Early Symptoms of Type 2 Diabetes You Shouldn’t Miss
Type 2 diabetes is one of the most common chronic health conditions worldwide, and its early signs often go unnoticed. Unlike other illnesses with sudden, dramatic symptoms, type 2 diabetes develops gradually. This slow progression means that many people may not realize they are affected until complications arise.
The early symptoms can be subtle, sometimes mistaken for normal signs of aging or everyday fatigue. Recognizing these signs early is crucial—prompt attention can help you manage the condition, prevent serious complications, and improve your long-term health.
Understanding what to look for is the first step in safeguarding your well-being.
1. Increased Thirst (Polydipsia)
One of the most recognizable early symptoms of type 2 diabetes is increased thirst, or polydipsia. This symptom arises when high blood sugar levels overwhelm the kidneys’ ability to filter and reabsorb glucose efficiently. As excess glucose is excreted in urine, the body loses more fluids, leading to dehydration. Your body responds by signaling you to drink more water to replenish lost fluids.
While everyone feels thirsty from time to time—after exercise, during hot weather, or following a salty meal—the thirst associated with diabetes is persistent and often unquenchable. This is not just a fleeting urge for a glass of water. You might find yourself needing to drink much more than usual and still not feeling satisfied, even waking up at night to drink.
If you notice that you’re constantly reaching for water, especially when accompanied by other symptoms, it’s important to pay attention. The American Diabetes Association provides valuable resources for understanding and managing type 2 diabetes and its warning signs. Early recognition of polydipsia can prompt timely testing and intervention, helping you regain control of your health before complications develop.
2. Frequent Urination (Polyuria)

Another common early symptom of type 2 diabetes is frequent urination, or polyuria. When blood sugar levels are elevated, the kidneys work overtime to filter and remove the excess glucose. As a result, more water is drawn from your bloodstream to dilute and excrete the sugar, leading to increased urine production.
Unlike occasional increases in urination caused by drinking large amounts of fluid or consuming caffeine, polyuria is persistent and often disrupts daily life. Many people notice they have to urinate much more frequently, including several times during the night—a condition known as nocturia. This repeated interruption to sleep can leave you feeling tired and unrested.
It’s important to distinguish between normal fluctuations in bathroom habits and the more constant, urgent need to urinate that can signal an underlying health problem. If you find yourself waking up multiple times each night or needing to use the restroom far more often than usual, it may be time to consult a healthcare provider.
For more information on this symptom and how it relates to diabetes, visit the Centers for Disease Control and Prevention: Diabetes Symptoms.
3. Unexplained Weight Loss

An early warning sign that often surprises people is unexplained weight loss, especially when it occurs despite eating as much or even more than usual. In type 2 diabetes, the body’s cells are unable to effectively use glucose for energy due to insulin resistance. As a result, the body starts breaking down fat and muscle for fuel, leading to noticeable weight loss.
This type of weight loss is different from healthy, intentional weight reduction through diet or exercise. If you’re eating normally and still losing weight rapidly—sometimes 10 pounds or more in just a few months—it could be a sign of an underlying issue. Unlike typical dieting or exercise-related weight changes, this loss is unintentional and can happen quickly.
While other medical conditions, such as hyperthyroidism or certain cancers, can also cause sudden weight loss, diabetes is a common culprit that is often overlooked. It’s important to recognize when weight loss cannot be explained by changes in lifestyle or eating habits.
If you experience unexplained weight changes, it’s wise to consult your healthcare provider. The Mayo Clinic offers additional information on diabetes symptoms and what to watch for.
4. Extreme Hunger (Polyphagia)

A persistent, excessive hunger—known as polyphagia—is another early indicator of type 2 diabetes. This symptom develops because, despite high levels of glucose in the blood, your body’s cells are unable to absorb and use that glucose for energy. As a result, your brain perceives a lack of fuel, triggering repeated hunger signals even shortly after eating.
Unlike the hunger you might experience from skipping meals, fasting, or following a calorie-restricted diet, polyphagia is relentless and difficult to satisfy. You may notice that, no matter how much you eat, your appetite remains unusually strong. This sensation can be confusing and frustrating, especially if it’s accompanied by other changes, such as weight loss or increased thirst.
If you find yourself constantly reaching for snacks or feeling ravenous soon after a meal, it’s important to consider whether there could be an underlying health issue. Persistent hunger, especially when paired with other diabetes symptoms, should not be ignored.
For more information on the causes and implications of polyphagia, visit the Cleveland Clinic: Polyphagia or consult a healthcare professional for personalized advice.
5. Fatigue and Weakness

