Innovative Advances in Lung Cancer Treatments
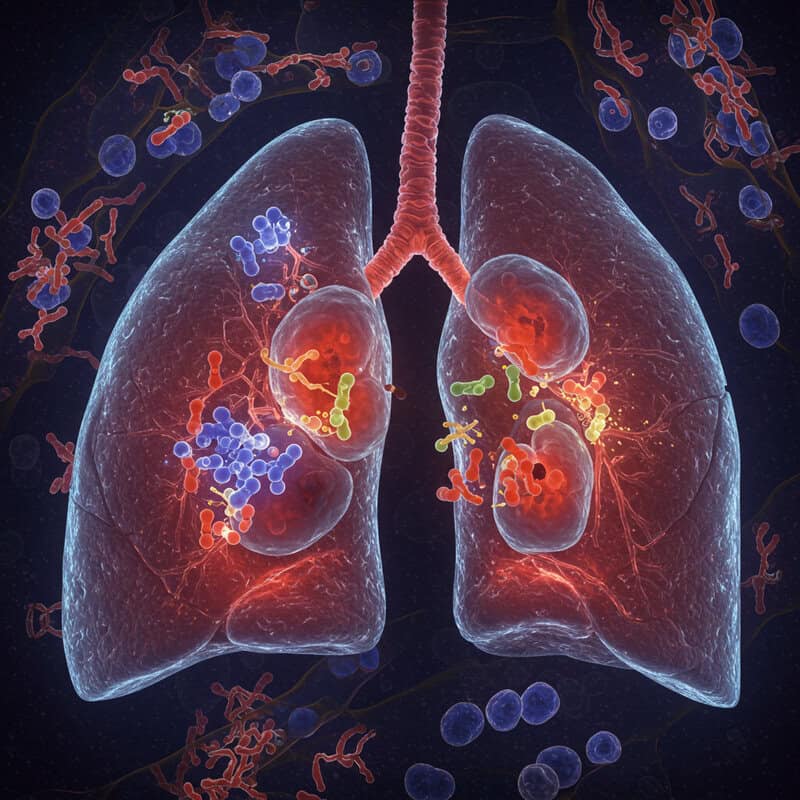
Lung cancer remains the leading cause of cancer deaths worldwide, responsible for nearly 1.8 million fatalities annually according to the World Health Organization. The lungs, vital organs within the respiratory system, are essential for oxygenating blood and removing carbon dioxide. Despite medical advances, late-stage detection is common, with over half of cases diagnosed after the cancer has spread, significantly reducing survival rates. This challenge underscores the urgent need for improved screening, early intervention, and innovative therapies to transform patient outcomes globally.
1. Liquid Biopsy for Early Detection

Liquid biopsy is revolutionizing the early detection of lung cancer by analyzing blood samples for circulating tumor DNA (ctDNA) and other biomarkers. Unlike traditional tissue biopsies, this minimally invasive method enables clinicians to detect genetic mutations and cancer-specific fragments shed by tumors into the bloodstream, often before symptoms arise. Recent studies, such as those published in The New England Journal of Medicine, have demonstrated the potential of liquid biopsies to identify lung cancer at earlier, more treatable stages, improving the chances of successful intervention.
Liquid biopsies offer several advantages, including reduced risk, faster turnaround times, and the ability to monitor disease progression or recurrence non-invasively. For individuals at high risk—such as long-term smokers or those with a family history of lung cancer—incorporating liquid biopsy into routine screening may enhance early detection rates. Experts advise discussing eligibility for such tests with healthcare providers and combining liquid biopsy with established imaging techniques for comprehensive screening. As technology advances, liquid biopsies are poised to become an integral part of personalized and proactive lung cancer care.
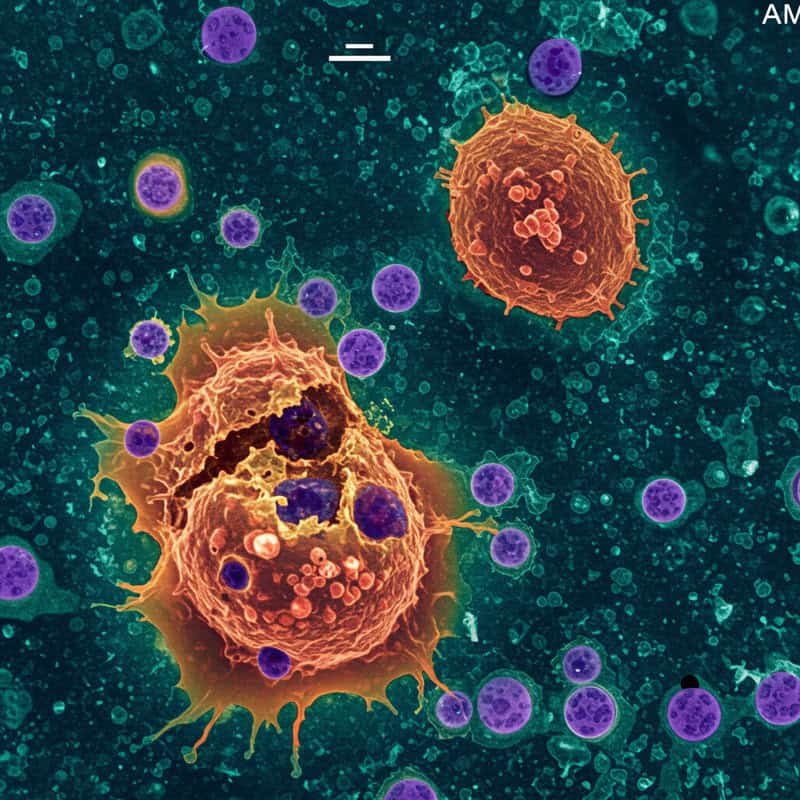
2. Immunotherapy Checkpoint Inhibitors

Immune checkpoint inhibitors have transformed the treatment landscape for lung cancer by harnessing the body’s own immune system to target and destroy cancer cells. These therapies work by blocking specific proteins—such as PD-1, PD-L1, or CTLA-4—that cancer cells use to evade immune detection. By inhibiting these checkpoints, drugs like pembrolizumab (source: National Cancer Institute) “release the brakes” on immune cells, enabling them to recognize and attack tumor cells more effectively.
Pembrolizumab, approved for both non-small cell and small cell lung cancer, has shown significant survival benefits in several clinical trials. For example, the KEYNOTE-024 study demonstrated that patients with high PD-L1 expression treated with pembrolizumab experienced longer progression-free and overall survival compared to those on traditional chemotherapy (New England Journal of Medicine). These results have led to checkpoint inhibitors becoming a standard of care for many lung cancer patients, either alone or in combination with other therapies. Ongoing research aims to expand their use and improve outcomes through combination regimens and novel checkpoint targets.
3. Targeted Therapy for EGFR Mutations

Targeted therapies have emerged as a groundbreaking approach for lung cancer patients with specific genetic alterations, notably mutations in the epidermal growth factor receptor (EGFR) gene. Drugs like osimertinib are designed to selectively inhibit the activity of mutated EGFR proteins, thereby blocking signals that promote cancer cell growth and survival. This precision medicine strategy spares healthy cells and reduces side effects compared to conventional treatments.
Clinical studies have demonstrated that EGFR inhibitors offer substantial benefits over traditional chemotherapy. The FLAURA trial, published in the New England Journal of Medicine, found that patients with advanced EGFR-mutated non-small cell lung cancer who received osimertinib had significantly longer progression-free and overall survival than those treated with earlier-generation EGFR inhibitors or chemotherapy. Furthermore, targeted therapies are associated with improved quality of life and fewer severe side effects. As genetic testing becomes more accessible, identifying EGFR mutations allows for more personalized and effective treatment plans. For patients, discussing genetic profiling with their healthcare provider is a crucial step in determining eligibility for these innovative therapies.
4. ALK Inhibitors for Non-Small Cell Lung Cancer
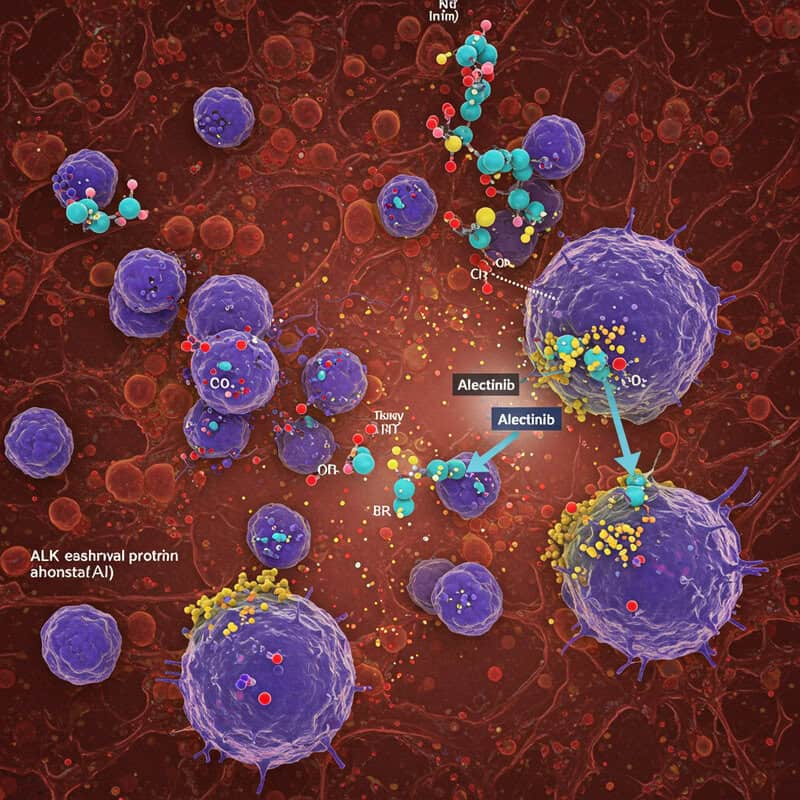
ALK inhibitors represent a major advancement for patients with non-small cell lung cancer (NSCLC) that harbor rearrangements in the anaplastic lymphoma kinase (ALK) gene. Medications such as alectinib are designed to specifically target and block the abnormal ALK protein, thereby interrupting signals that drive cancer cell growth. This targeted approach allows for highly effective treatment with reduced damage to healthy tissues.
Real-world evidence and clinical trials have demonstrated the significant benefits of ALK inhibitors like alectinib. The ALEX study, detailed in the New England Journal of Medicine, showed that patients treated with alectinib had markedly longer progression-free survival compared to those receiving earlier ALK inhibitors or chemotherapy. Additionally, alectinib has proven effective in controlling brain metastases—a common complication in ALK-positive lung cancer—thereby improving both disease outcomes and quality of life. The favorable safety and efficacy profile of ALK inhibitors has made them a standard first-line therapy for ALK-positive NSCLC. Genetic testing for ALK rearrangements is now routine, ensuring that eligible patients can benefit from these innovative, life-extending treatments.
5. Next-Generation Sequencing

