Natural Ways to Improve Your Insulin Sensitivity
Insulin resistance is on the rise globally, with over 537 million adults living with diabetes as of 2021, a number projected to reach 643 million by 2030 (International Diabetes Federation). Insulin, a hormone produced by the pancreas, plays a vital role in regulating blood sugar levels. Unfortunately, insulin resistance often develops silently and is detected late, increasing the risk of type 2 diabetes and related complications. Exploring natural strategies to enhance insulin sensitivity can help prevent or delay the onset of these chronic conditions.
1. Increase Physical Activity

Regular physical activity is a cornerstone for enhancing insulin sensitivity. Exercise stimulates muscles to absorb glucose from the bloodstream, reducing blood sugar levels and lowering insulin demand. Both aerobic activities—such as brisk walking, cycling, or swimming—and resistance training, like weightlifting or bodyweight exercises, significantly improve insulin action. Research shows that combining both aerobic and resistance training offers the most profound benefits (National Institutes of Health).
For beginners, starting with 150 minutes of moderate-intensity aerobic exercise per week, along with two sessions of strength training, is recommended (CDC). Simple changes, such as taking the stairs, walking during lunch breaks, or using resistance bands at home, can make a significant difference. The key is consistency and gradually increasing intensity and duration. Regardless of age or fitness level, regular movement helps the body use insulin more efficiently and can substantially reduce the risk of insulin resistance and diabetes.
2. Choose Whole Grains Over Refined Carbs
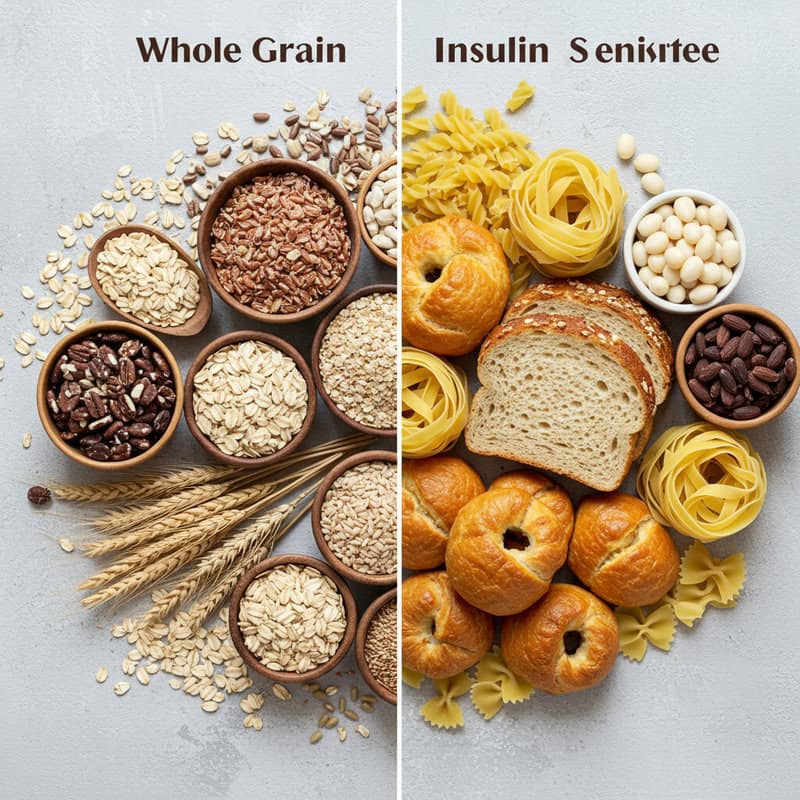
Whole grains have a positive impact on blood sugar control and insulin sensitivity, largely due to their high fiber and nutrient content. Unlike refined carbohydrates, which are stripped of fiber and key nutrients during processing, whole grains release glucose more slowly into the bloodstream, preventing rapid spikes in blood sugar and insulin levels. Studies indicate that diets rich in whole grains are associated with lower rates of insulin resistance and type 2 diabetes (Harvard T.H. Chan School of Public Health).
Refined carbs, such as white bread, pastries, and many breakfast cereals, cause quick sugar surges that challenge the body’s insulin response. In contrast, whole grains like brown rice, quinoa, oats, barley, and whole wheat bread support steadier glucose levels. To make healthier choices, consider swapping white rice for brown or wild rice, choosing whole wheat or sprouted grain bread instead of white, and opting for steel-cut oats over instant varieties. Simple substitutions like these can make a meaningful difference in your body’s ability to manage blood sugar and improve insulin sensitivity over time.
3. Manage Stress Levels
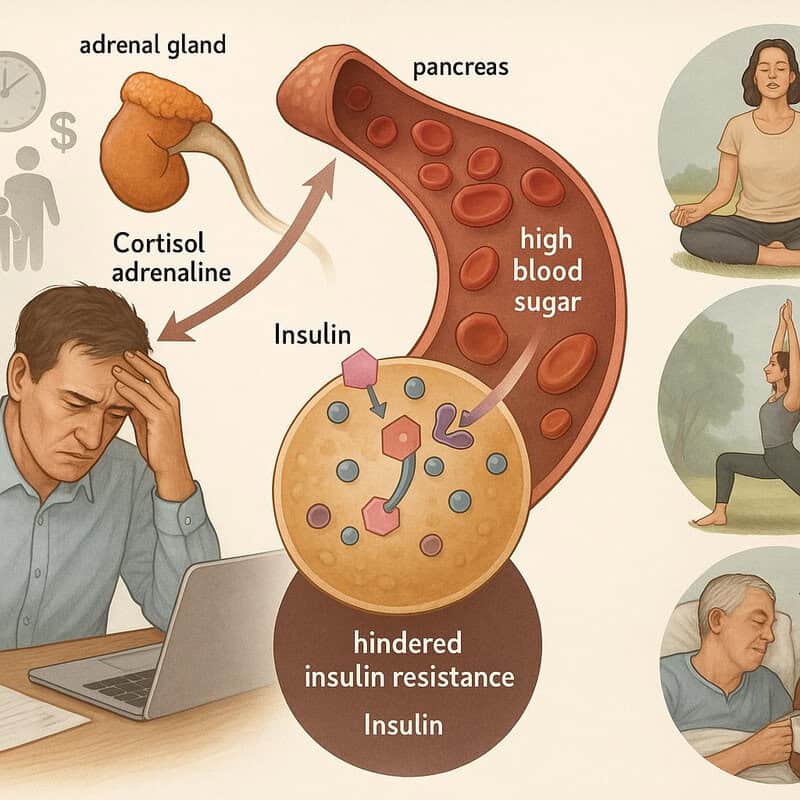
Chronic stress is closely linked to increased insulin resistance. When you experience stress, your body releases hormones like cortisol and adrenaline, which can temporarily raise blood sugar levels. Over time, persistently high cortisol can hinder insulin’s effectiveness, making it more difficult for cells to absorb glucose (National Institutes of Health). For example, juggling work deadlines, family responsibilities, and financial worries can keep your body in a prolonged state of stress, contributing to higher blood sugar and insulin resistance.
Incorporating daily stress-reducing activities can help counteract these effects. Mindfulness practices such as meditation and deep breathing exercises have been shown to lower stress hormones and improve insulin sensitivity. Physical activities like yoga, tai chi, or even a brisk walk in nature can also be effective. Additionally, setting aside time for hobbies, connecting with supportive friends or family, and ensuring adequate sleep are crucial steps. Making stress management a regular part of your routine not only benefits your mental well-being but also supports healthier blood sugar and insulin responses.
4. Prioritize Quality Sleep

Getting enough high-quality sleep is essential for optimal insulin function. Sleep deprivation or poor sleep quality disrupts the body’s hormonal balance, leading to decreased insulin sensitivity and higher blood sugar levels. Research has demonstrated that even a few nights of insufficient sleep can significantly impair glucose metabolism (Sleep Foundation). For instance, someone who stays up late to finish work and only sleeps five hours a night for several days may notice increased cravings, low energy, and difficulty concentrating—signs of fluctuating blood sugar and reduced insulin effectiveness.
Establishing healthy sleep hygiene habits can greatly improve both sleep quality and insulin sensitivity. Helpful strategies include maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and keeping electronics out of the bedroom. Limiting caffeine and heavy meals in the hours before bed, and ensuring your sleeping environment is dark, quiet, and cool, also support restful sleep. Aim for 7-9 hours of uninterrupted sleep each night. By prioritizing restorative sleep, you give your body the chance to regulate hormones and blood sugar, reducing the risk of insulin resistance and related health issues.
5. Add More Fiber to Your Diet

