to catch their breath after only a few steps, or struggling to breathe when lying down. According to the American Heart Association, unexplained or persistent shortness of breath—especially when accompanied by chest pain, swelling, or fatigue—can be a warning sign of heart failure or hypertensive crisis. If you experience sudden or worsening breathlessness, it’s important to seek medical attention immediately, as this could be a sign of a life-threatening cardiovascular event.
5. Nosebleeds

Nosebleeds, or epistaxis, can occasionally signal that blood pressure is climbing, particularly when they occur without an obvious cause. High blood pressure puts extra force on the tiny, fragile blood vessels inside the nose, making them more likely to rupture. While most nosebleeds are benign and often triggered by dry air, allergies, or minor trauma, hypertension can make these vessels even more susceptible to breaking. For example, someone might wake up with a bloodstained pillow despite not having any recent nasal injury or cold symptoms.
According to the Mayo Clinic, high blood pressure is not the most common cause of nosebleeds, but frequent or severe episodes may warrant a closer look. If nosebleeds occur more often than usual—especially if they happen several times a week, are difficult to stop, or are accompanied by other symptoms like headache or dizziness—it’s important to consult a healthcare provider. Persistent nosebleeds could be a warning sign of uncontrolled hypertension and may require both blood pressure management and further evaluation to rule out more serious underlying conditions.
6. Chest Pain or Tightness
Chest pain or tightness is a serious symptom that may indicate your blood pressure is dangerously high and straining the heart muscle. Elevated blood pressure increases the resistance against which the heart must pump, forcing it to work harder and potentially reducing the flow of oxygen-rich blood to the heart itself. Over time, this excessive workload can lead to conditions like angina, where the heart muscle does not get enough oxygen, resulting in pain, pressure, or tightness in the chest.
While anxiety and stress can also trigger chest discomfort, anxiety-induced pain is often fleeting, sharp, or associated with emotional distress and may improve with relaxation. In contrast, hypertension-related chest pain is more likely to feel like a persistent, squeezing pressure, often brought on by physical activity or even at rest. According to the Centers for Disease Control and Prevention (CDC), chest pain should never be ignored—particularly if it is severe, lasts more than a few minutes, or is accompanied by symptoms like shortness of breath, nausea, or pain radiating to the arm or jaw. These could signal a heart attack or hypertensive emergency, requiring immediate medical attention.
7. Irregular Heartbeat
An irregular heartbeat, or arrhythmia, can be a subtle yet significant sign that your blood pressure is climbing. Hypertension causes the heart’s muscles and electrical system to work harder, potentially leading to disruptions in the heart’s normal rhythm. Over time, this added strain can make the heart’s walls thicken and stiffen, increasing the risk of conditions like atrial fibrillation. An arrhythmia may feel like your heart is racing, fluttering, skipping beats, or pounding unexpectedly.
To visualize this, imagine the heart as a drummer keeping a steady beat; high blood pressure acts like a disruptive force, causing the drummer to lose rhythm or speed up erratically. According to the American Heart Association, occasional palpitations can be harmless, but frequent, persistent, or sudden irregular heartbeats should not be ignored—especially if paired with dizziness, chest pain, shortness of breath, or fainting. These symptoms may indicate a more serious underlying issue requiring immediate evaluation. If you notice your heartbeat feels unusually fast, slow, or irregular, it’s important to consult a healthcare provider promptly for further assessment and management.
8. Fatigue or Unusual Tiredness

