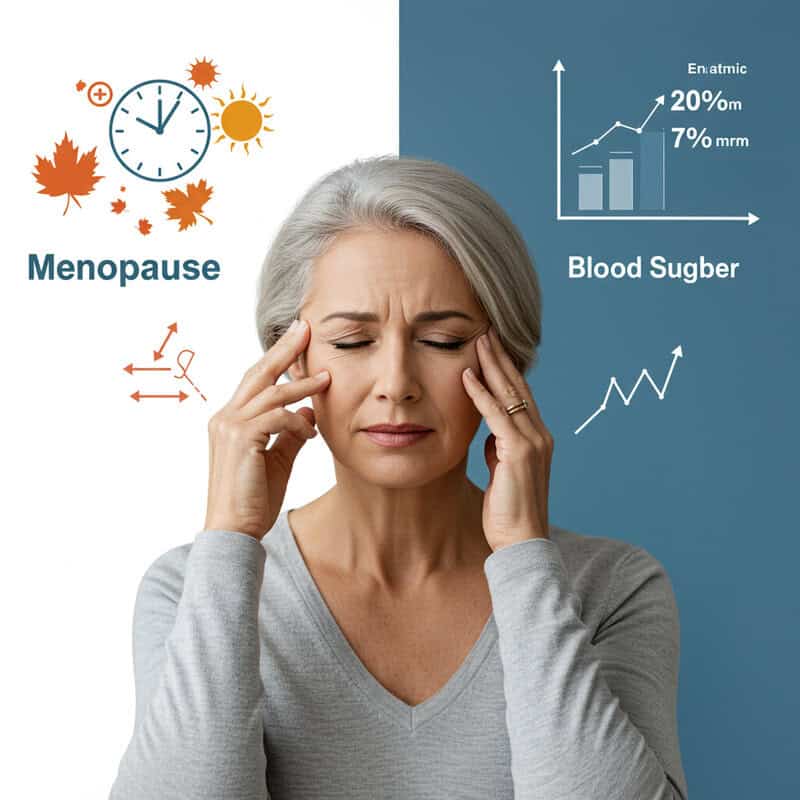
She Thought It Was Menopause… But It Was Her Blood Sugar
Millions of women worldwide experience symptoms such as hot flashes, fatigue, and mood swings, often attributing them to menopause. However, over 14 million women in the United States alone have undiagnosed blood sugar disorders, including prediabetes and type 2 diabetes (CDC). The endocrine system regulates both reproductive hormones and blood sugar, leading to significant symptom overlap. This overlap can result in misdiagnosis or delayed diagnosis, causing women to miss critical treatment opportunities. Recognizing the subtle differences is essential for timely intervention and better health outcomes.
1. Hot Flashes or Blood Sugar Spikes?

Hot flashes are commonly associated with menopause, but blood sugar fluctuations can produce nearly identical sensations: sudden warmth, sweating, and even heart palpitations. According to the American Diabetes Association, low blood sugar (hypoglycemia) can cause intense sweating, anxiety, and a flushed feeling—symptoms that are easily mistaken for menopausal hot flashes.
Consider the story of Linda, a 52-year-old woman who assumed her frequent hot flashes were simply a sign of menopause. After months of discomfort and unsuccessful hormone therapy, her doctor finally ordered a glucose tolerance test, revealing episodes of hypoglycemia. This misdiagnosis delayed appropriate treatment and lifestyle adjustments that could have helped her sooner.
To distinguish between menopause and blood sugar issues, track the timing and triggers of your symptoms. Hot flashes related to low blood sugar often follow skipped meals, intense exercise, or high-sugar snacks. Keeping a symptom diary and monitoring blood sugar levels with a glucometer can help you and your healthcare provider identify patterns (NIDDK). Early detection is crucial for effective management and avoiding unnecessary treatments.
2. Night Sweats: Not Always Hormonal

Many women experiencing night sweats assume they’re entering menopause, but nocturnal hypoglycemia—a drop in blood sugar levels during sleep—can trigger the same drenching perspiration. According to the Centers for Disease Control and Prevention (CDC), low blood sugar at night can result in sudden sweating, confusion, irritability, and even nightmares. While menopausal night sweats are typically linked to hormonal fluctuations, hypoglycemic episodes often occur after eating a high-carbohydrate dinner, late-night alcohol consumption, or skipping evening snacks.
The key difference lies in the timing and accompanying symptoms. Menopausal night sweats may be part of a broader pattern of hormonal changes, whereas hypoglycemic sweats often coincide with shakiness, racing heartbeat, or morning headaches. The American Diabetes Association recommends tracking when night sweats occur and noting any related symptoms such as hunger, dizziness, or confusion upon waking.
Maintaining a symptom journal can help distinguish between hormone-related and blood sugar-related night sweats. If you suspect your night sweats might be linked to blood sugar, discuss overnight glucose monitoring options with your healthcare provider for a more accurate diagnosis and targeted management.
3. Mood Swings Beyond Estrogen

While mood swings are often attributed to fluctuating estrogen during menopause, blood sugar instability can have a profound impact on emotional well-being. Sudden drops or spikes in glucose levels can trigger irritability, anxiety, and even symptoms resembling depression. The National Institute of Mental Health (NIMH) highlights that blood sugar imbalances can directly affect the brain’s neurotransmitter levels, leading to unpredictable mood changes.
For example, Sarah, a 49-year-old teacher, noticed her irritability and mood swings seemed out of proportion to her circumstances. She assumed menopause was to blame, but after tracking her feelings alongside her meal schedule, she realized her worst moments occurred when she skipped breakfast or indulged in sugary snacks. Once she adjusted her eating habits to stabilize her blood sugar, her mood swings dramatically decreased.
The CDC recommends noting mood changes in relation to meals and snacks. If irritability or anxiety tends to occur before meals or after consuming high-sugar foods, blood sugar could be the culprit. Keeping a detailed journal can empower you and your healthcare provider to spot these patterns and implement effective dietary changes.
4. Fatigue: Double-Edged Symptom
Fatigue is a hallmark of both menopause and blood sugar imbalances, making it a particularly confusing symptom. High blood sugar (hyperglycemia) can cause persistent tiredness by preventing glucose from entering cells for energy, while low blood sugar (hypoglycemia) deprives the brain and muscles of fuel, leading to exhaustion. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), both extremes can leave individuals feeling drained, regardless of sleep quality.
Maria, a 55-year-old accountant, battled unrelenting fatigue for months, attributing her lack of energy to menopause. Despite trying hormone therapy and improving her sleep hygiene, she noticed no improvement. Only after her doctor suggested a blood sugar test did she discover she had undiagnosed type 2 diabetes. With proper management, her energy levels quickly rebounded, illustrating the importance of accurate diagnosis.
The American Diabetes Association recommends keeping an energy-symptom diary to track how your energy fluctuates with meals, snacks, and physical activity. Noting when fatigue strikes in relation to eating or fasting can help differentiate between hormonal and blood sugar causes, ultimately guiding you toward the right treatment approach.
5. Sudden Weight Changes

Unexpected weight gain or loss is often seen as a natural part of menopause due to hormonal shifts that slow metabolism. However, blood sugar imbalances can also cause dramatic changes in weight. CDC notes that high blood sugar levels can cause the body to store excess glucose as fat, resulting in unexplained weight gain, especially around the abdomen. Conversely, undiagnosed diabetes can lead to rapid weight loss as the body breaks down muscle and fat for energy when it cannot access glucose efficiently.
Menopause-related weight changes typically develop gradually, while blood sugar-driven fluctuations may be more sudden. For example, unintentional weight loss despite normal or increased appetite, or gaining weight quickly without major lifestyle changes, could signal an underlying glucose issue. According to the American Diabetes Association, these symptoms warrant further investigation, especially if accompanied by fatigue, excessive thirst, or frequent urination.
When to consider checking blood sugar? If you experience sudden weight changes that do not align with your eating habits or activity level, or if menopause interventions aren’t helping, ask your healthcare provider about blood glucose testing. Early detection is key to effective management and preventing complications.
6. Increased Thirst