One of the most common early symptoms of type 2 diabetes is persistent fatigue and weakness. This isn’t just the usual tiredness caused by a busy schedule or a late night; it’s a deep, ongoing exhaustion that doesn’t improve with rest. When your body can’t effectively use glucose for energy, your cells are deprived of their primary fuel source, leading to a constant feeling of low energy.
Fatigue related to type 2 diabetes often interferes with daily activities. You may find it hard to concentrate, struggle to get through your usual routines, or feel unusually weak even after a full night’s sleep. Unlike normal tiredness from a hectic day, diabetes-related fatigue lingers and can become overwhelming.
This symptom is especially concerning when it appears alongside other warning signs like increased thirst or frequent urination. If you’re experiencing unexplained, relentless fatigue, it’s worth discussing with your doctor.
For more insight into why diabetes causes chronic tiredness and how to manage it, explore the research on Diabetes Fatigue from Diabetes.co.uk, which provides helpful information and support.
6. Blurred Vision
Blurred vision can be one of the earliest and most unsettling signs of type 2 diabetes. Elevated blood sugar levels cause fluid to be pulled into and out of the lenses of your eyes, resulting in swelling. This swelling temporarily changes the shape and flexibility of the lens, making it difficult for your eyes to focus properly. The result is vision that becomes blurry or fuzzy, even if you’ve never needed glasses before.
Unlike the gradual vision changes associated with aging or common eye conditions like astigmatism or presbyopia, diabetes-induced blurred vision can come on suddenly and may fluctuate with your blood sugar levels. Sometimes, vision may clear up only to become blurry again later in the day or after meals.
If you notice abrupt or recurring changes in your eyesight—such as trouble reading, difficulty seeing distant objects, or a feeling that your vision is “off”—it’s important to seek medical advice. Eye issues related to diabetes are usually temporary in the early stages, but if left untreated, they can progress to more serious complications.
For more details, the American Academy of Ophthalmology offers comprehensive information on how diabetes can affect your eyes.
7. Slow-Healing Sores or Cuts

A lesser-known but significant early symptom of type 2 diabetes is the presence of sores or cuts that heal slowly. Elevated blood sugar levels can damage blood vessels, leading to poor circulation, especially in the extremities such as the feet and legs. When circulation is impaired, it becomes more difficult for oxygen and nutrients to reach wounds, delaying the healing process.
Additionally, high glucose levels weaken the immune system’s ability to respond to injuries and fight infections. This double impact means that even minor scrapes or blisters can linger for weeks or become easily infected. Common sites for slow-healing wounds include the feet, ankles, and lower legs—areas where blood flow is naturally reduced.
You might notice that a small cut on your foot doesn’t close up, or a blister from new shoes becomes red and swollen rather than improving. These seemingly minor issues can escalate if not properly managed. Paying close attention to how quickly your body recovers from everyday injuries can provide valuable clues about your health.
For more information on diabetic wound care and prevention, visit the American Podiatric Medical Association: Diabetes and Foot Care.
8. Frequent Infections

Type 2 diabetes often leads to a higher risk of infections due to a compromised immune system. Elevated blood sugar weakens the body’s natural defenses, making it easier for bacteria and fungi to thrive. As a result, people with diabetes are more prone to frequent infections, especially in areas like the urinary tract, skin, and gums.
Urinary tract infections (UTIs) are particularly common and may recur more often than in individuals without diabetes. Skin infections, such as boils, fungal rashes, or persistent athlete’s foot, also tend to occur more frequently and can be harder to treat. In contrast, those without diabetes typically experience infections less often and recover more quickly.
It’s important to pay attention if you notice that you’re getting sick more frequently than usual or if minor infections seem unusually severe or slow to resolve. These recurring illnesses can sometimes be the first sign that something is wrong with your body’s ability to fight off germs.
For a deeper understanding of how diabetes affects infection risk and what you can do about it, visit the CDC’s resource on diabetes and infections.
9. Tingling or Numbness in Hands and Feet (Neuropathy)

A subtle but serious early symptom of type 2 diabetes is tingling, numbness, or pain in the hands and feet. This sensation, known as peripheral neuropathy, occurs when elevated blood sugar damages the small nerves, especially those in the extremities. Over time, nerve fibers become less able to transmit signals, resulting in sensations that can range from mild tingling to sharp, burning pain or persistent numbness.
This differs from the temporary numbness you might feel after sitting in one position for too long or sleeping on your arm. With diabetic neuropathy, the symptoms often start gradually and worsen over time. You may notice that your feet or fingers feel “asleep,” tingle for no apparent reason, or become unusually sensitive to touch.
Ignoring these warning signs can lead to more severe nerve damage and, in some cases, loss of sensation, which increases the risk of unnoticed injuries. Prompt recognition and management are essential for protecting nerve health.
For further reading on diabetes-related nerve damage and tips for prevention, refer to the National Institute of Diabetes and Digestive and Kidney Diseases: Diabetic Neuropathies.
10. Darkened Skin Patches (Acanthosis Nigricans)

One of the more visible early signs of type 2 diabetes is the appearance of darkened, velvety patches of skin, a condition known as acanthosis nigricans. This skin change is closely linked to insulin resistance, which is a hallmark of type 2 diabetes. When insulin levels are elevated, skin cells may reproduce more rapidly, causing thickened, hyperpigmented areas.
Acanthosis nigricans most commonly appears in body folds where skin rubs together, such as the neck, armpits, groin, and sometimes the elbows or knees. The affected skin may feel soft or velvety to the touch and can vary in color from light brown to nearly black. These patches are usually not itchy or painful, but their sudden appearance or spread can be concerning.
While acanthosis nigricans can sometimes be associated with other medical conditions or obesity, its presence is often a warning sign of underlying insulin resistance. If you notice these skin changes, particularly in the areas mentioned, it’s a good idea to consult your healthcare provider.
For more information about this condition and its relationship with diabetes, see the American Academy of Dermatology: Acanthosis Nigricans.
11. Itchy Skin