Fatigue or unusual tiredness can be a subtle but important sign that blood pressure is on the rise. When blood pressure is consistently elevated, the heart and blood vessels must work harder to circulate blood throughout the body. This persistent strain can reduce the efficiency of oxygen and nutrient delivery to tissues, leaving you feeling drained even after a full night’s sleep or minimal exertion. Unlike the normal tiredness that follows a busy day or poor rest, hypertension-related fatigue tends to be persistent, unexplained, and difficult to shake off.
For example, someone might notice feeling sluggish or lacking energy for everyday activities like walking, grocery shopping, or climbing stairs, despite no recent changes in routine or sleep habits. According to the Centers for Disease Control and Prevention (CDC), ongoing fatigue can be a warning sign of underlying cardiovascular strain, especially if accompanied by other symptoms like shortness of breath, swelling, or chest discomfort. If you experience tiredness that is persistent, worsens over time, or interferes with daily life, it’s wise to schedule a checkup to evaluate your blood pressure and rule out more serious health concerns.
9. Confusion or Trouble Concentrating
High blood pressure doesn’t just strain the heart and blood vessels—it can also impact the brain, sometimes resulting in confusion or difficulty concentrating. Hypertension may reduce blood flow to the brain, affecting the delivery of oxygen and essential nutrients to brain tissues. Over time, this can impair cognitive function, making it harder to focus, remember details, or process information quickly. For instance, someone might find themselves consistently forgetting appointments, misplacing everyday items, or struggling to follow conversations that were once easy to understand.
While it’s normal to experience some lapses in concentration due to stress or lack of sleep, persistent or sudden cognitive changes can signal a more serious underlying issue. According to the American Stroke Association, confusion and trouble concentrating—especially when accompanied by other symptoms like headache, vision changes, or numbness—can sometimes precede a stroke or indicate a hypertensive crisis. If you or someone you know experiences sudden confusion, disorientation, or difficulty understanding speech, it is critical to seek immediate medical attention, as these symptoms may require urgent evaluation and treatment to prevent permanent damage.
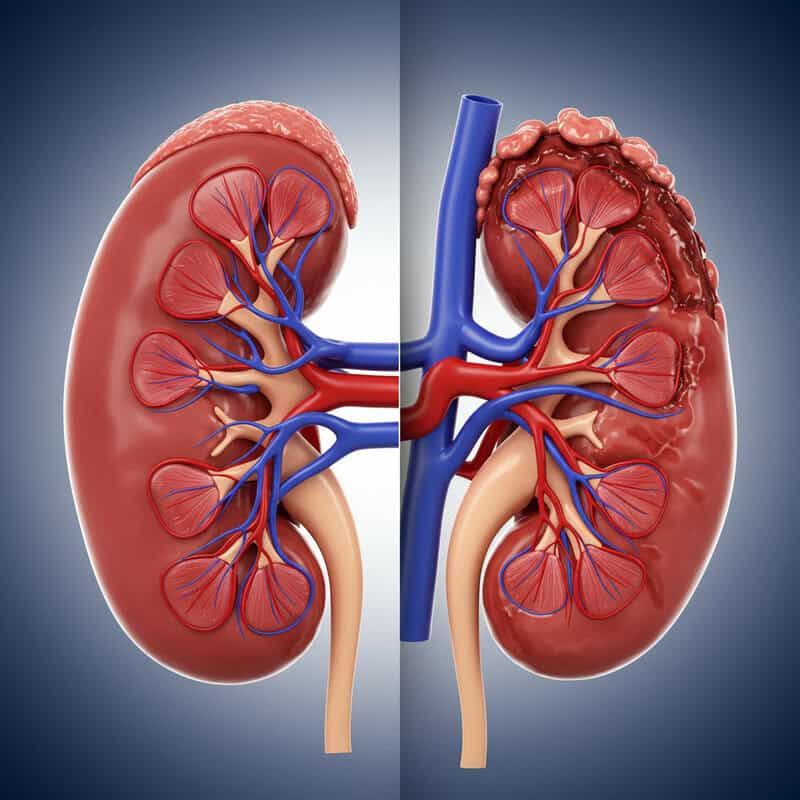
10. Blood in Urine
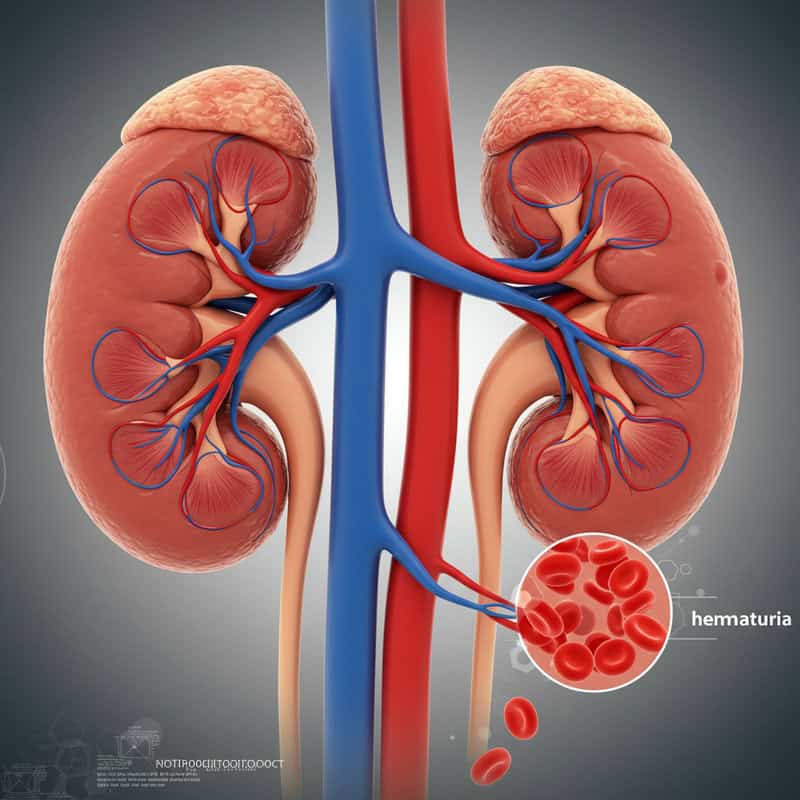
Blood in the urine, known medically as hematuria, can be a concerning sign that high blood pressure is affecting kidney function. The kidneys play a crucial role in filtering waste and excess fluids from the blood, but elevated pressure can damage the delicate network of blood vessels within these organs. This damage may allow blood cells to leak into the urine, resulting in pink, red, or tea-colored discoloration. For example, someone might suddenly notice reddish urine without any history of urinary tract infection, kidney stones, or recent injury.
According to the National Kidney Foundation, hematuria can indicate that high blood pressure is beginning to impair kidney function, which, if left untreated, may progress to chronic kidney disease or even kidney failure. Any appearance of blood in the urine should prompt immediate medical evaluation, particularly if it is accompanied by symptoms such as swelling, pain in the lower back, fever, or decreased urine output. Prompt assessment can help identify the underlying cause, prevent further kidney damage, and ensure appropriate treatment for both hypertension and kidney health.
11. Swelling in the Legs or Feet

Swelling in the legs or feet, also known as peripheral edema, can be a sign that high blood pressure is causing the body to retain excess fluid. When blood pressure is elevated, it puts added strain on the heart and blood vessels, particularly those responsible for circulating blood back from the lower extremities. This increased pressure can cause fluid to leak from the blood vessels into the surrounding tissues, resulting in noticeable swelling. Unlike the mild swelling that may occur after standing or sitting for a long time—which typically resolves with movement and elevation—hypertension-related edema is often persistent and may worsen throughout the day.
For example, someone might observe that their socks leave deep indentations, or that their shoes feel tighter by evening, even without recent changes in activity. According to the American Heart Association, swelling that is persistent, rapidly increasing, or accompanied by symptoms such as shortness of breath, chest pain, or sudden weight gain should not be ignored. These could be warning signs of heart failure or kidney complications related to uncontrolled hypertension and require prompt medical evaluation.
12. Facial Flushing

Facial flushing, or sudden redness of the face, can occur when blood pressure spikes and causes blood vessels near the skin’s surface to dilate. These episodes may be triggered by physical activity, emotional stress, exposure to heat, or even consuming spicy foods or alcohol. Unlike the harmless blushing that comes from embarrassment or excitement, facial flushing related to hypertension is often more intense and persistent, sometimes accompanied by a sensation of warmth or tingling.
For example, someone might notice their face turning noticeably red after climbing a flight of stairs or during moments of anger or anxiety, even if these situations didn’t cause such reactions in the past. According to the American Heart Association, facial flushing alone doesn’t necessarily mean you have high blood pressure, but frequent or unexplained episodes—especially if experienced along with other symptoms like headache, dizziness, or chest pain—may be a sign your blood pressure is climbing. If you notice recurrent flushing that is severe, persistent, or associated with additional symptoms, it’s wise to discuss these changes with your healthcare provider for further evaluation.
13. Palpitations or Pounding in Chest, Neck, or Ears
Palpitations, or the sensation of a pounding heartbeat, can occur when blood pressure rises and forces the heart to pump harder against increased resistance. This heightened workload may cause you to feel your heart beating strongly or rapidly in your chest, neck, or even your ears. While it’s normal for your heart rate to increase during stress, excitement, or physical activity, palpitations related to high blood pressure often arise unexpectedly and may be more pronounced or persistent.
For example, a person might notice their heart thumping loudly when lying down at night, or feel a rhythmic pulsing in their neck or ears during periods of rest. According to the Johns Hopkins Medicine, occasional palpitations are common and usually harmless. However, if you experience frequent, intense, or long-lasting episodes—especially if accompanied by dizziness, chest pain, shortness of breath, or fainting—it may indicate an underlying cardiovascular issue requiring evaluation. Persistent palpitations linked with other symptoms should prompt a visit to your healthcare provider to check your blood pressure and rule out more serious heart conditions.
14. Anxiety or Feeling of Impending Doom

