Habits That Spike Blood Sugar at Night
Nighttime hyperglycemia affects an estimated 30% of people with diabetes, often going undetected until complications arise (Diabetes Care). The endocrine system, especially the pancreas, orchestrates blood sugar control, but its delicate balance can be disrupted by common habits after dusk. The challenge lies in the subtle or delayed symptoms, making early detection difficult (NIH). Understanding how nighttime behaviors impact glucose levels is critical for prevention and effective management of hyperglycemia during sleep.
1. Eating Large Late-Night Meals

Consuming heavy, calorie-dense meals close to bedtime can overwhelm the body’s ability to manage blood glucose effectively. When you eat a large dinner—think pasta with rich sauces, bread, desserts, and sugary drinks—the pancreas is tasked with releasing a substantial amount of insulin to process this influx of carbohydrates and sugars. At night, insulin sensitivity naturally decreases, making it harder for glucose to be cleared from the bloodstream (NIH). This scenario can lead to prolonged elevated blood sugar levels while you sleep, increasing the risk of nighttime hyperglycemia.
To mitigate this, experts recommend practicing portion control and scheduling earlier dinnertimes. Opt for smaller, balanced meals that include lean proteins, non-starchy vegetables, and whole grains, which are digested more slowly and cause less dramatic blood sugar spikes (CDC). Ideally, finish eating at least two to three hours before bedtime to allow your body sufficient time to process the meal. These strategies support the body’s natural circadian rhythm and help maintain healthier blood glucose levels overnight.
2. Snacking on High-Glycemic Foods

Indulging in snacks like white bread, sweetened cereals, candy, or cookies before bed can result in a rapid spike in blood sugar due to their high glycemic index (GI). These foods are quickly broken down into glucose, causing an immediate surge in blood sugar levels, which is especially problematic at night when the body’s insulin response is already diminished (Harvard T.H. Chan School of Public Health). This surge can not only disrupt sleep but also contribute to a cycle of elevated glucose throughout the night, increasing the risk of long-term complications.
Studies highlight that individuals who frequently consume high-GI snacks in the evening are more likely to experience nighttime hyperglycemia and poor glycemic control overall (NIH). To avoid these spikes, it is advisable to choose snacks with a low GI, such as a small handful of nuts, Greek yogurt, or vegetables with hummus. These foods are digested slowly, resulting in a steadier release of glucose and more stable overnight blood sugar levels, supporting overall metabolic health and restful sleep.
3. Drinking Sugary Beverages Before Bed

Consuming sugary beverages such as soda, fruit juice, or sweetened tea in the hours before sleep can cause significant nocturnal glucose surges. These drinks contain rapidly absorbed simple sugars that flood the bloodstream, leading to a sharp increase in blood sugar levels. Unlike solid foods, liquids are digested even faster, which means glucose enters the bloodstream almost immediately after consumption (CDC). This rapid spike is especially concerning at night, when insulin sensitivity is reduced and the body is less able to compensate for high glucose, increasing the risk for nighttime hyperglycemia.
In contrast, choosing water or unsweetened herbal teas has no impact on blood sugar levels and supports hydration without adding extra calories or sugar. Water is essential for proper metabolic function, while herbal teas like chamomile or peppermint can promote relaxation and better sleep without affecting glucose (Sleep Foundation). To reduce your risk of nocturnal glucose spikes, swap sugary drinks for these healthier alternatives, particularly in the evening. Making this switch can greatly support stable overnight blood sugar and overall metabolic health.
4. Skipping Dinner and Overcompensating Later

Skipping dinner might seem like a way to reduce calorie intake, but this habit often backfires, especially for blood sugar management. When a standard mealtime is missed, hunger can intensify as the night progresses, leading to a strong urge to overeat or reach for convenient, high-sugar snacks. This overeating, especially late at night, causes a dramatic influx of glucose into the bloodstream, overwhelming the body’s nighttime insulin response and resulting in significant blood sugar fluctuations (American Diabetes Association).
Studies show that irregular meal patterns, particularly skipping main meals, are associated with poorer glucose control and an increased risk of developing type 2 diabetes (NIH). To maintain a balanced blood sugar profile, it is vital to have regular, well-portioned meals throughout the day. If dinner must be delayed, opt for a small, balanced snack such as a piece of fruit with nuts or a serving of yogurt, rather than high-sugar processed foods. This approach helps prevent late-night cravings and supports more stable overnight glucose levels.
5. Consuming Alcohol in the Evening

Drinking alcohol in the evening can have a complex impact on blood sugar levels. Initially, alcohol may cause blood sugar to drop, particularly in individuals taking insulin or other diabetes medications, because it interferes with the liver’s ability to release glucose into the bloodstream (CDC). However, as the effects of alcohol wear off, especially if consumed alongside carbohydrate-rich mixers or snacks, blood sugar can rebound and spike later in the night. This delayed hyperglycemia can be unpredictable and difficult to manage during sleep.
Studies indicate that alcohol disrupts the body’s normal glucose regulation, increasing the risk for both hypoglycemia and hyperglycemia (NIH). The risk is higher when alcohol is consumed without food or in excessive amounts. To minimize these risks, it is recommended to limit alcohol intake, avoid drinking on an empty stomach, and choose lower-sugar options such as dry wine or spirits mixed with water or club soda. Always monitor blood sugar levels closely if drinking alcohol in the evening, as its effects can linger and disrupt overnight glucose stability.
6. Lack of Physical Activity After Dinner

Spending evenings in a sedentary manner, such as watching TV, playing video games, or using mobile devices after dinner, can significantly impair the body’s ability to utilize glucose efficiently. After a meal, physical activity stimulates muscle cells to absorb glucose from the bloodstream, reducing postprandial (after-eating) blood sugar spikes (CDC). When activity levels are low, this important mechanism is diminished, resulting in higher nighttime glucose levels that can persist through the night.
Research has shown that even light activity, such as a short walk or gentle stretching after dinner, helps lower blood sugar and improves overall insulin sensitivity (NIH). In contrast, consistently sedentary habits contribute to elevated glucose, increasing the risk of nighttime hyperglycemia and long-term metabolic concerns. To counteract this, consider integrating a 10- to 20-minute walk, leisurely bike ride, or simple yoga routine into your evening schedule. These activities do not have to be strenuous to be effective; the key is to avoid remaining inactive for extended periods after eating, thereby promoting healthier overnight blood sugar control.
7. Stressful Evening Routines

Evening routines filled with stress—such as responding to work emails, engaging in heated discussions, or worrying about the next day—can trigger the release of cortisol, the body’s primary stress hormone. Elevated cortisol levels are well-known to raise blood sugar by signaling the liver to release more glucose into the bloodstream, preparing the body for a “fight or flight” response (NIH). When these stress-induced glucose surges occur at night, they can cause higher-than-normal blood sugar levels during sleep and contribute to overall poor glycemic control.
Real-life examples of stress-inducing evening activities include cramming for deadlines, doomscrolling news or social media, or managing challenging family dynamics right before bed. These habits not only hinder relaxation but also lead to persistent cortisol elevation long after the stressful event has passed. To minimize this effect, experts recommend establishing a calming pre-bedtime routine, such as practicing mindfulness, reading, or gentle stretching (Sleep Foundation). Such activities help reduce stress hormone levels, supporting more stable overnight blood glucose and better sleep quality.
8. Poor Sleep Hygiene