Persistent or excessive thirst, known as polydipsia, is a classic sign of elevated blood sugar. When glucose levels are high, the kidneys work overtime to filter and remove the excess sugar, which leads to more frequent urination and, in turn, increased thirst. According to the Centers for Disease Control and Prevention (CDC), this cycle is a hallmark symptom of both prediabetes and diabetes, and it can easily be mistaken for menopause-related changes.
Menopause can also cause dryness—particularly in the mouth, eyes, and skin—due to declining estrogen, which may prompt women to drink more water for comfort. However, menopause-related dryness typically isn’t accompanied by increased urination. In contrast, blood sugar-driven thirst often goes hand-in-hand with frequent trips to the bathroom, especially at night.
To help distinguish the cause, the NIDDK recommends tracking your daily fluid intake and urination frequency. If you are constantly thirsty and find yourself urinating more than usual—especially if you wake up multiple times overnight—it’s wise to discuss these patterns with your healthcare provider and consider a blood glucose test.
7. Frequent Urination

One of the most telling signs of elevated blood sugar is frequent urination, or polyuria. When blood glucose levels are too high, the kidneys are unable to reabsorb all the excess sugar, causing it to spill into the urine. This process pulls additional water from the body, resulting in the need to urinate more often. The CDC lists frequent urination as a key symptom of both type 1 and type 2 diabetes.
Menopause can also bring changes in urinary patterns, often due to declining estrogen weakening the pelvic floor muscles, leading to increased urgency or even incontinence. However, menopause-related urinary symptoms are less likely to be associated with large volumes of urine or to occur alongside excessive thirst and fatigue.
To distinguish between the two, the NIDDK recommends tracking how often you urinate and the amount each time. If you find yourself making frequent trips to the bathroom both day and night, and especially if the volume of urine is high, it could be a sign of blood sugar imbalance rather than just menopausal changes. Monitoring these patterns can help guide accurate diagnosis and timely treatment.
8. Blurred Vision Episodes

Episodes of blurred vision can be unsettling and are sometimes mistaken for a normal part of aging or menopause. However, rapid changes in blood sugar levels—both highs (hyperglycemia) and lows (hypoglycemia)—can cause the lenses in your eyes to swell or shrink, temporarily altering your ability to focus. According to the CDC, these fluctuations are common in undiagnosed or poorly managed diabetes.
Menopause may also affect vision, but typically this is due to dry eyes or hormonal changes that gradually impact tear production and eye health over time. These changes are usually persistent rather than episodic, and do not fluctuate as rapidly as those caused by blood sugar swings.
The American Academy of Ophthalmology recommends tracking when blurred vision episodes occur and noting whether they coincide with meals, periods of hunger, or other symptoms such as headache or dizziness. If your blurred vision seems to come and go, especially after eating or skipping a meal, it may be time to discuss blood sugar testing with your healthcare provider.
9. Tingling or Numbness

Persistent tingling or numbness in the hands, feet, or legs can be an early sign of neuropathy, a form of nerve damage caused by prolonged high blood sugar. According to the CDC, diabetic neuropathy develops gradually, with symptoms such as pins-and-needles sensations, burning, or loss of feeling. These symptoms are a result of excess glucose damaging the small blood vessels that supply nerves, leading to impaired nerve function over time.
While menopause can cause some neurological symptoms, such as temporary tingling due to hormonal shifts or anxiety, these are generally fleeting and less likely to be persistent or progressive. Menopausal changes are more often associated with muscle aches and joint stiffness rather than chronic numbness or burning sensations in the extremities.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends carefully tracking any new or unusual sensations in your limbs. If you experience ongoing tingling, numbness, or weakness—especially if these symptoms worsen at night or interfere with daily activities—consult your healthcare provider and request blood sugar testing to rule out underlying neuropathy.
10. Headaches: A Common Overlap
Headaches are frequently reported by women experiencing both menopause and blood sugar fluctuations, making them a challenging symptom to interpret. Blood sugar swings—either low (hypoglycemia) or high (hyperglycemia)—can trigger headaches as the brain responds to changes in glucose supply. The CDC notes that sudden drops in blood sugar can cause headaches, confusion, and even migraines, while chronic high blood sugar can also lead to persistent head pain.
Menopause is often associated with hormone-driven migraines or tension headaches, particularly as estrogen levels fluctuate. These headaches may be cyclical, coinciding with hormonal changes during perimenopause or following missed periods. In contrast, blood sugar-related headaches tend to occur in relation to meals—either after skipping food, eating high-sugar foods, or experiencing long gaps between eating.
The NIDDK recommends monitoring the timing of headaches and noting if they coincide with hunger, fatigue, or episodes of shakiness. If headaches frequently appear before meals or after consuming sweets, consider discussing blood sugar testing with your healthcare provider to rule out glucose instability as a contributing factor.
11. Brain Fog

Brain fog—characterized by forgetfulness, confusion, and difficulty concentrating—is a frequently reported symptom among women in midlife. While hormonal changes in menopause can certainly impair cognitive function, unstable blood sugar can have a similar, often overlooked, impact on mental clarity. According to the CDC, both high and low blood glucose levels can disrupt the brain’s ability to function efficiently, leading to episodes of confusion, slow thinking, or memory lapses.
Consider the case of Brenda, a 57-year-old who began struggling with forgetfulness and trouble focusing at work. She initially assumed it was “just menopause,” but after multiple episodes of confusion coincided with skipped meals or sugary snacks, her doctor suggested blood sugar testing. Brenda was ultimately diagnosed with prediabetes, and her cognitive symptoms improved greatly with better glucose control.
The NIDDK recommends tracking cognitive symptoms alongside your eating patterns. If brain fog, forgetfulness, or sudden confusion often emerge before meals, after eating sweets, or when you go long hours without food, unstable glucose could be the cause. Documenting these patterns can help your healthcare provider pinpoint the underlying issue.
12. Irregular Periods and Blood Sugar

While irregular periods are a hallmark of perimenopause, blood sugar issues—particularly insulin resistance—can also disrupt the menstrual cycle. Insulin resistance interferes with how the body regulates both glucose and reproductive hormones, sometimes leading to skipped or unpredictable periods. According to the CDC, women with insulin resistance or prediabetes are at increased risk for polycystic ovary syndrome (PCOS), a condition that can cause missed periods, heavy bleeding, or prolonged cycles even before menopause begins.
Menopause-driven cycle changes usually appear as a natural transition in your late 40s or early 50s, with periods becoming lighter or less frequent over time. In contrast, blood sugar-related irregularities can occur at any age and may be accompanied by other symptoms such as unexplained weight gain, acne, or excessive hair growth. These changes are often more abrupt and may be reversible with improved glucose management.
The Office on Women’s Health recommends meticulously tracking your menstrual cycles—noting frequency, flow, and any associated symptoms. Sharing this information with your healthcare provider can help distinguish between perimenopausal changes and those linked to underlying blood sugar imbalances, ultimately guiding more effective treatment.
13. Sleep Disturbances

Sleep disturbances are a frustrating and common complaint for women in midlife, often blamed solely on menopause. However, both high and low blood sugar can significantly disrupt sleep quality and duration. According to the CDC, low blood sugar (hypoglycemia) at night can cause sudden awakenings, night sweats, and even nightmares, while high blood sugar (hyperglycemia) may lead to frequent urination, excessive thirst, and difficulty falling or staying asleep.
Menopause-related insomnia is typically linked to hormonal changes, hot flashes, and mood shifts, resulting in trouble falling asleep or waking up too early. These symptoms often present gradually as estrogen levels decline. In contrast, sleep issues from blood sugar swings may appear suddenly and are frequently associated with specific triggers, such as eating a heavy, high-carbohydrate meal before bed or skipping dinner.
The Sleep Foundation recommends tracking your sleep patterns alongside meal timing and nighttime symptoms. Note when you wake up, any physical symptoms (like sweating or rapid heartbeat), and your last meal or snack. This information can help your healthcare provider differentiate between menopause-related insomnia and sleep disturbances linked to blood sugar, leading to more targeted support.
14. Skin Changes