Dietary fiber, especially soluble fiber, plays a crucial role in improving insulin sensitivity by slowing the absorption of sugar into the bloodstream and preventing sudden spikes in blood glucose. Fiber also supports healthy gut bacteria, which may further benefit metabolic health (Harvard T.H. Chan School of Public Health). For example, a high-fiber meal like a lentil and vegetable soup paired with whole grain bread leads to steadier blood sugar levels compared to a low-fiber meal of white bread with processed meat, which can cause rapid glucose surges and greater insulin demand.
Boosting your daily fiber intake doesn’t have to be complicated. Start by including more fruits, vegetables, legumes, nuts, seeds, and whole grains in your meals. Swap white rice for brown rice, choose whole fruit over fruit juice, and add beans or lentils to salads and soups. Aim for at least 25-30 grams of fiber per day, increasing gradually to allow your digestive system to adjust. These simple changes can help regulate digestion, promote longer-lasting satiety, and ultimately support your body’s ability to use insulin more effectively.
6. Maintain a Healthy Weight

Carrying excess weight, particularly around the abdomen, is strongly associated with reduced insulin sensitivity. Fat tissue, especially visceral fat stored deep within the abdominal cavity, releases inflammatory substances and hormones that interfere with insulin’s ability to help cells absorb glucose (CDC). As global rates of overweight and obesity continue to rise, so does the prevalence of insulin resistance and type 2 diabetes.
Fortunately, even modest weight loss can significantly improve insulin sensitivity. Research shows that losing just 5-10% of your body weight can lead to meaningful reductions in blood sugar and insulin levels (American Diabetes Association). For many people, this may mean losing as little as 10-20 pounds. Sustainable changes, such as increasing physical activity, making healthier food choices, and monitoring portion sizes, are often more effective than rapid or extreme diets. Setting realistic, achievable goals and celebrating progress along the way can help maintain motivation. Achieving and maintaining a healthy weight is one of the most powerful natural strategies for preventing or reversing insulin resistance.
7. Balance Your Meal Timing
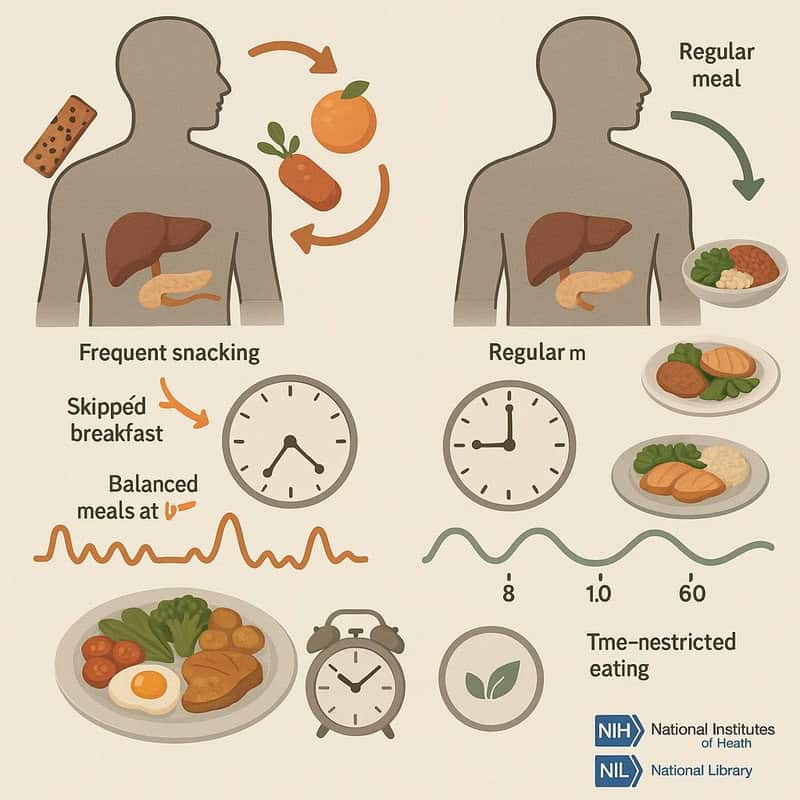
The frequency and timing of meals can significantly affect insulin sensitivity. Eating at irregular times or frequently snacking throughout the day can lead to constant insulin production and eventual insulin resistance. Conversely, regular meal patterns help the body anticipate and efficiently process nutrient intake, reducing the strain on insulin production (National Institutes of Health).
For example, skipping breakfast and then overeating at lunch or dinner can cause sharp spikes and crashes in blood sugar levels. In contrast, eating balanced meals at roughly the same times each day supports more stable insulin and glucose responses. Some research also suggests that time-restricted eating, such as consuming all meals within an 8-12 hour window, may improve insulin sensitivity and metabolic health (National Library of Medicine).
To optimize meal timing, aim for three balanced meals per day, spaced evenly, and avoid late-night eating. Listen to your body’s hunger signals and try to maintain a consistent eating schedule. These strategies can help keep insulin levels steady and support better blood sugar management over time.
8. Practice Mindful Eating

Mindful eating involves paying full attention to the experience of eating and listening to your body’s hunger and fullness cues. This practice can help prevent overeating, reduce stress-related eating, and ultimately improve insulin response. When you eat mindlessly—such as snacking in front of the TV or rushing through meals—you’re more likely to consume excess calories and highly processed foods, which can strain your insulin system (National Institutes of Health).
Consider the example of someone who eats lunch while working at their desk and barely notices what they’re consuming. They may finish their meal quickly, feel unsatisfied, and reach for more snacks shortly after. In contrast, mindful eating—savoring each bite, chewing slowly, and noticing flavors—can lead to greater satisfaction and better portion control.
To practice mindful eating, try these steps:
Eliminate distractions like phones or TVs during meals.
Take small bites and chew thoroughly.
Notice the taste, texture, and aroma of your food.
Pause between bites and check in with your hunger level.
Stop eating when you feel comfortably full.
9. Include Healthy Fats

