Skin Cancer Removal: What to Expect & How to Prevent It Forever
Skin cancer is the most commonly diagnosed cancer in the United States, with over 5 million cases treated each year according to the American Cancer Society. The skin, our body’s largest organ, is often exposed to harmful ultraviolet (UV) rays, making it particularly susceptible to cancerous changes. Unfortunately, many cases are detected late due to subtle early symptoms, which complicates treatment and recovery. Early diagnosis and awareness are crucial in combating this growing health challenge, as highlighted by recent statistics from the Centers for Disease Control and Prevention.
1. Understanding Skin Cancer Types
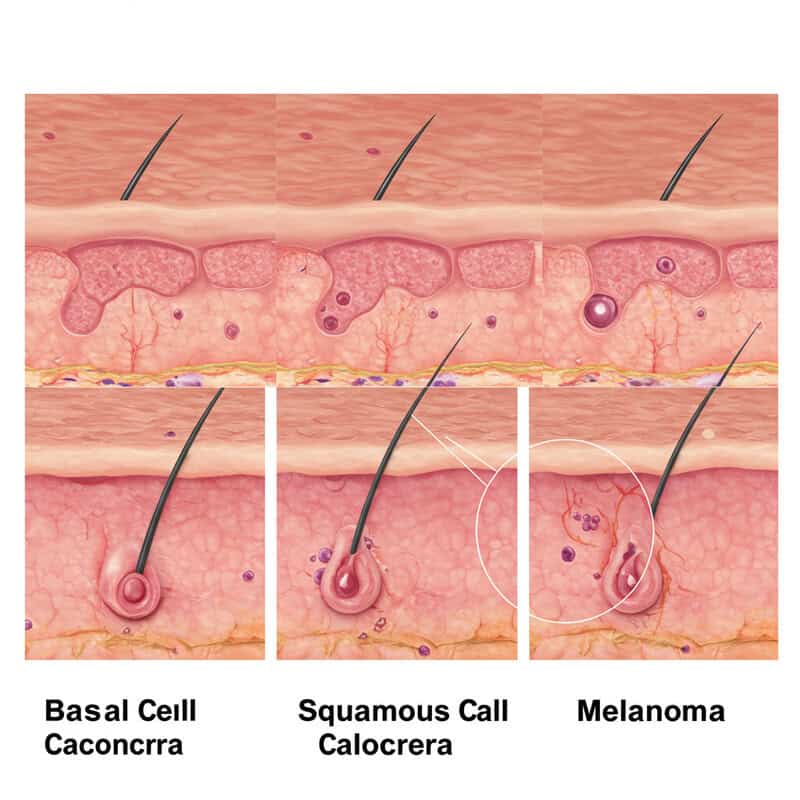
Skin cancer is not a single disease but a group of different cancers that originate in the skin. The three main types are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. Basal cell carcinoma is the most common and usually grows slowly, rarely spreading to other parts of the body. Squamous cell carcinoma, while also slow-growing, can sometimes metastasize if left untreated. Melanoma, though less common, is the most aggressive and deadly form, as it can spread quickly to other organs if not caught early. Understanding the differences between these types is crucial because their treatment approaches and prognoses vary significantly. For example, melanoma often requires more extensive treatment and has a higher risk of recurrence compared to BCC or SCC. Recognizing early signs and seeking prompt medical evaluation can dramatically improve outcomes, especially for melanoma. For more information on skin cancer types and their characteristics, visit the American Cancer Society: Skin Cancer Types and the Skin Cancer Foundation.
2. The Role of UV Radiation