High blood pressure doesn’t just affect the body physically—it can also influence your emotional and psychological state. Hypertension may cause or worsen feelings of anxiety, restlessness, or even a pronounced sense of impending doom. This psychological response is partly due to the body’s heightened stress and adrenaline levels as it struggles to cope with elevated pressure. While general anxiety is often triggered by external stressors or persistent worry, anxiety linked to hypertension may occur suddenly and be accompanied by other physical symptoms such as palpitations, sweating, or chest tightness.
For instance, someone experiencing a hypertensive crisis might feel an overwhelming sense that something is terribly wrong, even in the absence of an obvious threat. According to the Centers for Disease Control and Prevention (CDC), a sudden and intense feeling of anxiety—especially when combined with symptoms like severe headache, vision changes, chest pain, or difficulty breathing—should not be ignored. To distinguish between general anxiety and a more serious problem, pay attention to the presence of new or severe physical symptoms. If such symptoms accompany your anxiety, seek immediate medical evaluation to rule out life-threatening complications.
15. Trouble Sleeping

High blood pressure can disrupt normal sleep patterns, making it difficult to fall asleep, stay asleep, or feel rested upon waking. The body’s stress response to elevated blood pressure may cause increased heart rate, palpitations, or feelings of anxiety, all of which interfere with restful sleep. Furthermore, hypertension is closely linked to sleep disorders such as sleep apnea, where breathing repeatedly stops and starts during the night, depriving the body and brain of necessary oxygen. These disturbances may leave individuals feeling fatigued or irritable during the day.
For example, someone who previously slept soundly might begin waking several times during the night, tossing and turning, or feeling their heart pounding when lying down. According to the Sleep Foundation, persistent trouble sleeping, frequent nighttime awakenings, or loud snoring could be signs of underlying hypertension or a related sleep disorder. If you notice ongoing sleep issues—especially when combined with symptoms like morning headaches, daytime sleepiness, or high blood pressure readings—it’s important to consult a healthcare provider. Addressing poor sleep early can help manage both hypertension and overall health more effectively.
16. Ringing in the Ears (Tinnitus)

Ringing in the ears, or tinnitus, can sometimes be linked to high blood pressure, particularly when the condition causes changes in the blood flow through the small vessels of the inner ear. Elevated blood pressure increases the force of blood flow, which may be perceived as a whooshing, buzzing, or pulsing sound in one or both ears. This is often more noticeable in quiet environments or when lying down, as external noise is minimized and internal sounds become more apparent.
Unlike the temporary ringing experienced after exposure to loud noises, tinnitus associated with hypertension tends to be persistent and may coincide with other symptoms of elevated blood pressure, such as headaches or palpitations. According to the Johns Hopkins Medicine, ongoing or pulsatile tinnitus—especially when accompanied by dizziness, hearing loss, or a pounding sensation in your head—should not be ignored. These symptoms could indicate that high blood pressure is affecting your vascular system. If you experience persistent or worsening tinnitus, it’s important to seek medical advice to rule out hypertension-related complications and protect your hearing and overall health.
17. Nausea or Vomiting

Nausea or vomiting can be alarming symptoms that, in some cases, are linked to dangerously high blood pressure—particularly during a hypertensive crisis. When blood pressure rises to critical levels, it can disrupt blood flow to the brain and other vital organs, triggering the body’s emergency response. This lack of proper circulation and oxygenation may result in digestive upset, leading to feelings of queasiness or episodes of vomiting. Unlike the gastrointestinal discomfort associated with food poisoning or a stomach virus, nausea caused by hypertension is often sudden, severe, and accompanied by other neurological or cardiovascular symptoms.
For example, someone may experience intense nausea along with a pounding headache, vision changes, or confusion, which does not improve after resting or avoiding certain foods. According to the Centers for Disease Control and Prevention (CDC), the presence of nausea or vomiting—especially when paired with symptoms like severe headache, chest pain, or shortness of breath—may be a sign of a hypertensive emergency. Immediate medical attention is essential in these situations, as untreated hypertensive crises can lead to stroke, heart attack, or organ damage.
18. Excessive Sweating

Excessive sweating, or hyperhidrosis, can be a physiological response to high blood pressure, particularly when it causes the heart to race or the body to enter a state of heightened stress. Elevated blood pressure activates the sympathetic nervous system—the “fight or flight” response—leading to the release of stress hormones like adrenaline. This hormonal surge can cause sweating that feels out of proportion to the environment or physical activity. Unlike sweating from exercise or hot weather, hypertension-induced sweating often occurs suddenly and without an obvious external trigger.
For example, someone might break into a sweat while sitting quietly at their desk or while lying in bed at night, accompanied by feelings of anxiety or a pounding heart. According to the American Heart Association, excessive or unexplained sweating, especially when paired with additional symptoms such as chest pain, shortness of breath, or dizziness, should not be dismissed. These signs may indicate a hypertensive emergency or an underlying heart problem. If you experience sudden, severe, or recurrent episodes of sweating unrelated to temperature or activity, it’s important to consult your healthcare provider for evaluation.
19. Vision Loss

Severe hypertension can have a profound impact on the eyes, especially the retina—the layer at the back of the eye responsible for processing visual information. Extremely high blood pressure can cause the small blood vessels in the retina to swell, leak, or even rupture, leading to a condition known as hypertensive retinopathy. This damage can cause sudden, partial, or complete loss of vision in one or both eyes. Unlike gradual, age-related vision changes such as presbyopia or cataracts, vision loss related to high blood pressure often occurs abruptly and may be accompanied by other symptoms like headache or confusion.
For instance, a person may suddenly notice a dark patch, blurry vision, or difficulty seeing out of part of their visual field without any prior warning. According to the American Academy of Ophthalmology, sudden vision loss is a medical emergency and may indicate a hypertensive crisis or even retinal artery or vein occlusion. Immediate medical attention is crucial, as prompt treatment may help preserve eyesight and prevent further complications. Any rapid or unexplained change in vision should be evaluated by an eye doctor or emergency medical personnel without delay.
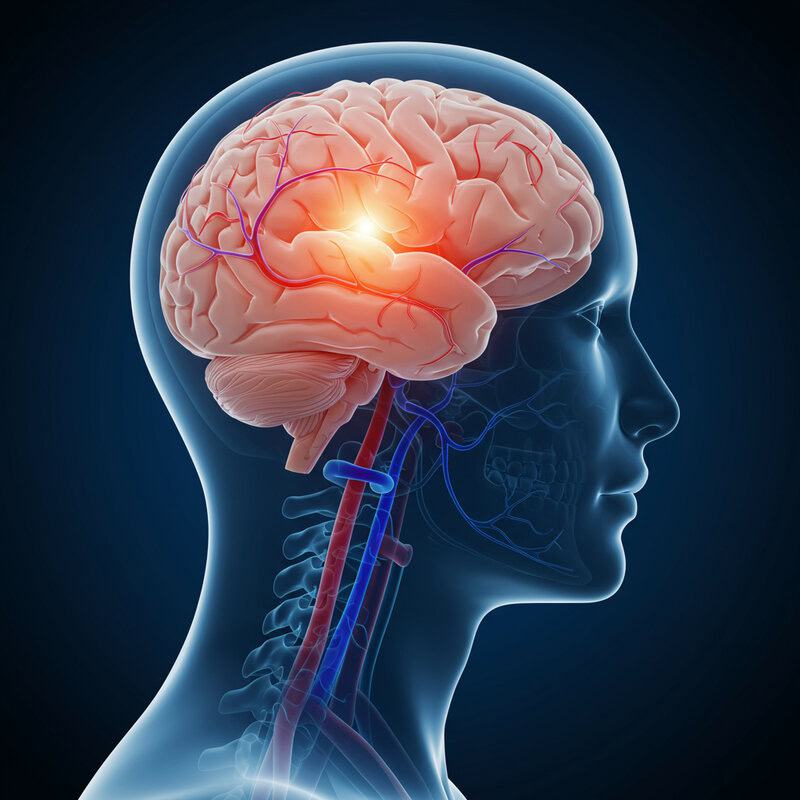
20. Weakness or Numbness (Especially on One Side)