Unsaturated fats, particularly monounsaturated and polyunsaturated fats, play an important role in enhancing insulin sensitivity. These healthy fats can help reduce inflammation and support more stable blood sugar levels by improving how cells respond to insulin. In contrast, diets high in trans fats or saturated fats are linked to increased insulin resistance and a higher risk of metabolic diseases (Harvard T.H. Chan School of Public Health).
Healthy fats are found in foods like avocados, olive oil, nuts, seeds, and fatty fish such as salmon and sardines. Unhealthy fats, including those found in fried foods, processed snacks, pastries, and fatty cuts of red meat, can negatively impact insulin function. Swapping unhealthy fats for healthier alternatives is a simple and effective way to support metabolic health. For example, use olive oil instead of butter for cooking, choose nuts or seeds as a snack instead of chips, and add avocado slices to salads or sandwiches rather than processed cheese or mayonnaise.
By prioritizing sources of unsaturated fats and minimizing unhealthy fat intake, you can help your body maintain better insulin sensitivity and overall cardiovascular health.
10. Limit Added Sugars
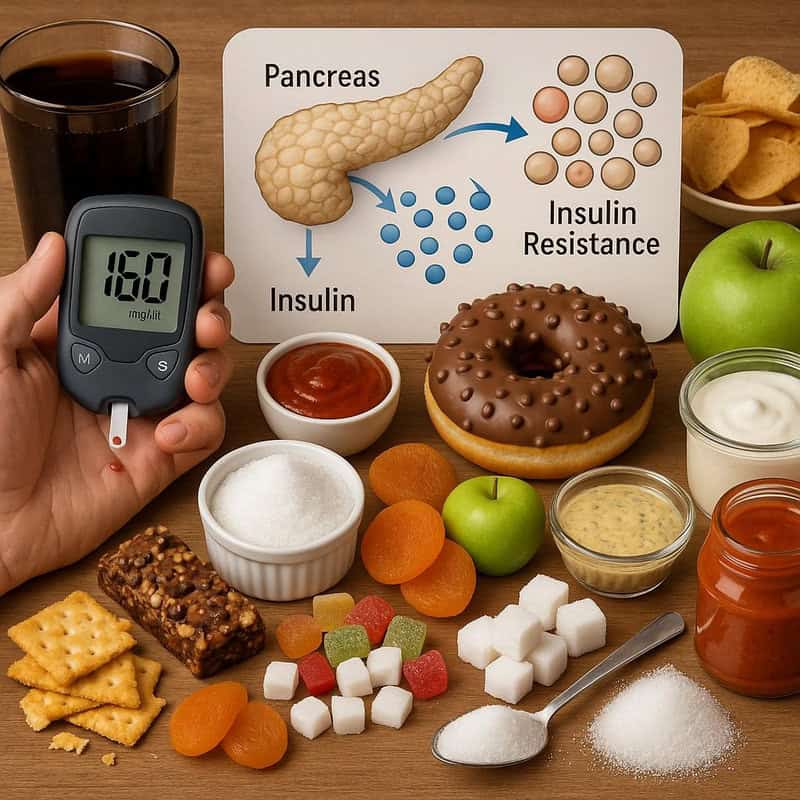
Consuming excessive added sugars can overwhelm the body’s insulin response, leading to insulin resistance over time. When you eat foods high in added sugars, such as sugary drinks, desserts, and many processed snacks, your blood sugar rises rapidly, prompting the pancreas to release more insulin. Chronic exposure to high insulin levels can cause the body’s cells to become less responsive, increasing the risk for type 2 diabetes (CDC).
Added sugars often hide in foods where you might not expect them—salad dressings, pasta sauces, granola bars, and flavored yogurts can all contain significant amounts. For example, a single can of soda may have up to 10 teaspoons of sugar, far exceeding daily recommendations. To reduce sugar intake, carefully read nutrition labels and ingredient lists, choose unsweetened versions of foods and beverages, and satisfy sweet cravings with naturally sweet foods like fresh fruit or a small handful of dried fruit.
Gradually cutting back on added sugars can retrain your taste buds and support better insulin sensitivity. Aim to limit added sugars to less than 10% of your daily calories for optimal metabolic health.
11. Stay Hydrated

Proper hydration is essential for maintaining healthy blood sugar levels and supporting insulin sensitivity. Water helps your kidneys flush excess glucose from the bloodstream through urine, reducing the burden on insulin (National Institutes of Health). In contrast, consuming sugary drinks such as sodas, fruit-flavored beverages, or sweetened coffees can cause rapid spikes in blood sugar and place extra stress on your body’s insulin production.
Opting for water instead of sugar-sweetened beverages is a simple yet powerful way to help regulate blood sugar. For example, replacing a daily can of soda with a glass of water can significantly reduce your overall sugar intake and lower your risk of developing insulin resistance. Other hydrating options include unsweetened herbal teas, sparkling water with a splash of lemon, or water infused with fresh fruit for flavor without the added sugar.
General hydration guidelines recommend drinking about 8 cups (64 ounces) of water per day, but individual needs may vary based on age, activity level, and climate. Paying attention to thirst cues and the color of your urine (pale yellow indicates good hydration) can help ensure you’re getting enough fluids to support your metabolism and insulin sensitivity.
12. Get Enough Magnesium

Magnesium is a vital mineral involved in hundreds of biochemical reactions in the body, including those that regulate insulin action and glucose metabolism. Research has shown that low magnesium levels are associated with increased risk of insulin resistance and type 2 diabetes (National Institutes of Health). Magnesium assists insulin in transporting glucose into cells, and a deficiency can impair this process, making it harder for the body to manage blood sugar effectively.
Good dietary sources of magnesium include leafy green vegetables (such as spinach and Swiss chard), nuts and seeds (especially almonds, pumpkin seeds, and sunflower seeds), whole grains, legumes, and certain types of fish like mackerel. Incorporating a variety of these foods into your daily meals can help you meet the recommended magnesium intake—about 310-420 mg per day for most adults.
While magnesium supplements are available, it’s best to obtain this nutrient from whole foods whenever possible. If you suspect a deficiency or have trouble reaching your needs through diet alone, consult with a healthcare professional before starting supplements, as excessive intake can cause adverse effects. Maintaining adequate magnesium levels can promote better insulin sensitivity and overall metabolic health.
13. Eat More Leafy Greens

Leafy green vegetables, such as spinach, kale, Swiss chard, and collard greens, are rich in antioxidants and essential minerals that support insulin function and overall metabolic health. These vegetables provide high levels of magnesium, vitamin C, and polyphenols, all of which have been shown to help improve insulin sensitivity and reduce oxidative stress that can impair glucose uptake (Harvard T.H. Chan School of Public Health).
Both raw and cooked leafy greens offer health benefits. Raw greens preserve the highest levels of vitamin C and some antioxidants, while cooking can enhance the bioavailability of certain nutrients like magnesium and carotenoids. For variety, try including raw spinach in salads, blending kale or Swiss chard into smoothies, or sautéing collard greens as a flavorful side dish. Other easy recipes include adding chopped greens to soups and stews, making a vegetable stir-fry, or preparing stuffed cabbage rolls.
Regularly incorporating leafy greens into meals is a simple and effective way to boost your intake of nutrients that promote insulin sensitivity. Aim for at least one to two servings of leafy greens daily to maximize their health benefits.
14. Embrace Probiotic Foods

The gut microbiome—the collection of microorganisms living in your digestive tract—plays a significant role in metabolic health, including insulin sensitivity. A balanced gut flora can help reduce inflammation, regulate blood sugar, and improve how your body responds to insulin (National Institutes of Health). Probiotic foods, which contain beneficial live bacteria, support a healthy gut microbiome and may lower the risk of insulin resistance.
Popular probiotic foods include yogurt with live cultures, kefir, sauerkraut, kimchi, miso, tempeh, and kombucha. Each food offers different strains of probiotics and unique flavors. For instance, yogurt and kefir are excellent for breakfast or snacks, while kimchi and sauerkraut make flavorful additions to salads, sandwiches, or grain bowls. Miso can be used for soups and marinades, and tempeh works well in stir-fries or as a plant-based protein source.
To incorporate probiotics into your diet, start with one serving per day and experiment with different sources to discover what you enjoy most. Choose products labeled with “live and active cultures” for maximum benefit. Regularly eating probiotic-rich foods can help optimize your gut health and, in turn, support better insulin sensitivity.
15. Try Intermittent Fasting (With Caution)
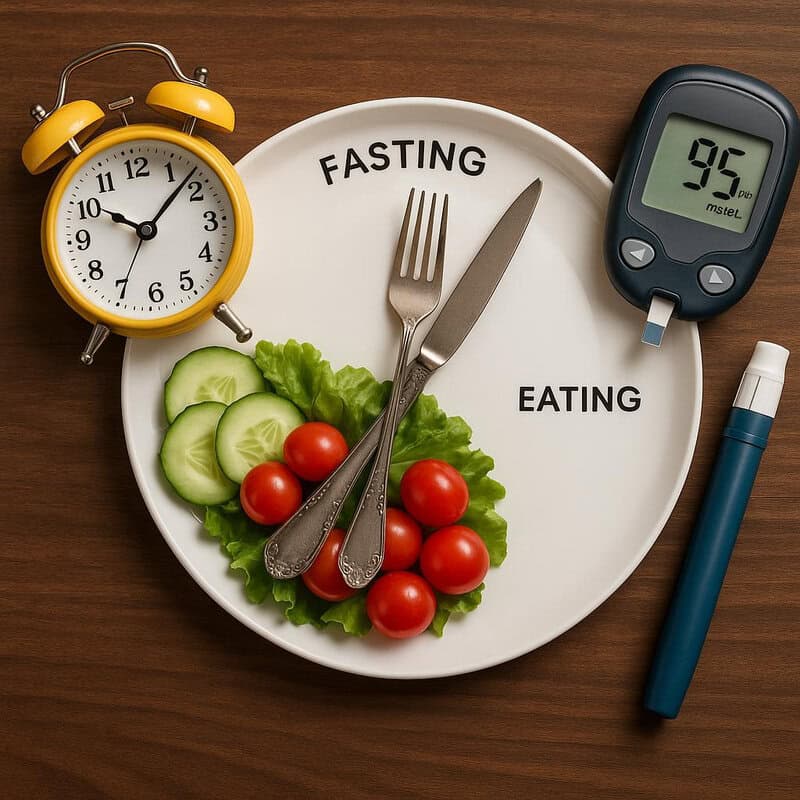
Intermittent fasting (IF) has gained attention for its potential to improve insulin sensitivity and regulate blood sugar levels. By alternating periods of eating and fasting, this approach gives your body extended breaks from insulin production, helping cells become more responsive to insulin over time (National Institutes of Health). Studies suggest that IF can lower fasting insulin levels, enhance metabolic function, and even promote modest weight loss, which further benefits insulin action.
Common IF protocols include the 16:8 method (16 hours fasting, 8 hours eating window), the 5:2 diet (eating normally five days a week, restricting calories on two non-consecutive days), and alternate-day fasting. The effectiveness and sustainability of each protocol may vary based on individual preferences and lifestyles. However, IF may not be appropriate for everyone—especially those with a history of eating disorders, pregnant or breastfeeding women, or individuals taking medications for blood sugar management.
If you are considering intermittent fasting, consult a healthcare provider or registered dietitian to ensure it is safe and suitable for your needs. Personalized guidance will help you avoid potential risks and achieve the best possible outcomes for your insulin sensitivity.
16. Use Vinegar in Meals