Ultraviolet (UV) radiation, primarily from the sun and tanning beds, is the leading environmental cause of skin cancer. UV rays penetrate the skin and damage the DNA in skin cells, leading to mutations that can initiate cancer development. This damage accumulates over time, increasing the risk of all major types of skin cancer, especially in those with frequent or intense sun exposure. Unlike many other carcinogens, such as tobacco or industrial chemicals, UV radiation is both invisible and often underestimated in daily life. Its effects may not be immediately apparent but can result in significant harm over years. Sun protection is therefore vital—using sunscreen, wearing protective clothing, and seeking shade during peak sunlight hours can dramatically reduce your risk of skin cancer. According to the CDC and the American Cancer Society, practicing sun safety is one of the most effective ways to prevent UV-induced skin damage and lower your lifetime risk of developing skin cancer. Prioritizing sun protection is essential for everyone, regardless of age or skin type.
3. Early Warning Signs
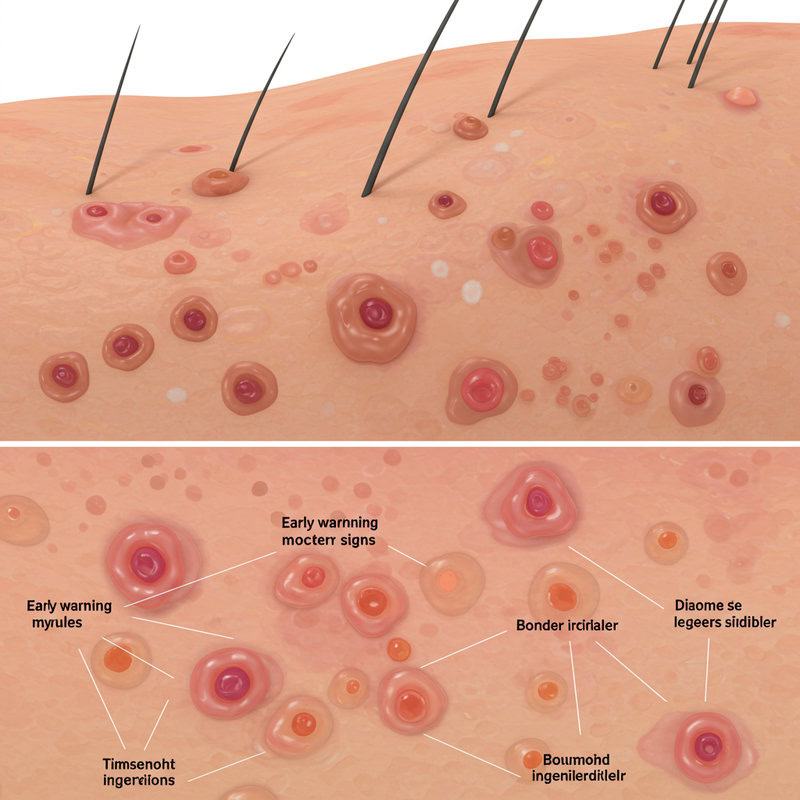
Recognizing the early warning signs of skin cancer can be lifesaving. Common symptoms include new growths, changes in existing moles, or unusual lesions that do not heal. The ABCDE rule is a helpful guide for identifying suspicious moles: A for Asymmetry (one half doesn’t match the other), B for Border irregularity (edges are ragged or blurred), C for Color variation (multiple colors or uneven distribution), D for Diameter (larger than 6 mm, about the size of a pencil eraser), and E for Evolving (changes in size, shape, or color over time). Other warning signs include moles that itch, bleed, or form a scab. Non-melanoma skin cancers, like basal cell and squamous cell carcinoma, may present as persistent, pearly, or scaly bumps, open sores, or red patches. It’s important to perform regular self-examinations and be alert for any skin changes. Early detection greatly increases the chances of successful treatment and recovery. For more details on recognizing early symptoms, visit the American Cancer Society: Signs and Symptoms of Skin Cancer and the Skin Cancer Foundation: Warning Signs.
4. The Importance of Self-Examinations

Regular self-examinations are a proactive way to detect skin cancer early, often before it spreads or becomes more difficult to treat. By familiarizing yourself with the normal appearance of your skin, you can quickly notice any new growths, changes in moles, or unusual spots. Experts recommend performing a full-body skin check once a month, ideally in a well-lit room with the help of a mirror. Don’t forget hard-to-see areas like your back, scalp, soles of the feet, and between your toes. Enlist a partner or use a hand-held mirror for these spots. Take note of any lesions that change, bleed, or do not heal. If you notice something suspicious, schedule a professional evaluation promptly. Keeping a record of your moles through photos can help you track changes over time. According to the American Cancer Society and the American Academy of Dermatology, early detection via self-exam can significantly improve survival rates, especially for melanoma. Making self-examinations a routine habit is a simple yet powerful tool in the fight against skin cancer.
5. Professional Skin Screenings