High blood pressure is one of the leading risk factors for stroke, a condition that occurs when blood flow to a part of the brain is interrupted or severely reduced. This lack of circulation can result in sudden weakness or numbness, particularly on one side of the body, affecting the face, arm, or leg. Such symptoms arise because the brain is no longer receiving the oxygen and nutrients it needs to function normally. Unlike temporary numbness from sitting awkwardly, stroke-related weakness or numbness comes on suddenly and does not resolve with movement or time.
For example, a person may suddenly find themselves unable to lift one arm, smile symmetrically, or feel sensation in one leg while performing ordinary activities. According to the American Stroke Association, these are classic signs of a stroke and constitute a medical emergency. Prompt recognition and immediate action are critical; call emergency services if you or someone else experiences sudden weakness, numbness, difficulty speaking, or facial drooping. Rapid treatment can greatly improve the chances of recovery and minimize lasting damage from a stroke caused by uncontrolled high blood pressure.
21. Difficulty Speaking
Difficulty speaking, medically known as aphasia, can occur when high blood pressure leads to changes or damage in the brain, especially during a stroke. Hypertension increases the risk of blood vessel rupture or blockage in the brain, which can disrupt the areas responsible for language and communication. This may result in slurred speech, trouble finding the right words, or the inability to speak clearly or understand others. Unlike the occasional word-finding difficulty everyone experiences, hypertension-related speech problems typically come on suddenly and are often accompanied by other neurological symptoms.
Imagine a scenario where someone is having a conversation and abruptly starts talking in a way that is difficult to understand, or their sentences become garbled without any obvious cause. According to the American Stroke Association, sudden difficulty speaking or understanding speech is a hallmark sign of stroke and should be treated as a medical emergency. Immediate action—calling emergency services—can be lifesaving and may minimize long-term damage. If you or someone around you develops sudden speech problems, especially with other stroke symptoms such as weakness, numbness, or confusion, seek urgent medical attention without delay.
22. Sudden Severe Headache
A sudden, severe headache can be a warning sign of a hypertensive crisis, where blood pressure rises to dangerously high levels. During such episodes, the force of blood against the vessel walls increases rapidly, potentially causing blood vessels in the brain to leak or rupture. This abrupt change may result in an intense, “worst-ever” headache that comes on quickly and is often described as throbbing or explosive. Unlike migraines, which may be preceded by aura, sensitivity to light, or gradual onset, headaches from hypertensive crises usually appear suddenly and are often accompanied by other alarming symptoms such as confusion, blurred vision, or nausea.
For instance, a person may be going about their daily routine and then, without warning, experience a headache so severe that it quickly incapacitates them. According to the Centers for Disease Control and Prevention (CDC), this type of headache warrants immediate medical attention, as it could signal a life-threatening complication like a stroke or brain hemorrhage. If you or someone else experiences a sudden, severe headache—especially if it is accompanied by neurological symptoms—call emergency services without delay to minimize the risk of permanent damage or death.
23. Difficulty Breathing When Lying Down

Difficulty breathing when lying down, known as orthopnea, can be a telling sign that high blood pressure is placing excess strain on the heart. When you recline, blood that has pooled in your legs during the day returns to the heart, increasing its workload. If hypertension has weakened the heart or led to heart failure, the heart may struggle to pump this extra volume efficiently, causing fluid to back up into the lungs and making it hard to breathe comfortably in a horizontal position.
For example, someone might find they need to prop themselves up with multiple pillows or even sleep sitting up to avoid a feeling of suffocation or gasping for air at night. According to the American Heart Association, this symptom, especially when accompanied by swelling in the legs, sudden weight gain, or fatigue, can be an early indicator of congestive heart failure. If you experience new or worsening difficulty breathing when lying down, it’s important to seek medical evaluation promptly, as this may signify serious complications from uncontrolled high blood pressure.
24. Unexplained Weight Gain

Unexplained weight gain can sometimes be linked to high blood pressure, especially when it results from the body retaining excess fluid due to cardiovascular or kidney strain. Elevated blood pressure can damage the blood vessels in the kidneys, impairing their ability to filter waste and regulate fluid balance. This can lead to accumulation of fluid in the tissues, which manifests as rapid weight gain rather than gradual increases associated with changes in diet or activity. Unlike the typical fluctuations in weight that occur with overeating, hormonal changes, or exercise patterns, hypertension-related weight gain often occurs over just a few days and is frequently accompanied by swelling in the legs, feet, or abdomen.
For example, someone might notice their clothes fitting tighter and observe puffiness around their ankles or abdomen, even though their eating habits haven’t changed. According to the American Heart Association, unexplained weight gain—particularly increases of more than two to three pounds in 24 hours or five pounds in a week—should be monitored closely. This could indicate fluid retention from worsening heart or kidney function due to uncontrolled hypertension. If you notice rapid, persistent weight gain, it’s important to contact your healthcare provider for timely evaluation and management.
25. Frequent Urination at Night

Frequent urination at night, known as nocturia, may be an early sign that high blood pressure is affecting your kidneys. Hypertension can damage the small blood vessels in the kidneys, impairing their ability to regulate fluid and waste removal efficiently. As a result, more fluid may be filtered and excreted overnight, causing you to wake up multiple times to urinate. While nocturia can also be caused by drinking excessive fluids in the evening, consuming caffeine or alcohol, or having conditions like diabetes or an enlarged prostate, a sudden increase in nighttime urination without clear cause can be a red flag.
For example, a person who previously slept through the night may begin waking up two or more times to use the bathroom, even when limiting fluid intake before bed. According to the National Kidney Foundation, persistent nocturia, especially when accompanied by other signs such as swelling, fatigue, or changes in urine color, may indicate impaired kidney function from hypertension. If you experience frequent nighttime urination that disrupts your sleep or comes with other symptoms of high blood pressure, it is important to consult your healthcare provider for further evaluation.
26. Reduced Exercise Tolerance