Poor sleep hygiene—such as maintaining irregular sleep schedules, using electronic devices late at night, or sleeping in an uncomfortable environment—can significantly disrupt blood sugar regulation. Research shows that inadequate or inconsistent sleep impairs the body’s ability to use insulin effectively, increasing insulin resistance and leading to higher blood sugar levels overnight (Sleep Foundation). This effect is particularly pronounced in people who go to bed at widely different times each night or frequently wake up during the night.
Studies reveal that even a single night of poor sleep can elevate blood glucose the next day, and chronic sleep deprivation is linked to a greater risk of developing type 2 diabetes (NIH). To improve sleep hygiene, experts recommend establishing a consistent bedtime routine, limiting screen exposure at least an hour before sleep, and creating a cool, dark, and quiet sleep environment. These practices not only promote restorative rest but also support stable blood sugar levels throughout the night, contributing to better overall metabolic health and daytime energy.
9. Late-Night Screen Use

Exposure to blue light from screens—such as smartphones, tablets, and televisions—late at night can disrupt the production of melatonin, the hormone responsible for regulating sleep-wake cycles. Melatonin not only affects sleep quality but also plays a role in insulin regulation and glucose metabolism. Suppressing melatonin through late-night screen use can impair the body’s ability to manage blood sugar effectively, leading to higher glucose levels overnight (Sleep Foundation).
Research has shown that people who use electronic devices before bed experience delayed melatonin release, shorter sleep duration, and increased insulin resistance (NIH). This combination can result in nocturnal blood sugar spikes and a greater risk for metabolic disturbances over time. To minimize these effects, experts recommend turning off electronic devices at least an hour before bedtime and considering alternatives such as reading a printed book or practicing relaxation techniques. Utilizing blue light filters or night mode settings on devices can also help, but the most effective strategy is reducing overall screen exposure in the evening to promote healthy melatonin and insulin function.
10. Eating Dessert Right Before Bed

Indulging in sugary desserts—such as ice cream, pastries, or chocolate—right before bed can lead to significant blood sugar fluctuations during sleep. These treats are typically high in refined sugars and simple carbohydrates, which are rapidly absorbed and cause a quick spike in blood glucose. Because insulin sensitivity decreases at night, the body struggles to bring these levels down efficiently, raising the risk for sustained overnight hyperglycemia (CDC). This can disrupt sleep quality and increase the risk for long-term metabolic complications.
Instead of traditional desserts, consider practical alternatives that promote blood sugar stability. Options like a small bowl of berries with a dollop of Greek yogurt, a few slices of apple with nut butter, or a square of dark chocolate (70% cocoa or higher) offer natural sweetness with added fiber, protein, or healthy fats. These components slow glucose absorption and help prevent dramatic spikes in blood sugar (American Diabetes Association). Making mindful choices for bedtime treats not only improves overnight glucose control but also supports lasting metabolic health and better sleep.
11. Skipping Evening Medication or Insulin

Failing to take prescribed evening medications or insulin poses serious risks, particularly for individuals managing diabetes. These medications are carefully timed to help regulate blood sugar levels overnight, when the body’s natural glucose control is less effective. Skipping a dose can result in elevated blood glucose throughout the night, increasing the risk of hyperglycemia and its associated complications, such as dehydration, fatigue, and in severe cases, diabetic ketoacidosis (CDC).
Adherence to medication regimens is a cornerstone of effective diabetes management. Studies have shown that consistent medication use significantly improves glycemic control and reduces the risk of both short-term and long-term complications (NIH). To prevent missed doses, consider setting daily reminders, using pill organizers, or enlisting the support of family members. Healthcare providers can also help adjust medication timing or simplify regimens to fit individual routines. Ultimately, taking evening medication or insulin as prescribed is essential for maintaining stable overnight blood sugar and safeguarding overall health.
12. Eating Processed or Fast Foods

Late-night cravings often lead to the consumption of processed or fast foods, which are notorious for their high content of hidden sugars, unhealthy fats, and refined carbohydrates. Items such as burgers, fries, pizza, and packaged snacks may seem convenient, but they deliver a rapid influx of glucose into the bloodstream due to low fiber and high glycemic index ingredients. This can result in sharp blood sugar spikes during the night, overwhelming the body’s ability to regulate glucose effectively (Harvard T.H. Chan School of Public Health).
Processed foods often contain added sugars and trans fats, which further impair insulin sensitivity and promote inflammation (NIH). These metabolic disturbances are especially concerning when such foods are consumed before sleep, as the body’s natural glucose metabolism slows down overnight. Opting for whole, minimally processed foods—such as fresh vegetables, lean proteins, and whole grains—helps maintain steady blood sugar levels. Preparing easy, healthy snacks in advance can also reduce the temptation to reach for processed convenience foods late at night, supporting better overnight glucose control and overall health.
13. Not Drinking Enough Water

Inadequate hydration is a frequently overlooked factor that can lead to higher blood sugar concentrations, particularly overnight. When the body is dehydrated, the volume of fluid in the bloodstream decreases, causing glucose to become more concentrated and increasing the risk of hyperglycemia (CDC). This effect is compounded during sleep, as the body naturally loses water through respiration and minimal fluid intake. Dehydration can also reduce the kidneys’ efficiency in flushing excess glucose out of the body, further compounding nighttime blood sugar spikes.
To support optimal hydration and blood sugar control, it’s important to drink water consistently throughout the day and into the evening. The general recommendation is to consume at least eight 8-ounce glasses of water daily, but individual needs may vary based on activity level, climate, and health status (Harvard T.H. Chan School of Public Health). Carrying a water bottle, setting hydration reminders, and choosing water over sugary beverages can help maintain proper fluid balance. Avoid excessive caffeine or alcohol in the evening, as these can contribute to dehydration. Prioritizing hydration supports healthy overnight glucose regulation and overall well-being.
14. Eating Too Quickly at Night

Rushing through evening meals can inadvertently lead to overeating and subsequent blood sugar spikes. When meals are eaten too quickly, the body doesn’t have enough time to register fullness, resulting in consuming larger portions than necessary before satiety signals reach the brain (CDC). This pattern is particularly problematic at night, as the intake of excess calories and carbohydrates can overwhelm the body’s reduced nighttime insulin sensitivity, leading to elevated glucose levels during sleep.
Mindful eating practices—such as slowing down, savoring each bite, and paying attention to hunger and fullness cues—have been shown to promote more balanced eating and improved blood sugar control (NIH). Strategies include setting aside screens during meals, chewing food thoroughly, and taking small pauses between bites. By adopting these habits, individuals are less likely to overeat and more likely to choose appropriate portion sizes, supporting better glycemic regulation. Making mealtime a relaxed and intentional experience not only aids digestion but also helps prevent nighttime blood sugar spikes, contributing to improved metabolic health and sleep quality.
15. Consuming Hidden Sugars in Sauces or Dressings