Next-generation sequencing (NGS) has revolutionized the diagnosis and management of lung cancer by enabling comprehensive genetic profiling of tumor samples. This advanced technology rapidly analyzes the DNA of lung tumors to identify a wide array of genetic mutations, including alterations in EGFR, ALK, ROS1, and other actionable genes. By uncovering these genetic drivers, NGS empowers oncologists to tailor treatment strategies to the unique molecular makeup of each patient’s cancer.
NGS facilitates precision medicine, allowing clinicians to select targeted therapies or immunotherapies most likely to be effective based on individual tumor characteristics. Studies, such as those referenced by the National Cancer Institute, have shown that integrating NGS into clinical practice leads to improved patient outcomes, particularly as more therapies are developed for rare genetic mutations. The ability to identify resistance mutations also helps guide subsequent treatment decisions and avoid ineffective therapies. As NGS becomes more accessible and cost-effective, its use is expanding in both initial diagnosis and ongoing disease monitoring. Patients are encouraged to discuss comprehensive genomic testing with their healthcare providers to ensure the most personalized and effective treatment plan possible.
6. Stereotactic Body Radiotherapy (SBRT)

Stereotactic Body Radiotherapy (SBRT) is a cutting-edge radiation treatment that delivers highly focused, intense doses of radiation directly to lung tumors, with remarkable precision. Unlike conventional radiation therapy, which typically involves smaller doses over several weeks, SBRT can often be completed in just a few sessions. This approach is made possible by advanced imaging and motion-tracking technologies that accurately target tumors while minimizing exposure to surrounding healthy tissues.
Clinical studies have demonstrated that SBRT is particularly effective for patients with early-stage non-small cell lung cancer who are not candidates for surgery. According to research published in Frontiers in Oncology, SBRT achieves local control rates comparable to surgical removal, with fewer side effects and shorter recovery times than traditional radiation therapy. The focused delivery reduces the risk of long-term complications and allows for the treatment of tumors located near sensitive structures in the chest. As a result, SBRT is rapidly becoming a preferred option for select lung cancer patients. Those considering radiation therapy should consult their oncologist about the suitability and benefits of SBRT for their specific clinical situation.
7. Robotic-Assisted Surgery
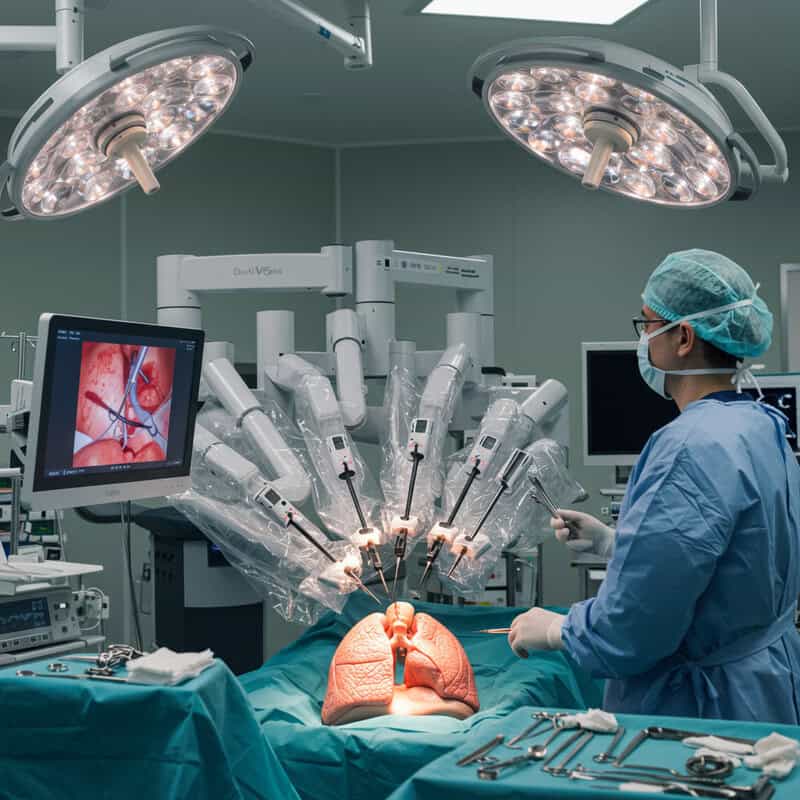
Robotic-assisted surgery represents a significant leap forward in the minimally invasive treatment of lung cancer. Utilizing sophisticated robotic systems, such as the da Vinci Surgical System, surgeons can perform complex lung resections through small incisions with enhanced precision, flexibility, and control. This technology provides surgeons with a high-definition, 3D view of the surgical site and articulated instruments that mimic the natural movements of the human hand, allowing for meticulous dissection of tumors while preserving healthy tissue.
Compared to traditional open surgery, robotic-assisted procedures are associated with reduced postoperative pain, lower complication rates, and faster recovery times. A study published in Annals of Thoracic Medicine found that patients undergoing robotic lobectomy for lung cancer experienced shorter hospital stays and quicker return to daily activities. Additionally, minimally invasive techniques may result in less blood loss and smaller scars, contributing to improved patient satisfaction and quality of life. As robotic technology continues to evolve, its application is expanding to more complex cases, making it an increasingly valuable tool in the surgical management of lung cancer. Patients should discuss surgical options with their care team to determine the most appropriate approach.
8. Personalized Cancer Vaccines