Skin changes can provide important clues about underlying health issues. One of the hallmark signs of insulin resistance and elevated blood sugar is acanthosis nigricans—dark, velvety patches that commonly appear on the neck, armpits, elbows, or groin. According to the CDC, these patches are caused by excess insulin stimulating skin cells to grow abnormally, and they may be an early warning sign of prediabetes or type 2 diabetes.
In contrast, menopause often leads to skin thinning and dryness due to declining estrogen levels. These changes make the skin more fragile, prone to bruising, and slower to heal, but they do not typically result in darkened or thickened patches. Menopausal skin changes tend to develop gradually and are usually accompanied by other signs of aging, such as wrinkles and loss of elasticity.
The American Academy of Dermatology recommends paying close attention to any new or unusual skin changes, especially areas of darkening, thickening, or itchiness. Documenting when and where these changes occur—and sharing this with your healthcare provider—can support early identification of insulin resistance or blood sugar imbalance.
15. Slow-Healing Wounds

Slow-healing wounds are a key sign of elevated blood sugar and may be overlooked as simply part of the aging process. High glucose levels can damage blood vessels and impair circulation, making it harder for oxygen and nutrients to reach injured tissues. The CDC explains that this process weakens the immune response, delays clot formation, and increases the risk of infection, causing even minor cuts and scrapes to linger much longer than usual.
With normal aging, wound healing may slow somewhat due to reduced skin elasticity and a gradual decline in immune function. However, in menopause, this slowdown is typically modest and not as pronounced as the significant delays seen with uncontrolled blood sugar or diabetes. If you notice that small injuries, blisters, or sores take weeks to heal, or if redness and swelling persist, it could indicate an underlying glucose issue rather than just menopause or natural aging.
The NIDDK recommends monitoring recovery time for any wounds or infections. If healing seems unusually slow, especially when paired with other symptoms like frequent infections or skin changes, consult your healthcare provider to discuss blood sugar testing and appropriate care.
16. Yeast Infections
Recurring yeast infections can be a sign of elevated blood sugar, as high glucose levels create an ideal environment for yeast (especially Candida) to thrive. The CDC notes that women with poorly managed blood sugar are at greater risk for frequent vaginal yeast infections, since excess sugar is excreted in urine and can disrupt the natural balance of bacteria and yeast in the vaginal area.
While menopause is also associated with vaginal changes, such as dryness, thinning of the vaginal walls, and a shift in pH levels, these changes primarily increase discomfort and may lead to irritation or mild infections. However, true yeast infections—characterized by itching, burning, and thick, white discharge—are more commonly linked to blood sugar imbalances than to menopause alone.
The Office on Women’s Health recommends tracking the frequency and severity of yeast infections. If you experience multiple infections in a short period or if standard treatments are ineffective, it’s important to discuss these patterns with your healthcare provider. Persistent or recurrent yeast infections may warrant blood glucose testing to rule out diabetes or prediabetes as an underlying cause.
17. Sexual Health Changes

Sexual health changes are common in midlife, but blood sugar imbalances can play a significant role alongside menopause. High blood sugar can damage blood vessels and nerves, leading to decreased blood flow and reduced sensation in the genital area. According to the CDC, women with diabetes or insulin resistance may experience lower libido, difficulty achieving arousal, and even pain during intercourse due to these physiological changes.
Menopause also impacts sexual health, primarily through declining estrogen, which causes vaginal dryness, thinning of the vaginal walls, and reduced natural lubrication. While these changes can make intimacy uncomfortable or less pleasurable, they are different from the loss of sensation, reduced arousal, and delayed orgasm that can result from neuropathy or vascular impairment caused by uncontrolled blood sugar.
The Johns Hopkins Medicine recommends openly discussing any persistent sexual health concerns with your healthcare provider. If you notice a sudden or pronounced drop in libido, ongoing arousal difficulties, or pain not relieved by typical menopause therapies, it may be worthwhile to consider blood sugar testing as part of your evaluation for sexual health changes.
18. Increased Hunger

Experiencing increased hunger, known as polyphagia, is often a warning sign of blood sugar disorders such as diabetes or insulin resistance. When blood sugar remains elevated, glucose cannot effectively enter the body’s cells, leaving them starved for energy despite abundant sugar in the bloodstream. This prompts persistent or extreme hunger, sometimes accompanied by rapid weight loss or fatigue. The CDC lists excessive hunger as a hallmark symptom of both type 1 and type 2 diabetes.
Menopause can also influence appetite, but these changes are generally more subtle and related to hormone fluctuations, mood, or sleep disturbances rather than a physiological urge to eat continually. Appetite during menopause often fluctuates but rarely results in the unrelenting, urgent hunger seen with uncontrolled blood sugar.
The NIDDK recommends noting specific hunger patterns—such as strong urges to eat soon after a meal, waking up hungry at night, or feeling weak or shaky if you miss a meal. If you observe persistent or unexplained increases in hunger, especially when paired with other symptoms like fatigue or frequent urination, consult your healthcare provider to discuss blood glucose testing.
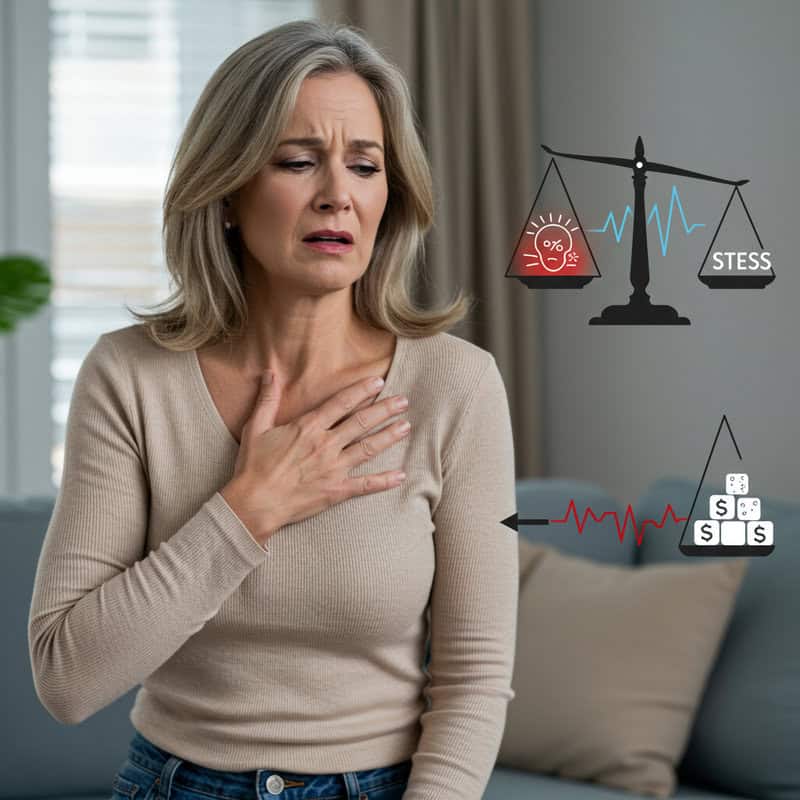
19. Heart Palpitations

Heart palpitations—the sensation of a racing, fluttering, or pounding heartbeat—can be alarming and are frequently experienced by women during both menopause and blood sugar fluctuations. Blood sugar extremes, particularly hypoglycemia (low blood sugar), can stimulate the release of adrenaline, the body’s “fight or flight” hormone, resulting in rapid heart rate and palpitations. According to the CDC, these symptoms may also be accompanied by shakiness, sweating, or anxiety. Conversely, high blood sugar can stress the cardiovascular system and sometimes cause similar sensations.
Menopause-related palpitations are typically linked to declining estrogen, which can affect how the body regulates heart rhythm and blood pressure. These episodes may occur independently or be triggered by hot flashes and anxiety, often appearing suddenly during perimenopause or early menopause. However, palpitations caused by blood sugar swings often follow skipped meals, heavy exercise, or consumption of sugary foods.
The American Heart Association recommends monitoring your heart rate and noting when palpitations occur. If you notice a pattern associated with eating, fasting, or other blood sugar-related symptoms, discuss these findings with your healthcare provider and request a blood glucose evaluation.
20. Dry Mouth