Reduced exercise tolerance refers to the inability to perform physical activities at your previous level of ease or endurance and can be an early warning sign that high blood pressure is affecting your cardiovascular health. Elevated blood pressure makes the heart work harder to pump blood, which can lead to the thickening or weakening of heart muscle over time. This extra strain diminishes the heart’s efficiency and may result in reduced oxygen delivery to muscles during exercise. Unlike the typical fatigue you might feel after a long day or an intense workout, hypertension-related exercise intolerance often appears as unexpected breathlessness, excessive tiredness, or needing to stop sooner than usual even during routine activities.
For example, a person who once enjoyed brisk walking or cycling may suddenly find themselves winded or needing frequent breaks, despite no significant lifestyle changes. According to the American Heart Association, a noticeable decrease in your ability to exercise can signal underlying heart or vascular issues caused by uncontrolled hypertension. If you find your stamina is dropping, or you’re unable to complete familiar workouts, it’s important to reassess your exercise goals with a healthcare provider and to check your blood pressure to rule out cardiovascular complications.
27. Forgetfulness
Ongoing high blood pressure can impair cognitive function, leading to episodes of forgetfulness that go beyond what’s expected with normal aging. Hypertension reduces the elasticity of blood vessels and can diminish blood flow to the brain, which is essential for optimal mental performance. Over time, this can damage small blood vessels and white matter in the brain, affecting memory, decision-making, and the ability to process new information. While everyone occasionally forgets names or misplaces keys, memory lapses caused by hypertension tend to be more frequent, persistent, and may interfere with daily life.
For example, a person might repeatedly forget appointments, struggle to recall recent conversations, or have difficulty following multi-step instructions, even though they previously managed these tasks with ease. According to the Alzheimer’s Association, persistent forgetfulness or confusion, particularly when accompanied by other symptoms of high blood pressure, could be an indication of vascular dementia or cognitive decline linked to chronic hypertension. If you notice a pattern of memory problems that seem to be worsening, it is wise to consult your healthcare provider for assessment and to discuss strategies to control blood pressure and support brain health.
28. Erectile Dysfunction
Erectile dysfunction (ED) is a common but often overlooked complication of high blood pressure. Hypertension damages blood vessels throughout the body, including those supplying the penis. This vascular damage reduces blood flow, making it more difficult to achieve or maintain an erection. Unlike occasional difficulties that may result from stress or fatigue, ED related to high blood pressure tends to develop gradually and persist over time, regardless of mood or circumstances.
For example, a man who previously had normal sexual function may begin to notice a consistent inability to maintain an erection, even when feeling mentally and emotionally ready. According to the American Heart Association, ED can be an early warning sign of vascular problems and is often linked to the same risk factors as heart disease and stroke. If you experience ongoing issues with sexual function, it’s important to discuss these changes with your doctor. Not only can addressing ED improve quality of life, but it may also prompt early detection and management of underlying hypertension, reducing the risk of serious cardiovascular events.
29. Loss of Appetite

Loss of appetite can be a subtle indicator that high blood pressure is affecting your overall health. Hypertension can impact appetite in several ways. When blood pressure is elevated, it may lead to organ strain, particularly in the heart, kidneys, and digestive system, which can reduce the desire to eat. Additionally, some blood pressure medications—such as diuretics—may cause gastrointestinal side effects like nausea or altered taste, further decreasing appetite. While it’s common to temporarily lose interest in food due to stress, viral illness, or dietary changes, appetite loss caused by hypertension or its treatment tends to persist and may be accompanied by other symptoms, such as fatigue or nausea.
For example, someone may notice they’re skipping meals or feeling full quickly, even though they previously enjoyed a healthy appetite. According to the Centers for Disease Control and Prevention (CDC), persistent loss of appetite—especially when paired with unintentional weight loss, nausea, or swelling—warrants medical attention. If you experience ongoing appetite changes without a clear explanation, consult your healthcare provider. Addressing loss of appetite can help uncover underlying complications from hypertension and ensure you’re receiving adequate nutrition for overall well-being.
30. Increased Thirst

Increased thirst can sometimes indicate that your body is responding to high blood pressure or related complications. When blood pressure is elevated, the kidneys may struggle to regulate fluid and electrolyte balance, leading to increased urine output and a compensatory urge to drink more fluids. Additionally, some antihypertensive medications—especially diuretics—can cause dehydration, further driving thirst. Unlike ordinary thirst after exercise or on a hot day, persistent or excessive thirst related to hypertension tends to occur even without obvious triggers, and may be accompanied by frequent urination or dry mouth.
For example, someone might find themselves needing to sip water constantly throughout the day and night, even when not physically active or exposed to heat. According to the National Kidney Foundation, ongoing increased thirst can be a sign of underlying kidney stress or diabetes, both of which are commonly linked to uncontrolled high blood pressure. If you experience persistent or unexplained thirst, especially when combined with other symptoms like fatigue, swelling, or changes in urination, it’s important to seek medical evaluation to rule out serious complications and ensure your blood pressure and fluid balance are well managed.
31. Irregular Pulse in the Wrist

An irregular pulse in the wrist can be a sign that high blood pressure is disrupting the normal electrical signals that control heart rhythm. When hypertension persists, it can cause the heart’s chambers to thicken or stretch, leading to arrhythmias—abnormal heart rhythms that may be felt as skipped beats, extra beats, or a fluttering sensation. This irregularity can sometimes be detected by simply feeling your own pulse at the wrist and noticing that the beats are not evenly spaced. Unlike occasional skipped beats that might result from caffeine or stress, persistent pulse irregularities are more likely to be linked to cardiovascular changes caused by prolonged high blood pressure.
For example, someone might check their pulse during a moment of rest and notice varying intervals between beats, or a pulse that feels erratic rather than steady. According to the American Heart Association, any new or frequent irregularities in your pulse—especially if accompanied by symptoms like dizziness, chest discomfort, or shortness of breath—should prompt a medical evaluation. Detecting and treating arrhythmias early can help prevent more serious complications, such as stroke or heart failure, often associated with uncontrolled hypertension.
32. Muscle Tremors or Twitching

Muscle tremors or twitching can sometimes accompany spikes in blood pressure, particularly during hypertensive episodes or as a side effect of certain blood pressure medications. Elevated blood pressure can disrupt the normal function of nerves and muscles by altering blood flow, electrolyte balance, and nerve signaling. This may result in involuntary muscle contractions, shaking, or twitching, most commonly in the hands, face, or legs. Unlike the fine tremors often seen with anxiety or stress, which usually subside with relaxation, hypertension-related muscle activity may appear suddenly and persist even when you are calm.
For instance, someone might notice their hand shaking while holding a cup or feel persistent muscle twitches in their legs at rest, despite no recent increase in caffeine intake or anxiety levels. According to the Mayo Clinic, persistent or unexplained muscle tremors and twitching should be evaluated by a healthcare provider, especially if accompanied by other symptoms like weakness, numbness, or changes in consciousness. These signs could be related to underlying electrolyte imbalances, medication side effects, or neurological effects of severe hypertension and require prompt assessment.
33. Easy Bruising