Personalized cancer vaccines are an emerging innovation in lung cancer treatment, designed to stimulate the patient’s immune system to recognize and attack tumor cells with unique mutations. These vaccines are custom-made based on the specific genetic and protein changes found in an individual’s cancer, allowing for a highly targeted immune response. By presenting these tumor-specific antigens to the immune system, personalized vaccines can boost the body’s natural defenses and potentially prevent cancer recurrence.
Recent clinical trials, such as those highlighted by the National Cancer Institute, have demonstrated promising results in patients with advanced lung cancer. Early data show that these vaccines can enhance immune activation and may increase the effectiveness of other treatments, including immune checkpoint inhibitors. While still experimental, the approach represents a significant step toward individualized medicine, where therapies are tailored not only to the cancer type but to the patient’s unique tumor profile. As research advances, personalized cancer vaccines could become an integral part of combination therapy for lung cancer. Patients interested in these innovative options are encouraged to inquire about clinical trials and emerging immunotherapy strategies with their healthcare providers.
9. Tumor Microenvironment Modulation
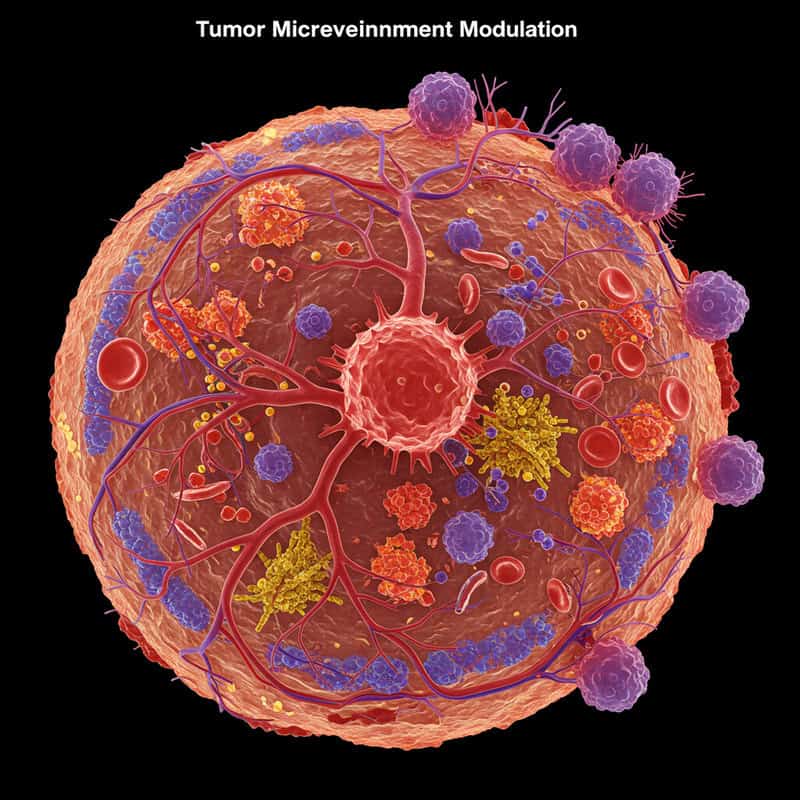
Modulating the tumor microenvironment has become a promising strategy in the fight against lung cancer. The tumor microenvironment includes not only cancer cells but also surrounding blood vessels, immune cells, and connective tissue, all of which interact to support tumor growth and protect cancer from traditional therapies. One key approach is targeting angiogenesis, the process by which tumors stimulate new blood vessel formation to secure a nutrient supply.
Anti-angiogenic therapies, such as bevacizumab, block signals like vascular endothelial growth factor (VEGF), effectively “starving” tumors by cutting off their blood supply. This approach can slow tumor progression and enhance the effectiveness of chemotherapy or immunotherapy. Studies, including those detailed in the National Cancer Institute, have shown that combining angiogenesis inhibitors with standard treatments can extend survival in patients with advanced non-small cell lung cancer. Researchers are also exploring drugs that modify other components of the tumor microenvironment, such as reprogramming immune cells to become more hostile to cancer or altering the extracellular matrix to prevent metastasis. As this field evolves, therapies targeting the tumor microenvironment are expected to play an increasingly critical role in comprehensive lung cancer care.
10. Bispecific Antibodies
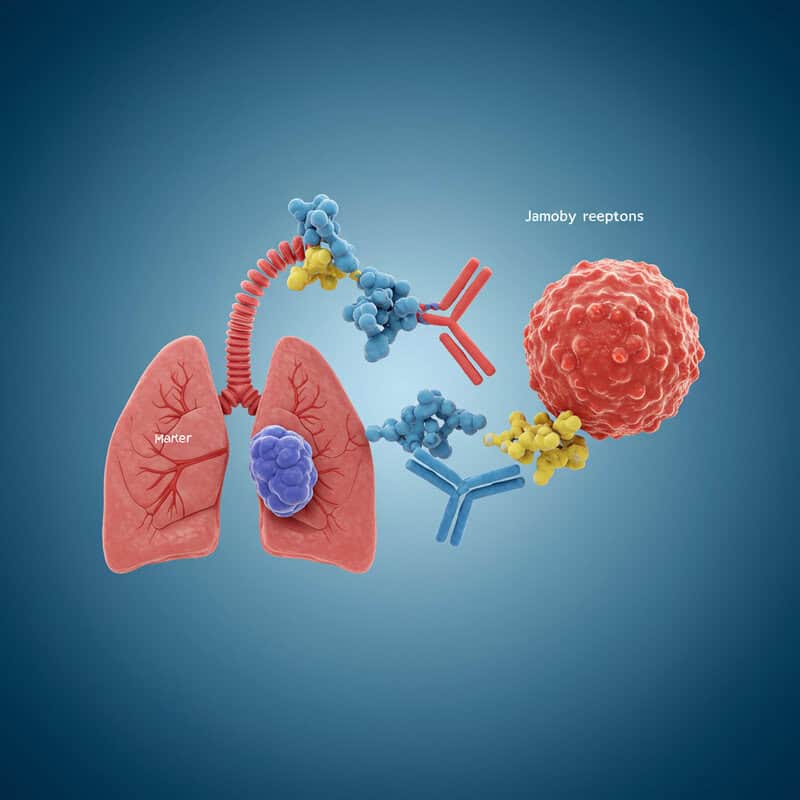
Bispecific antibodies are a novel class of immunotherapy designed to simultaneously bind two different targets, such as a marker on lung cancer cells and an activating receptor on immune cells. By bridging tumor cells with immune effector cells—most commonly T cells—these engineered antibodies create a direct link that enables the immune system to recognize and destroy cancer more efficiently. This approach bypasses some of the mechanisms tumors use to evade immune detection, enhancing the precision and potency of the immune response.
One example is the development of bispecific T-cell engagers (BiTEs), which have shown promising results in early clinical studies for various cancers, including lung cancer. Research highlighted by the National Cancer Institute illustrates how these drugs can shrink tumors and, in some cases, produce durable remissions. Ongoing trials are exploring different combinations and formats, seeking to maximize efficacy while minimizing side effects. As more bispecific antibodies enter clinical practice, they are expected to expand the arsenal of targeted immunotherapies available to lung cancer patients, offering hope for improved outcomes, especially in cases resistant to other treatments.
11. Tumor Treating Fields Therapy
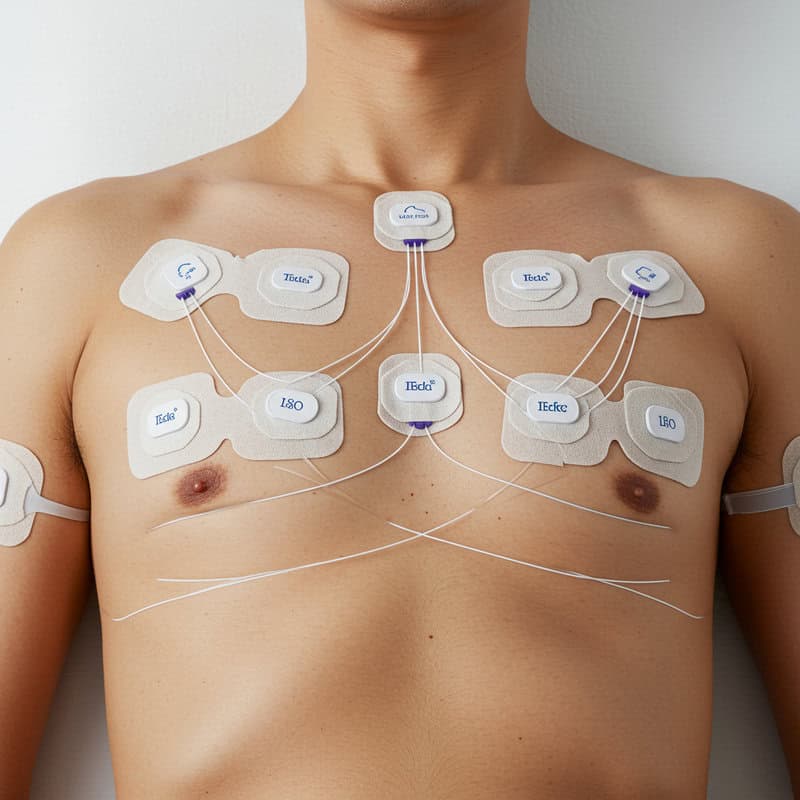
Tumor Treating Fields (TTFields) therapy is an innovative, non-invasive treatment that uses low-intensity, alternating electric fields to disrupt cancer cell division. Delivered through adhesive electrodes placed on the patient’s chest, these electrical fields interfere with the normal process of mitosis, causing cancer cells to die while sparing healthy tissue. Originally approved for glioblastoma, TTFields are now being explored in clinical trials for lung cancer, expanding their potential impact.
Recent studies, such as the LUNAR trial described by Novocure, have demonstrated that adding TTFields therapy to standard treatments, including immunotherapy and chemotherapy, can improve survival in patients with advanced non-small cell lung cancer. The therapy is well tolerated, with the most common side effects being mild skin irritation at the electrode sites. TTFields represent a new modality that complements existing treatments without adding systemic toxicity. As ongoing research continues to refine protocols and expand indications, TTFields therapy could offer an additional, effective tool for patients with hard-to-treat lung cancers. Patients interested in this cutting-edge therapy should consult their oncologist about clinical trial availability and eligibility.
12. Artificial Intelligence in Imaging

Artificial intelligence (AI) is making a significant impact on lung cancer diagnostics by enhancing the accuracy and efficiency of imaging techniques. AI-powered algorithms can analyze CT scans with remarkable speed, identifying subtle nodules and abnormalities that might be missed by the human eye. These advanced systems are trained on vast datasets, enabling them to recognize early signs of lung cancer, measure tumor size, and evaluate changes over time with high precision.
Recent research, such as the study published in Nature Medicine, demonstrates that AI models can match or even surpass radiologists in detecting lung tumors and predicting malignancy. This early and accurate detection is crucial for improving patient prognosis, as it allows for timely intervention and increases the likelihood of successful treatment. AI also assists in reducing false positives, minimizing unnecessary biopsies and patient anxiety. As AI continues to integrate into clinical workflows, it promises to streamline the screening process and personalize patient care. Patients are encouraged to seek out facilities utilizing advanced imaging technologies, as these innovations offer new hope for earlier diagnosis and better outcomes in lung cancer management.
13. Circulating Tumor DNA Monitoring

Monitoring circulating tumor DNA (ctDNA) in blood samples has emerged as a powerful tool for tracking lung cancer progression and treatment response. ctDNA consists of small fragments of genetic material shed by tumor cells into the bloodstream, which can be detected and analyzed through non-invasive “liquid biopsy” techniques. By examining changes in ctDNA levels and specific genetic mutations, oncologists can gain real-time insights into how a patient’s cancer is responding to therapy or if the disease is evolving.
Recent studies, such as those reported in The New England Journal of Medicine, show that ctDNA monitoring can detect relapse or drug resistance earlier than conventional imaging. This allows for quicker adjustments to treatment plans, potentially improving outcomes and sparing patients from ineffective therapies. ctDNA analysis can also help identify minimal residual disease after surgery or other interventions, providing early warning signs of recurrence. As this technology advances, its integration into routine clinical practice is expected to facilitate more personalized and adaptive approaches to lung cancer care. Patients interested in ctDNA monitoring should discuss its availability and potential benefits with their oncology team.
14. KRAS G12C Inhibitors
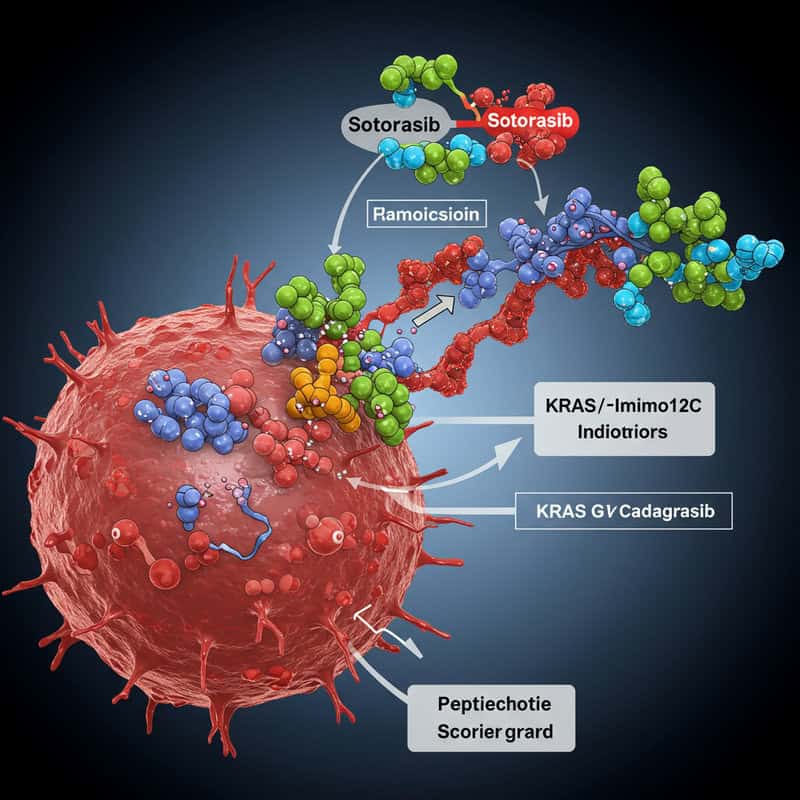
KRAS mutations, and particularly the KRAS G12C variant, have long been considered a challenging target in lung cancer therapy. Recent breakthroughs have led to the development of specific inhibitors, such as sotorasib and adagrasib, which are designed to selectively block the aberrant signaling caused by this mutation. These drugs bind to the mutant KRAS G12C protein, inhibiting its activity and thereby slowing or stopping cancer cell growth. This represents a major advancement for patients with non-small cell lung cancer (NSCLC) harboring this particular genetic alteration.
Clinical trials have shown promising results for these inhibitors. For example, the CodeBreaK 100 trial, detailed in the New England Journal of Medicine, reported meaningful tumor shrinkage and disease control in patients treated with sotorasib, many of whom had few other treatment options. KRAS G12C inhibitors have thus expanded the therapeutic landscape for a group that was previously considered largely untreatable with targeted therapies. As research continues, these drugs are being tested in combination with other agents to further enhance their effectiveness. Patients with lung cancer are encouraged to undergo molecular testing to determine eligibility for these innovative treatments.
15. Combination Immunotherapies