Persistent itchy skin can be an early sign of type 2 diabetes, often resulting from a combination of dryness and reduced blood circulation. When blood sugar levels are high, the body loses more fluids, especially through frequent urination, which can leave the skin parched and prone to irritation. Poor circulation, particularly in the lower legs and feet, further contributes to dryness and itching by limiting the delivery of moisture and nutrients to the skin.
Unlike itching caused by allergies, bug bites, or eczema, diabetes-related itching tends to be widespread or focused on the lower extremities. Sometimes, small patches of skin may become red, flaky, or even develop minor cracks.
To manage itchy skin, keep the affected areas moisturized with fragrance-free lotions and avoid hot showers, which can worsen dryness. Wearing loose, breathable clothing and using a humidifier in dry environments may also help. If itching persists or is accompanied by other symptoms like slow-healing sores, it’s important to seek medical advice.
For more tips on managing dry, itchy skin with diabetes, visit the American Diabetes Association: Skin Complications.
12. Recurrent Yeast Infections
Frequent or recurrent yeast infections are another early symptom that may signal type 2 diabetes. High blood sugar levels create an environment where yeast, particularly Candida species, can thrive. Glucose serves as a food source for yeast, so when it’s abundant in the body’s tissues and fluids, infections can occur more often and be harder to eliminate.
Both women and men can experience these infections. For women, vaginal yeast infections may cause itching, burning, redness, and a thick, white discharge. Men can develop infections around the genital area, leading to redness, soreness, and itching. Yeast can also affect other warm, moist areas of the body, such as under the breasts, between fingers and toes, or in skin folds.
While yeast infections are common and can result from antibiotics, hormonal changes, or other health conditions, recurring or stubborn infections may warrant further investigation. If you find yourself dealing with repeated bouts of itching, irritation, or discharge, it’s important to discuss this with your healthcare provider.
For more information, the CDC’s overview of genital candidiasis offers helpful insight into causes, symptoms, and treatment options.
13. Gum Disease and Dental Problems

Type 2 diabetes not only affects your body’s ability to manage blood sugar but also increases your risk of gum disease and dental problems. Elevated glucose levels in the saliva create a breeding ground for harmful bacteria, leading to gum infections such as gingivitis and periodontitis. Symptoms may include red, swollen gums that bleed easily, persistent bad breath, and even loose teeth.
People with diabetes are more likely to develop dental issues compared to those with normal blood sugar levels. Poor blood flow and a reduced immune response make it harder for the gums to heal and fight off infection. As a result, minor gum irritation can quickly escalate into more serious dental complications if not addressed promptly.
Practicing good oral hygiene is crucial. Brush your teeth at least twice a day, floss daily, and schedule regular dental check-ups. If you notice bleeding gums, mouth sores, or changes in your bite, consult your dentist sooner rather than later.
For more guidance on oral health and diabetes, visit the American Dental Association: Diabetes and Oral Health for tips on prevention and care.
14. Increased Hunger After Eating

A unique and often confusing symptom of type 2 diabetes is increased hunger immediately after eating. Normally, eating a balanced meal leads to feelings of fullness and satisfaction as glucose enters your cells and provides energy. However, in diabetes, insulin resistance prevents glucose from moving efficiently into cells, leaving your body’s tissues “starved” even though your stomach is physically full.
This persistent hunger is not the same as the mild craving you might feel after a light meal or snack. Instead, it’s an intense, ongoing urge to eat, even if you’ve just finished a hearty meal. This can lead to overeating, unwanted weight gain, and further destabilization of blood sugar levels. You might notice that your hunger doesn’t subside after meals, or that you quickly become hungry again, prompting you to eat more frequently.
If you find yourself experiencing this cycle of eating without true satiety, it could be a sign of an underlying issue with blood sugar control. Addressing both diet and underlying metabolic health is key.
For further reading on post-meal hunger and diabetes, check out the Diabetes UK guide to eating with diabetes.
15. Headaches
Frequent or persistent headaches can be an early warning sign of type 2 diabetes, often linked to fluctuating blood sugar levels. When glucose levels rise or fall rapidly, the brain may not receive a steady supply of energy, which can trigger headaches. These may feel like a dull, throbbing pain or a more intense, pressure-like discomfort and often occur alongside other diabetes symptoms such as fatigue or blurred vision.
Unlike headaches caused by dehydration, lack of sleep, tension, or sinus issues, diabetes-related headaches are more likely to coincide with periods of blood sugar instability. They may occur after meals, during periods of fasting, or when your body is struggling to regulate glucose properly.
To help manage these headaches, focus on maintaining stable blood sugar levels through regular meals, balanced nutrition, and staying hydrated. Tracking your blood sugar and headache patterns can also offer insights into triggers and help your healthcare provider adjust your treatment plan if needed.
For detailed strategies on managing headaches related to diabetes, visit the Diabetes.co.uk: Headaches and Diabetes for practical advice and support.
16. Mood Changes and Irritability

Mood swings and irritability are often overlooked symptoms of type 2 diabetes but can be among the earliest to appear. Unstable blood sugar levels directly affect brain chemistry and emotional regulation, making you more prone to sudden changes in mood. You might notice feeling uncharacteristically impatient, angry, or easily upset, even in situations that wouldn’t normally bother you.
These mood changes are different from those caused by stress, lack of sleep, or external pressures. In diabetes, irritability can arise seemingly out of nowhere or fluctuate throughout the day, often coinciding with periods of high or low blood sugar. Chronic instability in glucose levels may also contribute to feelings of sadness or even depression, making everyday life more challenging.
If you find yourself experiencing frequent mood swings or unexplained irritability, it’s important to consider your overall health. Addressing blood sugar control through healthy eating, regular exercise, and medical guidance can help stabilize your mood.
For more on the link between diabetes and mental health, visit The American Diabetes Association: Diabetes and Mental Health for support and resources.
17. Vision Fluctuations