Many people are unaware of the significant sugar content found in common condiments such as ketchup, barbecue sauce, salad dressings, and even pasta sauces. These hidden sugars can quickly add up, especially when multiple condiments are used in a single meal. Consuming these products at night can lead to unexpected blood sugar surges, as the added sugars are rapidly absorbed and contribute to overall carbohydrate intake (CDC).
For individuals aiming to manage their blood glucose, it is important to read nutrition labels carefully and be mindful of serving sizes. Many store-bought sauces and dressings contain several grams of sugar per tablespoon, which can significantly impact blood sugar if consumed in larger amounts. Opting for homemade dressings with olive oil, vinegar, herbs, or choosing “no added sugar” or low-sugar varieties can help minimize this risk (Harvard T.H. Chan School of Public Health). Awareness of hidden sugars in sauces and dressings empowers individuals to make smarter choices, reducing the likelihood of nocturnal glucose spikes and supporting healthier eating habits overall.
16. Eating Refined Carbs Instead of Whole Grains

The choice between refined carbohydrates and whole grains can significantly influence blood sugar regulation, particularly at night. Refined carbs—such as white rice, white bread, and many packaged snack foods—have been stripped of their fiber and nutrient-rich outer layers. As a result, these foods are digested and absorbed much more quickly, causing rapid spikes in blood glucose levels after consumption (Harvard T.H. Chan School of Public Health).
Whole grains, such as brown rice, quinoa, whole wheat bread, and oats, retain their fiber, vitamins, and minerals. The higher fiber content in whole grains slows down digestion and the release of glucose into the bloodstream, resulting in steadier blood sugar levels throughout the night (NIH). Replacing refined carbs with whole grains in evening meals and snacks can help prevent nocturnal glucose surges and support long-term metabolic health. Incorporating whole grains not only improves blood sugar control but also increases satiety, potentially reducing the urge for late-night snacking and supporting overall well-being.
17. Ignoring Portion Sizes

Portion distortion—the tendency to underestimate the amount of food consumed—can lead to excessive calorie and carbohydrate intake, especially at night. Oversized servings of pasta, rice, snacks, or desserts are increasingly common and can significantly drive up blood sugar levels when eaten before bed. The body’s natural insulin response is already slower at night, making it more difficult to manage the influx of glucose from large meals (CDC).
Research shows that consistently eating portions larger than recommended serving sizes is a major contributor to hyperglycemia and weight gain (NIH). To avoid this pitfall, it’s important to become familiar with standard serving sizes and use tools such as measuring cups, food scales, or visual cues (like the size of your fist) to guide portions. Eating slowly and checking in with your body’s hunger and fullness signals can also help prevent overeating. Practicing mindful portion control at night supports steadier blood sugar levels, reduced risk of hyperglycemia, and promotes better long-term health outcomes.
18. Eating Out Late at Restaurants

Dining out late at restaurants can be a major contributor to nighttime blood sugar spikes. Restaurant meals are often larger in portion size and typically contain more sugar, refined carbohydrates, and unhealthy fats than home-cooked dishes. Common menu items like pasta with creamy sauces, loaded burgers on white buns, fried appetizers, and desserts can quickly add up to a high glycemic load (CDC). Even seemingly healthy choices, such as salads, may be topped with sugary dressings, candied nuts, or croutons that elevate carbohydrate content.
Research has shown that frequent consumption of restaurant meals is associated with poorer glycemic control and increased risk of obesity and diabetes (NIH). Unlike home-cooked options, diners have less control over ingredients, preparation methods, and hidden sugars or additives. To minimize the impact on blood sugar, consider reviewing menus in advance, choosing grilled or baked options, asking for dressings and sauces on the side, and paying close attention to portion sizes. Making informed choices when eating out late can help reduce nocturnal glucose surges and support overall metabolic health.
19. Grazing Throughout the Evening

Frequent snacking or “grazing” throughout the evening can have a cumulative effect on blood sugar, even if each individual snack seems small. When food intake is spread continuously over several hours, the body has little opportunity to return to baseline glucose levels between eating episodes. This repeated stimulation of insulin can lead to persistent elevations in blood sugar, especially at night when glucose metabolism slows (CDC).
In contrast, structured meal timing—with defined meals and snacks spaced appropriately—allows the body to process and utilize glucose more efficiently. Studies suggest that regular eating patterns support better glycemic control and lower the risk of nighttime hyperglycemia (NIH). If evening hunger occurs, it’s best to plan for a single, mindful snack that combines protein, fiber, and healthy fats, such as a small portion of nuts or cottage cheese with fruit. Sticking to regular meal times and avoiding constant grazing helps stabilize blood sugar, prevent unnecessary spikes, and supports improved sleep and metabolic health.
20. Eating in Response to Boredom or Emotions

Emotional eating—turning to food in response to feelings such as boredom, stress, loneliness, or anxiety—is a common pattern, particularly in the evening. This behavior often leads to the consumption of high-sugar or high-calorie comfort foods like ice cream, cookies, chips, or candy. These choices provide temporary relief but can cause significant blood sugar spikes overnight, contributing to poor glycemic control and disrupted sleep (NIH).
To break the cycle of emotional eating, it’s important to develop alternative coping strategies. Techniques such as journaling, practicing mindfulness or meditation, engaging in a hobby, or taking a short walk can help manage emotions without resorting to food (CDC). Establishing a structured evening routine and keeping high-sugar snacks out of easy reach can also reduce temptation. If the urge to eat persists, opt for a healthy, portion-controlled snack like air-popped popcorn, a small serving of fruit, or a cup of herbal tea. Over time, building awareness of emotional triggers and adopting healthier habits can support more stable overnight blood sugar and improved emotional well-being.
21. Consuming Energy Drinks in the Evening