Combination immunotherapy regimens are providing new hope for lung cancer patients by leveraging the synergistic effects of multiple immune checkpoint inhibitors. By simultaneously targeting different pathways that tumors use to evade the immune system—such as PD-1/PD-L1 and CTLA-4—these combinations can unleash a more potent and comprehensive anti-tumor immune response. For example, nivolumab (a PD-1 inhibitor) and ipilimumab (a CTLA-4 inhibitor) have been studied together in the treatment of advanced non-small cell lung cancer (NSCLC).
Clinical trials, including the CheckMate 227 study published in the New England Journal of Medicine, have shown that dual immunotherapy can lead to improved survival rates and more durable responses compared to single-agent therapy or chemotherapy. These regimens may benefit patients with varying levels of PD-L1 expression and can sometimes be combined with chemotherapy for even greater efficacy. While combination immunotherapies can increase the risk of immune-related side effects, they offer a significant advance for patients who may not respond to monotherapy. Oncologists carefully assess each patient’s case to balance benefits and risks, ensuring the most effective and safe treatment strategy.
16. Adaptive Clinical Trial Designs
Adaptive clinical trial designs are transforming oncology research by introducing flexibility and efficiency into the evaluation of new lung cancer treatments. Unlike traditional trials that follow a fixed protocol from start to finish, adaptive designs allow for modifications—such as changes in dosage, patient selection, or even the addition or removal of treatment arms—based on interim results. This innovative approach accelerates the drug development process and enables researchers to identify promising therapies more quickly.
One notable example is the Lung-MAP trial, an umbrella study that uses adaptive methods to match patients with non-small cell lung cancer to targeted therapies based on their tumor’s genetic profile. According to the National Cancer Institute, adaptive designs have led to faster recruitment, more efficient use of resources, and earlier identification of effective treatments. This model is particularly valuable in the era of precision medicine, where numerous targeted agents and biomarkers are under investigation. For patients, adaptive trials may offer earlier access to cutting-edge therapies and a greater chance of receiving a treatment that matches their cancer’s unique characteristics. Patients should ask their oncologist about available clinical trials that use adaptive designs.
17. Oncolytic Virus Therapy
Oncolytic virus therapy is an innovative approach that utilizes genetically engineered viruses to selectively infect and destroy lung cancer cells while sparing healthy tissue. These oncolytic viruses are designed to replicate within tumor cells, causing them to rupture and die. In addition to directly killing cancer cells, this process releases tumor antigens that stimulate the patient’s immune system to mount a broader attack against the cancer.
Clinical trials have demonstrated the potential of oncolytic virus therapy in lung cancer. For example, research highlighted by the National Cancer Institute details how oncolytic viruses, such as modified adenoviruses and herpes simplex viruses, are being tested in combination with other immunotherapies to enhance their effectiveness. Early studies suggest that these therapies can improve immune recognition of tumors and may work synergistically with immune checkpoint inhibitors. While oncolytic virus therapy is still largely experimental in lung cancer, its promise lies in its dual action: direct tumor destruction and immune activation. Patients interested in participating in clinical trials involving oncolytic virus therapies should discuss eligibility and potential benefits with their oncology team, as this field continues to advance rapidly.
18. Lung Cancer Screening Programs

National lung cancer screening programs have become essential in the effort to detect the disease at earlier, more treatable stages. These initiatives often use low-dose computed tomography (LDCT), a sensitive imaging technique capable of identifying small lung nodules before symptoms arise. LDCT screening is especially recommended for high-risk individuals, such as adults aged 50-80 with a significant smoking history, as outlined by the Centers for Disease Control and Prevention.
Large-scale studies, such as the National Lung Screening Trial, have shown that LDCT screening can reduce lung cancer mortality by up to 20% compared to traditional chest X-rays. Early detection through screening enables curative treatments like surgery or stereotactic body radiotherapy to be offered before the cancer spreads. Many countries have implemented or are piloting national screening programs, aiming to reach populations at greatest risk and improve overall survival rates. Patients who meet screening criteria are urged to discuss the benefits and potential risks of LDCT with their healthcare provider. Widespread adoption of lung cancer screening is a critical step toward shifting diagnoses to earlier, more manageable stages and ultimately saving lives.
19. Adaptive Radiotherapy

Adaptive radiotherapy is an advanced approach that tailors radiation treatment plans in real time, responding to changes in tumor size, shape, and position during the course of therapy. Unlike conventional radiotherapy, which relies on a static plan, adaptive radiotherapy utilizes frequent imaging and sophisticated software to adjust the radiation dose and targeting for each session. This dynamic method ensures that the tumor receives the maximum possible dose while minimizing exposure to healthy tissues and organs at risk.
Recent advancements in imaging technology and artificial intelligence have made real-time adaptation feasible in clinical practice. According to research published in Frontiers in Oncology, adaptive radiotherapy has demonstrated improved tumor control and reduced side effects in lung cancer patients. This approach is particularly valuable for tumors that shrink or move significantly during the course of treatment, such as those located near the diaphragm. By continuously optimizing the treatment plan, adaptive radiotherapy offers more precise and effective care. Patients undergoing radiotherapy for lung cancer should ask their radiation oncologist about the availability and potential benefits of adaptive techniques as part of their personalized treatment strategy.
20. Telemedicine for Lung Cancer Care
Telemedicine has rapidly emerged as a vital component of lung cancer care, enabling patients to access expert consultations, second opinions, and routine follow-ups from the comfort of their homes. This technology-driven approach became especially prominent during the COVID-19 pandemic, but its benefits for lung cancer patients are enduring. Through secure video calls and digital health platforms, patients can discuss symptoms, treatment side effects, and medication management with their oncology team without the need for frequent in-person visits.
Studies, such as those published in JAMA Oncology, have shown that telemedicine maintains high levels of patient satisfaction and quality of care while reducing travel burdens and exposure risks—particularly important for those with compromised lung function. Telemedicine also supports multidisciplinary care coordination, allowing specialists from different locations to collaborate more efficiently. As healthcare systems invest in digital infrastructure, telemedicine is expected to remain a cornerstone of comprehensive lung cancer management. Patients should inquire about virtual care options and digital resources available through their treatment centers. This shift toward remote healthcare offers greater flexibility, improved access to specialists, and a more patient-centered approach in the ongoing fight against lung cancer.
21. PARP Inhibitors

PARP inhibitors are a class of drugs that target the enzyme poly (ADP-ribose) polymerase (PARP), which plays a key role in DNA repair within cells. By blocking PARP activity, these inhibitors prevent cancer cells from repairing the DNA damage caused by other treatments, such as chemotherapy or radiation, making the cancer cells more susceptible to destruction. While initially developed for cancers with specific genetic mutations like BRCA, PARP inhibitors are now being explored in lung cancer, particularly for tumors with deficiencies in DNA repair pathways.
Early-phase studies and ongoing clinical trials have shown that PARP inhibitors, such as olaparib and niraparib, can enhance the effectiveness of standard lung cancer therapies and may benefit patients with certain genetic backgrounds. Research summarized by the National Cancer Institute highlights how these drugs are often used in combination regimens to maximize their impact. As understanding of the molecular landscape of lung cancer grows, the role of PARP inhibitors continues to expand. Patients may be eligible for these innovative treatments if their tumors exhibit specific DNA repair gene alterations, making genetic testing a crucial step in personalized care.
22. Microbiome Modulation
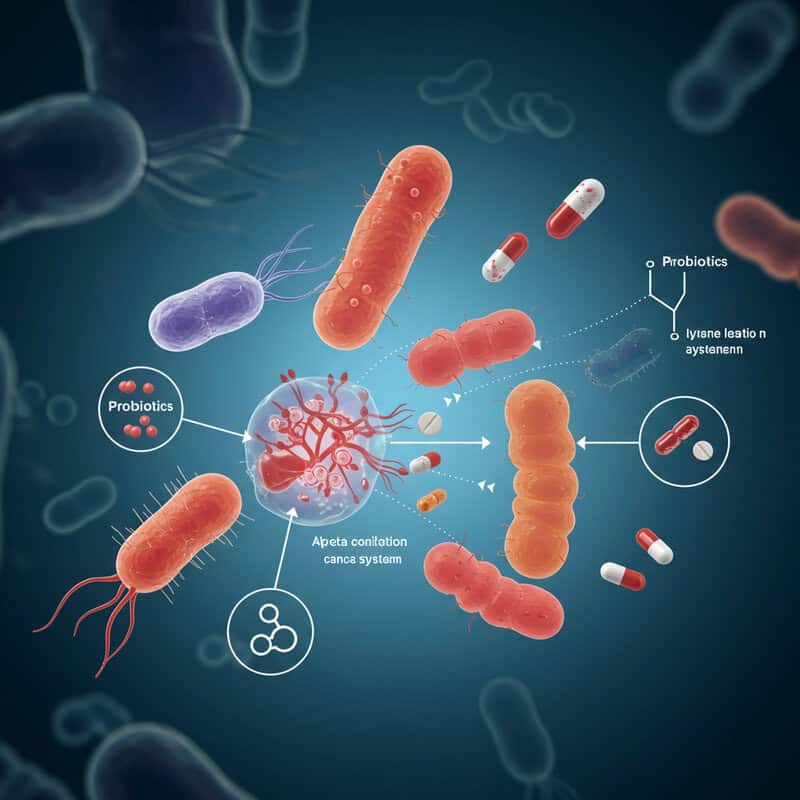
Emerging research suggests that the composition of gut bacteria, known as the microbiome, can significantly influence the effectiveness of lung cancer treatments, especially immunotherapy. The gut microbiome interacts with the immune system and may impact the body’s response to cancer and various therapies. Modulating the microbiome—through approaches such as probiotics, prebiotics, antibiotics, or even fecal microbiota transplantation—holds the potential to enhance the efficacy of immune checkpoint inhibitors and other lung cancer treatments.
Recent studies, including those highlighted in Cancer Currents by the National Cancer Institute, show that certain bacterial strains are associated with better clinical outcomes in patients receiving immunotherapy. Trials are underway to determine if deliberately altering the microbiome can boost treatment responses or reduce side effects. While this field is still in its early stages, the prospect of using microbiome modulation as an adjunct to standard therapies is exciting. Patients interested in microbiome-focused interventions should consult their oncology team before making changes, as the science continues to evolve. In the near future, strategies to optimize the gut microbiome may become an integral part of personalized lung cancer care.
23. Patient-Derived Organoids