Dry mouth, or xerostomia, is another symptom that can be easily confused between menopause and blood sugar disorders. Elevated blood sugar levels lead to dehydration as the body attempts to flush out excess glucose through increased urination, leaving the mouth feeling persistently dry. The CDC explains that this lack of moisture not only causes discomfort but can also increase the risk of dental problems, gum disease, and oral infections.
Menopause is also linked to dryness, not only in the mouth but also in the eyes and vaginal tissues, due to declining estrogen. While menopausal dryness is often widespread, dry mouth caused by blood sugar issues tends to be more severe and may be accompanied by increased thirst and frequent urination.
The American Dental Association recommends staying well-hydrated and practicing good oral hygiene, including regular dental checkups. If you experience ongoing dry mouth, especially alongside other symptoms such as increased thirst or urination, consult your healthcare provider about blood sugar testing to help protect both your oral and overall health.
21. Gum Disease

Gum disease—including gingivitis and periodontitis—has a strong connection to high blood sugar. When glucose levels are elevated, the body’s ability to fight bacteria is compromised, making the gums more susceptible to inflammation, swelling, and bleeding. The CDC highlights that people with diabetes are at a higher risk for gum infections, receding gums, and tooth loss, as bacteria thrive in the sugar-rich environment of the mouth.
Menopause can also bring oral health changes due to decreased estrogen, such as dry mouth, burning sensations, and a higher risk of cavities. However, menopause-related oral symptoms tend to be less severe than the chronic, progressive inflammation and infection associated with uncontrolled blood sugar. If you notice persistent gum tenderness, bleeding during brushing or flossing, or loose teeth, blood sugar imbalance could be a factor.
The American Dental Association recommends regular dental checkups and cleanings to catch gum disease early. Good oral hygiene, combined with blood sugar control, is vital for preventing complications. If you experience worsening gum issues alongside other symptoms of blood sugar imbalance, discuss testing options with both your dentist and healthcare provider.
22. Frequent Infections
High blood sugar can significantly impair the immune system, making it harder for the body to fight off bacteria, viruses, and fungi. Prolonged hyperglycemia weakens white blood cell function and slows down the body’s natural healing processes, leading to a higher risk of recurrent infections. The CDC notes that people with diabetes are particularly susceptible to urinary tract infections, skin infections, respiratory illnesses, and even more serious complications like pneumonia.
For example, Karen, a 54-year-old librarian, noticed she was getting frequent urinary tract and sinus infections despite maintaining good personal hygiene. Initially, she attributed these illnesses to stress and menopause, but her infections persisted over several months. After finally seeking medical advice and undergoing blood glucose testing, Karen was diagnosed with type 2 diabetes. Her infection rate decreased dramatically once her blood sugar was brought under control.
The NIDDK urges women to report any pattern of frequent or stubborn infections to their healthcare provider. Repeated illness is not a normal part of menopause or aging and could be a sign of an underlying blood sugar disorder requiring timely diagnosis and treatment.
23. Itchy Skin

Itchy skin, or pruritus, is a common but often overlooked symptom of blood sugar imbalance. Elevated glucose levels can lead to dehydration and poor circulation, both of which dry out the skin and cause persistent itching. Additionally, high blood sugar can increase the risk of skin infections and fungal overgrowth, compounding discomfort. The CDC notes that people with diabetes are more prone to itchy, irritated skin—especially on the legs, arms, and trunk.
Menopause can also bring skin dryness and itching, usually due to declining estrogen, which reduces oil production and skin elasticity. Menopausal itching tends to be more generalized and may present alongside other symptoms such as hot flashes and night sweats. However, when itching is persistent, severe, or accompanied by visible skin changes like dark patches or slow-healing sores, it may point to an underlying blood sugar issue.
The American Academy of Dermatology recommends using moisturizer regularly to soothe dry skin and keeping an eye on other diabetes symptoms. If you experience ongoing or unexplained itching, consider discussing blood sugar testing with your healthcare provider to rule out diabetes or prediabetes as a contributing factor.
24. Vision Changes Over Time

Gradual vision changes can signal more than just the normal effects of aging. Persistent high blood sugar can damage the tiny blood vessels in the retina, leading to a condition called diabetic retinopathy. This progressive eye disease can result in blurred vision, floaters, difficulty seeing at night, and eventually, vision loss if left untreated. According to the CDC, diabetic retinopathy is a leading cause of blindness among adults and is often preventable with early detection and blood sugar control.
Age-related vision loss and menopause can also affect eyesight, typically through presbyopia (trouble focusing on close objects), cataracts, or dry eyes. These changes develop slowly and are not accompanied by the sudden or fluctuating vision disturbances seen in diabetic eye disease. Menopausal changes in vision are rarely severe or progressive unless complicated by other underlying conditions.
The American Academy of Ophthalmology strongly recommends regular, comprehensive eye exams—especially for women with risk factors for diabetes or a history of blood sugar problems. Early diagnosis of diabetic retinopathy can help prevent serious complications, preserve vision, and ensure prompt intervention if changes are detected.
25. Swelling in Hands or Feet

Swelling in the hands or feet, known as edema, can be an indicator of underlying blood sugar problems. Consistently high blood sugar can damage blood vessels and impair circulation, making it harder for fluids to be properly returned from the extremities to the heart. Over time, this can cause persistent puffiness, tightness, or a feeling of heaviness, particularly in the ankles, feet, or fingers. The CDC highlights that people with diabetes are at increased risk for swelling due to both poor circulation and kidney involvement.
Menopause may also cause mild, temporary swelling due to hormonal shifts and water retention, but these episodes tend to be short-lived and less severe. Menopausal swelling often fluctuates with diet, heat, or physical activity, whereas blood sugar-related edema may become chronic and progressively worse if not addressed.
The NIDDK recommends closely monitoring any swelling that persists for more than a few days or is accompanied by skin color changes, numbness, or pain. If you notice ongoing or worsening swelling in your hands or feet, consult your healthcare provider to discuss blood sugar testing and further evaluation.
26. Nausea and Vomiting

Nausea and vomiting can be distressing symptoms of blood sugar imbalance, particularly when glucose levels are either extremely high or low. In cases of severe hyperglycemia, such as diabetic ketoacidosis (DKA), the body produces excess acids, leading to nausea, vomiting, abdominal pain, and even confusion. According to the CDC, these symptoms are a medical emergency and require prompt attention. Even mild blood sugar swings can irritate the stomach, causing periodic queasiness or indigestion.
Menopause is less commonly associated with nausea or vomiting. While some women may experience mild gastrointestinal discomfort during hormonal transitions, persistent or severe nausea is more likely to indicate another underlying problem, such as blood sugar dysregulation or infection.
The NIDDK advises seeking immediate medical care if nausea or vomiting is severe, persistent, or accompanied by symptoms like abdominal pain, dehydration, or confusion. For milder cases, tracking the timing and frequency of gastric upset in relation to meals and other symptoms can help your healthcare provider determine whether blood sugar fluctuations may be the root cause.
27. Dizziness or Fainting