Adding vinegar, especially apple cider or white vinegar, to your meals can help moderate post-meal blood sugar spikes and improve insulin sensitivity. Research indicates that vinegar slows the digestion of carbohydrates and enhances the body’s response to insulin, resulting in steadier blood sugar levels after eating (National Institutes of Health). The acetic acid in vinegar is thought to inhibit enzymes that break down starches, thus reducing the rate at which glucose enters the bloodstream.
For example, including a simple vinaigrette dressing on a salad before a carbohydrate-rich meal—like pasta or rice—can help blunt the typical rise in blood sugar that follows. In one study, participants who consumed vinegar with their meal experienced lower postprandial glucose and insulin levels compared to those who did not.
To incorporate vinegar into your diet, try adding 1-2 tablespoons to salad dressings, marinades, or as a finishing touch on roasted vegetables. You can also mix a small amount with water as a pre-meal tonic, but always dilute vinegar to protect your teeth and digestive tract. Including vinegar regularly in your meals is a simple, natural strategy to support better blood sugar and insulin management.
17. Enjoy Berries

Berries such as blueberries, strawberries, raspberries, and blackberries are rich in polyphenols—powerful plant compounds known for their antioxidant and anti-inflammatory properties. Polyphenols in berries have been shown to improve insulin sensitivity by enhancing cellular glucose uptake and supporting a balanced inflammatory response (National Institutes of Health). Studies suggest that regular berry consumption can help regulate blood sugar after meals and support metabolic health.
Compared to many other fruits, berries tend to have a lower glycemic index, meaning they have a gentler effect on blood sugar levels. For instance, a serving of berries will generally cause a smaller rise in blood glucose than the same amount of tropical fruits like bananas or mangos. This makes berries an ideal fruit choice for those looking to improve insulin sensitivity.
Incorporate berries into your daily meals by adding them to oatmeal, yogurt, or smoothies, sprinkling them over salads, or enjoying them as a fresh snack. You can also use frozen berries, which preserve nutrients and are convenient year-round. Including a handful of berries each day is a delicious and easy way to harness their insulin-supportive benefits.
18. Limit Highly Processed Foods

Highly processed foods often contain refined grains, added sugars, unhealthy fats, and a range of artificial additives, all of which can contribute to insulin resistance. These foods are typically low in fiber and nutrients, causing rapid spikes in blood sugar and demanding more insulin from the body. Frequent consumption of processed snacks, sugary cereals, packaged baked goods, and fast food is strongly linked to a higher risk of developing type 2 diabetes and metabolic syndrome (National Institutes of Health).
In contrast, whole foods—such as fresh fruits and vegetables, whole grains, legumes, nuts, and lean proteins—provide the fiber, vitamins, and minerals needed for optimal blood sugar and insulin regulation. For example, a home-cooked meal of grilled chicken, brown rice, and sautéed vegetables will support better metabolic health than a meal of chicken nuggets, white bread, and fries.
To reduce processed food intake, shop the perimeter of the grocery store where fresh foods are usually located, read ingredient lists to avoid products with added sugars or trans fats, and prepare more meals at home. Prioritizing whole, minimally processed ingredients can help maintain healthy insulin sensitivity and long-term wellness.
19. Include Spices Like Cinnamon

Certain spices, particularly cinnamon, have been studied for their potential to support insulin action and promote better blood sugar control. Cinnamon contains bioactive compounds that may mimic insulin’s effects and increase glucose uptake by cells, thus improving insulin sensitivity (National Institutes of Health). Other spices such as turmeric and ginger also possess anti-inflammatory and antioxidant properties that can benefit metabolic health and aid in maintaining stable glucose levels.
Comparing different spices, cinnamon stands out for its direct effect on glucose metabolism, while turmeric is known for its active compound curcumin, which may reduce inflammation linked to insulin resistance. Ginger can help regulate blood sugar and improve digestion. Including a variety of these spices in your diet can offer complementary benefits.
To enjoy these spices daily, sprinkle cinnamon on oatmeal, yogurt, or fruit, blend turmeric into smoothies or curries, and add fresh or powdered ginger to stir-fries, teas, or baked goods. Using herbs and spices not only adds flavor but can also support your efforts to manage insulin sensitivity naturally and deliciously.
20. Avoid Trans Fats

Trans fats are well-documented for their harmful effects on insulin function and overall metabolic health. These artificial fats are created through a process called hydrogenation, which turns liquid oils into solid fats to extend shelf life. Consuming trans fats increases inflammation, disrupts insulin signaling, and raises the risk of insulin resistance and type 2 diabetes (Harvard T.H. Chan School of Public Health).
Common sources of trans fats include commercially baked goods (like cookies, crackers, and pastries), fried fast foods, margarine, and certain packaged snacks. Even though many countries have taken steps to reduce or ban trans fats in foods, they can still be found in some products. Always check ingredient labels for “partially hydrogenated oils,” which indicate the presence of trans fats.
To minimize your intake, opt for whole or minimally processed foods and choose healthier fats such as olive oil, avocado, and nuts. Be especially cautious with pre-packaged and fast foods. Reading labels carefully and avoiding foods containing partially hydrogenated oils will help protect your insulin sensitivity and support long-term health.
21. Increase Omega-3 Intake

Omega-3 fatty acids are renowned for their powerful anti-inflammatory properties, which can play a crucial role in improving insulin sensitivity. Chronic inflammation is a known contributor to insulin resistance, and omega-3s help counteract this process by reducing inflammatory markers in the body (National Institutes of Health). Research indicates that a diet rich in omega-3s is associated with better glucose metabolism and a lower risk of developing type 2 diabetes.
The best dietary sources of omega-3s include fatty fish such as salmon, sardines, mackerel, and anchovies. Plant-based options like flaxseeds, chia seeds, walnuts, and hemp seeds also provide omega-3s, though in the form of alpha-linolenic acid (ALA), which is less efficiently converted to the active forms found in fish (EPA and DHA). For those who do not consume fish, algae-based omega-3 supplements are available as a vegan alternative.
Incorporate omega-3s into your meals by grilling or baking fish, adding chia or flaxseeds to smoothies and oatmeal, or sprinkling walnuts on salads. Regularly including these foods can help manage inflammation, support healthy insulin function, and promote overall metabolic health.
22. Try a Mediterranean-Style Diet

The Mediterranean diet has been extensively researched for its positive effects on insulin sensitivity and overall metabolic health. Characterized by an abundance of fruits, vegetables, whole grains, legumes, nuts, olive oil, and moderate consumption of fish and poultry, this eating pattern is rich in fiber, antioxidants, and healthy fats. Studies show that people following a Mediterranean-style diet have a significantly lower risk of developing insulin resistance and type 2 diabetes compared to those adhering to typical Western diets (National Institutes of Health).
In contrast, Western diets tend to be higher in red and processed meats, refined grains, sugary foods, and unhealthy fats, all of which can worsen insulin sensitivity. The Mediterranean diet, by focusing on minimally processed foods and plant-based nutrition, helps regulate blood sugar and insulin levels more effectively.
To adopt this eating style, try meals like grilled fish with roasted vegetables and quinoa, Greek salad with feta and olives, or whole grain toast with smashed avocado and tomato. Incorporating beans into soups or stews, and enjoying fruit for dessert are other easy ways to embrace this healthy approach. Consistent adherence to a Mediterranean diet can be both satisfying and supportive of long-term insulin health.
23. Get Regular Health Screenings