Patient-derived organoids are an exciting innovation in lung cancer research and personalized medicine. These three-dimensional mini-tumors are grown in the laboratory from a patient’s own cancer cells, faithfully replicating the structure and genetic characteristics of the original tumor. Organoids allow researchers and clinicians to test various drug combinations and treatment strategies in a controlled environment, helping to identify therapies most likely to be effective for each individual patient.
Recent advancements have made it possible to establish lung cancer organoids quickly and efficiently, as highlighted in studies published in Nature Medicine. By observing how these organoids respond to different drugs, oncologists can tailor treatment plans, avoid ineffective therapies, and potentially improve outcomes. Organoids are also valuable for studying mechanisms of drug resistance and for accelerating the development of new therapeutics. While not yet routinely available in clinical practice, the use of patient-derived organoids is expanding rapidly, offering a glimpse into the future of truly individualized cancer care. Patients interested in this approach should inquire about ongoing clinical trials or research programs that utilize organoid technology for lung cancer treatment selection.
24. Real-Time Genomic Profiling

Real-time genomic profiling is transforming lung cancer care by enabling rapid analysis of tumor DNA during surgery or biopsy. Using advanced sequencing technologies, clinicians can obtain crucial genetic information within hours, rather than waiting days or weeks for traditional testing. This accelerated approach allows oncologists to identify actionable mutations—such as EGFR, ALK, or KRAS—on the spot, guiding immediate and personalized treatment decisions.
Rapid genomic testing has shown particular promise in the operating room, where surgeons and pathologists can collaborate closely to determine the most appropriate next steps. For example, a study published in Nature Medicine demonstrated that intraoperative genomic profiling could influence surgical margins, the extent of resection, or even the initiation of targeted therapies. This real-time information is especially valuable for patients with aggressive or advanced disease, as it minimizes delays in starting the most effective treatments. As technology advances, point-of-care genomic testing is expected to become more widely available, further personalizing lung cancer management. Patients should discuss the availability and benefits of rapid genomic profiling with their care team to ensure timely and optimal treatment strategies.
25. Wearable Health Monitoring Devices

Wearable health monitoring devices are increasingly integrated into the care of lung cancer patients, offering real-time tracking of vital health metrics such as heart rate, oxygen saturation, respiratory rate, and physical activity. These devices, which include smartwatches, fitness bands, and specialized medical sensors, provide continuous data that can alert patients and healthcare teams to potential complications or deteriorating health status.
Recent studies, such as those published in JCO Clinical Cancer Informatics, highlight the utility of wearables in detecting early signs of infection, respiratory distress, or adverse reactions to treatment. By enabling prompt intervention, these technologies can help prevent hospitalizations and improve overall outcomes. Wearables also support patient engagement, allowing individuals to monitor their own health trends and communicate more effectively with their providers. As wearable technology evolves, integration with telemedicine platforms and electronic health records is making remote monitoring even more seamless. Patients undergoing lung cancer treatment are encouraged to explore wearable device options with their care teams, as these tools represent a proactive approach to managing health, supporting early detection of complications, and enhancing quality of life throughout the cancer journey.
26. Peptide Receptor Radionuclide Therapy (PRRT)
Peptide Receptor Radionuclide Therapy (PRRT) is a targeted radiotherapy approach that delivers radioactive isotopes directly to lung tumors using peptides designed to bind specific receptors on cancer cells. This innovative therapy is especially promising for lung neuroendocrine tumors, which often overexpress somatostatin receptors. The peptides, labeled with radioactive agents such as lutetium-177, selectively attach to tumor cells, allowing for precise internal radiation delivery while minimizing exposure to healthy tissue.
Clinical evidence, such as studies referenced by the National Cancer Institute, demonstrates that PRRT can achieve significant tumor shrinkage and symptom relief, even in advanced or inoperable cases. Patients generally tolerate PRRT well, with fewer side effects compared to conventional external beam radiation. The targeted nature of the therapy also makes it suitable for treating widespread or metastatic disease. As PRRT gains regulatory approval for broader indications, its role in lung cancer management is expanding. Patients with neuroendocrine or receptor-positive tumors should consult their oncology team about eligibility for PRRT, as it represents a promising option for those seeking more precise and effective radiotherapeutic interventions.
27. Minimally Invasive Lung Biopsy Techniques
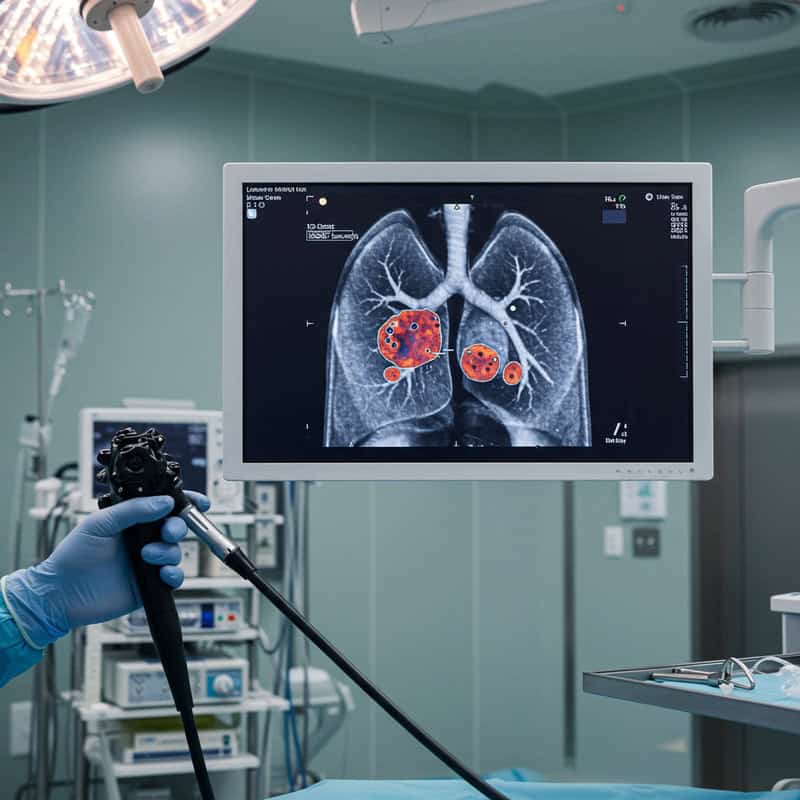
Advanced, minimally invasive biopsy techniques are significantly improving the safety and accuracy of lung cancer diagnosis. Navigational bronchoscopy, also known as electromagnetic navigation bronchoscopy (ENB), enables physicians to reach and sample small or hard-to-access lung nodules using a flexible bronchoscope guided by real-time 3D imaging and GPS-like technology. This approach minimizes the risk of complications, such as lung collapse or bleeding, especially when compared to traditional needle biopsies or surgical procedures.
Recent advancements, as highlighted by The New England Journal of Medicine, show that navigational bronchoscopy increases diagnostic yield and enables molecular profiling from even tiny lesions. This is crucial for guiding personalized treatment decisions based on genetic testing. Other minimally invasive methods, such as endobronchial ultrasound (EBUS), further enhance access to lymph nodes and peripheral lung tumors. Patients experience less discomfort, shorter recovery times, and fewer complications, making these procedures ideal for those with limited respiratory reserve or other health conditions. Individuals undergoing evaluation for lung cancer should ask their healthcare team about the availability and suitability of these advanced biopsy techniques, which are setting new standards in diagnostic safety and precision.
28. Chimeric Antigen Receptor (CAR) T-cell Therapy
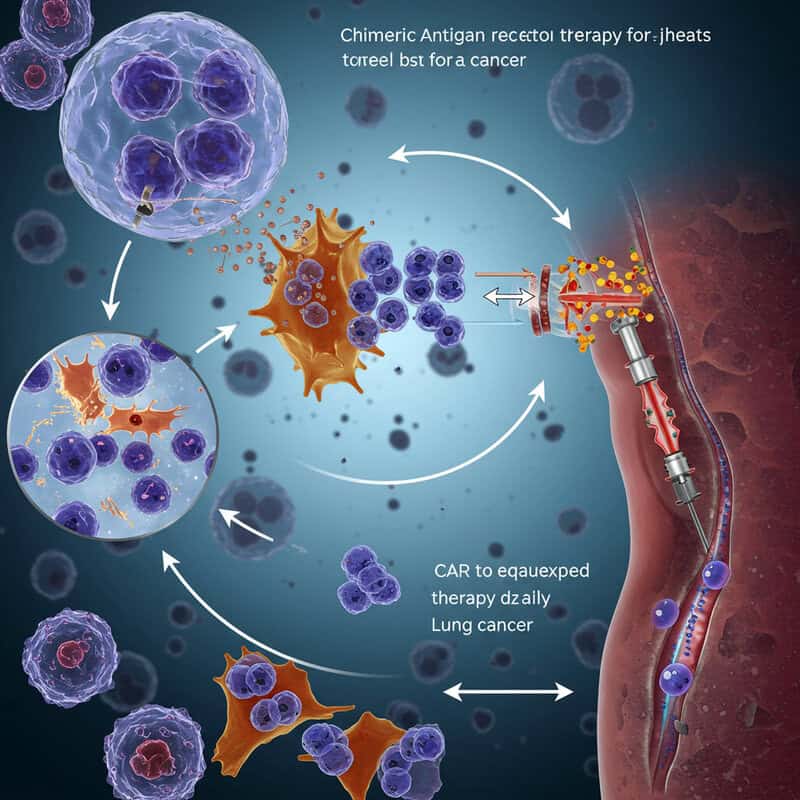
Chimeric Antigen Receptor (CAR) T-cell therapy is a groundbreaking immunotherapy originally developed for blood cancers and now being adapted for solid tumors such as lung cancer. This technique involves collecting a patient’s own T cells, genetically engineering them in the laboratory to express special receptors (CARs) that recognize specific proteins on the surface of lung cancer cells, and then reinfusing these “supercharged” cells back into the patient. Once in the body, the CAR T-cells seek out and destroy cancer cells with high precision.
Early-phase clinical trials, as highlighted by the National Cancer Institute, are exploring various CAR designs and target antigens suitable for lung cancer. While challenges such as the immunosuppressive tumor microenvironment and potential side effects remain, initial results are encouraging, showing tumor shrinkage and durable responses in some patients. Researchers are also investigating combination approaches to enhance CAR T-cell activity and persistence in solid tumors. As development continues, CAR T-cell therapy could offer a highly personalized and potent option for patients with refractory or advanced lung cancer. Participation in clinical trials is recommended for those interested in accessing this innovative treatment.
29. Exosome-Based Diagnostics
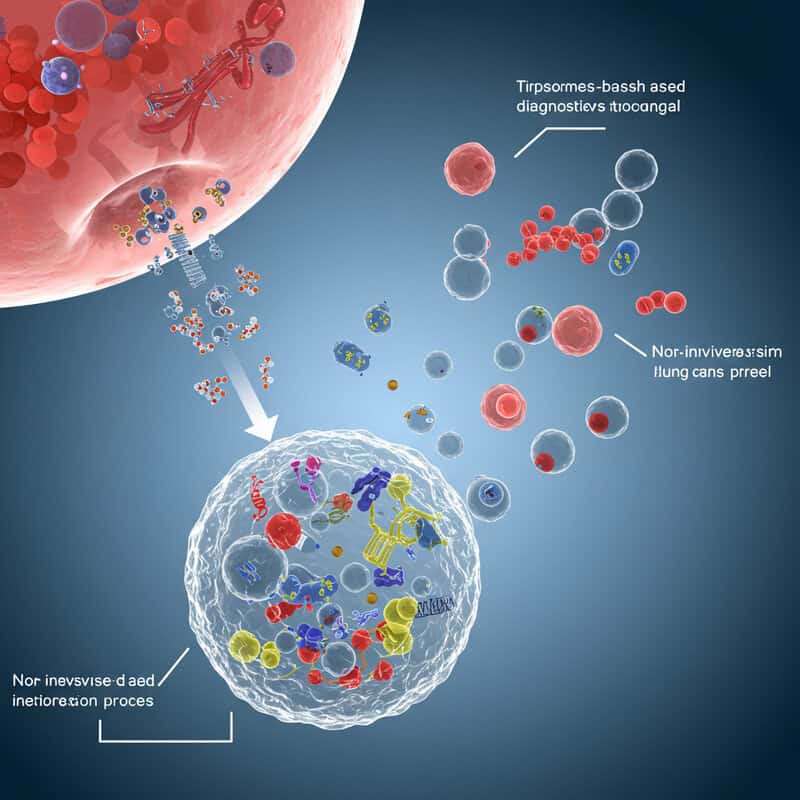
Exosome-based diagnostics represent a promising advance in the non-invasive detection and monitoring of lung cancer. Exosomes are tiny, membrane-bound vesicles released by cells—including cancer cells—into the bloodstream. These vesicles contain a variety of molecular cargo, such as DNA, RNA, proteins, and lipids, which reflect the biological status of their cell of origin. By analyzing the contents of exosomes in blood samples, clinicians can gain valuable information about the presence and characteristics of lung tumors without the need for invasive tissue biopsies.
Recent studies, such as those reviewed in Nature Reviews Genetics, have demonstrated the potential of exosome-based tests to detect lung cancer at an early stage, monitor disease progression, and identify resistance to therapies. These tests offer advantages in terms of patient comfort, repeatability, and the ability to provide a comprehensive molecular profile of the tumor. As the technology matures, exosome-based diagnostics are expected to complement or even supersede some current liquid biopsy approaches. Patients and providers can look forward to a future where regular, non-invasive blood tests play a central role in the early diagnosis and personalized management of lung cancer.
30. Tumor Mutation Burden Testing