Drinking energy drinks in the evening can have a dramatic impact on both blood sugar levels and sleep quality. Most energy drinks are loaded with sugar and high doses of caffeine, both of which can cause immediate blood glucose surges. The simple sugars in these beverages are rapidly absorbed and can overwhelm the body’s ability to manage glucose, especially before bed when insulin sensitivity is lower (CDC).
Caffeine, a major ingredient in energy drinks, further complicates matters by stimulating the release of stress hormones like cortisol, which promotes the release of glucose from the liver, driving blood sugar even higher (NIH). Additionally, the stimulating effects of both sugar and caffeine can disrupt the body’s natural sleep cycle, making it harder to fall asleep and reducing sleep quality. Poor sleep then feeds into a cycle of impaired glucose regulation. For better nighttime blood sugar control and restful sleep, it’s best to avoid energy drinks in the evening and opt for caffeine-free, unsweetened beverages like water or herbal tea.
22. Ignoring Fiber in Evening Meals
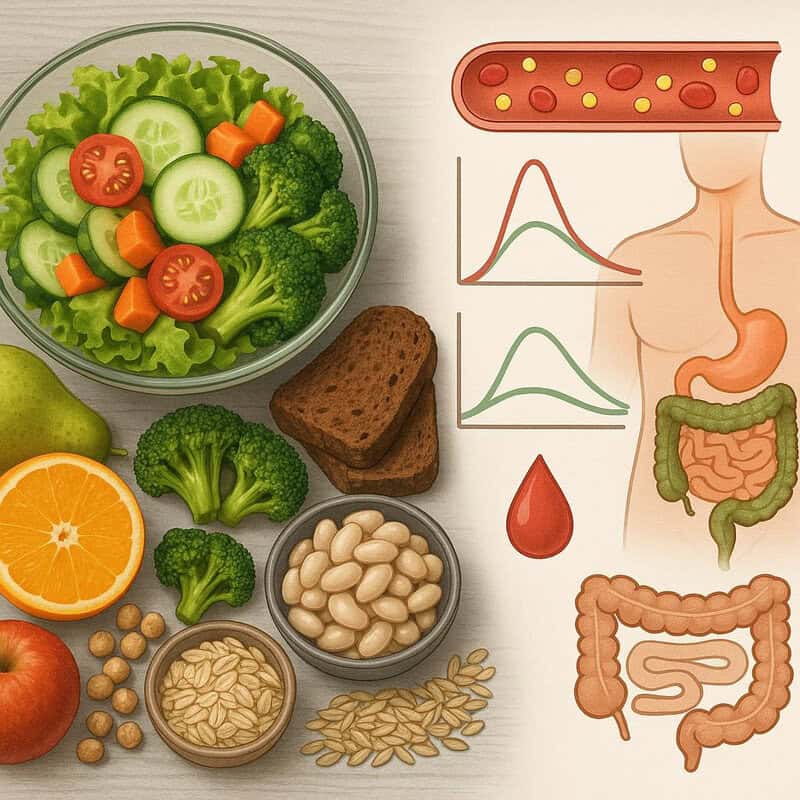
Dietary fiber plays a crucial role in moderating blood sugar levels by slowing the absorption of glucose from the digestive tract into the bloodstream. When evening meals are low in fiber—often due to reliance on refined grains, processed foods, or minimal vegetable intake—glucose is absorbed more rapidly, resulting in pronounced spikes in blood sugar after eating (Harvard T.H. Chan School of Public Health).
Including adequate fiber from sources such as vegetables, legumes, whole grains, and fruits helps create a gradual release of glucose, supporting more stable overnight blood sugar levels. Studies indicate that diets rich in fiber are linked to better glycemic control and a lower risk of developing type 2 diabetes (NIH). To enhance fiber intake at dinner, incorporate side salads, roasted vegetables, whole grain breads, or beans into evening meals. Reading nutrition labels and aiming for at least 25-30 grams of fiber daily can make a significant difference. Prioritizing fiber-rich foods not only benefits blood glucose regulation but also supports digestive health and satiety, reducing the urge for late-night snacking.
23. Eating Fried Foods at Night

Fried foods—such as fried chicken, French fries, onion rings, and fried snacks—are commonly consumed during late-night meals and can have a detrimental impact on blood sugar control. These foods are typically high in both carbohydrates and unhealthy fats, which together slow digestion but still deliver a substantial glycemic load. The combination of refined flour coatings and deep frying causes a delayed yet prolonged rise in blood glucose, often peaking overnight when the body’s insulin response is less effective (Harvard T.H. Chan School of Public Health).
Additionally, the high fat content in fried foods can further impair insulin sensitivity and contribute to metabolic disturbances. Research links frequent consumption of fried foods with increased risk of type 2 diabetes and poor overall glycemic control (NIH). These foods can also cause digestive discomfort or exacerbate acid reflux, which may disturb sleep. To support healthier overnight glucose levels and digestion, opt for baked, grilled, or steamed alternatives, and include more vegetables or whole grains in evening meals. Making these swaps helps maintain metabolic balance and promotes better sleep quality.
24. Consuming Excess Dairy Before Bed

While dairy products can be a source of protein and calcium, consuming excess amounts before bed—especially products like flavored yogurts, sweetened milk, or ice cream—can result in higher nighttime blood sugar levels. Many of these dairy items contain added sugars or high amounts of lactose, a naturally occurring sugar, both of which are rapidly absorbed and can drive glucose spikes when eaten late in the evening (CDC).
For example, a single serving of flavored or fruit-on-the-bottom yogurt may contain as much as 20 grams of sugar or more. Consuming these products in large portions before sleep can overwhelm the body’s ability to manage blood glucose, especially when insulin sensitivity is lower at night (NIH). To mitigate this risk, choose plain Greek yogurt, unsweetened milk alternatives, or small portions of cheese, and pair them with high-fiber foods like berries or nuts. Reading nutrition labels and being mindful of serving sizes can help keep sugar intake in check, supporting more stable overnight blood sugar and better overall metabolic health.
25. Late-Night Baking or Cooking Sessions

Engaging in late-night baking or cooking often leads to sampling freshly made treats or dishes, many of which are high in sugar and refined carbohydrates. Tasting cookie dough, sampling cakes, or nibbling on freshly baked bread can quickly add up to a significant intake of simple sugars and empty calories at a time when the body is least prepared to manage them. These habits can cause sharp blood sugar spikes that persist throughout the night, undermining glucose control and sleep quality (CDC).
To curb the impact of late-night culinary activities, consider preparing healthier alternatives. Swapping regular flour for whole grain varieties, using natural sweeteners like fruit purees, and adding fiber-rich ingredients such as oats or nuts can help lower the glycemic impact of homemade snacks (Harvard T.H. Chan School of Public Health). Additionally, setting a cutoff time for kitchen activities and saving finished baked goods for the next day can reduce temptation. Practicing mindful tasting and portion control while baking supports healthier overnight blood sugar and reinforces positive, lasting kitchen habits.
26. Consuming Artificial Sweeteners

Artificial sweeteners, such as aspartame, sucralose, and saccharin, are often marketed as blood sugar-friendly alternatives to sugar. However, emerging research indicates that their impact on glucose regulation may be more complex than previously thought. Some studies suggest that artificial sweeteners can alter gut microbiota, potentially impairing glucose tolerance and paradoxically leading to higher blood sugar levels in certain individuals (NIH).
While these sweeteners do not directly raise blood glucose like traditional sugars, their use may increase cravings for sweet foods, influence appetite regulation, and affect insulin sensitivity over time. For example, a study published in Cell found that saccharin consumption led to glucose intolerance in both mice and some human participants (Cell). As a result, consuming large amounts of artificially sweetened products in the evening may not provide the metabolic benefits one hopes for and could disrupt overnight glucose control in susceptible individuals. Moderation is key; opting for naturally sweet foods like fruit or choosing unsweetened beverages may offer a safer path for maintaining stable blood sugar levels at night.
27. Overeating After Exercise