Early detection of insulin resistance is essential for preventing the progression to type 2 diabetes and other metabolic disorders. Many people are unaware they have insulin resistance until symptoms become severe, making routine health screenings a vital tool for timely intervention (CDC). For example, a middle-aged adult with no apparent symptoms went for an annual check-up and, through routine blood tests, discovered elevated fasting glucose and insulin levels. With this early warning, they were able to make lifestyle changes and avoid developing diabetes.
Screenings typically include blood tests such as fasting glucose, insulin, hemoglobin A1c, and sometimes oral glucose tolerance tests. These can help identify problems before they lead to complications. Adults over 45, those with a family history of diabetes, or individuals with risk factors like obesity or high blood pressure should be particularly vigilant about regular testing.
Most experts recommend getting screened at least every three years, or more frequently if risk factors are present. Talk to your healthcare provider about the best screening schedule for you. Early detection empowers you to take control of your health and implement changes to improve insulin sensitivity before serious conditions develop.
24. Limit Alcohol Intake

Alcohol consumption can significantly affect insulin sensitivity and blood sugar control. While moderate alcohol intake may have a neutral or even slightly beneficial effect on insulin in some studies, heavy or frequent drinking is strongly associated with increased insulin resistance and a higher risk of developing type 2 diabetes (National Institutes of Health). Alcohol can disrupt the liver’s ability to regulate glucose, interfere with hormone balance, and contribute to weight gain—all factors that impair insulin action.
Moderate drinking is generally defined as up to one standard drink per day for women and up to two for men. In contrast, heavy drinking—such as consuming several drinks in a sitting or drinking most days of the week—can lead to chronic health issues, including worsening insulin resistance. For example, regularly exceeding these guidelines is linked to higher fasting blood sugar and increased belly fat.
To protect your insulin sensitivity, consider limiting your alcohol intake or opting for alcohol-free days each week. If you do choose to drink, select lower-sugar options, stay mindful of portion sizes, and avoid drinking on an empty stomach. Always consult your healthcare provider about what’s appropriate for your individual health needs.
25. Address Sleep Apnea

Sleep apnea, a common sleep disorder characterized by repeated interruptions in breathing during sleep, has a well-established connection to insulin resistance. The frequent drops in oxygen levels and sleep fragmentation caused by sleep apnea can trigger stress responses and inflammation, both of which disrupt normal insulin action (National Institutes of Health). Research shows that untreated sleep apnea increases the risk of developing type 2 diabetes and makes blood sugar management more challenging for those already diagnosed.
For example, a person experiencing chronic daytime fatigue, loud snoring, and frequent nighttime awakenings may be suffering from undiagnosed sleep apnea. Upon seeking medical evaluation, they might undergo a sleep study and receive a diagnosis. Treatment with continuous positive airway pressure (CPAP) or other therapies often leads to improved sleep quality and, over time, better insulin sensitivity and metabolic health.
If you or a loved one experiences symptoms such as excessive daytime sleepiness, loud snoring, or observed breathing pauses during sleep, it’s important to consult a healthcare provider. Early diagnosis and management of sleep apnea can significantly reduce your risk of insulin resistance and help you maintain better long-term health.
26. Boost Vitamin D Levels

Vitamin D plays a pivotal role in supporting insulin sensitivity and regulation of blood sugar. Research indicates that low vitamin D levels are associated with an increased risk of insulin resistance and the development of type 2 diabetes (National Institutes of Health). Vitamin D is believed to enhance the function of pancreatic beta cells, which are responsible for insulin production, and may also help reduce inflammation that impairs insulin action.
The most natural source of vitamin D is sunlight exposure, as your skin can synthesize the vitamin when exposed to UVB rays. However, factors such as limited outdoor activity, darker skin pigmentation, and living in northern latitudes can reduce this synthesis. Dietary sources include fatty fish (such as salmon and mackerel), fortified dairy or plant-based milks, egg yolks, and mushrooms exposed to sunlight. Despite these options, many people struggle to maintain optimal vitamin D levels, especially during winter months.
If you suspect a deficiency, consult with your healthcare provider about testing your vitamin D status. Supplementation may be recommended, with typical daily doses ranging from 800 to 2,000 IU, but individual needs can vary. Adequate vitamin D supports healthy insulin function and overall metabolic well-being.
27. Try Resistance Training

Resistance training, also known as strength or weight training, is highly effective for enhancing insulin sensitivity. Building muscle mass increases the body’s demand for glucose, as muscles use glucose for energy during and after exercise. This process improves how efficiently insulin transports glucose into cells (National Institutes of Health). Studies show that incorporating resistance training into your fitness routine can significantly lower blood sugar levels and reduce the risk of insulin resistance.
Compared to aerobic exercise, which primarily benefits cardiovascular health and burns calories, resistance training specifically targets muscle strength and size. Both forms of exercise are beneficial, but combining them delivers the greatest improvements in insulin sensitivity and overall metabolic health. Resistance training does not require a gym or heavy equipment—bodyweight exercises can be just as effective, especially for beginners.
Beginner routines may include exercises like squats, lunges, push-ups, and planks, performed two to three times per week. Start with one set of 8-12 repetitions for each exercise and gradually increase sets and resistance as you build strength. Consistency is key—regular resistance training supports glucose uptake, aids weight management, and boosts long-term metabolic health.
28. Limit Sedentary Time

Prolonged sedentary behavior, such as sitting for long periods at a desk or in front of a screen, can impair insulin sensitivity and contribute to higher blood sugar levels. When you remain inactive, your muscles use less glucose, and the body becomes less responsive to insulin’s signals. Research shows that breaking up extended sitting with short bouts of movement can significantly improve glucose metabolism and lower the risk of insulin resistance (National Institutes of Health).
Comparing sitting to standing, studies find that even standing or light activity—like a brief walk—every 30-60 minutes helps regulate blood sugar and insulin. For instance, employees who use standing desks or take regular movement breaks have better metabolic markers than those who sit continuously throughout the day.
To reduce sedentary time, try setting reminders to stand up and stretch every hour, take phone calls while walking, use a standing desk, or incorporate “walking meetings” into your workday. At home, get up during commercial breaks or do simple exercises while watching TV. These small, consistent efforts throughout the day can make a substantial difference in maintaining healthy insulin sensitivity and overall metabolic health.
29. Use Herbs Like Fenugreek

Fenugreek, a traditional herb used in cuisines and medicine worldwide, has gained attention for its potential to support insulin sensitivity and blood sugar control. Research suggests that fenugreek seeds contain soluble fiber and compounds such as 4-hydroxyisoleucine, which may help enhance insulin secretion and improve glucose uptake by cells (National Institutes of Health). Several clinical studies indicate that fenugreek supplementation can lower fasting blood sugar and post-meal glucose spikes, making it a promising natural aid for those with insulin resistance.
Compared to other herbal supplements, fenugreek stands out for its unique combination of fiber and phytochemicals. Other herbs, like bitter melon and gymnema sylvestre, have also shown potential benefits for blood sugar management, but their mechanisms and effectiveness may differ. It’s important to note that herbal remedies can interact with medications or cause side effects in some individuals.
If you are considering fenugreek supplements or incorporating fenugreek seeds into your diet (such as in teas, curries, or baked goods), consult your healthcare provider, especially if you are taking medications for diabetes. Monitoring your blood sugar and using herbs as a complement—not a substitute—to a healthy lifestyle is the safest approach.
30. Eat Regular, Balanced Meals