In addition to chronic blurred vision, some people with early type 2 diabetes experience episodes of rapidly changing vision quality. These vision fluctuations are a result of unstable blood sugar levels causing shifts in fluid balance within the eyes. As glucose rises and falls, the amount of fluid in the lens changes, which can temporarily alter your ability to focus.
You may notice that your vision is sharp at certain times of the day but suddenly becomes blurry, then clears up again. This is different from age-related vision changes or conditions like astigmatism, which remain fairly constant. Diabetes-related fluctuations can affect both distance and close-up vision, making it difficult to read, drive, or perform daily tasks reliably.
The good news is that these changes are often reversible when blood sugar levels are brought under control. Vision typically stabilizes once glucose returns to a healthy range, although it may take a few weeks for the eyes to fully adjust.
If you experience unpredictable vision changes, it’s important to have your blood sugar and eye health evaluated. For more on diabetes and temporary vision changes, refer to the American Diabetes Association: Eye Complications.
18. Frequent Colds or Flus

A weakened immune system is a lesser-known but important early sign of type 2 diabetes, often resulting in frequent colds or flus. High blood sugar impairs the function of white blood cells, which are essential for fighting off viruses and bacteria. As a result, people with diabetes may notice they catch respiratory infections more often and take longer to recover.
While catching a cold or flu occasionally is normal, especially during certain seasons, experiencing these infections repeatedly or with greater severity can signal an underlying issue. For someone without diabetes, getting sick a few times a year is typical, but if you find yourself battling viral illnesses far more often, it’s worth considering your body’s immune health.
This susceptibility to infection can also mean that minor illnesses linger longer or develop into more serious complications, such as bronchitis or pneumonia. Taking steps to control blood sugar can help restore immune function and reduce the frequency of illness.
For further information, the CDC’s Sick Day Toolkit for People with Diabetes offers helpful advice on managing illness and supporting your immune system.
19. Dry Mouth

Persistent dry mouth, or xerostomia, is another early symptom of type 2 diabetes that often goes unrecognized. High blood sugar draws fluids from tissues throughout the body, including the mouth, resulting in a dry, sticky sensation that doesn’t go away with normal hydration. This symptom is more than just feeling thirsty after physical activity or a salty meal—it’s a constant dryness that lingers even after drinking water.
Dry mouth can make it difficult to chew, swallow, or even speak comfortably. In addition to discomfort, it also increases the risk of dental issues. Saliva plays a vital role in neutralizing acids, washing away food particles, and protecting the teeth from decay. When saliva production decreases, your mouth becomes more susceptible to cavities, gum disease, and oral infections.
If you notice that your mouth feels unusually dry, especially alongside other symptoms of diabetes, it’s important to address it promptly. Drinking plenty of water, chewing sugar-free gum, and practicing good oral hygiene can help manage dry mouth.
For more on this topic, see the American Dental Association’s guide to diabetes and oral health, which offers additional tips and resources.
20. Fruity-Smelling Breath

A distinctive, fruity or acetone-like odor on the breath can be an early and sometimes alarming symptom of type 2 diabetes. This occurs when the body, unable to use glucose for energy, begins breaking down fat instead, resulting in the production of chemicals called ketones. Excess ketones are released in the urine and breath, creating the telltale sweet or fruity scent.
This type of breath odor is different from morning breath or the result of eating certain foods like garlic or onions. Instead, it’s persistent and can be noticed by others. While mild ketone buildup can happen in early or uncontrolled diabetes, a strong fruity breath may signal a more serious condition called diabetic ketoacidosis (DKA), which is rare but can be life-threatening and requires immediate medical attention.
If you or someone you know experiences this symptom, especially alongside nausea, vomiting, confusion, or rapid breathing, seek urgent care. Early recognition of fruity-smelling breath can help prevent dangerous complications.
For more on ketones and diabetes, visit the American Diabetes Association: Ketoacidosis and Ketones to learn about risks and when to seek help.
21. Erectile Dysfunction

One of the early and often distressing symptoms of type 2 diabetes in men is erectile dysfunction (ED). Diabetes can cause damage to both nerves and blood vessels, which are crucial for achieving and maintaining an erection. Persistently high blood sugar levels impair blood flow and nerve signaling in the genital area, making ED more common and sometimes more challenging to treat.
Studies estimate that between 35% and 75% of men with diabetes will experience some degree of erectile dysfunction during their lifetime, with symptoms often appearing several years before a diabetes diagnosis. This rate is much higher than in men of the same age without diabetes, making it a significant warning sign.
Unlike occasional issues with performance that may be linked to stress, fatigue, or relationship concerns, diabetes-related ED tends to be persistent and progressive. If you notice ongoing difficulty with erections, it’s important to address not only the symptom but also the underlying health factors.
For more information about diabetes and sexual health, visit the American Diabetes Association: Sexual Health for Men for guidance, support, and treatment options.
22. Loss of Interest in Sex (Low Libido)