Evening exercise is beneficial for overall health and blood sugar management, but it can sometimes trigger intense post-workout hunger. When this hunger is not met with balanced nutrition, individuals may gravitate toward high-sugar or high-calorie foods, such as sports drinks, energy bars, or sweet treats, to quickly satisfy cravings. These choices can lead to a rapid influx of glucose into the bloodstream, undermining the benefits of the workout and causing blood sugar spikes overnight (CDC).
Research shows that the body’s sensitivity to insulin is heightened after exercise, making it an ideal time to refuel with nutrient-dense options that combine complex carbohydrates, lean protein, and healthy fats (NIH). Examples include a small turkey sandwich on whole grain bread, a banana with nut butter, or Greek yogurt with berries. These snacks help replenish energy stores without causing dramatic blood sugar surges. Planning a balanced post-exercise meal or snack can curb excessive hunger and reduce the temptation to overeat on sugary foods, supporting more stable glucose levels through the night and enhancing recovery from physical activity.
28. Eating Without Monitoring Blood Sugar

For individuals at risk of hyperglycemia or managing diabetes, not routinely monitoring blood sugar can lead to unrecognized nighttime spikes. Many foods and habits can cause subtle changes in glucose levels, and without regular self-checks, these fluctuations may go unnoticed until symptoms or complications arise (CDC). Evening meals and snacks, in particular, can have prolonged effects on overnight glucose, making routine monitoring crucial for early detection and effective management.
Research has shown that self-monitoring of blood glucose is associated with improved glycemic control, better dietary decision-making, and reduced risk of long-term complications (NIH). Using a glucose meter or continuous glucose monitor (CGM) allows individuals to track the impact of different foods and behaviors on blood sugar, enabling timely adjustments to medication, meal composition, or portion sizes. Setting a routine for checking blood sugar before bed and, if necessary, during the night can help catch and address spikes early. Ultimately, regular self-monitoring empowers individuals to make informed choices and maintain more stable overnight glucose levels.
29. Consuming High-Sodium Foods

Eating high-sodium foods—such as processed meats, canned soups, salty snacks, and fast food—can have indirect but significant effects on glucose metabolism, particularly when consumed at night. Excess sodium intake leads to fluid retention, which can increase blood pressure and place added strain on the kidneys. This can impair the body’s ability to excrete excess glucose through urine, potentially resulting in higher blood sugar levels (CDC).
Furthermore, fluid retention caused by salty foods can disrupt sleep by causing nighttime thirst or frequent urination, both of which are linked to poor sleep quality. Research has shown that inadequate sleep negatively impacts insulin sensitivity and glucose regulation, creating a cycle where salty foods indirectly contribute to nighttime blood sugar spikes and metabolic disturbances (NIH). To minimize these effects, it’s best to limit high-sodium foods in the evening and choose fresh, minimally processed ingredients. Preparing meals at home, reading nutrition labels, and using herbs and spices for flavor can help keep sodium intake in check, supporting better sleep and more stable overnight blood sugar levels.
30. Nighttime Cravings and Giving In

Nighttime cravings are driven by a combination of psychological and biological factors. As the day winds down, fatigue, stress, and fluctuating hormone levels—such as ghrelin (the hunger hormone) and leptin (the satiety hormone)—can intensify the urge to snack, particularly on sugary or high-carbohydrate foods (Sleep Foundation). Giving in to these cravings often leads to the consumption of calorie-dense, low-nutrient foods like chocolate, chips, or pastries, which rapidly elevate blood sugar at a time when the body’s insulin response is diminished.
Research suggests that emotional cues, boredom, and habitual eating patterns are also powerful triggers for nighttime snacking (NIH). Unfortunately, these late-night indulgences can result in prolonged hyperglycemia, disrupted sleep, and increased risk of metabolic issues. To manage cravings, experts recommend establishing a consistent sleep routine, eating balanced meals throughout the day, and practicing mindful eating. Keeping healthy, low-glycemic snacks available and addressing emotional triggers with non-food strategies can help reduce the likelihood of giving in to nighttime cravings and better support overnight glucose stability.
31. Not Planning Evening Meals

Failing to plan evening meals often results in impulsive food choices that can quickly spike blood sugar. When dinner or late-night snacks are unplanned, convenience becomes the priority, leading many to reach for fast food, processed snacks, or sugary treats that are readily available. These options are typically high in refined carbohydrates, unhealthy fats, and added sugars, all of which can cause rapid elevations in blood glucose (CDC).
Research shows that meal planning is associated with improved dietary quality and better glycemic control, as it encourages more balanced, nutrient-dense choices and appropriate portion sizes (NIH). By setting aside time to prepare or select healthy evening meals and snacks in advance, individuals can avoid the temptation of high-glycemic, impulsive foods. Strategies include prepping ingredients, batch-cooking, or keeping nutritious options like cut vegetables, hummus, or whole-grain crackers on hand. Planning also makes it easier to incorporate fiber, lean protein, and healthy fats—all of which support stable blood sugar. Adopting a proactive approach to evening meals helps prevent nocturnal glucose spikes and promotes overall metabolic health.
32. Eating Close to Bedtime
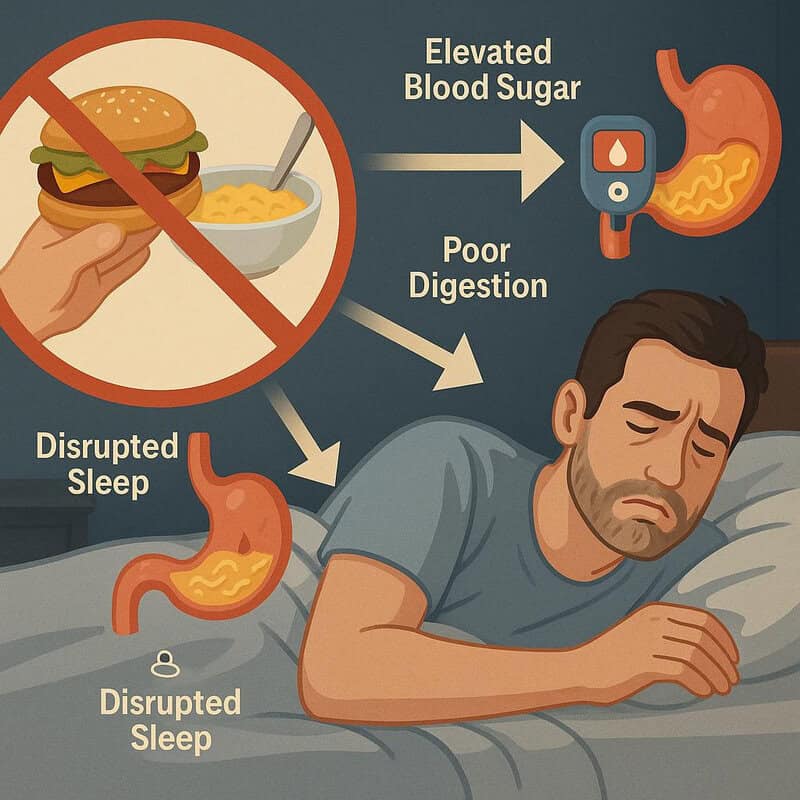
Consuming food shortly before going to bed can disrupt normal glucose regulation and impede digestion. When meals or snacks are eaten within an hour or two of lying down, the body has less time to process and utilize the glucose from food before shifting into its overnight metabolic state. This can lead to elevated blood sugar levels persisting throughout the night, as insulin sensitivity tends to decrease in the later hours (Sleep Foundation).
Research indicates that late-night eating is associated with higher fasting glucose and increased risk of metabolic dysfunction (NIH). Additionally, eating close to bedtime interferes with normal digestion, which can contribute to discomfort, acid reflux, and fragmented sleep. To promote better blood sugar control and overall health, experts recommend finishing your last meal or snack at least two to three hours before going to sleep. This practice supports natural circadian rhythms, enhances overnight glucose regulation, and may contribute to deeper, more restorative sleep.
33. Ignoring Protein in Night Meals