Professional skin screenings by a dermatologist are a critical step in detecting skin cancer early and assessing your overall skin health. During a dermatology exam, the doctor will conduct a thorough inspection of your entire skin surface, including areas not easily visible to you, such as the scalp, back, and soles of your feet. The dermatologist uses a bright light and sometimes a dermatoscope—a specialized magnifying tool—to closely examine moles and lesions for suspicious features. If a concerning spot is found, a biopsy may be recommended for further analysis. The frequency of screenings depends on your risk factors, such as personal or family history of skin cancer, fair skin, or significant sun exposure. Generally, adults should have a full-body skin exam by a dermatologist once a year, but those at higher risk may require more frequent visits. Between professional exams, continue performing regular self-checks. For more guidance on what to expect and how often to get screened, refer to the Skin Cancer Foundation: Professional Screenings and the American Academy of Dermatology. Early detection by a professional dramatically increases the chances of successful treatment.
6. Biopsy: The Diagnostic Gold Standard

A biopsy is the definitive method for diagnosing skin cancer, confirming whether a suspicious lesion is benign or malignant. During a biopsy, a dermatologist removes a sample—or the entirety—of the abnormal skin tissue for examination under a microscope by a pathologist. There are several types of skin biopsies, each suited to different situations. A shave biopsy involves removing the top layers of skin and is often used for raised lesions. A punch biopsy extracts a deeper, circular section of skin, ideal for sampling all skin layers. An excisional biopsy removes the entire lesion with a margin of normal skin, typically used when melanoma is suspected. The choice of biopsy depends on the size, depth, and location of the lesion as well as the suspected cancer type. Biopsies are usually quick, performed under local anesthesia, and minimally invasive. Only a biopsy can confirm a skin cancer diagnosis and determine the exact type and stage, which guides the choice of treatment. For more on biopsy methods and when they are needed, visit the American Cancer Society: Skin Cancer Diagnosis and the American Academy of Dermatology.
7. Staging Skin Cancer

Staging is a critical process that determines how far skin cancer has progressed, directly impacting treatment decisions and prognosis. The staging system evaluates tumor size, depth, involvement of nearby lymph nodes, and whether the cancer has spread (metastasized) to distant organs. The most widely used system is the TNM system (Tumor, Node, Metastasis), which assigns a stage from 0 (in situ, or localized) to IV (advanced, with widespread metastasis). Early-stage cancers (stage 0 or I) are usually small, confined to the skin, and have a much higher cure rate, often treatable with outpatient procedures. In contrast, higher-stage cancers may require more extensive surgery, immunotherapy, radiation, or chemotherapy, and have a less favorable prognosis. Accurate staging ensures that patients receive the most appropriate and effective treatment. Real-world studies, such as those published by the American Cancer Society and National Cancer Institute, demonstrate that early detection and correct staging significantly improve survival rates and quality of life for skin cancer patients. Understanding the stage of your cancer empowers you to make informed decisions about your care.
8. Excisional Surgery Basics

Excisional surgery is a common and effective method for removing skin cancers, especially when the lesion is small and localized. In this procedure, a surgeon uses a scalpel to cut out the cancerous tissue along with a margin of healthy skin to ensure all malignant cells are removed. The area is then closed with stitches, and the removed tissue is sent to a lab for further examination to confirm clear margins. Most excisional surgeries are performed under local anesthesia in an outpatient setting, allowing patients to return home the same day. Healing time varies depending on the size and location of the excision, but most patients experience minimal discomfort and scarring compared to more invasive procedures. Compared to other treatments like cryotherapy or topical medications, excisional surgery offers a higher cure rate for many skin cancers. Proper wound care, keeping the area clean, and following post-operative instructions are crucial for optimal healing. For more information on what to expect and tips for recovery, visit the Skin Cancer Foundation: Excisional Surgery and the American Academy of Dermatology. Early intervention generally results in better cosmetic and health outcomes.
9. Mohs Micrographic Surgery

Mohs micrographic surgery is a specialized and highly precise technique for removing skin cancer, especially in areas where preserving healthy tissue is crucial, such as the face, ears, and hands. In this procedure, the surgeon removes the visible tumor and then examines thin layers of surrounding skin under a microscope, repeating the process layer by layer until no cancer cells remain. This meticulous approach results in the highest cure rates—up to 99% for certain types of skin cancers—while minimizing the removal of healthy tissue. Mohs surgery is especially recommended for basal cell carcinoma and squamous cell carcinoma that are large, aggressive, have indistinct borders, or have recurred after previous treatment. It’s also ideal for cancers located in cosmetically or functionally sensitive areas. Patients typically receive local anesthesia, and most can go home the same day. Post-operative healing is generally quick, and the cosmetic outcome is often superior due to the tissue-sparing nature of the procedure. For more details on Mohs surgery, including patient experiences and clinical recommendations, visit the Skin Cancer Foundation: Mohs Surgery and the American Academy of Dermatology.
10. Curettage and Electrodessication