Consuming regular, balanced meals is fundamental to supporting healthy insulin sensitivity. Meals that contain a harmonious mix of carbohydrates, protein, and healthy fats help stabilize blood sugar levels and prevent large insulin spikes. Balanced macronutrients slow the absorption of glucose, keeping you fuller for longer and reducing the likelihood of overeating or energy crashes (CDC).
For example, a meal of grilled chicken, quinoa, and roasted vegetables provides protein, fiber-rich carbs, and healthy fats, leading to gradual blood sugar increases. In contrast, a meal of white bread and sugary drinks rapidly elevates glucose, requiring more insulin and increasing the risk of insulin resistance over time. Eating at regular intervals—such as three balanced meals and one or two healthy snacks—also helps maintain steady energy and glucose levels throughout the day.
Meal planning can simplify balanced eating. Start by including a source of lean protein, plenty of non-starchy vegetables, whole grains, and a small amount of healthy fat in each meal. Preparing meals in advance and having healthy snacks on hand further supports consistent, nutritious choices. Prioritizing balanced, regular meals is a key part of naturally improving and maintaining insulin sensitivity.
31. Try Green Tea

Green tea is rich in antioxidants called catechins, particularly epigallocatechin gallate (EGCG), which have been shown to improve insulin sensitivity and help regulate blood sugar levels. These antioxidants combat oxidative stress and inflammation, both of which can impair insulin function (National Institutes of Health). Regular green tea consumption has been linked to lower fasting glucose and improved insulin activity in several studies.
Compared to sugary beverages or even sweetened teas, green tea is a healthier choice as it contains virtually no calories and offers beneficial phytochemicals without added sugars. Herbal teas like chamomile or peppermint also provide health benefits, but green tea’s catechin content is uniquely effective for metabolic support. To maximize benefits, avoid sweetening your green tea with sugar or honey, which could counteract its positive effects.
For optimal flavor and antioxidant preservation, brew green tea by steeping loose leaves or a tea bag in hot (not boiling) water—around 160-180°F (70-80°C)—for 2-3 minutes. Enjoy it hot or iced, and consider adding a slice of lemon for extra antioxidants. Incorporating one to three cups of green tea daily is a simple way to support your insulin sensitivity naturally.
32. Limit Red and Processed Meats

Frequent consumption of red and processed meats, such as beef, pork, sausage, and deli meats, has been associated with an increased risk of insulin resistance and type 2 diabetes. These meats are often high in saturated fat, sodium, and preservatives, all of which can promote inflammation and interfere with healthy insulin function (Harvard T.H. Chan School of Public Health). Studies have found that individuals who eat more red and processed meat are more likely to develop metabolic syndrome and struggle with blood sugar control.
In contrast, protein sources such as fish, poultry, eggs, legumes, nuts, and seeds are linked with improved insulin sensitivity and overall metabolic health. Plant-based proteins, in particular, provide fiber, antioxidants, and beneficial fats that support stable blood sugar and lower disease risk.
To reduce your intake of red and processed meats, try plant-based swaps like lentil or bean stews, tofu or tempeh stir-fries, and chickpea or black bean burgers. Incorporate fish, chicken, or eggs as alternatives to red meat in meals. Making these changes can help decrease inflammation, improve insulin response, and support long-term health.
33. Include Legumes in Your Diet

Legumes, including beans, lentils, chickpeas, and peas, are nutritional powerhouses that support insulin sensitivity thanks to their high fiber and protein content. These foods help slow the absorption of glucose, resulting in more stable blood sugar and insulin levels after meals (National Institutes of Health). The unique combination of soluble fiber and plant-based protein in legumes also promotes satiety and helps with weight management, both of which are important for metabolic health.
Compared to refined carbohydrates like white bread, rice, or pasta, legumes have a much lower glycemic index, meaning they produce a gentler rise in blood sugar. This makes them an excellent carbohydrate choice for individuals aiming to improve their insulin response and prevent diabetes. Additionally, legumes are naturally low in fat and rich in micronutrients such as magnesium, potassium, and folate.
Incorporate legumes into your meals by adding black beans or kidney beans to salads, preparing lentil soups or stews, blending hummus as a snack, or making chili with mixed beans. Swapping processed carbs for legumes a few times a week can significantly enhance your dietary fiber intake and support healthier insulin function.
34. Avoid Smoking

Smoking has a detrimental impact on insulin sensitivity and overall metabolic health. Nicotine and other chemicals in tobacco can trigger chronic inflammation, increase oxidative stress, and disrupt the normal function of insulin, making it harder for glucose to enter your cells (CDC). Research has shown that smokers are more likely to develop insulin resistance and are at a higher risk of type 2 diabetes compared to non-smokers. The negative effects persist even with light or occasional smoking.
Quitting smoking can quickly begin to reverse some of these harmful effects and significantly improve insulin action. For example, a person who stopped smoking after years of use noticed improved energy levels, better blood sugar control, and a lower need for diabetes medication within months of quitting. The earlier you quit, the greater the long-term health benefits for your metabolic and cardiovascular systems.
Support resources for quitting include counseling, nicotine replacement therapies, prescription medications, and support groups. The Smokefree.gov website offers free tools, helplines, and personalized quit plans. Seeking professional help and leaning on friends and family can make the quitting process more manageable and successful, supporting both your insulin sensitivity and overall wellness.
35. Manage Underlying Conditions
Many underlying health conditions—such as polycystic ovary syndrome (PCOS), thyroid disorders, high blood pressure, and chronic inflammation—can negatively impact insulin sensitivity. These conditions often disrupt hormonal balance, increase inflammation, or directly interfere with how the body processes glucose, making it more difficult for insulin to work effectively (National Institutes of Health). For example, a person with undiagnosed hypothyroidism may experience unexplained weight gain, fatigue, and rising blood sugar levels, all of which can contribute to insulin resistance.
Properly managing these medical issues is critical for preserving or restoring insulin sensitivity. Regular check-ups with your healthcare provider allow for early detection and effective treatment of contributing conditions. This might include medications, lifestyle changes, or targeted therapies tailored to your situation. For instance, treating thyroid dysfunction or effectively managing PCOS can significantly improve blood sugar control and reduce the risk of developing type 2 diabetes.
Stay proactive by monitoring your health, following prescribed treatments, and discussing any new or unusual symptoms with your healthcare provider. Addressing underlying conditions as part of your overall wellness plan is a vital step in naturally supporting healthy insulin function and long-term metabolic health.
36. Address PCOS (Polycystic Ovary Syndrome)
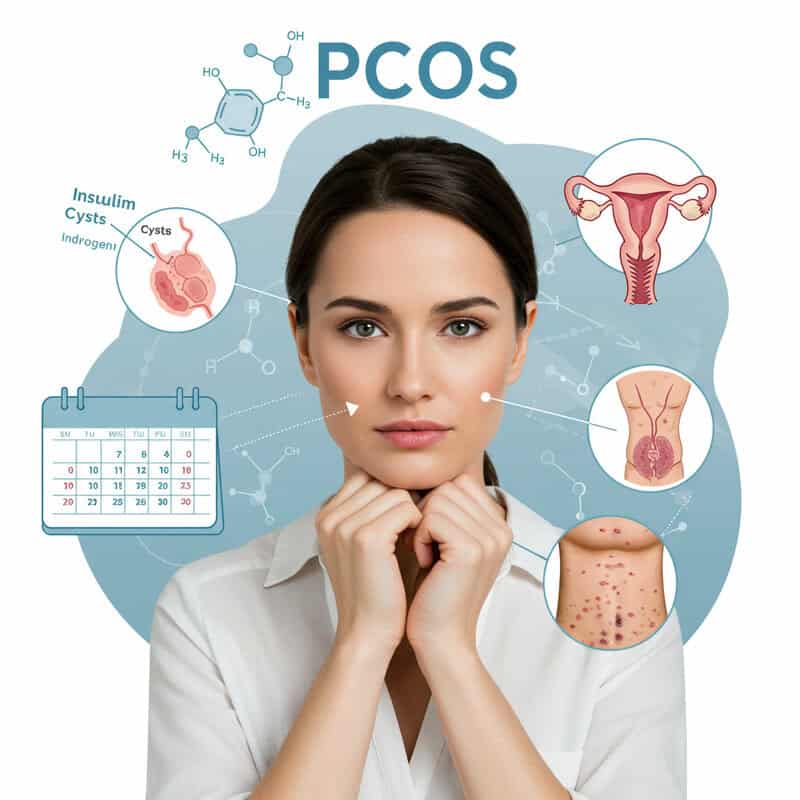
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age, and it is strongly linked to insulin resistance. Women with PCOS often produce excess androgens (male hormones), which can interfere with the body’s ability to use insulin effectively, leading to higher blood sugar and increased risk of type 2 diabetes (CDC). Symptoms of PCOS include irregular periods, ovarian cysts, acne, and weight gain, many of which are exacerbated by underlying insulin resistance.
Real-life stories highlight the challenges and successes women face in managing PCOS. For example, one woman found that adopting a balanced diet, increasing physical activity, and losing just 5-10% of her body weight significantly improved her insulin sensitivity and menstrual regularity. Others have benefited from medications like metformin, which can help regulate blood sugar and hormone levels.
Effective management of PCOS requires a tailored approach that addresses both hormonal imbalances and insulin resistance. This may include lifestyle modifications, medical therapies, and regular monitoring by a healthcare professional. Early diagnosis and comprehensive care can help mitigate the long-term health risks associated with PCOS and support overall metabolic health.
37. Avoid Crash Diets