A loss of interest in sex, or low libido, can be an early but often overlooked symptom of type 2 diabetes for people of all genders. This decline in sexual desire is influenced by a combination of hormonal imbalances, psychological stress, and physical changes linked to diabetes. Fluctuating blood sugar levels can disrupt the balance of sex hormones like estrogen and testosterone, diminishing arousal and sexual interest.
Additionally, diabetes can contribute to fatigue, depression, anxiety, and poor self-image, all of which may lower libido. Physical symptoms such as nerve damage or poor circulation may also result in reduced sensitivity or discomfort during sexual activity, further impacting desire.
Unlike the temporary dips in libido caused by relationship stress or life changes, diabetes-related low sex drive tends to persist or worsen over time if blood sugar remains uncontrolled. Addressing this symptom often involves both medical and emotional support, as well as improved diabetes management.
For more about sexual health and diabetes in all genders, visit the American Diabetes Association: Sexual Health for Women and their resources for people of all genders.
23. Persistent Nausea

Ongoing or persistent nausea can be an early and confusing symptom of type 2 diabetes, often mistaken for a stomach virus or a gastrointestinal issue. Blood sugar imbalances—whether too high or too low—can disrupt the normal functioning of your digestive system, leading to sensations of queasiness or discomfort that may not improve with typical remedies.
High blood sugar can slow stomach emptying, a condition known as gastroparesis, which results in bloating, nausea, and sometimes vomiting. Conversely, rapid drops in blood sugar can also trigger nausea as the body reacts to the imbalance. Unlike occasional stomach upset from food, stress, or infection, diabetes-related nausea tends to be more persistent and may coincide with other symptoms like fatigue, excessive thirst, or frequent urination.
If you experience ongoing nausea without an obvious cause, especially if it’s accompanied by other possible diabetes symptoms, it’s important to get evaluated by a healthcare provider.
For more on how diabetes can affect the digestive system and lead to symptoms like nausea, visit the Cleveland Clinic: Gastroparesis and Diabetes for expert guidance and management tips.
24. Dizziness or Lightheadedness

Episodes of dizziness or lightheadedness can be a subtle but important early symptom of type 2 diabetes. These sensations often result from rapid changes in blood sugar levels, which can impair the brain’s access to a steady supply of energy. You may notice dizziness particularly after standing up quickly, skipping meals, or during periods of physical exertion.
When blood sugar drops too low (hypoglycemia) or spikes too high (hyperglycemia), the body and brain may not receive enough glucose to function optimally, leading to feelings of faintness or instability. Unlike occasional dizziness from dehydration or standing up too fast, diabetes-related dizziness tends to recur, especially when eating patterns or blood sugar management are inconsistent.
If dizziness is persistent or frequently occurs alongside other symptoms such as fatigue, blurred vision, or excessive thirst, it’s important to consider blood sugar fluctuations as a potential cause. Monitoring your symptoms and maintaining regular, balanced meals can help minimize these episodes.
For more information about dizziness and diabetes, visit the Diabetes.co.uk: Dizziness and Diabetes for practical advice on prevention and management.
25. Muscle Cramps

Frequent or severe muscle cramps, especially at night, can be an early indication of type 2 diabetes. These cramps occur when electrolyte imbalances and poor circulation—both common in uncontrolled diabetes—interfere with normal muscle function. High blood sugar can alter fluid balance and lead to losses of important minerals like potassium, magnesium, and calcium, all of which are essential for proper muscle contraction and relaxation.
You might notice sudden, painful tightening of muscles in your legs, calves, or feet while resting or sleeping. Unlike the occasional cramp from overexertion or dehydration, diabetes-related cramps may become more frequent and harder to relieve. Poor circulation due to damaged blood vessels can further reduce the delivery of oxygen and nutrients to muscle tissue, compounding the risk of cramping.
Addressing muscle cramps involves maintaining good hydration, managing blood sugar, and ensuring a balanced intake of electrolytes. Gentle stretching before bed and regular physical activity can also help improve circulation and reduce cramp frequency.
For additional information, visit the Diabetes.co.uk: Muscle Cramps and Diabetes to learn more about prevention and relief strategies.
26. Frequent Skin Infections

Type 2 diabetes can make you more susceptible to frequent skin infections, often caused by bacteria or fungi. Elevated blood sugar creates an environment where these microorganisms can flourish, leading to infections that may be more intense, stubborn, or recurrent than typical skin rashes or irritations. Common bacterial infections include boils, styes, and infected hair follicles, while fungal infections often appear as itchy, red patches in warm, moist areas such as under the breasts, between fingers and toes, or in the groin.
Unlike occasional rashes from allergies or contact irritants, diabetes-related skin infections may take longer to resolve and can quickly worsen if not treated. Signs to watch for include swelling, redness, warmth, pus, or a rash that spreads. Infections can also recur in the same spot or appear in multiple places at once.
Keeping your blood sugar in check, practicing good hygiene, and treating minor wounds promptly can help reduce the risk of skin infections. If you notice that skin problems are becoming a regular issue, consult a healthcare provider for evaluation and tailored advice.
To learn more, visit the American Academy of Dermatology: Diabetes and Skin Problems.
27. Unintentional Bedwetting (in Adults)