Curettage and electrodessication is a common treatment for certain superficial skin cancers, particularly small basal cell carcinomas and squamous cell carcinomas in situ. In this procedure, a dermatologist first numbs the area with local anesthesia, then uses a curette—a sharp, spoon-shaped instrument—to scrape away the cancerous tissue. After scraping, an electric needle is applied to the site to cauterize (burn) the tissue, destroy any remaining cancer cells, and control bleeding. This cycle may be repeated several times to ensure thorough removal. Curettage and electrodessication is most effective for lesions located on the trunk, arms, or legs, where cosmetic appearance is less critical. The technique is not generally recommended for large, aggressive, or recurrent tumors, nor for areas requiring precise cosmetic results, such as the face. Recovery is usually straightforward: the treated area may scab and heal over a few weeks, with mild discomfort and a low risk of infection. Keeping the wound clean and covered can promote faster healing and reduce scarring. For more details on these procedures and post-care advice, visit the Skin Cancer Foundation: Curettage & Electrodessication and the American Academy of Dermatology.
11. Cryotherapy: Freezing Away Cancer

Cryotherapy is a minimally invasive procedure that uses extreme cold—typically liquid nitrogen—to destroy abnormal or cancerous skin cells. During the treatment, a dermatologist applies liquid nitrogen directly to the lesion, causing the targeted tissue to freeze rapidly. As the frozen cells thaw, they are damaged and eventually die off, allowing healthy new skin to regenerate in their place. Cryotherapy is most effective for superficial, non-melanoma skin cancers such as actinic keratosis and some early-stage basal cell carcinomas. The procedure is quick, often performed in minutes, and requires no incisions or stitches. Patients may feel a brief stinging sensation during application, followed by redness, blistering, or crusting as the treated area heals over several weeks. Compared to surgical excision, cryotherapy offers the advantages of minimal downtime and scarring, but it is less precise and not suitable for deeper or more aggressive cancers. Recurrence rates can be higher for certain tumor types that extend beneath the surface. For comprehensive details on cryotherapy and how it compares to other removal techniques, visit the Skin Cancer Foundation: Cryosurgery and the American Academy of Dermatology.
12. Laser Therapy for Skin Lesions

Laser therapy is an advanced treatment option for certain superficial skin cancers and precancerous lesions, such as actinic keratosis and some early-stage basal cell carcinomas. This method uses highly focused beams of light to selectively target and destroy abnormal skin cells while sparing surrounding healthy tissue. Different types of lasers, such as pulsed dye lasers and carbon dioxide (CO2) lasers, are chosen based on the lesion’s depth and location. The technology allows for precision and minimal invasiveness, making it ideal for treating areas where cosmetic outcomes are important, such as the face and neck. During the procedure, patients typically experience a sensation similar to a rubber band snap or mild heat, and local anesthesia may be used to minimize discomfort. Recovery is generally quick, with redness or mild swelling lasting a few days to a week, and scarring is usually minimal. While laser therapy is not suitable for deeper or more aggressive cancers, it is an effective and convenient option for select cases. For more information about laser treatments and patient experiences, visit the Skin Cancer Foundation: Laser Surgery and the American Academy of Dermatology: Laser Skin Resurfacing.
13. Topical Chemotherapy Creams