Dizziness or fainting can be alarming and are classic signs of blood sugar instability, particularly hypoglycemia (low blood sugar). When glucose drops too low, the brain and other organs are deprived of the energy they need, causing symptoms such as dizziness, lightheadedness, shakiness, confusion, or even fainting. The CDC notes that hypoglycemic episodes can happen suddenly, especially after skipping meals, intense exercise, or taking certain diabetes medications.
Menopause can also contribute to episodes of lightheadedness, usually as a result of hot flashes, dehydration, or low blood pressure from hormonal changes. However, these are typically brief and associated with clear triggers, such as standing up quickly or being in a hot environment, rather than occurring in relation to meal timing or fasting.
The NIDDK recommends tracking all episodes of dizziness or fainting, noting when they occur, their severity, and any related factors such as missed meals or physical activity. If you notice a pattern, especially if symptoms correlate with eating habits, consult your healthcare provider for evaluation and possible blood sugar testing.
28. Slow Hair Growth or Loss
Slow hair growth or increased hair loss can be subtle signals that something is amiss with your body’s internal balance. Chronic high blood sugar damages the small blood vessels that supply hair follicles with nutrients and oxygen, leading to thinning hair, slower growth, and, in some cases, patchy hair loss. The CDC notes that diabetes-related circulation problems can affect both scalp and body hair, making growth cycles less robust and causing more strands to fall out than usual.
Menopause is also a common time for hair changes, usually due to declining estrogen and progesterone levels. These hormonal shifts can make hair finer, thinner, and more prone to shedding, but the progression is often gradual and affects the entire scalp rather than specific patches. In contrast, blood sugar-related hair changes may occur alongside other symptoms such as slow-healing skin, tingling in the extremities, or unexplained weight changes.
The American Academy of Dermatology suggests noting any new patterns of hair loss or slowed growth and sharing these observations with your healthcare provider. Sudden or pronounced hair changes should prompt consideration of blood glucose evaluation, especially if other diabetes warning signs are also present.
29. Darkening of Skin Folds
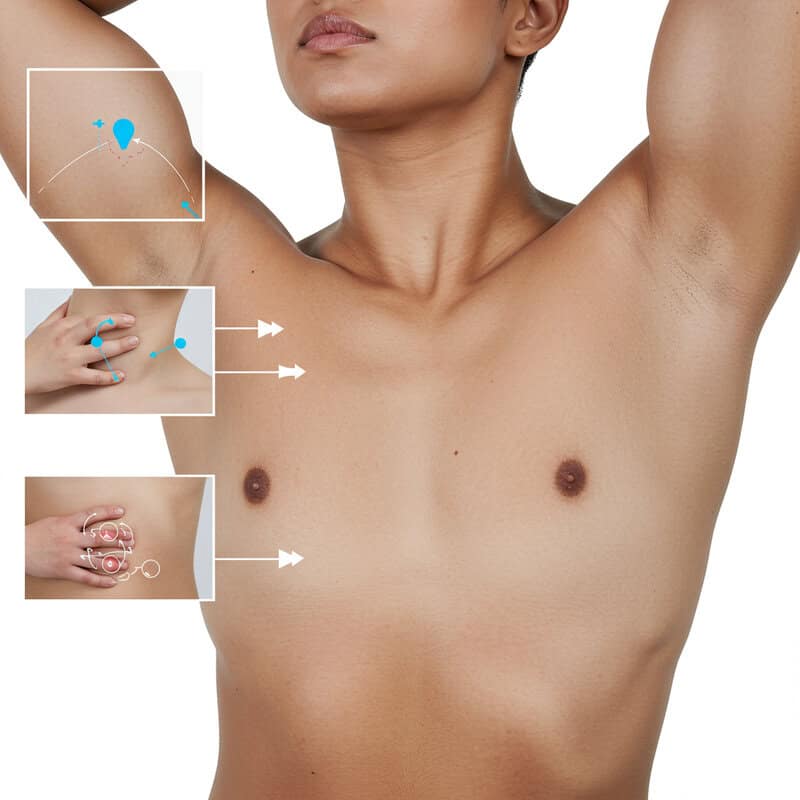
Darkening of skin folds, medically known as acanthosis nigricans, is a recognizable skin change often linked to insulin resistance and high blood sugar. This condition causes thickened, velvety, and dark patches to appear in areas where skin creases—such as the neck, armpits, groin, and sometimes the elbows or knees. According to the CDC, acanthosis nigricans is considered an early warning sign of prediabetes or type 2 diabetes, as elevated insulin levels stimulate skin cell growth and increased pigment production.
Typical menopausal skin changes, by contrast, include thinning, dryness, and a gradual loss of elasticity due to reduced estrogen levels. While menopause can lead to increased skin sensitivity and sometimes itchiness, it does not generally cause the distinctive dark, velvety patches seen with acanthosis nigricans.
The American Academy of Dermatology advises women to regularly check their skin for new or unusual changes, especially in body folds. Noting the appearance and timing of these changes—and reporting them to your healthcare provider—can lead to early intervention, lifestyle adjustments, and blood glucose evaluation if insulin resistance is suspected.
30. Unexplained Bruising

Unexplained bruising can be a subtle but important sign of underlying blood sugar problems. Chronic high blood glucose levels can damage blood vessels and interfere with the function of platelets, which are essential for proper blood clotting. This can make the skin more susceptible to bruising even after minor bumps, or sometimes without any apparent cause. The CDC states that poor circulation and delayed wound healing, both common in diabetes, also contribute to increased bruising and slower recovery.
Menopause may cause some increased bruising as a result of thinning skin and reduced collagen due to declining estrogen, but this is generally mild and develops gradually over time. If you notice frequent or severe bruising that appears suddenly or is accompanied by other signs of blood sugar imbalance—such as slow-healing wounds, persistent infections, or unexplained fatigue—this may indicate a more serious underlying issue.
The NIDDK recommends monitoring your skin for new or frequent bruises. Keeping track of when and where they appear, and sharing this with your healthcare provider, can help facilitate timely blood glucose testing and appropriate care.
31. Poor Circulation
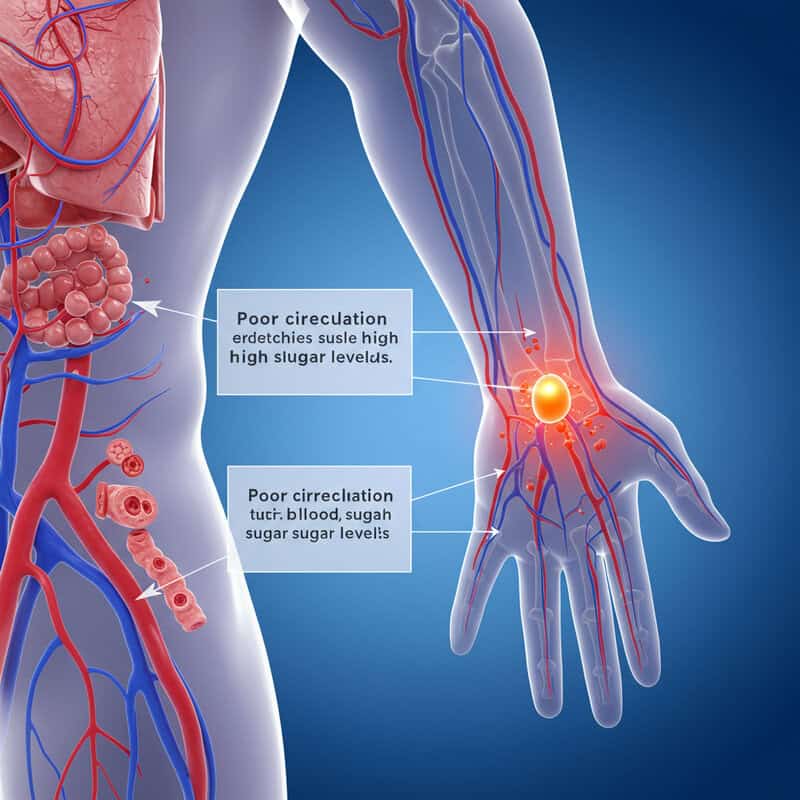
Poor circulation is a serious complication that can develop when high blood sugar persists over time. Chronic hyperglycemia damages the lining of blood vessels, leading to decreased elasticity, narrowing of the arteries, and impaired blood flow to the extremities. This can result in symptoms such as cold hands and feet, numbness, tingling, and even delayed wound healing. The CDC warns that people with diabetes are at higher risk for peripheral artery disease and other vascular conditions that further restrict circulation, heightening the risk of ulcers and infections.
Menopause can also affect vascular health, as declining estrogen may reduce blood vessel flexibility and increase the likelihood of hot flashes or mild temperature fluctuations. However, menopause-related vascular changes are generally less severe and typically do not cause persistent coldness, numbness, or significant reduction in peripheral blood flow.
The NIDDK recommends checking regularly for cold, pale, or numb extremities and being alert for any wounds or sores that heal slowly. If poor circulation is persistent or worsening, particularly if accompanied by other signs of blood sugar imbalance, consult your healthcare provider for evaluation and possible glucose testing.
32. Chest Pain or Tightness
Chest pain or tightness is a potentially serious symptom that can be linked to the cardiovascular complications of chronic high blood sugar. Long-term hyperglycemia accelerates the buildup of plaque in the arteries, increasing the risk of coronary artery disease and heart attacks. The CDC emphasizes that diabetes is a major risk factor for heart disease, and chest discomfort should never be ignored, especially if accompanied by shortness of breath, sweating, or pain radiating to the arm or jaw.
Menopause may also bring heart-related symptoms due to the drop in estrogen, which has a protective effect on the cardiovascular system. Some women experience palpitations, mild chest fluttering, or increased awareness of their heartbeat during hot flashes or periods of anxiety. However, these symptoms are generally less severe and not associated with exertion or persistent pain.
The American Heart Association strongly recommends seeking prompt medical attention for any chest pain or tightness, especially if you have risk factors for diabetes or cardiovascular disease. Quick evaluation can save lives and help distinguish between menopause-related symptoms and those caused by underlying blood sugar or heart issues.
33. Difficulty Concentrating