Unintentional bedwetting in adults, or nocturnal enuresis, is an unusual but important symptom that can sometimes point to undiagnosed type 2 diabetes. This issue is closely linked to polyuria—excessive urination due to high blood sugar levels. When the kidneys are overwhelmed by glucose, they produce more urine in an effort to flush out the excess. At night, this can lead to episodes where adults who previously had no issues with bladder control may unexpectedly wet the bed.
Unlike childhood bedwetting or occasional nighttime accidents caused by alcohol or certain medications, diabetes-related bedwetting tends to develop suddenly and may recur frequently. It often accompanies other symptoms like increased thirst, frequent urination during the day, or unexplained fatigue.
If you or a loved one begins to experience new-onset bedwetting as an adult, especially alongside other signs of type 2 diabetes, it’s crucial to seek medical evaluation. Identifying this symptom early can help prompt the necessary testing and interventions to manage blood sugar and prevent further complications.
For additional insights and support, visit the National Institute of Diabetes and Digestive and Kidney Diseases: Adult Bedwetting.
28. Swollen or Red Gums

Swollen or red gums are among the earliest oral health changes that can signal type 2 diabetes. Elevated blood sugar provides an ideal environment for bacteria to grow along the gumline, increasing the risk of inflammation, infection, and bleeding. You may notice that your gums appear puffy, feel tender to the touch, or bleed easily when brushing or flossing—even if you maintain regular oral hygiene.
Unlike mild gum irritation from temporary causes, such as eating rough foods or brushing too hard, diabetes-related gum inflammation tends to persist and worsen if blood sugar remains uncontrolled. Poor immune response further complicates the body’s ability to fight off infection, raising the risk of gingivitis and more advanced periodontal disease.
Early intervention is key. Practicing good oral care—brushing twice daily with a soft-bristled toothbrush, flossing regularly, and visiting your dentist—can help manage gum health and reduce complications. If swelling, redness, or bleeding gums persist, it’s important to discuss these symptoms with both your dentist and healthcare provider.
For more on gum health and diabetes, explore the CDC’s guide to diabetes and oral health.
29. Delayed Growth in Children or Adolescents

While type 2 diabetes is more common in adults, cases among children and adolescents are rising. One subtle but concerning symptom in this age group is delayed growth or slowed development. When blood sugar remains elevated for extended periods, the body’s ability to use nutrients efficiently is impaired. This can disrupt the hormones responsible for growth and puberty, ultimately slowing down height and weight gain or delaying the onset of puberty.
Parents may notice their child is not keeping up with peers in height, weight, or developmental milestones. Unlike temporary slowdowns caused by illness or genetics, diabetes-related growth delays persist and may be accompanied by other signs, such as increased thirst, frequent urination, or unexplained fatigue.
Early intervention is essential for supporting healthy growth and preventing complications. If a child or teen shows signs of stunted growth along with other possible symptoms of diabetes, prompt medical evaluation is recommended.
For additional information about diabetes in young people and its effects on growth, visit the CDC’s resource on diabetes in children and teens.
30. Dark Rings Around the Eyes

Dark rings around the eyes, also known as periorbital dark circles, can sometimes be an indirect sign of type 2 diabetes. While these dark circles are frequently attributed to fatigue, genetics, or lack of sleep, they may also develop due to dehydration and poor circulation associated with elevated blood sugar. When the body is persistently dehydrated, blood vessels beneath the thin skin around the eyes become more prominent, leading to a shadowed or discolored appearance.
In people with diabetes, poor circulation can further exacerbate this effect, preventing adequate delivery of oxygen and nutrients to delicate skin tissue. The result is a tired, sunken look that’s not easily remedied by extra rest or topical creams.
While dark rings around the eyes are not exclusive to diabetes, their sudden appearance—especially when paired with other symptoms like dry mouth, increased thirst, or frequent urination—may warrant further investigation.
If you notice persistent or worsening dark circles, consider discussing them with your healthcare provider. For more on skin changes and diabetes, visit the American Diabetes Association: Skin Complications for useful tips and resources.
31. Increased Susceptibility to Bruising

Increased susceptibility to bruising is an often-overlooked symptom that can occur in people with type 2 diabetes. High blood sugar over time can weaken blood vessel walls and impair normal clotting mechanisms, making it easier for small bumps or minor injuries to cause visible bruises. These bruises may appear more often and take longer to heal than usual, especially on the arms, legs, or other areas prone to minor trauma.
Unlike bruising from blood thinners, aging, or vitamin deficiencies, diabetes-related bruising is more closely tied to chronic changes in blood vessels and reduced circulation. The skin may also become thinner and more fragile, compounding the issue. If you notice frequent or unexplained bruises, especially in combination with slow-healing wounds or other signs of poor circulation, it’s important to bring this up with your healthcare provider.
Keeping your blood sugar within target ranges and protecting your skin from unnecessary trauma can help minimize bruising. For more information on circulatory and skin complications in diabetes, visit the CDC’s resource on skin care and diabetes.
32. Restless Leg Syndrome