Easy bruising can be a noticeable but often overlooked sign that high blood pressure is affecting the integrity of your blood vessels. Elevated pressure places extra stress on the small capillaries and veins just beneath the skin, making them more fragile and susceptible to breaking. As a result, even minor bumps or seemingly insignificant contact can cause blood to leak into surrounding tissues, leading to bruises. This differs from normal bruising, which typically follows a clear injury or impact and resolves predictably over time.
For example, an individual might find new bruises on their arms or legs without recalling any trauma, or notice that bruises are appearing more frequently and taking longer to heal. According to the Centers for Disease Control and Prevention (CDC), persistent or unexplained bruising—especially when accompanied by other symptoms like bleeding gums, nosebleeds, or swelling—warrants closer monitoring and medical attention. Such bruising may indicate that high blood pressure is weakening blood vessel walls or could be a side effect of certain antihypertensive medications. If you notice a sudden increase in bruising, consult your healthcare provider to rule out underlying issues and ensure proper blood pressure management.
34. Cold Hands and Feet

Cold hands and feet can sometimes signal changes in circulation resulting from high blood pressure. When blood pressure is elevated for prolonged periods, it can cause blood vessels to narrow or stiffen, reducing blood flow to the body’s extremities. This diminished circulation may leave your fingers and toes feeling unusually cold, numb, or even tingly, especially in comparison to the rest of your body. Unlike the temporary chill experienced during cold weather or after touching something cold, hypertension-related coldness typically persists regardless of external temperature or activity.
For example, someone may notice their hands and feet remain cold even indoors or while wearing warm clothing, and rubbing or massaging them offers little relief. According to the American Heart Association, persistent coldness in the extremities can be a sign of impaired blood flow and may indicate peripheral artery disease or other vascular issues associated with uncontrolled hypertension. If you experience ongoing coldness, discoloration, or numbness in your hands or feet—especially if it worsens or is accompanied by pain or sores—it’s important to seek medical evaluation to assess your circulation and blood pressure management.
35. Difficulty Climbing Stairs

Difficulty climbing stairs can be a sign that high blood pressure is impacting your cardiovascular and respiratory systems, limiting your ability to perform everyday activities. When blood pressure is consistently elevated, the heart has to work harder to pump blood, which can lead to reduced oxygen delivery to muscles during exertion. As a result, tasks that once felt routine—like walking up a flight of stairs—may suddenly leave you breathless, fatigued, or with a rapid heart rate. This is different from the mild shortness of breath or tiredness that can occur after intense exercise or a long day, as hypertension-related problems tend to develop gradually and persist over time.
For example, someone might find themselves pausing halfway up the stairs to catch their breath or experiencing leg weakness with each step, even though they previously managed stairs without issue. According to the American Heart Association, a noticeable decrease in your ability to climb stairs or perform similar daily tasks could indicate reduced heart or lung function associated with uncontrolled hypertension. If you observe persistent changes in your exercise tolerance or daily abilities, it’s important to discuss these symptoms with your healthcare provider for further evaluation and management.
36. Frequent Muscle Cramps

Frequent muscle cramps can be linked to high blood pressure, especially when hypertension or its treatment causes imbalances in key electrolytes like potassium, magnesium, and calcium. Certain blood pressure medications, such as diuretics, increase urine output and may lead to the loss of these important minerals, which are essential for normal muscle function. When electrolyte levels drop, muscles are more prone to involuntary contractions, spasms, or painful cramps, often occurring in the legs, feet, or hands. Unlike occasional cramps from overexertion or dehydration, hypertension-related cramps can arise even with minimal activity or at rest.
For example, someone might wake up in the middle of the night with severe calf cramps or experience frequent muscle spasms after starting a new blood pressure medication. According to the Mayo Clinic, persistent or recurrent muscle cramps—especially when accompanied by other symptoms like weakness, fatigue, or heart palpitations—should prompt a review of your blood pressure treatment and electrolyte levels. If you notice frequent or severe cramps without a clear cause, consult your healthcare provider to ensure proper blood pressure control and address any underlying imbalances.
37. Poor Wound Healing

Poor wound healing can be an overlooked consequence of high blood pressure, as hypertension can damage blood vessels and reduce the efficiency of blood flow to tissues. When circulation is compromised, oxygen and essential nutrients struggle to reach injured areas, slowing the repair process. This is similar to what occurs in diabetes, where persistent high blood sugar impairs vascular health and immune response, leading to delayed recovery from cuts, scrapes, or ulcers. With hypertension, even minor wounds may persist longer than expected, become infected more easily, or develop into chronic sores.
For example, someone might notice that a simple scratch or blister on their foot remains red, swollen, or unhealed for weeks, despite basic wound care. According to the American Heart Association, wounds that do not heal within a reasonable period or show signs of infection (such as increasing redness, pus, or pain) should prompt a medical evaluation. Persistent poor wound healing, especially when paired with other symptoms of high blood pressure, may indicate underlying vascular problems or compromised immune function. Early intervention can help prevent complications and support overall healing and cardiovascular health.
38. Fluttering in the Chest
Fluttering sensations in the chest, often described as heart palpitations, can be directly linked to arrhythmias caused by high blood pressure. Hypertension puts extra stress on the heart’s electrical system and muscle tissue, increasing the risk of abnormal heart rhythms such as atrial fibrillation or premature beats. These episodes may feel like your heart is skipping, racing, or fluttering unexpectedly, especially during periods of rest or minimal exertion. Unlike the occasional flutter caused by excitement, caffeine, or anxiety, hypertension-related palpitations may persist or occur without a clear trigger.
For example, someone relaxing on the couch may suddenly feel a rapid, irregular flutter in their chest that lasts for several seconds or recurs repeatedly throughout the day. According to the American Heart Association, frequent, prolonged, or intense fluttering—particularly when associated with symptoms like dizziness, chest pain, or shortness of breath—should prompt prompt medical evaluation. These sensations can be signs of underlying heart rhythm disturbances that increase the risk of stroke or heart failure if left untreated. If chest fluttering becomes a regular occurrence, consult your healthcare provider for assessment and appropriate management.
39. Increased Sensitivity to Noise
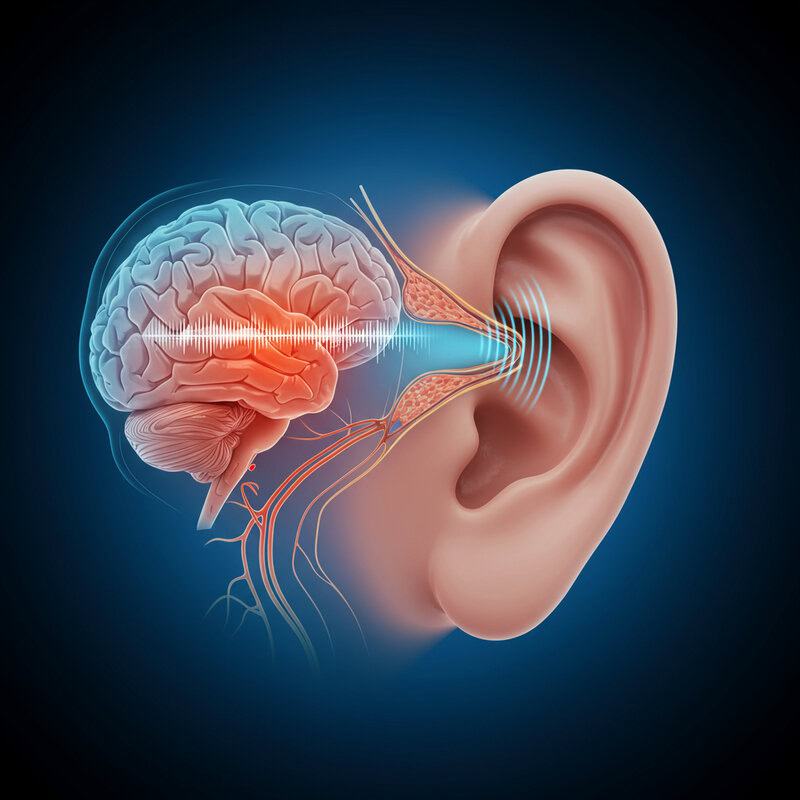
Increased sensitivity to noise, known as hyperacusis, can sometimes occur when blood pressure is elevated. High blood pressure may alter blood flow to the auditory nerves and parts of the brain responsible for sensory processing, intensifying your reactions to everyday sounds. Unlike the normal discomfort you might feel from sudden loud noises or prolonged exposure to a noisy environment, hypertension-related noise sensitivity can make ordinary sounds—like clinking dishes, traffic, or conversation—feel unusually jarring, overwhelming, or even physically uncomfortable.
For instance, a person might suddenly find themselves flinching or feeling anxious in situations that never bothered them before, such as watching television at a moderate volume or being in a crowded restaurant. According to the Centers for Disease Control and Prevention (CDC), new or increased sensitivity to noise, especially if it develops alongside other symptoms such as headaches, dizziness, or ringing in the ears, can be a sign your blood pressure is climbing. If you notice a persistent change in your tolerance to sound, it may be wise to monitor your blood pressure and consult your healthcare provider to rule out underlying cardiovascular or neurological issues.
40. Red Spots in Eyes