Crash diets—extreme, restrictive eating plans that promise rapid weight loss—can actually harm insulin sensitivity and disrupt metabolic health. While these diets may lead to quick results on the scale, they often force the body into a state of stress, reduce muscle mass, and slow down metabolism. Studies show that repeated cycles of severe calorie restriction followed by weight regain (known as “yo-yo dieting”) are linked to increased insulin resistance and a higher risk of developing type 2 diabetes (National Institutes of Health).
In contrast, sustainable lifestyle habits—such as balanced eating, regular physical activity, and gradual weight loss—promote long-term improvements in insulin sensitivity. For example, losing 1-2 pounds per week through modest calorie reduction and exercise is much more beneficial for your metabolism than losing a large amount of weight very quickly.
To make lasting changes, focus on small, manageable steps: swap sugary drinks for water, add more vegetables to meals, and find enjoyable ways to move your body. These gradual adjustments are easier to maintain and support healthier insulin function over time. Embracing patience and consistency, rather than extreme approaches, is key to successful, long-term metabolic health.
38. Eat More Nuts and Seeds

Nuts and seeds are nutrient-dense foods that offer a variety of health benefits, including improving insulin sensitivity. They are rich in healthy fats, plant-based protein, magnesium, fiber, and antioxidants—all nutrients that contribute to better blood sugar control and reduced inflammation (Harvard T.H. Chan School of Public Health). For example, almonds, walnuts, chia seeds, flaxseeds, and sunflower seeds have been shown to help stabilize blood glucose and promote satiety, aiding in weight management.
Compared to common snack foods like chips, cookies, or candy bars, nuts and seeds have a lower glycemic index and provide sustained energy without causing sharp blood sugar spikes. Choosing a handful of raw or lightly roasted nuts over processed snacks can support your efforts to maintain healthy insulin function.
Portion control is important, as nuts and seeds are calorie-dense. A typical serving is about 1 ounce—or a small handful—per day. You can add nuts to salads, sprinkle seeds on yogurt or oatmeal, or enjoy them as a stand-alone snack. Choosing unsalted and unflavored varieties maximizes health benefits while keeping added sodium and sugars to a minimum.
39. Use Portion Control

Practicing portion control is essential for preventing overeating, which can overwhelm your body’s insulin response and contribute to insulin resistance over time. Consistently consuming large meals or snacks forces the pancreas to release more insulin to manage the higher influx of glucose, increasing the risk of metabolic imbalances and weight gain (CDC). Smaller, well-portioned meals help regulate blood sugar and allow insulin to work more effectively.
Comparing serving sizes can be eye-opening. For example, a standard serving of cooked pasta is just 1/2 cup, yet restaurant portions often exceed two cups. Similarly, a proper portion of meat is about the size of a deck of cards, while steaks served in restaurants are frequently much larger. Being aware of these differences can help you make healthier choices both at home and when dining out.
Practical portioning tips include using smaller plates and bowls, pre-portioning snacks rather than eating from the package, and filling half your plate with non-starchy vegetables. Take your time eating, and check in with your hunger cues before deciding on seconds. Adopting mindful portion control makes it easier to support healthy insulin sensitivity and long-term weight management.
40. Choose Low-Glycemic Foods

The glycemic index (GI) measures how quickly a carbohydrate-containing food raises blood sugar levels. Low-GI foods are digested and absorbed more slowly, leading to gradual increases in blood glucose and less strain on insulin production (Harvard T.H. Chan School of Public Health). In contrast, high-GI foods cause rapid spikes and crashes in blood sugar, which can worsen insulin resistance over time.
For example, a meal of steel-cut oats, lentils, and berries (all low-GI foods) provides steady energy and promotes better insulin sensitivity. Conversely, a breakfast of sugary cereal, white bread, and jam (high-GI foods) leads to swift glucose surges, making it harder for the body to maintain balance. Over time, consistently choosing low-GI foods helps regulate appetite, manage weight, and support metabolic health.
To make healthier swaps, replace white rice with brown or wild rice, choose whole grain bread instead of white, opt for sweet potatoes over regular potatoes, and enjoy fresh fruit rather than fruit juice. Incorporating more legumes, non-starchy vegetables, and whole grains into your diet can naturally lower the glycemic impact of your meals and improve insulin sensitivity.
41. Try Yoga or Tai Chi

Mind-body practices such as yoga and tai chi offer holistic benefits that extend beyond flexibility and balance—they also help reduce stress, which is a key factor in insulin resistance. Chronic stress elevates cortisol, a hormone that increases blood sugar and disrupts healthy insulin function. Studies have shown that regular participation in yoga or tai chi can lower cortisol levels, improve mood, and enhance insulin sensitivity (National Institutes of Health).
Yoga combines physical postures, controlled breathing, and mindfulness meditation, making it effective for both physical and emotional wellness. Tai chi, a gentle form of Chinese martial arts, emphasizes slow, flowing movements and deep breathing, promoting relaxation and body awareness. Both activities are suitable for people of all ages and fitness levels, and can be adapted for those with mobility limitations.
For beginners, many community centers, gyms, and online platforms offer introductory yoga and tai chi classes. Look for certified instructors with experience guiding newcomers. Even practicing for 15-30 minutes a few times per week can yield noticeable benefits for stress management and metabolic health. Incorporating these practices into your routine can naturally support better insulin sensitivity and overall well-being.
42. Reduce Salt Intake

High sodium intake is not only linked with elevated blood pressure but also with impaired metabolic health and reduced insulin sensitivity. Consuming excessive amounts of salt can contribute to fluid retention, increased inflammation, and a higher risk of developing metabolic syndrome and type 2 diabetes (National Institutes of Health). Many processed foods—including canned soups, packaged snacks, deli meats, and fast food—contain large amounts of hidden sodium, while fresh, homemade meals typically allow for better control over salt content.
For instance, a homemade vegetable stir-fry prepared with fresh herbs and minimal salt will contain far less sodium than a frozen entrée or takeout option. Over time, consistently choosing fresh foods helps reduce sodium intake and supports healthier blood pressure and insulin function.
To lower your salt consumption, start by reading nutrition labels and selecting products labeled “low sodium” or “no added salt.” Flavor foods with herbs, spices, lemon juice, or vinegar instead of salt. Gradually reduce the amount of salt you add during cooking or at the table, and rinse canned beans or vegetables to remove excess sodium. These small changes can have a meaningful impact on your metabolic and overall health.
43. Eat More Colorful Vegetables

Colorful vegetables are packed with antioxidants, vitamins, and phytochemicals that play a vital role in supporting insulin sensitivity and overall metabolic health. Each color in produce—red, orange, yellow, green, purple, and white—reflects different beneficial compounds. For example, red peppers and tomatoes are rich in lycopene, while orange carrots and squash contain beta-carotene, both of which help reduce oxidative stress and inflammation that can impair insulin function (Harvard T.H. Chan School of Public Health).
Meals that feature a variety of vegetable colors provide a broader spectrum of antioxidants and nutrients compared to dishes with only one or two types of produce. For instance, a salad with greens, cherry tomatoes, purple cabbage, grated carrots, and yellow bell pepper is far richer in health-promoting compounds than a salad made with just iceberg lettuce and cucumber.
To add more color to your diet, aim to fill half your plate with vegetables at each meal. Try roasting a mix of root vegetables, adding spinach or kale to smoothies, or topping sandwiches with sliced peppers and shredded carrots. Experimenting with seasonal produce and trying new recipes can make eating a rainbow both enjoyable and beneficial for insulin sensitivity.
44. Monitor Blood Sugar at Home