Tumor Mutation Burden (TMB) testing is an emerging biomarker strategy that measures the total number of mutations present within a tumor’s DNA. This information is crucial in lung cancer, as tumors with a high mutation burden tend to produce more abnormal proteins (neoantigens) that can be recognized by the immune system. High TMB has been associated with a greater likelihood of response to immunotherapies, particularly immune checkpoint inhibitors.
Several clinical studies, including those referenced by the National Cancer Institute, have shown that patients with high TMB in non-small cell lung cancer are more likely to benefit from immunotherapy treatments such as pembrolizumab or nivolumab. TMB testing can be performed using next-generation sequencing on tumor tissue or even through blood-based liquid biopsies, making it accessible in various clinical scenarios. Understanding a patient’s TMB helps oncologists tailor treatment strategies and select those most likely to respond to immunotherapy. As research continues, TMB is becoming an integral part of precision oncology, guiding both clinical trial enrollment and routine care decisions for lung cancer patients seeking the most effective therapies.
31. Personalized Smoking Cessation Programs

Personalized smoking cessation programs are a vital component of comprehensive lung cancer care, as continued smoking can hinder treatment effectiveness and worsen outcomes. These tailored interventions go beyond generic advice by considering each patient’s smoking history, preferences, psychological factors, and readiness to quit. Programs may include behavioral counseling, pharmacotherapy (such as nicotine replacement, varenicline, or bupropion), and ongoing support, all customized to maximize the chances of long-term abstinence.
Research, including findings published by the American Cancer Society, demonstrates that patients who quit smoking after a lung cancer diagnosis experience improved response to therapy, reduced complications, and longer survival. Many cancer centers now offer integrated cessation services as part of routine oncology care, using motivational interviewing and digital tools like mobile apps or telehealth to support patients remotely. Personalized programs recognize the unique challenges faced by lung cancer patients, including nicotine dependence and the emotional burden of diagnosis. Patients are encouraged to discuss available cessation resources with their care team, as quitting smoking at any stage can lead to significant health benefits, improved quality of life, and better treatment outcomes.
32. Digital Pathology and AI Analysis

Digital pathology, combined with artificial intelligence (AI) analysis, is rapidly transforming the diagnosis and classification of lung cancer. Traditional pathology relies on manual examination of tissue slides under a microscope, which can be time-consuming and subject to variability. Digital pathology digitizes these slides, allowing high-resolution images to be stored, shared, and analyzed on computers. AI algorithms can then process these images, identifying subtle features and patterns that may be missed by the human eye.
Recent advancements, such as those reported in Nature Medicine, show that AI-powered pathology systems can assist in distinguishing between lung cancer subtypes, grading tumor aggressiveness, and even predicting genetic mutations based on tissue morphology. This technology speeds up diagnostic workflows, reduces errors, and enables more precise, personalized treatment planning. Digital pathology also facilitates remote consultations and second opinions, making expert pathology services more widely accessible. As AI models continue to improve and integrate with electronic health records, digital pathology is poised to become a cornerstone of modern lung cancer care, offering faster turnaround times and enhanced diagnostic accuracy for patients and clinicians alike.
33. Inhaled Chemotherapy

Inhaled chemotherapy is an innovative approach that delivers anti-cancer drugs directly to the lung tissues via inhalation, aiming to maximize the concentration of medication at the tumor site while minimizing systemic exposure and side effects. This method utilizes nebulizers or inhalers to transform chemotherapy agents into fine aerosols, which patients breathe in, allowing the drugs to reach deep into the lungs where cancer cells reside.
Early-phase clinical trials and feasibility studies, such as those discussed in Translational Lung Cancer Research, have shown promising results regarding the safety and localized effectiveness of inhaled chemotherapy. By reducing systemic absorption, patients often experience fewer common side effects like nausea, hair loss, or immune suppression compared to intravenous chemotherapy. This targeted delivery is particularly advantageous for early-stage lung cancers or localized recurrences and may be combined with other treatments for enhanced outcomes. Researchers are also exploring nanoparticle-based formulations and novel drug carriers to further improve drug deposition and retention in lung tissues. Although not yet standard practice, inhaled chemotherapy represents a forward-thinking strategy for improving the tolerability and precision of lung cancer treatment.
34. Non-Invasive Respiratory Function Monitoring