Protein plays a vital role in stabilizing blood sugar levels, particularly when consumed as part of evening meals. Unlike carbohydrates, protein is digested more slowly and does not cause rapid rises in blood glucose. When evening meals are heavily carb-based and low in protein—such as pasta with minimal meat or rice with vegetables only—there is a greater risk of post-meal glucose spikes and subsequent crashes during the night (CDC).
Including adequate protein in night meals helps slow the absorption of carbohydrates, resulting in a more gradual and sustained release of glucose into the bloodstream. Research demonstrates that balanced meals containing lean proteins, such as chicken, fish, tofu, or legumes, are associated with improved glycemic control and greater satiety, which can also curb late-night snacking (NIH). Ignoring protein can leave blood sugar regulation largely dependent on insulin’s action against carbs, increasing the risk of overnight hyperglycemia. To support stable nighttime glucose, aim to include a source of lean protein at dinner and in any planned evening snacks.
34. Eating for Social Reasons at Night

Social gatherings and shared evening meals can easily lead to overconsumption of sugary, carb-rich foods. Whether it’s a family dinner, a party with friends, or a late-night outing, the focus on celebration and connection often shifts attention away from mindful eating. Foods commonly served at these events—such as pizzas, cakes, chips, and sweetened beverages—are typically high in refined carbohydrates and added sugars, which can cause rapid spikes in blood glucose levels (CDC).
Research shows that people tend to eat more in social settings, especially when encouraged by group norms or the availability of abundant food choices (NIH). The relaxed atmosphere and distractions often result in eating larger portions or going back for seconds, further increasing carbohydrate intake. To mitigate these effects, try to be mindful of portion sizes, choose healthier options when available, and focus on social interaction rather than just food. Bringing a nutritious dish to share or eating a balanced meal beforehand can also help curb the temptation to overindulge. Practicing these strategies supports better overnight blood sugar control while still enjoying social connections.
35. Using Food to Unwind

Many people turn to comfort foods—such as ice cream, pastries, chips, or chocolate—as a way to relax and unwind after a long day. While these foods may provide temporary emotional relief, they are typically high in sugar and refined carbohydrates, leading to rapid increases in blood sugar levels, especially when consumed in the evening (CDC). This habit of using food as a form of relaxation can unintentionally disrupt glucose regulation overnight and interfere with restorative sleep.
Research indicates that emotional eating and reliance on comfort foods for stress relief are associated with poorer glycemic control and increased risk of metabolic syndrome (NIH). Instead of reaching for high-sugar snacks, consider alternative relaxation techniques such as deep breathing, gentle stretching, reading, or listening to calming music. Preparing a cup of caffeine-free herbal tea or engaging in a creative hobby can also help ease stress without impacting blood sugar. By breaking the cycle of using food to unwind, individuals can better support stable overnight glucose levels and promote healthier coping strategies for stress and relaxation.
36. Eating Leftovers Late at Night

Reaching for leftovers late at night is a common habit, especially after a busy day or when seeking a quick snack before bed. However, many leftovers—such as pizza, pasta, rice dishes, or casseroles—are often carb-heavy and can lead to unexpected blood sugar spikes when consumed during the evening hours. Reheating and eating these foods close to bedtime gives the body little time to process the carbohydrates before insulin sensitivity naturally wanes at night, increasing the risk of overnight hyperglycemia (CDC).
Studies suggest that the glycemic impact of starchy foods can sometimes increase when reheated, as the structure of the starches becomes more easily digestible (NIH). This means that even a moderate portion of leftovers could cause a more pronounced blood sugar response than anticipated. To avoid this, consider portioning leftovers when initially storing them and pairing them with fiber-rich vegetables or lean proteins if consumed at night. Being mindful of the carbohydrate content and timing can help reduce the likelihood of nocturnal glucose surges and promote more balanced overnight blood sugar.
37. Drinking Sweetened Milk or Hot Chocolate

Many people enjoy sweetened milk or hot chocolate as a comforting bedtime beverage, but these drinks can be surprisingly high in added sugars. A typical cup of commercial hot chocolate or chocolate milk often contains 15-25 grams of sugar per serving, which can cause a rapid increase in blood glucose when consumed close to bedtime (CDC). Even homemade versions that use sweetened cocoa mixes or flavored syrups can contribute to significant nocturnal blood sugar spikes, as the body is less able to efficiently process excess glucose at night.
For better blood sugar outcomes, consider alternatives such as unsweetened almond or soy milk, plain low-fat milk, or making hot chocolate with unsweetened cocoa powder and a non-caloric sweetener. These options minimize sugar content while still providing a warm, soothing beverage. Adding a sprinkle of cinnamon or a dash of vanilla can enhance flavor without affecting glucose levels. Reading nutrition labels and being mindful of portion sizes are key to avoiding hidden sugars in bedtime drinks (Harvard T.H. Chan School of Public Health). Choosing lower-sugar alternatives supports more stable overnight blood sugar and a healthier nightly routine.
38. Mindless Eating While Distracted

Mindless eating—such as consuming snacks or meals while watching TV, scrolling on a phone, or working on a computer—can lead to significant overconsumption of calories and carbohydrates. When attention is diverted from eating, individuals are less likely to notice portion sizes or recognize feelings of fullness, which increases the risk of eating far more than intended (CDC). This habit is especially concerning at night, when large or frequent intakes of food can overwhelm the body’s reduced nighttime insulin sensitivity and cause pronounced blood sugar spikes.
Research has shown that distracted eating is associated with higher total energy and sugar intake, as well as poorer dietary choices overall (NIH). To counteract this, practice mindful eating by setting aside electronics and focusing solely on the meal or snack. Paying attention to hunger and satiety cues, eating slowly, and truly savoring each bite can help regulate intake and support healthier blood glucose levels. Adopting these habits in the evening can reduce the risk of nocturnal hyperglycemia and promote better metabolic health and sleep quality.
39. Not Adjusting Insulin for Nighttime Snacks