Difficulty concentrating or maintaining focus—sometimes described as “brain fog”—is a common symptom of blood sugar fluctuations. When glucose levels drop too low or spike too high, the brain does not receive a steady supply of energy, leading to lapses in attention, forgetfulness, and trouble processing information. The CDC notes that both hypoglycemia and hyperglycemia can significantly impair cognitive function, making it hard to complete tasks, remember details, or make decisions.
Menopause can also impact mental clarity due to declining estrogen, resulting in temporary forgetfulness or reduced multitasking ability. These cognitive changes tend to be more gradual and are often intertwined with poor sleep or mood fluctuations. In contrast, blood sugar-related concentration problems may come on suddenly, especially before meals, after eating sugary foods, or during long periods without food.
The NIDDK recommends noting patterns in your mental clarity, such as when you feel most alert or foggy during the day and how these episodes relate to your meals or snacks. Documenting these details can help your healthcare provider distinguish between menopause-related cognitive shifts and those triggered by blood sugar instability.
34. Anxiety or Panic Attacks
Anxiety or panic attacks can be triggered or worsened by blood sugar swings, particularly hypoglycemia. When blood glucose drops too low, the body releases stress hormones such as adrenaline to counteract the deficit, resulting in symptoms like nervousness, trembling, racing heart, and even intense panic. According to the CDC, these episodes may be sudden and severe, often mistaken for generalized anxiety or menopausal mood changes.
Consider the scenario of Diane, a 50-year-old woman who began experiencing panic attacks at work, particularly late in the morning after skipping breakfast. She described sweating, heart palpitations, and a sense of impending doom—symptoms that subsided after eating. Upon tracking her episodes, she and her healthcare provider traced the cause to low blood sugar rather than menopause or an anxiety disorder.
The National Institute of Mental Health (NIMH) recommends tracking anxiety episodes in relation to your eating habits, physical activity, and other symptoms. If you notice anxiety or panic frequently occurs when you haven’t eaten or after consuming sugary foods, consider discussing blood sugar testing with your healthcare provider to address the underlying cause.
35. Restless Legs

Restless legs—an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations—can be a symptom of nerve damage (neuropathy) associated with blood sugar disorders. Chronically high blood glucose can damage the nerves in the legs, causing tingling, burning, itching, or a creepy-crawly feeling that worsens at night or while at rest. According to the CDC, diabetic neuropathy can significantly disrupt sleep, leading to increased fatigue and reduced quality of life.
Menopause can also contribute to sleep disturbances and periodic leg discomfort, usually due to hormonal changes, hot flashes, or muscle cramps. However, menopausal symptoms tend to be more generalized and are less likely to produce the specific, persistent sensations characteristic of restless legs from neuropathy.
The NIDDK recommends noting the timing, frequency, and severity of nighttime leg discomfort. If you experience ongoing restless legs, particularly if symptoms worsen at night or are accompanied by numbness, tingling, or burning, discuss these patterns with your healthcare provider to determine if blood sugar testing and further evaluation are warranted.
36. Loss of Muscle Mass
Loss of muscle mass, also known as muscle wasting, can be a consequence of prolonged high blood sugar. When glucose cannot efficiently enter cells due to insulin resistance or deficiency, the body starts breaking down muscle tissue for energy. The CDC notes that unexplained muscle loss—particularly when accompanied by fatigue, weight loss, and increased hunger—may signal undiagnosed diabetes or poor glucose control. Muscle breakdown is often more rapid and severe in blood sugar disorders than in normal aging processes.
Menopause is naturally associated with gradual muscle loss due to declining estrogen and physical inactivity, but this process tends to be slow and can often be counteracted with diet and resistance exercise. Menopause-related muscle loss rarely results in pronounced weakness or visible wasting unless compounded by other health issues. In contrast, muscle loss from blood sugar imbalances may be sudden and happen alongside other symptoms like increased thirst or frequent urination.
The NIDDK recommends monitoring changes in muscle strength and mass. If you notice difficulty performing everyday tasks, rapid muscle loss, or new weakness, especially when paired with other diabetes symptoms, consult your healthcare provider for blood sugar testing and a comprehensive evaluation.
37. Shortness of Breath

Shortness of breath can be a serious signal of complications related to blood sugar disorders. In cases of severely uncontrolled diabetes, diabetic ketoacidosis (DKA) may develop, causing rapid, deep breathing and a fruity breath odor as the body attempts to expel excess acids. According to the CDC, DKA is a medical emergency, and breathlessness may be accompanied by nausea, confusion, or abdominal pain. Chronic high blood sugar also increases the risk of heart disease, which can present as chest tightness and difficulty breathing.
Menopause itself does not typically cause shortness of breath, though some women may experience temporary breathlessness during hot flashes or anxiety attacks. These episodes are usually brief and not associated with exertion or progressive symptoms.
The American Heart Association urges prompt evaluation of any new or unexplained shortness of breath, especially if it is accompanied by chest pain, palpitations, or signs of illness. If you develop sudden or persistent breathlessness, seek immediate medical care to rule out diabetic emergencies, heart complications, or other serious underlying conditions related to blood sugar imbalance.
38. Bloating or Digestive Changes