Non-invasive respiratory function monitoring is revolutionizing the way lung cancer patients manage their respiratory health and detect complications early. New digital tools, including portable spirometers, smart inhalers, and wearable respiratory sensors, allow for continuous or regular at-home assessment of vital parameters such as lung capacity, airflow, oxygen saturation, and respiratory rate. These devices transmit data wirelessly to healthcare teams, enabling prompt intervention if any concerning trends or abnormalities are detected.
Studies, such as those highlighted by Frontiers in Digital Health, demonstrate that remote respiratory monitoring can help identify early signs of infection, treatment-related lung toxicity, or worsening pulmonary function—conditions that require immediate clinical attention. This proactive approach reduces unnecessary hospital visits, supports timely medication adjustments, and empowers patients to play an active role in their own care. Non-invasive monitoring also provides reassurance for patients undergoing surgery, chemotherapy, or radiotherapy, as clinicians can closely track recovery and intervene before complications escalate. As technology continues to advance, these remote monitoring solutions are expected to become a standard part of comprehensive lung cancer management, improving safety, outcomes, and quality of life for patients at every stage of treatment.
35. mRNA-Based Cancer Therapies
mRNA-based cancer therapies are at the forefront of innovative biomedical research, utilizing messenger RNA (mRNA) technology to instruct the body’s own cells to produce proteins that target and fight lung cancer. Much like mRNA vaccines developed for COVID-19, these therapies deliver synthetic mRNA sequences encoding tumor-specific antigens or immune-activating proteins directly into cells. Once inside, the cells translate the mRNA into proteins that can stimulate a robust immune response against cancer cells or disrupt tumor growth processes.
Recent clinical trials and preclinical studies, such as those discussed in Nature Reviews Drug Discovery, highlight promising results for mRNA-based vaccines and therapeutics in lung cancer. These therapies offer the advantages of rapid development, customization to a patient’s unique tumor mutations, and the ability to induce both cellular and antibody-mediated immunity. Researchers are also investigating mRNA platforms for delivering cytokines, checkpoint inhibitors, and other cancer-fighting proteins directly to the tumor microenvironment. While still in the early stages for lung cancer, mRNA-based therapies hold great potential for highly personalized, adaptable treatment strategies that can complement existing modalities and address drug resistance or tumor heterogeneity.
36. Photodynamic Therapy
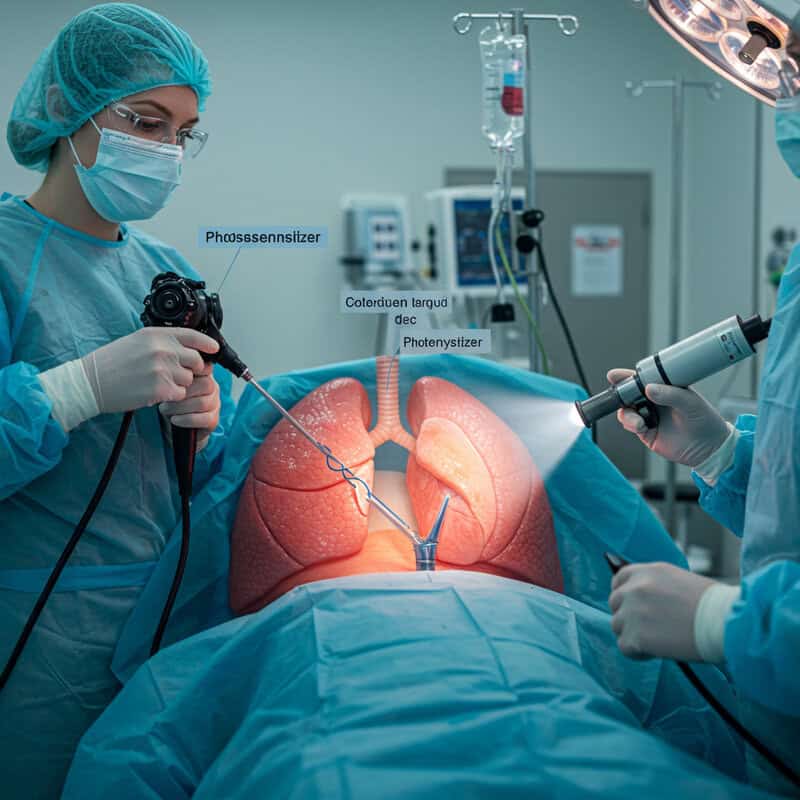
Photodynamic therapy (PDT) is a minimally invasive treatment that uses light-activated drugs, known as photosensitizers, to selectively destroy lung cancer cells. After the photosensitizer is administered—either intravenously or directly to the lung—it accumulates preferentially in tumor tissue. When the targeted area is exposed to a specific wavelength of light, usually delivered via a bronchoscope or optical fiber, the drug is activated, producing reactive oxygen species that damage and kill cancer cells while sparing healthy tissue.
PDT is particularly effective for small, localized tumors, or early-stage non-small cell lung cancer, and is also used to relieve airway obstruction caused by tumor growth. Research summarized by the American Cancer Society shows that PDT can achieve tumor shrinkage, improve breathing, and reduce symptoms with fewer side effects compared to traditional therapies. Limitations include restricted penetration depth of the activating light and the need for careful patient selection, but ongoing advances in photosensitizer development may expand its use. Patients considering PDT should consult their oncology and pulmonary teams to determine suitability, as this therapy offers a non-surgical, organ-sparing option for select cases of lung cancer.
37. Pathology AI for Mutation Detection
Artificial intelligence (AI) is transforming the field of pathology by enabling rapid and accurate identification of genetic mutations directly from digital tumor slides. Advanced AI algorithms are trained on thousands of annotated pathology images, allowing them to recognize subtle morphological patterns that correspond to specific gene alterations such as EGFR, ALK, KRAS, and others. This technology streamlines the diagnostic process, allowing oncologists to quickly match lung cancer patients with the most effective targeted therapies.
Recent studies, including those published in Nature Medicine, demonstrate that AI-powered pathology systems can predict the presence of actionable mutations with high accuracy, sometimes even before confirmatory molecular testing is complete. By reducing turnaround time and ensuring no key mutations are overlooked, these tools help optimize treatment decisions and improve patient outcomes. AI-driven mutation detection also supports large-scale screening efforts and resource-limited settings where access to comprehensive genomic testing may be restricted. As integration with digital pathology platforms becomes more widespread, AI for mutation detection is poised to play a pivotal role in personalized lung cancer care, ensuring the right therapy reaches the right patient as quickly as possible.
38. Clinical Decision Support Systems

Clinical Decision Support Systems (CDSS) powered by artificial intelligence are rapidly becoming indispensable tools in the management of lung cancer. These sophisticated platforms integrate vast amounts of patient data—including clinical history, imaging, pathology, genomics, and treatment response—to provide evidence-based recommendations for personalized care. By analyzing up-to-date research, guidelines, and real-world outcomes, AI-powered CDSS can assist clinicians in selecting the most effective therapies, anticipating side effects, and identifying patients eligible for clinical trials.
Recent developments, such as those discussed in Frontiers in Oncology, illustrate how these systems help reduce diagnostic errors, standardize treatment protocols, and streamline multidisciplinary team discussions. CDSS can also flag potential drug interactions and contraindications, enhancing patient safety. As lung cancer treatment options expand and become increasingly complex, these digital tools offer clinicians timely insights and support shared decision-making with patients. Ongoing improvements in AI, data integration, and user interface design promise even greater utility in the future. Patients may benefit from asking their care teams if CDSS are used in their treatment planning, as these innovations help ensure that every clinical decision is informed by the latest evidence and tailored to individual needs.
39. Enhanced Recovery After Surgery (ERAS) Pathways

Enhanced Recovery After Surgery (ERAS) pathways are specialized, multidisciplinary protocols designed to improve outcomes and accelerate recovery for lung cancer patients undergoing surgery. These evidence-based programs incorporate strategies before, during, and after the surgical procedure to reduce complications, minimize hospital stays, and enhance overall patient well-being. Components of ERAS protocols include preoperative education, optimal pain management with minimal reliance on opioids, early mobilization, nutritional support, and minimally invasive surgical techniques whenever possible.
Research highlighted by the Journal of Thoracic Disease demonstrates that ERAS pathways can significantly lower rates of postoperative complications such as pneumonia, deep vein thrombosis, and prolonged air leak. Patients following ERAS protocols tend to experience less pain, regain mobility sooner, and return to normal activities more quickly than those receiving standard care. These pathways are tailored to individual patient needs and involve close collaboration among surgeons, anesthesiologists, nurses, physiotherapists, and nutritionists. Patients scheduled for lung cancer surgery should inquire about the availability of ERAS protocols at their treatment center, as participation in such programs can lead to a safer, smoother, and more positive surgical experience.
40. Proton Beam Therapy
Proton beam therapy is an advanced form of radiation treatment that uses high-energy protons instead of traditional X-rays to target and destroy lung cancer cells. The unique physical properties of protons allow them to deposit their maximum energy directly at the tumor site—a phenomenon known as the Bragg peak—while minimizing radiation exposure to surrounding healthy lung tissue and critical structures, such as the heart and esophagus.
This precision makes proton therapy especially valuable for patients with tumors located near sensitive areas or for those who have previously received radiation. According to research published by the National Cancer Institute, proton beam therapy can reduce the risk of treatment-related side effects, such as lung inflammation, heart damage, and secondary cancers, compared to conventional photon-based radiation. Clinical studies also suggest comparable or improved tumor control rates in both early-stage and locally advanced lung cancer. As more proton therapy centers become available worldwide, patients should discuss with their oncologist whether this high-precision modality is an appropriate option for their specific diagnosis. Access to proton therapy may vary, but its potential to enhance outcomes while preserving quality of life continues to drive its adoption in modern lung cancer care.
41. Personalized Nutrition Interventions

Personalized nutrition interventions are increasingly recognized as a crucial element in the comprehensive care of lung cancer patients. Malnutrition and weight loss are common challenges during cancer treatment, often due to reduced appetite, treatment side effects, or disease-related metabolic changes. Tailored nutrition plans, developed by oncology dietitians, address each patient’s unique needs, preferences, and medical conditions to help maintain strength, support immune function, and improve overall quality of life.
Evidence, including guidelines from the American Cancer Society, emphasizes the importance of providing adequate calories, protein, vitamins, and fluids, while also managing symptoms like nausea, taste changes, or difficulty swallowing. Personalized interventions may involve oral supplements, meal planning, and strategies for coping with side effects to ensure optimal nutritional intake. For patients undergoing surgery, chemotherapy, or radiation, individualized nutrition support has been shown to reduce complications, speed recovery, and enhance tolerance to treatment. Patients are encouraged to seek guidance from registered dietitians specializing in oncology, as early and proactive nutrition management can make a significant difference in treatment outcomes and day-to-day well-being throughout the lung cancer journey.
42. Tumor Board Virtual Collaboration

Virtual tumor board collaboration is transforming the management of complex lung cancer cases by enabling real-time, multidisciplinary discussions regardless of geographical barriers. These digital meetings bring together oncologists, radiologists, pathologists, surgeons, pulmonologists, and other specialists to review patient histories, imaging, pathology, and genetic data. Using secure teleconferencing platforms, experts from different locations can collectively evaluate challenging cases, offer diverse perspectives, and reach consensus on the best diagnostic and treatment strategies.
Research highlighted by Cancer Network demonstrates that virtual tumor boards improve the quality and consistency of care, accelerate decision-making, and increase access to subspecialty expertise—especially valuable for patients in remote or underserved areas. These virtual collaborations also support ongoing education and the rapid adoption of new evidence-based practices. For lung cancer patients, participation in cases reviewed by a multidisciplinary tumor board can mean more comprehensive evaluations and personalized treatment recommendations. Patients should ask their care team if their case will be discussed in a tumor board setting, as this approach is increasingly recognized as a gold standard for delivering coordinated, high-quality lung cancer care in the digital age.
43. Adaptive Dosing Algorithms
Adaptive dosing algorithms are revolutionizing medication management for lung cancer patients by using automated systems to tailor drug dosages in real time. These advanced algorithms integrate patient-specific data—such as lab results, genetic markers, side effect profiles, and therapeutic response—to dynamically adjust treatment regimens. This personalized approach ensures optimal drug exposure, maximizes therapeutic benefits, and minimizes the risk of adverse effects.
Recent research, such as that published in JCO Clinical Cancer Informatics, demonstrates the value of adaptive dosing in oncology, highlighting its ability to improve drug tolerability and clinical outcomes. For lung cancer therapies with narrow therapeutic windows or significant toxicity risks, these systems offer an extra layer of safety. Algorithms may be embedded within electronic health records or linked to wearable devices for continuous monitoring, enabling rapid dose modifications based on real-world patient data. As adaptive dosing technology becomes more sophisticated, it is expected to play a key role in the delivery of precision medicine. Lung cancer patients should discuss with their care teams whether adaptive dosing tools are available, as these systems can support more effective, individualized treatment with fewer complications.
44. Comprehensive Genomic Tumor Boards