Self-monitoring your blood sugar at home is a powerful tool for understanding how your lifestyle choices impact insulin sensitivity and overall metabolic health. Regular tracking allows you to see the effects of different foods, activities, stress, and sleep on your glucose levels, helping you make informed decisions to improve or maintain healthy insulin function (CDC).
There are several types of home glucose meters, ranging from basic fingerstick devices to advanced continuous glucose monitors (CGMs) that provide real-time data throughout the day. While fingerstick meters require manual readings, CGMs can track trends and fluctuations, offering a clearer picture of your overall blood sugar control. Choosing the right device depends on your needs, budget, and healthcare provider’s recommendations.
Effective monitoring strategies include checking your blood sugar at consistent times—such as fasting in the morning and two hours after meals—to identify patterns and triggers. Keep a log of readings, meals, exercise, and other factors that might influence your glucose levels. Share this information with your healthcare team to adjust your lifestyle or treatment plan as needed. Proactive self-monitoring empowers you to take charge of your health and supports natural improvements in insulin sensitivity.
45. Limit Artificial Sweeteners

Artificial sweeteners, such as aspartame, sucralose, and saccharin, are widely used as sugar substitutes in beverages and processed foods. While they are generally considered safe and offer a calorie-free alternative to sugar, emerging research suggests that frequent use of artificial sweeteners may negatively impact insulin sensitivity and alter gut microbiota, which can influence blood sugar regulation (National Institutes of Health). Some studies have found that certain sweeteners may trigger insulin secretion despite not containing calories, or may increase cravings for sweet foods, potentially leading to overeating.
There are differences among types of sweeteners, with some, like stevia and monk fruit, considered more “natural” and possibly less likely to affect glucose metabolism compared to synthetic varieties. However, the long-term effects of both artificial and natural low-calorie sweeteners are still being studied, and individual responses can vary.
For practical use, it’s wise to limit overall intake of all sweeteners and focus on reducing the desire for intensely sweet flavors. Opt for water, unsweetened beverages, and whole fruits to satisfy your sweet tooth. When using sweeteners, choose the least processed options and use them sparingly, prioritizing a diet based on whole, minimally processed foods for optimal insulin health.
46. Stay Consistent With Habits

Consistency is a cornerstone of improving and maintaining insulin sensitivity. Adopting healthy routines—such as balanced eating, regular exercise, and quality sleep—reinforces positive changes in your body’s ability to manage blood sugar. Steady habits help minimize fluctuations in glucose and insulin, making it easier to achieve long-term metabolic health (CDC). While occasional lapses are normal, returning to your routine quickly prevents setbacks from becoming long-term obstacles.
Consider the example of someone who struggled with irregular meal times and sporadic physical activity. By setting a schedule for daily meals and committing to a morning walk each day, they noticed not only more stable energy levels, but also improved blood sugar readings and easier weight management over several months. Small, incremental habit changes—made consistently—yield significant results over time.
To stay on track, try keeping a journal or using an app to log meals, workouts, sleep, and stress-management activities. Review your progress regularly and celebrate milestones, no matter how small. If you encounter challenges, adjust your approach rather than giving up. Building and maintaining consistent habits is one of the most effective ways to naturally support insulin sensitivity and overall well-being.
47. Seek Social Support

Social support plays a vital role in achieving and maintaining healthy habits that improve insulin sensitivity. Having encouragement and accountability from friends, family, or a community group increases motivation, makes it easier to overcome obstacles, and enhances adherence to lifestyle changes (National Institutes of Health). People who try to adopt new behaviors on their own may struggle with consistency, while those who engage with others are more likely to reach their goals and sustain them over time.
Research shows that group-based interventions—such as exercise classes, healthy cooking workshops, or diabetes prevention programs—lead to better outcomes compared to solo efforts. The camaraderie, shared experiences, and collective problem-solving foster a sense of belonging and accountability. For example, joining a walking group or participating in an online healthy eating challenge can provide the encouragement needed to stick with changes, even when motivation wanes.
Support options include local community centers, fitness groups, workplace wellness programs, and online forums or social media groups focused on healthy living. You can also enlist friends or family members as accountability partners. Reaching out for support not only makes lifestyle changes more enjoyable but also boosts your chances of long-term success in improving insulin sensitivity.
48. Read Nutrition Labels Carefully

Reading nutrition labels is a crucial skill for identifying hidden ingredients that can negatively impact insulin sensitivity. Many packaged foods contain added sugars, refined grains, unhealthy fats, and sodium—all of which can disrupt blood sugar and insulin balance (U.S. Food & Drug Administration). Ingredients like high-fructose corn syrup, partially hydrogenated oils, and various forms of added sugar may be listed under different names, making it easy to underestimate their effect.
People who consistently check labels are better equipped to make healthier choices than those who shop based on marketing claims or packaging alone. For instance, a “healthy” granola bar may contain more sugar than a candy bar or breakfast cereal, yet appear wholesome at first glance. By learning to interpret serving sizes, total and added sugars, fiber, and fat content, shoppers can make informed decisions that support insulin health.
Smart shopping tips include choosing products with short ingredient lists, prioritizing whole foods, and avoiding items with added sugars or trans fats. When in doubt, compare brands to find options lower in sugar, sodium, and unhealthy fats. Developing label reading skills empowers you to manage your diet and improve insulin sensitivity naturally.
49. Work With a Registered Dietitian

Partnering with a registered dietitian (RD) offers the advantage of personalized nutrition strategies tailored to your unique lifestyle, preferences, and health needs. RDs are trained experts in nutrition science who can assess your current diet, identify areas for improvement, and develop realistic, sustainable plans to help you improve insulin sensitivity and overall metabolic health (Academy of Nutrition and Dietetics).
Many people find greater success and confidence in making dietary changes with professional support. For example, someone struggling to manage blood sugar despite multiple attempts at self-directed diet changes may experience significant improvement after working with an RD. Through meal planning, education, and ongoing encouragement, the individual learns how to balance meals, navigate food choices, and stay accountable, resulting in more stable blood sugar and enhanced well-being.
To find a qualified dietitian, start by asking your healthcare provider for a referral or use online directories like the Academy of Nutrition and Dietetics’ “Find a Nutrition Expert” tool. Many insurance plans cover RD services for diabetes prevention and management. Investing in expert guidance can be a powerful step toward naturally improving insulin sensitivity and achieving your health goals.
50. Re-Evaluate Medications With Your Doctor

Some commonly prescribed medications can impact insulin sensitivity or blood sugar regulation, either as a side effect or through their primary action. For example, certain steroids, antipsychotics, beta-blockers, and some birth control pills may contribute to increased insulin resistance or elevated glucose levels (CDC). Understanding how these medications interact with your body is crucial for maintaining optimal metabolic health, especially if you have risk factors for diabetes or insulin resistance.
Drug types vary in their effects—while some may worsen insulin sensitivity, others, such as metformin or GLP-1 agonists, are specifically prescribed to improve it. It’s important to never stop or change prescribed medications without medical guidance. However, regular medication reviews with your healthcare provider can identify opportunities to switch to alternatives with fewer metabolic side effects or to adjust dosages for better balance.
Schedule periodic check-ins, especially if you notice changes in weight, energy levels, or blood sugar readings. Bring a complete list of your medications to each appointment and discuss any concerns or symptoms. Proactive communication and collaboration with your doctor help ensure your medication regimen supports your long-term insulin health and overall well-being.
Conclusion

Addressing insulin sensitivity is more urgent than ever due to the rising rates of insulin resistance and type 2 diabetes globally (International Diabetes Federation). The good news is that even small, consistent lifestyle changes—such as improving diet, increasing activity, managing stress, and prioritizing sleep—can have cumulative, long-term benefits for metabolic health. Proactive self-care, regular health screenings, and seeking guidance from healthcare professionals or registered dietitians can significantly reduce your risk and empower you to take control of your well-being. Start with manageable steps, track your progress, and remember that every positive change supports better insulin sensitivity and a healthier future.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