Bloating or digestive changes can sometimes be a sign of blood sugar disorders, particularly when related to a condition called gastroparesis. Gastroparesis is a form of delayed stomach emptying caused by damage to the nerves (especially the vagus nerve) that control digestive muscles, a complication often seen in diabetes. According to the NIDDK, symptoms include bloating, nausea, early satiety, abdominal pain, and erratic blood sugar levels due to unpredictable digestion and absorption of food.
Menopause may also affect digestion, but these changes are typically related to fluctuating hormones that can slow gut motility, increase constipation, or cause mild bloating. Menopausal digestive symptoms are usually less severe and rarely lead to significant weight loss or persistent gastric distress.
The CDC recommends tracking the frequency and severity of gastrointestinal symptoms such as bloating, nausea, vomiting, or changes in bowel habits. If you notice ongoing digestive discomfort, particularly if it interferes with eating or is accompanied by other signs of blood sugar imbalance, speak with your healthcare provider to discuss further evaluation and possible blood glucose testing.
39. Difficulty Healing from Infections
Difficulty healing from infections is a significant concern for individuals with chronically high blood sugar. Elevated glucose levels impair the function of white blood cells, which are crucial for mounting an effective immune response. This makes it harder for the body to fight off bacteria, viruses, and fungi, leading to illnesses that linger or frequently recur. The CDC reports that people with diabetes often experience longer recovery times from common infections and are at higher risk for complications such as cellulitis, pneumonia, and urinary tract infections.
In menopause, recovery from infections may be slightly slower due to age-related changes in immune function, but this delay is generally mild. Menopausal women may experience more frequent vaginal or urinary infections because of hormonal changes, but overall healing is not as severely compromised as it is in those with poorly controlled blood sugar.
The NIDDK recommends noting any pattern of prolonged illness or slow recovery from infections. If you find that colds, wounds, or other infections take much longer to resolve than in the past, or if you experience frequent relapses, consult your healthcare provider to discuss blood glucose testing and personalized treatment plans.
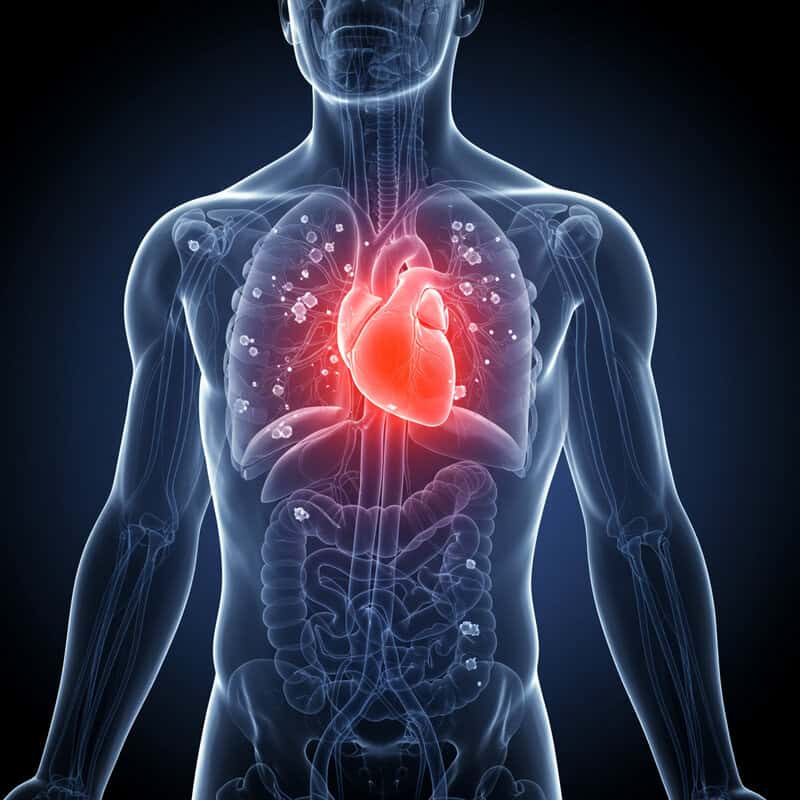
40. Increased Risk of Cardiovascular Disease
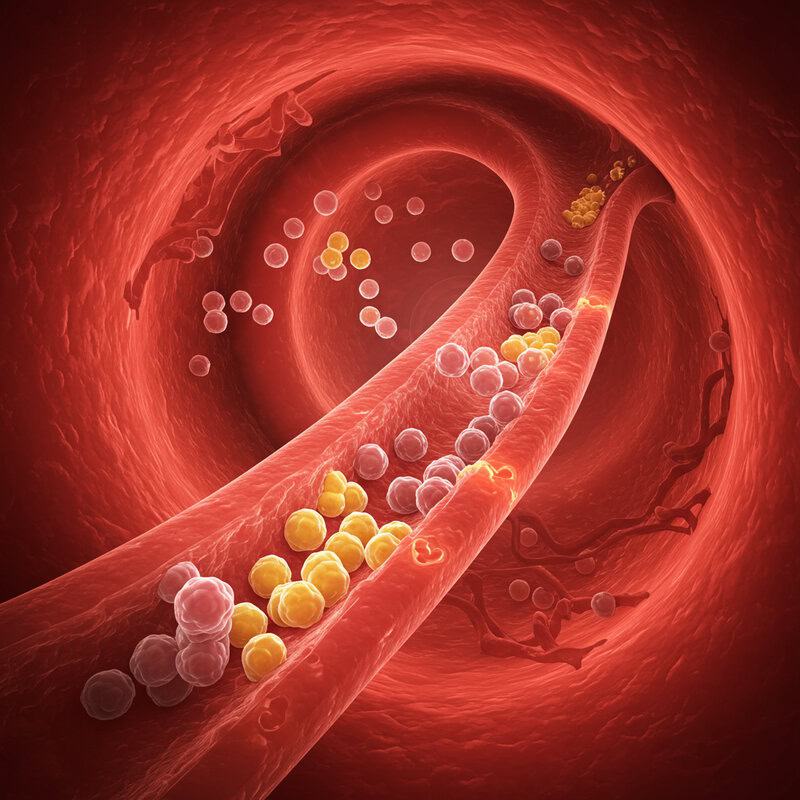
Increased risk of cardiovascular disease is one of the most serious long-term complications of blood sugar disorders such as diabetes and insulin resistance. Chronic high glucose levels damage the lining of blood vessels, promote inflammation, and accelerate the buildup of plaque in the arteries, raising the risk of heart attack, stroke, and peripheral arterial disease. According to the CDC, adults with diabetes are twice as likely to have heart disease or stroke compared to those without diabetes, and these conditions often develop at a younger age.
Menopause also increases cardiac risk, primarily due to the loss of estrogen’s protective effect on the heart and blood vessels. However, menopause-related risk develops more gradually and is often compounded by other factors such as weight gain, high cholesterol, and inactivity. When combined with uncontrolled blood sugar, the dangers to heart health are greatly magnified.
The American Heart Association recommends regular heart health screenings for women, especially those with additional risk factors like high blood sugar, high blood pressure, or a family history of heart disease. Early detection and management are key to preventing life-threatening complications and maintaining long-term cardiovascular wellness.
41. Muscle Cramps

Muscle cramps are a painful and sometimes debilitating symptom that can be linked to blood sugar imbalances. In cases of uncontrolled diabetes or frequent blood sugar fluctuations, the body may lose excessive fluids and electrolytes (such as sodium, potassium, and magnesium) through increased urination. These shifts in electrolyte balance can trigger involuntary muscle contractions and cramps, especially in the legs and feet. The CDC highlights cramps and muscle pain as possible warning signs of poorly managed diabetes.
Menopause can also bring occasional muscle cramps, usually related to hormone-driven changes in fluid retention, reduced physical activity, or night sweats. However, cramps from menopause tend to be less frequent and not as strongly tied to dehydration or electrolyte loss.
The NIDDK recommends staying hydrated and monitoring for recurring muscle cramps. If cramps occur often—particularly if they wake you at night or coincide with other symptoms of blood sugar imbalance—consider discussing blood sugar testing with your healthcare provider. Prompt evaluation can help identify the root cause and prevent further complications.
42. Changes in Sense of Smell or Taste

Changes in sense of smell or taste can occur when blood sugar is poorly controlled. High glucose levels and related nerve damage (neuropathy) can impair the function of the sensory nerves in the mouth and nose, leading to dulled or altered perception of flavors and scents. According to the CDC, people with diabetes often report a metallic taste, decreased ability to taste sweetness, or a general blunting of their sense of taste. These issues may also be compounded by dry mouth, frequent infections, or oral inflammation linked to blood sugar problems.
Menopause can bring some mild changes in taste or smell due to hormonal fluctuations, but these are typically subtle and not as persistent as those caused by blood sugar instability. Sensory changes in menopause are more often related to medication side effects or nasal congestion from allergies rather than nerve damage.
The NIDDK recommends noting any persistent changes in sense of smell or taste, especially if they coincide with other symptoms of blood sugar imbalance. Sharing these observations with your healthcare provider can help facilitate early diagnosis and targeted treatment.
43. Persistent Dry Eyes

Persistent dry eyes are a frequent complaint among people with blood sugar disorders, especially diabetes. High blood glucose can disrupt the normal functioning of the tear glands and nerves responsible for eye lubrication, leading to inadequate tear production. This results in dryness, burning, redness, and a gritty or sandy sensation in the eyes. According to the CDC, people with diabetes are at increased risk for dry eye syndrome, which can further raise the risk of infections, corneal damage, and impaired vision if left untreated.
Menopause is another common cause of dry eyes, as declining estrogen levels reduce tear film stability and moisture. However, menopausal dry eye is generally less severe and may respond more readily to simple lifestyle changes or over-the-counter remedies. In contrast, dry eyes from blood sugar disorders may be persistent and resistant to standard treatments, especially when accompanied by other symptoms like blurry vision or frequent infections.
The American Academy of Ophthalmology recommends using artificial tears to relieve symptoms and monitoring for persistent or worsening dryness. If relief is temporary or symptoms are accompanied by other diabetes warning signs, consult your healthcare provider or eye doctor for a comprehensive evaluation.
44. Loss of Interest in Hobbies