Comprehensive genomic tumor boards are specialized multidisciplinary meetings where expert teams review full genomic profiles of lung cancer patients to design highly personalized care plans. These boards typically include oncologists, pathologists, geneticists, bioinformaticians, and pharmacists who analyze extensive data from next-generation sequencing and other molecular tests. By interpreting a patient’s unique tumor mutations, copy number variations, and gene expression patterns, the team can match individuals with targeted therapies, immunotherapies, or relevant clinical trials.
As described in research from the National Cancer Institute, genomic tumor boards help ensure that even rare or complex genetic findings are thoroughly evaluated and optimally translated into treatment recommendations. This collaborative approach accelerates the adoption of precision medicine and fosters continual learning among clinicians. It also improves patient access to novel and investigational therapies, which may not be considered during standard case reviews. Patients with advanced or treatment-resistant lung cancer are encouraged to inquire whether their case may be presented at a genomic tumor board, as this process can provide additional options and insights, ultimately leading to more effective and individualized lung cancer management.
45. Remote Symptom Monitoring Apps
Remote symptom monitoring apps are transforming lung cancer care by enabling patients to report symptoms, side effects, and general health concerns in real time using their smartphones or tablets. These digital tools allow patients to log data such as pain, shortness of breath, cough, fatigue, or medication side effects from home, which is then transmitted directly to their healthcare team. Clinicians can review the information promptly, identify concerning trends, and intervene early—often before symptoms escalate to require emergency care or hospitalization.
Research published in JAMA Oncology demonstrates that remote symptom monitoring can improve quality of life, reduce complications, and even extend survival for cancer patients. These apps often include features such as reminders, educational content, and direct messaging with care providers, further supporting patient engagement and empowerment. As digital health platforms continue to evolve, integration with electronic health records and wearable devices is making remote monitoring even more effective. Lung cancer patients are encouraged to ask their oncology team about available symptom monitoring tools, as these apps represent a proactive approach to managing side effects, ensuring timely interventions, and enhancing the overall treatment experience.
46. Real-World Evidence Studies

Real-world evidence (RWE) studies are increasingly shaping the landscape of lung cancer treatment by analyzing data collected from actual patient experiences outside the controlled environment of clinical trials. These large-scale studies draw on sources such as electronic health records, cancer registries, insurance claims, and patient-reported outcomes to evaluate how therapies perform in everyday practice. RWE provides crucial insights into the effectiveness, safety, and tolerability of treatments across diverse populations, including those often underrepresented in traditional trials.
As detailed by the U.S. Food and Drug Administration, RWE can reveal patterns in survival, treatment adherence, and side effects that may not emerge in randomized clinical studies. This evidence helps clinicians refine treatment guidelines, inform regulatory decisions, and personalize therapy selection for individuals with lung cancer. RWE is also valuable for assessing new therapies, rare tumor subtypes, and long-term patient outcomes. Lung cancer patients may benefit from participating in data-sharing initiatives and registries, as their experiences contribute to the broader understanding and continuous improvement of cancer care in real-world settings.
47. Tumor-Infiltrating Lymphocyte Therapy
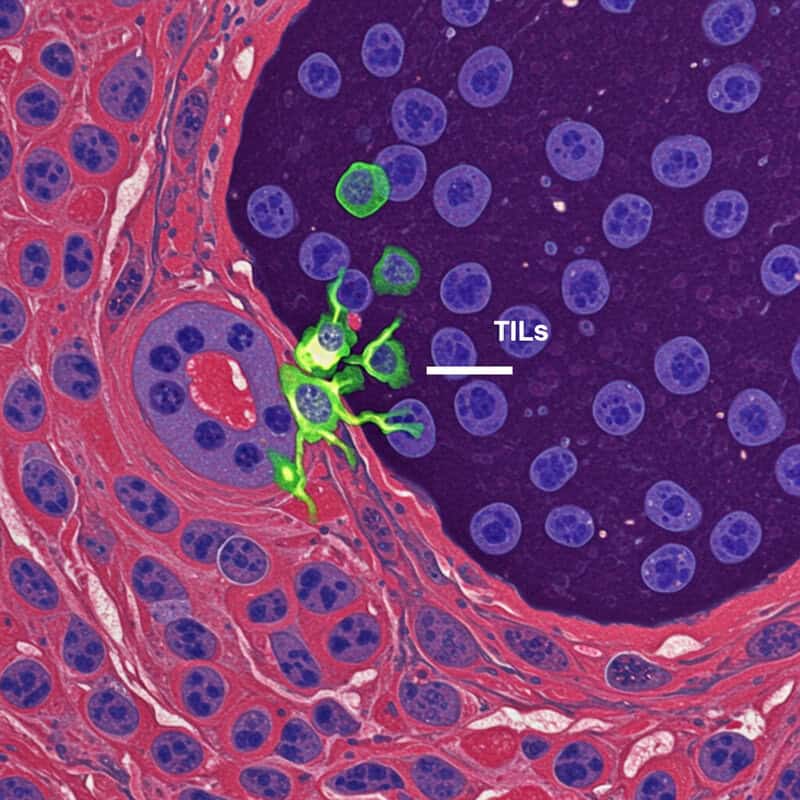
Tumor-infiltrating lymphocyte (TIL) therapy is an innovative form of adoptive cell therapy that harnesses a patient’s own immune system to target and destroy lung cancer cells. The process begins by isolating TILs—immune cells that have naturally migrated into a patient’s tumor—during surgery or biopsy. These TILs are then expanded and activated in the laboratory to generate large numbers, after which they are infused back into the patient, often following a preparative regimen to enhance their effectiveness.
Early research, such as studies summarized by the National Cancer Institute, indicates that TIL therapy can induce durable responses in some patients with solid tumors, including lung cancer, particularly when other treatments have failed. The infused lymphocytes are primed to recognize and attack cancer cells, offering a highly personalized therapeutic approach. Clinical trials are underway to refine this technique and explore combinations with other immunotherapies for even greater efficacy. While still experimental, TIL therapy represents a promising avenue for patients with treatment-resistant or advanced lung cancer. Interested patients should consult their oncology team about eligibility for ongoing TIL therapy trials and its potential role in their care.
48. Nanoparticle Drug Delivery

Nanoparticle drug delivery is an innovative strategy designed to enhance the precision and efficacy of lung cancer treatments by packaging chemotherapy or targeted agents into ultra-small carriers. These nanoparticles, often engineered from lipids, polymers, or proteins, can be tailored to recognize and bind specifically to lung tumor cells. Once at the tumor site, nanoparticles release their drug payload directly into the cancerous tissue, maximizing therapeutic impact while minimizing exposure to healthy cells.
Studies, such as those summarized in Nature Nanotechnology, show that nanoparticle-based therapies can improve drug solubility, prolong circulation time, and allow for controlled, sustained drug release. This targeted approach reduces common side effects associated with conventional chemotherapy—such as nausea, hair loss, and immune suppression—while increasing drug concentrations at the tumor. Nanoparticles are also being investigated as carriers for gene therapies, immunomodulators, and imaging agents, further expanding their potential. As research advances, nanoparticle drug delivery is expected to play a growing role in personalized lung cancer care, offering hope for more effective treatments with improved tolerability, especially for patients with aggressive or drug-resistant tumors.
49. Lung Cancer Survivorship Programs

Lung cancer survivorship programs are structured initiatives designed to address the unique needs of individuals who have completed active treatment and are transitioning into long-term recovery. These multidisciplinary programs provide ongoing medical monitoring to detect cancer recurrence early, manage late or lingering side effects, and support physical and emotional well-being. Survivorship care plans often include regular follow-up visits, imaging tests, and assessments of lung function, as well as strategies for managing fatigue, pain, and respiratory symptoms.
Beyond medical surveillance, survivorship programs focus on improving quality of life by offering resources for nutrition, exercise, smoking cessation, mental health counseling, and social support. According to the American Cancer Society, these comprehensive services help survivors cope with anxiety about recurrence, rebuild strength, and navigate the challenges of returning to work or daily activities. Some programs also connect survivors with peer support groups and educational workshops. Participation in a dedicated survivorship program ensures that lung cancer survivors receive holistic, patient-centered care tailored to their ongoing needs, promoting optimal health and well-being throughout the post-treatment journey.
50. Policy Advocacy and Awareness Initiatives

Policy advocacy and awareness initiatives play a critical role in advancing lung cancer research, improving patient access to care, and reducing stigma associated with the disease. National and international campaigns, such as those led by the American Lung Association’s LUNG FORCE, focus on increasing public understanding of lung cancer risk factors, screening benefits, and the importance of early detection. These efforts strive to dispel misconceptions and emphasize that lung cancer affects people of all backgrounds—not just smokers.
Advocacy organizations work with policymakers to secure increased funding for lung cancer research, expand insurance coverage for screening and advanced therapies, and promote equitable access to care for underserved communities. Policy initiatives may also address tobacco control, air quality, and workplace safety regulations to reduce lung cancer incidence. Awareness months, educational events, and survivor stories further amplify the message, empowering patients and families to seek timely care and support. According to the National Cancer Institute, ongoing advocacy is essential for driving policy changes that improve outcomes, foster innovation, and ensure all individuals affected by lung cancer receive the resources and attention they deserve.
Conclusion

Rapid advances in lung cancer treatment are transforming patient care, offering new hope through innovative diagnostics, personalized therapies, and comprehensive support programs. Despite these breakthroughs, lung cancer remains a leading cause of cancer mortality, emphasizing the urgency of early detection and intervention. Individuals at risk—particularly those with a history of smoking or exposure to lung carcinogens—should prioritize regular screening and remain vigilant for symptoms such as persistent cough or unexplained weight loss. Timely consultation with healthcare professionals is essential for optimal outcomes. For more information on risks and screening, visit the CDC’s lung cancer screening resources.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