Topical chemotherapy creams, such as 5-fluorouracil (5-FU) and imiquimod, are non-invasive treatments used for specific superficial skin cancers and precancerous lesions like actinic keratosis and some superficial basal cell carcinomas. These medications are applied directly to the affected area, allowing the active ingredient to penetrate and destroy abnormal cells while minimizing systemic side effects. Patients generally apply the cream once or twice daily for several weeks, as directed by their dermatologist. During treatment, the targeted area may become red, inflamed, and crusty—signs that the medication is working to eliminate cancerous or precancerous cells. It’s important for patients to follow their doctor’s instructions closely and not discontinue use prematurely, even if the skin becomes uncomfortable. Topical chemotherapy is not effective for deeper or nodular cancers and is reserved for select cases where surgery might not be practical or desirable. After treatment, follow-up visits are essential to ensure the lesion has resolved completely. For more information on topical chemotherapy for skin cancer and patient guidance, visit the American Cancer Society: Topical Therapy for Skin Cancer and the Skin Cancer Foundation: Topical Medications.
14. Radiation Therapy Options
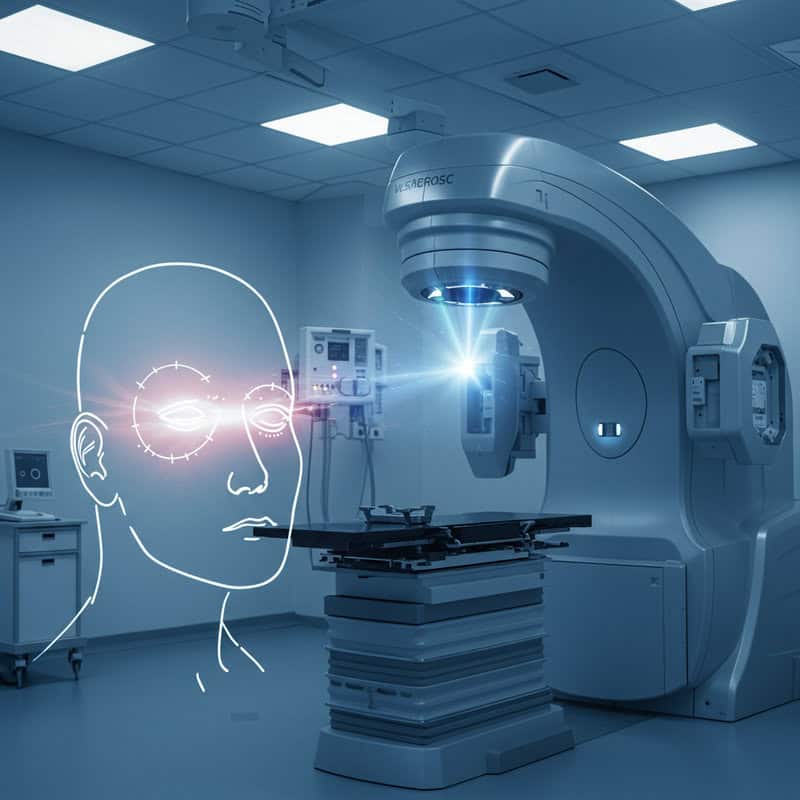
Radiation therapy is a non-surgical option for treating certain skin cancers, particularly when surgery is not feasible due to the patient’s health, tumor size, or location. It is commonly used for older adults, tumors in delicate areas (like the eyelids, ears, or nose), or cancers that have recurred after previous treatments. This therapy uses targeted high-energy rays to kill cancer cells by damaging their DNA, preventing them from growing and dividing. Treatment is typically delivered in short, daily sessions over several weeks. While effective for basal cell and squamous cell carcinomas, radiation is rarely used for melanoma due to its resistance.
Side effects can include redness, irritation, or blistering in the treated area—similar to a sunburn. Over time, skin may become dry, discolored, or scarred, and there’s a small risk of developing secondary cancers in the treated region years later. Despite these risks, radiation therapy can be highly effective, especially for tumors in challenging locations. It’s important for patients to discuss all options and potential side effects with their healthcare team. For more detailed information on radiation therapy for skin cancer, visit the American Cancer Society: Radiation Therapy for Skin Cancer and Skin Cancer Foundation: Radiation Therapy.
15. Immunotherapy for Advanced Cases

Immunotherapy is a groundbreaking treatment for advanced or metastatic skin cancers, particularly melanoma and, in some cases, advanced squamous cell carcinoma. This approach works by stimulating the patient’s own immune system to recognize and destroy cancer cells more effectively. Immunotherapy drugs, such as checkpoint inhibitors, block proteins that prevent immune cells from attacking cancer. Common examples include pembrolizumab (Keytruda), nivolumab (Opdivo), and cemiplimab (Libtayo). These medications are administered intravenously, typically every few weeks, and are reserved for patients whose cancer has spread beyond the skin or has not responded to traditional therapies.
Immunotherapy can lead to remarkable long-term remissions, but it is not without risks. Side effects may include fatigue, skin rashes, diarrhea, and inflammation of organs such as the lungs or liver, as the activated immune system may attack healthy tissues. Despite these challenges, immunotherapy has transformed the outlook for many patients with advanced skin cancer. For more details on immunotherapy and current research, visit the American Cancer Society: Immunotherapy for Skin Cancer and National Cancer Institute: Immunotherapy.
16. Understanding Risk Factors