Restless Leg Syndrome (RLS) is a neurological condition that can be more common in people with type 2 diabetes. RLS is characterized by an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations such as tingling, crawling, or itching, especially during periods of rest or at night. The connection between diabetes and RLS lies largely in the impact of high blood sugar on nerve health. Over time, diabetes can damage peripheral nerves, leading to symptoms similar to those found in RLS.
This condition can significantly interfere with sleep, leading to daytime fatigue and worsening overall quality of life. Unlike occasional leg discomfort from exercise or sitting too long, RLS is persistent, and symptoms tend to intensify in the evening or when lying down.
Managing blood sugar and addressing nerve health through regular check-ups, physical activity, and appropriate medications can help reduce RLS symptoms. If you experience persistent urges to move your legs or nightly restlessness, discuss these symptoms with your healthcare provider for a tailored approach.
For more on the link between diabetes and restless leg syndrome, visit the Sleep Foundation: Restless Leg Syndrome and Diabetes.
33. High Blood Pressure
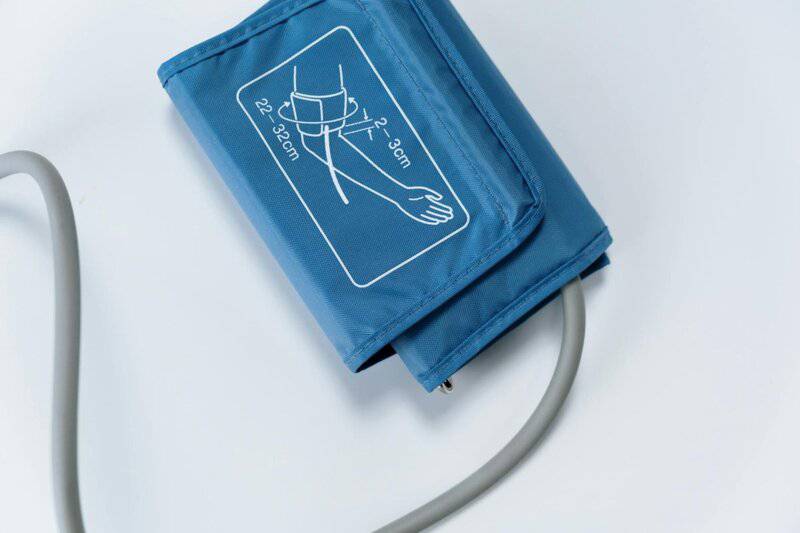
High blood pressure (hypertension) commonly coexists with type 2 diabetes, and its presence can sometimes serve as an early warning sign. Both conditions share risk factors such as obesity, sedentary lifestyle, and poor dietary habits, and they often develop together as part of metabolic syndrome. Elevated blood sugar and insulin resistance can damage blood vessel walls, making them less elastic and more prone to increased pressure.
Hypertension may go unnoticed without regular monitoring, as it rarely causes symptoms in its early stages. However, when paired with other subtle signs of type 2 diabetes—like fatigue, increased thirst, or frequent urination—it becomes a critical clue for early detection. High blood pressure further raises the risk of complications from diabetes, including heart disease, stroke, and kidney damage.
If you have a history of hypertension or your blood pressure readings are consistently above normal, it’s wise to have your blood sugar checked as well. Managing both conditions through lifestyle changes, medication, and regular check-ups greatly improves long-term health outcomes.
For more on the connection between diabetes and hypertension, see the American Heart Association: Diabetes and High Blood Pressure.
34. Loss of Coordination or Balance

A less obvious but concerning symptom of type 2 diabetes is a loss of coordination or balance. Chronic high blood sugar levels can lead to diabetic neuropathy, which impairs nerve communication between the brain, muscles, and limbs. As sensation in the feet and legs diminishes and muscle strength weakens, you may notice increasing unsteadiness, difficulty walking, or even frequent tripping and falls.
Unlike occasional clumsiness that follows fatigue or distraction, diabetes-related loss of balance is persistent and may worsen over time. You might feel unsure on your feet, have trouble navigating stairs or uneven surfaces, or experience a “rubbery” sensation in your legs. This is particularly concerning for older adults, as falls can result in serious injuries.
If you or a loved one begins to notice a decline in coordination, it’s important to discuss these changes with a healthcare provider. Early intervention—through physical therapy, blood sugar management, and fall prevention strategies—can help reduce risks and improve mobility.
For more information, visit the American Diabetes Association: Nerve Damage (Neuropathy) for guidance on symptoms and support.
35. Reduced Sense of Smell and Taste

A reduced sense of smell and taste is a lesser-known but possible early symptom of type 2 diabetes. High blood sugar levels can affect the delicate nerves responsible for transmitting sensory information from the nose and tongue to the brain. This neuropathy may dull your perception of flavors and aromas, making food seem bland or less enjoyable than before.
Unlike temporary changes that occur with a cold, allergies, or certain medications, diabetes-related sensory loss tends to be gradual and persistent. You may notice that favorite foods lack their usual zing, or that you have to add extra seasoning to achieve the same flavor. Even familiar scents—like coffee, flowers, or spices—might become muted or go unnoticed.
While these changes are less common than other symptoms, they can still impact quality of life and nutritional choices. If you experience a persistent reduction in your ability to taste or smell, especially alongside other signs of diabetes, it’s important to talk to your healthcare provider.
For more on nerve-related complications and sensory changes, visit the American Diabetes Association: Nerve Damage (Neuropathy).
36. Menstrual Irregularities