Red spots in the eyes, medically referred to as subconjunctival hemorrhages, can sometimes be a visible sign of high blood pressure. Sudden spikes in blood pressure can cause small, fragile blood vessels on the surface of the eye to burst, resulting in bright red patches or spots on the white part of the eye. Unlike the mild redness that may occur from eye strain, allergies, or lack of sleep, subconjunctival hemorrhages appear as distinct, well-defined spots that do not cause pain or affect vision but can look alarming.
For example, someone might notice a red spot in their eye after a bout of intense coughing, sneezing, or even seemingly without any obvious cause. According to the American Academy of Ophthalmology, while most subconjunctival hemorrhages are harmless and resolve on their own, frequent or unexplained occurrences—especially when accompanied by other symptoms like headaches, blurred vision, or high blood pressure readings—should be evaluated by a healthcare professional. Persistent or recurrent red spots could indicate ongoing blood pressure problems or underlying vascular issues that require medical assessment and management.
41. Frequent Nightmares

Frequent nightmares and vivid dreams can sometimes be linked to sleep disturbances caused by high blood pressure. Hypertension is associated with sleep disorders such as insomnia and obstructive sleep apnea, both of which can fragment sleep and increase the likelihood of intense, disturbing dreams. When blood pressure is high, the body’s stress response may be heightened during sleep, making nightmares more frequent or memorable upon waking. This differs from the occasional bad dream that might follow a stressful day; nightmares related to hypertensive sleep disturbances often recur and may disrupt sleep quality night after night.
For example, someone might repeatedly wake from unsettling dreams, feeling anxious or with a racing heart, despite no recent emotional stress or changes in routine. According to the Sleep Foundation, persistent changes in sleep patterns—such as frequent nightmares, restless sleep, or difficulty staying asleep—can be a sign of underlying health problems, including high blood pressure. If you notice recurring nightmares or significant changes in your sleep quality, it is important to discuss these symptoms with your healthcare provider. Early intervention can help identify and manage hypertension, improving both sleep and overall well-being.
42. Chest Congestion
Chest congestion can occur when high blood pressure leads to fluid buildup in the lungs, a condition often associated with heart failure. When the heart is strained by persistent hypertension, its ability to efficiently pump blood diminishes, causing blood to back up in the pulmonary veins. This backup increases pressure in the lung’s blood vessels, forcing fluid into the air sacs and resulting in a feeling of heaviness, tightness, or congestion in the chest. Unlike congestion from respiratory infections, which may be accompanied by coughing, fever, or sore throat, hypertension-related chest congestion often develops gradually and may be associated with shortness of breath or swelling in the legs.
For example, someone with previously normal breathing might begin to notice a persistent sense of fullness or rattling in the chest, particularly when lying flat or after mild exertion. According to the American Heart Association, red flag symptoms such as sudden or severe shortness of breath, chest pain, or coughing up pink, frothy sputum require immediate medical attention. Persistent or unexplained chest congestion should always be evaluated by a healthcare provider, as it may be a sign of worsening heart failure or hypertensive complications.
43. Decreased Urine Output
Decreased urine output, medically known as oliguria, can be a sign that high blood pressure is impairing kidney function. The kidneys rely on healthy blood vessels to filter waste and regulate fluid balance. When blood pressure is persistently elevated, it can damage these vessels, reducing the kidneys’ ability to filter blood efficiently. As a result, less urine is produced, and waste products may build up in the body. Unlike temporary reductions in urination caused by dehydration or limited fluid intake, decreased urine output linked to hypertension often occurs even when hydration is adequate and may be accompanied by swelling, fatigue, or changes in urine color.
For instance, someone who normally urinates several times a day may notice they’re going much less frequently, or their urine appears dark and concentrated. According to the National Kidney Foundation, a sudden or persistent decrease in urine output—especially when accompanied by other symptoms like swelling, confusion, or shortness of breath—requires prompt medical evaluation. These signs may indicate acute kidney injury or worsening chronic kidney disease, both of which are serious complications of uncontrolled high blood pressure and require immediate intervention.
44. Difficulty Swallowing