For individuals who use insulin therapy, failing to adjust insulin doses in response to unplanned nighttime snacks can lead to significant blood sugar spikes. Nighttime snacks, especially those high in carbohydrates or sugar, require careful insulin management to ensure glucose is properly utilized and doesn’t accumulate in the bloodstream. Without appropriate dose adjustments, the body may not have enough insulin available to handle the influx of glucose, resulting in hyperglycemia during the night (CDC).
Research underscores the importance of matching insulin doses to carbohydrate intake, particularly for those with type 1 diabetes or insulin-dependent type 2 diabetes (NIH). This includes being vigilant with carbohydrate counting and using bolus insulin as needed when consuming extra evening snacks. Utilizing continuous glucose monitoring (CGM) systems or regularly checking blood sugar levels can help fine-tune insulin adjustments and prevent both hyperglycemia and hypoglycemia overnight. Consulting with a healthcare provider or diabetes educator for personalized insulin strategies is essential for effective long-term management and safer nighttime glucose control.
40. Consuming Sweetened Yogurt as a Snack

Sweetened and flavored yogurts are popular evening snacks, but they can contain surprisingly high amounts of added sugar. Many fruit-flavored or dessert-style yogurts have 15-25 grams of sugar per serving, with much of it coming from added sweeteners rather than natural milk sugars (CDC). Consuming these yogurts at night can cause rapid spikes in blood glucose, particularly problematic when the body’s insulin sensitivity is lower during evening hours.
In contrast, plain yogurt—especially Greek or Icelandic styles—contains little or no added sugar and higher protein content, making it a better choice for stable blood sugar. The protein and probiotics in plain yogurt can help slow digestion and promote satiety, further supporting overnight glucose control (NIH). For a naturally sweet yet blood sugar-friendly option, add fresh berries or a sprinkle of cinnamon to plain yogurt instead of reaching for pre-sweetened varieties. Reading ingredient lists and nutrition labels carefully allows for smarter snack choices that minimize sugar intake and support healthier overnight metabolic patterns.
41. Overindulging in Fruit Late at Night

While fruit is a nutritious part of a balanced diet, overindulging in fruit late at night can lead to unexpected blood sugar spikes due to their natural sugar content, primarily fructose. Certain fruits such as grapes, bananas, mangos, and cherries are particularly high in sugar and, when eaten in large quantities, can rapidly elevate blood glucose—especially problematic when insulin sensitivity is decreased in the evening (CDC).
Although fruit provides fiber, vitamins, and antioxidants, moderation is key for those monitoring blood sugar. Studies show that portion size is crucial; a small serving of berries or a single apple is less likely to disrupt glucose balance compared to several servings of high-sugar fruits (NIH). To enjoy fruit as a nighttime snack without spiking blood sugar, pair it with a protein or healthy fat, such as nuts or Greek yogurt, which can help slow glucose absorption. Being mindful of both type and amount of fruit consumed supports more stable overnight blood sugar and maintains the health benefits of fruit within a balanced diet.
42. Eating Ice Cream or Frozen Desserts

Indulging in ice cream or other frozen desserts before bed is a common habit, but these sweet treats are typically high in added sugars and simple carbohydrates. Consuming them late at night can cause a rapid surge in blood glucose levels, as the sugars in ice cream are quickly absorbed into the bloodstream (CDC). This spike is particularly concerning in the evening, when the body’s insulin sensitivity is naturally reduced, making it harder to bring glucose levels back down to normal before sleep.
Additionally, the high fat content in many frozen desserts can slow digestion, leading to prolonged elevated blood sugar and potentially causing discomfort, indigestion, or even fragmented sleep (NIH). Disrupted sleep cycles are linked to further metabolic disturbances and impaired glucose regulation the following day. For a healthier alternative, consider a small bowl of frozen berries or banana slices paired with a spoonful of plain Greek yogurt. These swaps offer sweetness with less sugar and more fiber, helping to prevent dramatic nighttime glucose spikes and supporting better sleep quality.
43. Drinking Unfiltered Fruit Juices

Drinking unfiltered fruit juices, such as orange juice or apple juice, can cause sharp increases in blood sugar, especially when consumed at night. Unlike whole fruit, which contains fiber that slows the absorption of natural sugars, juice is stripped of most or all fiber, allowing glucose and fructose to enter the bloodstream rapidly (CDC). This leads to quick and substantial spikes in blood sugar levels, a concern for those with diabetes or anyone seeking to maintain stable overnight glucose.
Research has shown that even 100% fruit juices can have a similar glycemic effect as sugary soft drinks due to their lack of fiber and concentration of sugars (NIH). In contrast, eating whole fruit provides not only fiber but also additional vitamins, minerals, and antioxidants, which support better metabolic health. To avoid nocturnal blood sugar surges, it’s best to choose whole fruits over juices, limit portion sizes, and pair fruit with a source of protein or healthy fat. Making these swaps supports steadier blood glucose and reduces the risk of overnight hyperglycemia.
44. Not Checking Nutrition Labels

Failing to check nutrition labels on packaged foods can lead to unintentional consumption of hidden sugars, which are common contributors to nighttime blood sugar spikes. Many seemingly healthy foods—such as granola bars, flavored yogurt, salad dressings, pasta sauces, and even whole grain breads—contain added sugars that can quickly add up when eaten in the evening (CDC). These hidden sugars are often listed under various names, making them easy to overlook without careful label reading.
Research highlights that regularly consuming packaged foods high in added sugars is associated with poorer glycemic control and increased risk of metabolic issues (NIH). To make informed choices, it’s essential to review ingredient lists and nutrition facts panels, paying close attention to total sugars and added sugars per serving. Opting for products labeled as “no added sugar” or “unsweetened” can help minimize sugar intake. Being a vigilant label reader empowers individuals to select foods that better support overnight blood sugar stability, promoting healthier eating habits and improved long-term metabolic health.
45. Consuming “Sugar-Free” Labeled Snacks

Snacks labeled as “sugar-free” can be misleading for those aiming to manage their blood sugar, especially when consumed at night. While these products may not contain traditional sugars, they often include sugar alcohols (such as sorbitol, maltitol, or xylitol), starches, or refined flours that can still affect glucose levels. According to FDA guidelines, “sugar-free” means less than 0.5 grams of sugar per serving, but does not guarantee the absence of other carbohydrates that may impact blood glucose.
Research indicates that certain sugar alcohols and alternative sweeteners can still raise blood sugar, particularly when consumed in large quantities or in combination with other carbohydrate sources (NIH). Additionally, some sugar-free snacks are highly processed and may lack nutritional value, leading to poor satiety and the temptation to overeat. To minimize risks, always check the total carbohydrate content, serving size, and ingredient list of “sugar-free” products. Prioritizing whole, minimally processed snacks—such as nuts, seeds, or fresh vegetables—supports more stable overnight blood sugar and better long-term metabolic health.
46. Ignoring Personal Glucose Patterns

Overlooking individual glucose patterns can undermine effective blood sugar management, especially at night. Everyone’s body responds differently to various foods, activities, and stressors, and what may cause a spike in one person might have little effect on another. Consistently tracking personal blood sugar responses—through regular checks or continuous glucose monitoring—helps identify unique trends and enables tailored adjustments to diet, medication, and lifestyle (CDC).
Research underscores the importance of individualized care, as recognizing personal glucose fluctuations allows for proactive management and reduces the risk of both nocturnal hyperglycemia and hypoglycemia (NIH). For example, some people may notice spikes after certain evening snacks or late dinners, while others are more affected by stress or lack of physical activity. Logging meals, activity, and glucose readings helps create a clearer picture of what influences nighttime blood sugar. Sharing these trends with a healthcare provider can further refine management strategies. Embracing a personalized approach empowers individuals to make informed choices and maintain more stable overnight glucose levels for better overall health.
47. Not Taking Time to Relax Before Bed