Menstrual irregularities can be an early and sometimes overlooked sign of type 2 diabetes in women. Insulin resistance and chronic high blood sugar can disrupt the delicate balance of hormones that regulate the menstrual cycle. This may lead to changes in the frequency, duration, or heaviness of periods. Some women may experience skipped cycles, unusually long or short cycles, or unpredictable bleeding.
Unlike occasional irregularities caused by stress, travel, or minor illness, diabetes-related menstrual changes often persist or worsen over time if blood sugar remains uncontrolled. These disruptions can also be accompanied by other symptoms of insulin resistance, such as weight gain, increased facial or body hair, and acne—especially in women with polycystic ovary syndrome (PCOS), a condition strongly linked to type 2 diabetes.
If you notice persistent changes in your cycle, it’s important to track your symptoms and discuss them with your healthcare provider. Early intervention can help restore hormonal balance, improve metabolic health, and reduce the risk of complications.
For more on reproductive health and diabetes, visit the CDC’s resource on diabetes in women.
37. Flushed Face

A flushed face, or persistent facial redness, can be a subtle sign of high blood sugar in people with type 2 diabetes. Unlike typical blushing triggered by emotion, heat, or exertion, this redness tends to linger and may appear even when you’re at rest. Elevated glucose levels can cause blood vessels near the skin’s surface to dilate, leading to a warm, reddish appearance on the cheeks, nose, or forehead.
This symptom is different from short-lived flushing after exercise or embarrassment. In diabetes, facial redness can be more pronounced and may come with other signs like dry skin, frequent urination, or increased thirst. Sometimes, the skin may feel warm to the touch, but there’s no fever or obvious cause for the change in color.
If you notice persistent facial flushing that doesn’t resolve on its own, especially when accompanied by other symptoms of high blood sugar, it’s important to speak with your healthcare provider. Early identification and proper management can help prevent further complications.
To learn more about skin changes and diabetes, visit the American Diabetes Association: Skin Complications.
38. Hearing Loss

Emerging research suggests that hearing loss may be another early symptom associated with type 2 diabetes. High blood sugar levels can damage the small blood vessels and nerves in the inner ear, much like they do elsewhere in the body. Over time, this damage may reduce the ear’s ability to transmit sound signals effectively, leading to gradual hearing impairment.
People with diabetes are twice as likely to experience hearing loss compared to those without the condition. This can manifest as difficulty understanding conversations, frequently asking others to repeat themselves, or needing to increase the volume on electronic devices. Unlike hearing loss from aging or loud noise exposure, diabetes-related changes can develop earlier and may go unnoticed until they interfere with daily life.
If you or someone you know notices a decline in hearing—especially alongside other signs of diabetes—it’s important to seek an evaluation. Early intervention and blood sugar management can help preserve hearing health and overall well-being.
For more details on the connection between diabetes and hearing loss, visit the National Institute on Deafness and Other Communication Disorders: Diabetes and Hearing Loss.
39. Increased Sweating

Increased sweating—or abnormal sweating patterns—can be an early and sometimes puzzling symptom of type 2 diabetes. Blood sugar fluctuations and nerve involvement (autonomic neuropathy) directly impact the body’s ability to regulate sweat production. This can result in excessive sweating, particularly at night (night sweats) or during periods of mild activity, even in cool environments.
Unlike normal sweating from heat, exertion, or emotional stress, diabetes-related sweating may occur without any obvious trigger. Some people experience profuse sweating on their upper body, face, or neck while their lower body remains dry. Others might notice reduced sweating in certain areas, which can make it hard to regulate body temperature.
These unusual patterns are linked to nerve damage caused by prolonged high blood sugar, which disrupts signals between the brain and sweat glands. If you notice persistent or unexplained changes in your sweating—especially alongside other symptoms of diabetes—it’s important to bring this to your healthcare provider’s attention.
For more on autonomic neuropathy and sweating in diabetes, visit the American Diabetes Association: Nerve Damage (Neuropathy) for guidance and support.
40. Persistent Mild Fevers

Persistent mild fevers—those that linger just above normal body temperature—can sometimes be an overlooked symptom in people with type 2 diabetes. Chronic low-grade fevers may result from the body’s ongoing battle with subtle infections or inflammation, both of which are more common in individuals with elevated blood sugar. The immune system’s ability to fight off bacteria, fungi, and even minor injuries is compromised, making it easier for infections to take hold and harder for them to resolve.
Unlike the high fevers associated with acute illness, diabetes-related fevers are typically mild, rarely exceeding 100-101°F (37.8-38.3°C). They may persist for days or weeks and can be accompanied by other signs of infection, such as fatigue, malaise, or localized pain. Sometimes, the source of infection may not be obvious, as it could be related to a hidden urinary tract infection, dental issue, or slow-healing sore.
If you experience recurring low-grade fevers without a clear cause—especially in combination with other symptoms of diabetes—it’s important to consult your healthcare provider.
For more insights into infections and inflammation in diabetes, see the CDC’s information on diabetes and infections.
Conclusion

Recognizing the early symptoms of type 2 diabetes can make a significant difference in your long-term health. While many of these signs can be subtle or mistaken for everyday issues, noticing several in combination should prompt a professional evaluation. Early detection and timely intervention can help you manage your blood sugar, prevent complications, and improve your overall quality of life. If you or a loved one notice multiple symptoms described in this guide, don’t hesitate to reach out to a healthcare provider. Your attention to these warning signs could be the key to a healthier future.
Disclaimer

This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with any questions or concerns about your health. Prompt medical attention can make all the difference—don’t delay seeking care if you notice concerning symptoms.