Difficulty swallowing, known as dysphagia, can sometimes arise as a rare but serious neurological complication of high blood pressure. Extremely elevated blood pressure can increase the risk of stroke or transient ischemic attacks (TIAs), both of which can affect the brain regions responsible for coordinating the muscles involved in swallowing. This disruption may result in sensations of food getting stuck, coughing or choking while eating, or even unintentional weight loss due to an inability to consume enough nutrients. Unlike occasional swallowing problems from eating too quickly or having a sore throat, hypertension-related dysphagia tends to be sudden and persistent.
For example, a person may find it unexpectedly difficult to swallow liquids or solids, or they may begin to cough or gag during meals without a clear cause. According to the American Stroke Association, sudden onset of swallowing difficulties—especially when associated with other neurological symptoms such as facial drooping, slurred speech, or weakness—should be treated as a medical emergency. If you or someone you know experiences new and unexplained trouble swallowing, seek immediate medical attention to rule out stroke or other acute neurological events related to uncontrolled hypertension.
45. Persistent Cough
A persistent cough can be linked to high blood pressure either directly, as a sign of heart failure, or indirectly, as a side effect of certain blood pressure medications. Some antihypertensive drugs, particularly ACE inhibitors, are known to cause a dry, chronic cough in sensitive individuals. Additionally, when high blood pressure leads to heart failure, fluid may accumulate in the lungs, triggering a wet, productive cough that may worsen at night or when lying down. Unlike the temporary cough from a cold or allergies, hypertension-related cough tends to linger and may not respond to standard remedies.
For example, someone might notice a persistent tickle in their throat or a cough that produces frothy or pink-tinged sputum, especially in conjunction with other symptoms like shortness of breath or swelling in the legs. According to the American Heart Association, any cough that lasts more than a few weeks, particularly if it is associated with breathing difficulties, chest pain, or changes in sputum, should prompt a consultation with a healthcare provider. Persistent coughs may signal side effects or complications from hypertension that require assessment and adjustment of treatment.
46. Swelling Around the Eyes

Swelling around the eyes, also known as periorbital edema, can be a sign that high blood pressure is causing fluid retention in some of the body’s most delicate tissues. The area around the eyes is particularly susceptible to swelling because the skin is thin and blood vessels are close to the surface. When hypertension impairs kidney function or leads to heart failure, the body’s ability to regulate fluid balance is compromised, allowing fluid to accumulate noticeably around the eyes. This type of swelling is typically most pronounced in the morning and may persist throughout the day.
Unlike the puffiness that can result from allergies, crying, or lack of sleep—which is often accompanied by itching, redness, or watery eyes—hypertension-related swelling is more likely to occur with other signs of fluid overload, such as swelling in the legs or sudden weight gain. According to the National Kidney Foundation, persistent or unexplained periorbital edema should prompt evaluation for underlying hypertension or kidney disease. If you notice ongoing swelling around your eyes, especially when paired with other symptoms of high blood pressure, consult your healthcare provider for assessment and appropriate management.
47. Frequent Hiccups

Frequent or persistent hiccups can, in rare cases, be a neurological sign of a hypertensive crisis or other serious complications of high blood pressure. When blood pressure suddenly spikes to dangerous levels, it can affect the brainstem—an area responsible for regulating involuntary reflexes, including the hiccup response. This disruption may result in hiccups that are difficult to control and last much longer than the typical brief episodes triggered by eating too quickly or consuming carbonated beverages. Unlike ordinary hiccups, which usually resolve on their own, those linked to neurological changes may persist for hours or even days.
For example, a person might experience repeated bouts of hiccups that interfere with eating, sleeping, or speaking, without any obvious dietary or situational cause. According to the American Stroke Association, persistent or intractable hiccups, especially when accompanied by other neurological symptoms like confusion, weakness, or difficulty speaking, could indicate a stroke or hypertensive emergency. If you or someone you know develops ongoing hiccups that do not go away or are associated with other signs of high blood pressure or nervous system changes, seek prompt medical evaluation to rule out serious underlying issues.
48. Changes in Mood or Personality
Changes in mood or personality can sometimes be linked to high blood pressure, especially when it is uncontrolled and begins to affect the brain’s blood flow and chemistry. Chronic hypertension can reduce the delivery of oxygen and nutrients to the brain, leading to subtle but significant changes in mental and emotional well-being. This may manifest as increased irritability, anxiety, depression, or unexpected outbursts of anger. These mood shifts differ from those caused by situational stress or normal life fluctuations, as they tend to be persistent and may not have an obvious external trigger.
For example, a person who is usually calm and easygoing may become easily frustrated, withdrawn, or unusually sad over minor issues, surprising themselves and others. According to the Alzheimer’s Association, ongoing changes in mood or personality—especially when accompanied by memory problems, confusion, or other symptoms of high blood pressure—could signal underlying neurological changes, such as vascular dementia or reduced brain function from chronic hypertension. If you or a loved one notices persistent or unexplained emotional changes, it’s important to seek a medical evaluation to address both blood pressure and mental health concerns.
49. Tingling or Burning Sensations

Tingling or burning sensations, known as paresthesia, can sometimes develop as a result of high blood pressure affecting the nerves. Chronic hypertension can damage the blood vessels that supply nerves, leading to decreased oxygen and nutrient delivery. This may cause nerves to misfire, resulting in abnormal sensations such as tingling, prickling, or burning—most commonly in the hands, feet, or legs. While occasional numbness may result from sitting awkwardly or temporary pressure on a nerve, hypertension-related paresthesia tends to be more persistent and may occur without any clear physical cause.
For example, someone might notice a constant tingling in their feet or a burning sensation in their hands that does not improve with movement or changes in position. According to the American Heart Association, these symptoms can be similar to those seen in other neuropathies, such as diabetic or vitamin deficiency-related nerve damage, but may also signal compromised circulation from high blood pressure. If you experience ongoing or worsening tingling or burning sensations—especially with other symptoms of hypertension—it’s important to report them to your healthcare provider for evaluation and appropriate management.
50. Unexplained Falls

Unexplained falls can be a serious consequence of high blood pressure, particularly when hypertension leads to dizziness, balance problems, or fainting spells. Elevated blood pressure can cause fluctuations in blood flow to the brain, resulting in lightheadedness, blurred vision, or sudden loss of balance. These effects increase the risk of stumbling or falling, even during routine activities. Unlike falls that are clearly caused by tripping or environmental hazards, hypertension-related falls may occur without warning and can be recurrent or difficult to explain.
For example, an individual might suddenly lose their balance and fall while standing up from a chair or walking across a familiar room, despite no obvious obstacle or reason. According to the Centers for Disease Control and Prevention (CDC), recurrent or unexplained falls, especially when accompanied by dizziness, weakness, or confusion, should prompt immediate medical evaluation. These incidents may signal underlying cardiovascular or neurological issues related to high blood pressure, such as orthostatic hypotension, arrhythmias, or mini-strokes. Addressing these symptoms early can help prevent injuries and improve long-term health outcomes for those with hypertension.
Conclusion

Recognizing the subtle and overt symptoms of rising blood pressure is crucial for protecting your heart, brain, and overall health. Because hypertension often develops silently, regular screening and self-monitoring are vital—even if you feel well. Early detection allows for timely intervention, reducing the risk of life-threatening complications such as stroke, heart attack, and kidney disease. Adopt practical steps, including maintaining a balanced diet, exercising regularly, managing stress, and following your healthcare provider’s advice. For more on prevention and management, visit the CDC’s guide to high blood pressure. Stay proactive about your health and encourage loved ones to do the same for a longer, healthier life.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