Skipping relaxation before bed can negatively impact blood sugar regulation by keeping stress hormone levels—particularly cortisol—elevated. High cortisol stimulates the liver to release more glucose into the bloodstream, which can lead to elevated blood sugar levels at night (NIH). When the body doesn’t have an opportunity to unwind, the stress response persists, making it harder for insulin to work effectively and increasing the likelihood of nocturnal hyperglycemia.
Research demonstrates that relaxation techniques such as deep breathing, progressive muscle relaxation, meditation, or gentle stretching can lower cortisol and support improved glycemic control (Sleep Foundation). Incorporating a calming pre-bed routine not only aids in falling asleep but also promotes steady overnight glucose by reducing the physiological stress response. Small steps—such as dimming lights, avoiding stimulating activities, and setting aside dedicated time for relaxation—can make a meaningful difference. Making relaxation a nightly habit supports both better sleep quality and more stable blood sugar, fostering overall well-being and resilience against metabolic disturbances.
48. Eating High-Calorie, Low-Nutrient Snacks

Consuming snacks that are high in calories but low in nutrients—such as chips, candy, pastries, and processed snack bars—can cause significant blood sugar surges, especially when eaten at night. These foods are typically rich in refined carbohydrates and added sugars, which are rapidly absorbed and lead to quick spikes in blood glucose levels (CDC). Additionally, they often lack fiber, protein, and healthy fats, all of which help slow glucose absorption and promote satiety.
Research indicates that high-calorie, low-nutrient foods are not only less filling but also tend to encourage overeating, as they do not trigger the same satisfaction signals as nutrient-dense options (NIH). The resulting blood sugar spikes can disrupt sleep and contribute to poor metabolic health over time. To avoid these pitfalls, opt for snacks that combine fiber, protein, and healthy fats—such as a handful of nuts, fresh vegetables with hummus, or a small serving of Greek yogurt with berries. Choosing nutrient-rich snacks supports more stable overnight blood sugar and keeps nighttime hunger at bay.
49. Not Seeking Professional Advice When Needed

Failing to consult healthcare professionals when experiencing persistent nighttime blood sugar spikes can lead to ongoing health risks and missed opportunities for effective management. Blood sugar regulation is complex, and untreated hyperglycemia can increase the risk of complications such as cardiovascular disease, neuropathy, and impaired sleep (CDC). Self-management strategies are valuable, but they may not address the underlying causes or account for individual health needs.
Healthcare providers can offer personalized advice, adjust medication regimens, recommend diagnostic testing, and provide referrals to specialists such as endocrinologists or dietitians. According to the CDC’s guidelines for diabetes management, routine consultations and check-ins are essential for optimal glycemic control and early detection of complications. If you notice patterns of unexplained high blood sugar at night, frequent symptoms, or difficulty managing your condition, it’s important to seek professional guidance promptly. Timely intervention ensures that treatment plans are tailored to your needs and supports better long-term health outcomes, empowering you to regain control over your blood sugar and overall well-being.
50. Overlooking Symptoms of Nocturnal Hyperglycemia
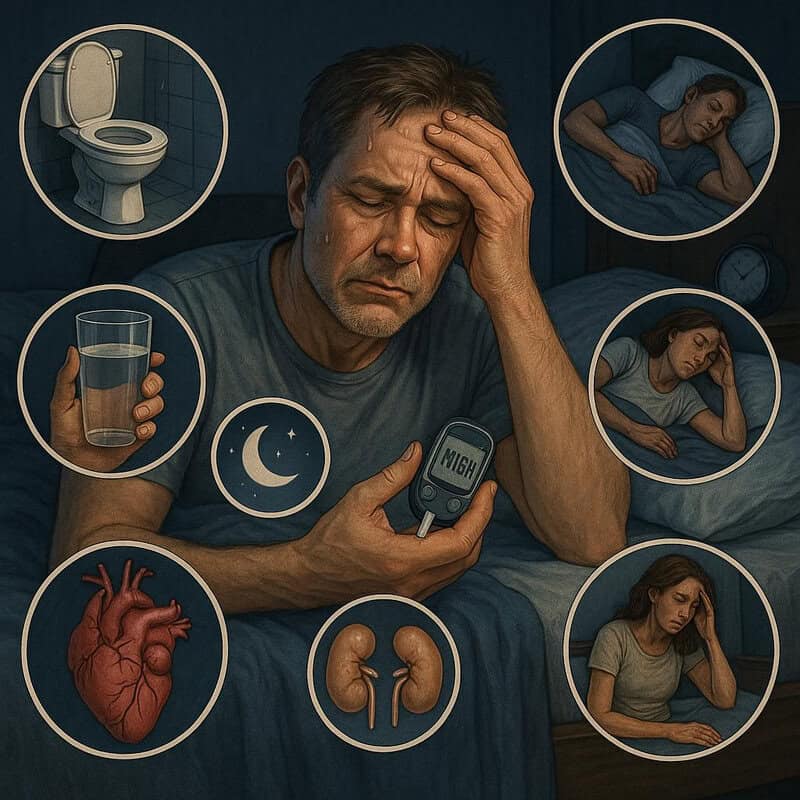
Failing to recognize the symptoms of nocturnal hyperglycemia can delay intervention and increase the risk of serious complications. Common signs of high blood sugar at night include frequent urination, excessive thirst, restless or disrupted sleep, headaches upon waking, night sweats, and unexplained fatigue (CDC). These symptoms may be subtle or mistaken for other sleep disturbances, leading many to overlook their connection to elevated glucose levels.
Prompt recognition and action are crucial because untreated nocturnal hyperglycemia can contribute to long-term health issues such as heart disease, kidney damage, and neuropathy (NIH). Monitoring blood sugar regularly, especially if symptoms are present, allows for early detection and timely adjustments to diet, medication, or lifestyle. Consulting a healthcare provider when nocturnal symptoms persist ensures that underlying causes are addressed and effective strategies are implemented. Being vigilant about nighttime blood sugar symptoms empowers individuals to prevent complications, improve sleep quality, and maintain better overall health and metabolic control.
Conclusion

Recognizing and addressing nighttime blood sugar spikes is essential for preventing long-term complications and maintaining optimal health. Reflect on your current evening habits, as even small changes can make a significant difference in glycemic control. Practical steps include adopting mindful eating, prioritizing nutrient-rich foods, and establishing a consistent bedtime routine. Regular glucose monitoring and prompt action if symptoms arise are crucial for effective management (CDC). If you experience persistent issues, consult a healthcare professional for personalized guidance (CDC Diabetes Management). Proactive attention to nighttime habits can help ensure stable blood sugar and improved overall well-being.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