Loss of interest in hobbies and activities previously enjoyed can be an underrecognized sign of blood sugar instability. Chronic highs or lows can disrupt the balance of neurotransmitters in the brain, leading to apathy, decreased motivation, and even depression. According to the National Institute of Mental Health (NIMH), poorly controlled diabetes is linked to an increased risk of mood disorders, including loss of interest in daily life and social withdrawal.
Menopause also brings mood changes that may affect motivation and pleasure, largely due to hormonal fluctuations. However, menopausal mood symptoms tend to fluctuate and are often accompanied by irritability, sleep disturbances, or hot flashes. In contrast, loss of interest associated with blood sugar issues may be more persistent and can occur with or without other classic menopausal symptoms.
The CDC recommends noting any sustained changes in your enjoyment of hobbies or social activities. If you notice a prolonged loss of interest—especially alongside fatigue, appetite changes, or other signs of blood sugar imbalance—bring these patterns to your healthcare provider’s attention for appropriate evaluation and support.
45. Unusual Body Odor

Unusual body odor can be a distinctive sign of uncontrolled blood sugar, particularly in cases of diabetic ketoacidosis (DKA). When the body cannot use glucose for energy due to lack of insulin, it begins to break down fat, producing ketones as a byproduct. These ketones can accumulate and cause a fruity or acetone-like odor on the breath, sweat, or urine. According to the CDC, DKA is a medical emergency most common in type 1 diabetes but can also occur in type 2 diabetes under extreme stress or illness.
Menopause may lead to changes in body odor due to increased sweating during hot flashes, but these odors are more likely to be described as musty or related to perspiration rather than the distinctive sweet, chemical scent associated with ketone buildup. Menopausal body odor changes typically fluctuate with hormonal cycles and improve with hygiene measures.
The NIDDK recommends noting any persistent or unusual changes in body odor, especially if accompanied by other symptoms like rapid breathing, confusion, or nausea. Persistent fruity or chemical-like odors should prompt immediate medical evaluation and blood sugar testing.
46. Tingling in the Face

Tingling in the face can be a sign of neuropathy caused by blood sugar imbalances, although it is less common than tingling in the hands and feet. Prolonged high glucose levels can damage nerves throughout the body, including those responsible for facial sensation. This may result in numbness, tingling, or a pins-and-needles feeling in the cheeks, lips, or jaw. According to the CDC, nerve problems due to diabetes—called diabetic neuropathy—can affect any part of the nervous system and may present in unusual locations when blood sugar is poorly controlled.
Menopause, on the other hand, very rarely causes persistent tingling in the face. While temporary sensations might occur during hot flashes or anxiety episodes, these typically resolve quickly and are not associated with ongoing nerve damage.
The NIDDK recommends reporting any persistent or unexplained facial tingling to your healthcare provider. Document the timing, frequency, and any factors that seem to trigger or relieve the sensation. Early evaluation can help determine if blood sugar testing or a neurological assessment is warranted to identify the underlying cause.
47. Loss of Coordination

Loss of coordination can occur when blood sugar levels swing to extremes, affecting the brain and nervous system’s ability to control balance and movement. Hypoglycemia (low blood sugar) can lead to confusion, slowed reflexes, clumsiness, and even difficulty walking, as the brain is deprived of its primary fuel source. Hyperglycemia (high blood sugar) can also damage nerves over time, resulting in impaired proprioception and muscle weakness. The CDC notes that severe or chronic glucose instability can make everyday tasks—such as buttoning a shirt or walking steadily—unexpectedly challenging.
Menopause itself does not typically cause significant loss of coordination, though some women may feel occasional mild dizziness or muscle stiffness from hormonal changes. These symptoms are usually short-lived and less likely to result in frequent stumbling or difficulty with fine motor skills.
The NIDDK recommends noting any new problems with balance, frequent stumbles, or trouble performing coordinated movements. If you notice a persistent or worsening pattern, especially alongside other symptoms of blood sugar imbalance, consult your healthcare provider for evaluation and appropriate testing.
48. Swings in Blood Pressure

Swings in blood pressure are a lesser-known but important sign of blood sugar imbalance. Chronic high blood sugar can damage the blood vessels and interfere with the body’s ability to regulate blood pressure, leading to episodes of both hypertension (high blood pressure) and hypotension (low blood pressure). The CDC highlights that people with diabetes are at increased risk for blood pressure fluctuations due to changes in kidney function, nerve health, and vascular tone.
Menopause can also bring temporary changes in blood pressure, particularly during hot flashes or periods of anxiety. However, these fluctuations are usually short-lived and less likely to cause sustained hypertension or dramatic swings in blood pressure readings. Persistent or extreme variations are more commonly linked to underlying metabolic issues such as diabetes or insulin resistance.
The American Heart Association recommends regular blood pressure monitoring at home for anyone with risk factors for diabetes or heart disease. If you notice frequent or unexplained changes in your blood pressure—especially when accompanied by other symptoms—inform your healthcare provider to determine if blood sugar testing or additional evaluation is necessary.
49. Changes in Body Odor

Changes in body odor can be a subtle indicator of underlying blood sugar issues. In diabetes or uncontrolled blood sugar, metabolic changes result in the production of ketones and other byproducts, which can alter the composition of sweat and give rise to distinct odors. According to the CDC, diabetic ketoacidosis (DKA) can cause a sweet, fruity, or acetone-like odor, while chronic hyperglycemia may lead to a musty or unusual body scent due to the body’s altered metabolic state.
Menopause can also affect body odor, but these changes are typically related to increased perspiration during hot flashes and fluctuations in hormone levels. Menopausal odors are often described as stronger or more pungent sweat, rather than the distinctly sweet or chemical-like scent associated with blood sugar problems. Menopausal body odor usually improves with hygiene and cooling measures, whereas diabetes-related odors may persist regardless of hygiene practices.
The NIDDK recommends noting any persistent or unusual changes in body odor. If you observe a new or ongoing smell that does not respond to regular hygiene, especially if accompanied by other symptoms of blood sugar imbalance, consult your healthcare provider for evaluation and possible glucose testing.
50. When to Get Tested: Key Triggers

Recognizing when to seek blood sugar testing can be challenging, especially as so many symptoms—such as hot flashes, night sweats, fatigue, mood swings, and weight changes—overlap with menopause. However, persistent or unexplained issues like increased thirst, frequent urination, blurred vision, recurring infections, or sudden changes in appetite and energy should prompt further investigation. According to the CDC, millions of women remain undiagnosed because these warning signs are often mistaken for “just menopause.”
Real-world stories illustrate the importance of timely screening. For example, a woman experiencing unrelenting fatigue and hot flashes despite hormone therapy discovered through a simple blood test that she had prediabetes, not early menopause. Another, frustrated by recurring yeast infections and skin changes, found her symptoms resolved after her blood sugar was brought under control.
The NIDDK strongly urges women to request blood sugar testing if they have ongoing symptoms without relief from menopause treatments, especially if there is a family history of diabetes or additional risk factors. Early testing and diagnosis are crucial for effective management and long-term health.
Conclusion

Because so many symptoms of blood sugar imbalances overlap with those of menopause, it’s easy to misinterpret warning signs or overlook a potentially serious underlying issue. Delayed diagnosis of diabetes or prediabetes can lead to complications affecting the heart, nerves, eyes, and overall well-being. If you experience persistent, unexplained, or worsening symptoms—even those commonly associated with menopause—don’t hesitate to seek professional advice. A simple blood sugar screening can provide clarity and guide appropriate treatment. For more information on testing and symptoms, visit the CDC or the NIDDK. Your health and peace of mind are worth the conversation.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