Identifying your risk factors for skin cancer is essential for prevention and early detection. The most significant risk factor is excessive exposure to ultraviolet (UV) radiation, whether from the sun or tanning beds. People with fair skin, light hair, and blue or green eyes are at greater risk because they have less melanin, which provides some natural protection against UV damage. A personal or family history of skin cancer further increases risk, as certain genetic mutations can be inherited. Other important risk factors include having many moles or atypical (dysplastic) nevi, a weakened immune system (such as from organ transplant or certain medications), a history of severe sunburns, and older age. Additionally, individuals who work outdoors or live in sunny climates have an elevated risk.
Understanding these factors is crucial because it helps people take proactive steps to protect themselves, including regular skin checks and consultations with a dermatologist. For those at higher risk, more frequent screenings and extra sun protection measures are recommended. For a comprehensive list and explanation of skin cancer risk factors, visit the American Cancer Society: Skin Cancer Risk Factors and the Centers for Disease Control and Prevention.
17. The Genetics of Skin Cancer
Genetics play a significant role in the risk and development of skin cancer. Certain hereditary syndromes, such as familial atypical multiple mole melanoma (FAMMM) syndrome and basal cell nevus syndrome (also known as Gorlin syndrome), greatly increase the likelihood of developing skin cancer at a younger age or in multiple locations. These inherited conditions are linked to specific gene mutations that affect the skin’s ability to repair DNA damage caused by ultraviolet (UV) radiation. Even without a defined syndrome, a family history of melanoma or non-melanoma skin cancer suggests a genetic predisposition, meaning family members share genetic variants that make them more susceptible to cancer when exposed to environmental triggers.
Understanding genetic risk is crucial for families, as it may warrant earlier and more frequent skin cancer screenings, as well as genetic counseling. Relatives of affected individuals should be vigilant about practicing sun safety and performing regular self-exams. Genetic testing may be considered in certain high-risk families to help guide prevention strategies. For more information on hereditary skin cancer syndromes and genetic risk, visit the National Cancer Institute: Genetic Testing Facts and National Human Genome Research Institute: Skin Cancer Genetics.
18. Sun Protection Habits

Adopting effective sun protection habits is one of the most critical steps in reducing the risk of skin cancer. Daily use of a broad-spectrum sunscreen with an SPF of 30 or higher is recommended by dermatologists and public health organizations. Sunscreen should be applied generously to all exposed skin, including often-missed areas like the ears, neck, and tops of the feet, and reapplied every two hours or after swimming or sweating. In addition to sunscreen, wearing protective clothing—such as long-sleeved shirts, wide-brimmed hats, and UV-blocking sunglasses—provides an extra layer of defense against harmful ultraviolet (UV) rays.
Seeking shade, especially during peak sunlight hours (10 a.m. to 4 p.m.), further reduces UV exposure. Children and individuals with fair skin are particularly vulnerable and should take extra precautions. These habits are not just for sunny days; UV rays can penetrate clouds and reflect off surfaces like water, sand, and snow. Establishing sun-safe routines lowers the cumulative UV damage that leads to premature aging and skin cancer. For comprehensive advice on sun protection, visit the Centers for Disease Control and Prevention: Sun Safety and the American Academy of Dermatology: Sun Protection.
19. Choosing the Right Sunscreen

Selecting the right sunscreen is vital for effective sun protection and skin cancer prevention. The sun protection factor (SPF) rating indicates how well a sunscreen protects against UVB rays, the main cause of sunburn and a contributor to skin cancer. Dermatologists recommend using a sunscreen with at least SPF 30, which blocks about 97% of UVB rays. Higher SPFs provide slightly more protection, but no sunscreen blocks 100% of UV rays. It is also essential to choose a broad-spectrum sunscreen, which protects against both UVA and UVB rays—UVA rays penetrate deeper into the skin and contribute to aging and cancer risk.
For best results, apply sunscreen generously to all exposed skin 15 minutes before going outdoors. Use about one ounce (a shot-glass full) for a full-body application, and don’t forget ears, lips, and the back of the neck. Reapply every two hours, or more frequently if swimming or sweating. Water-resistant formulas are ideal for outdoor activities, but still require regular reapplication. For more guidance on choosing and using sunscreen effectively, visit the American Academy of Dermatology: Sunscreen FAQs and the FDA: Sunscreen Tips.
20. Avoiding Tanning Beds

Using tanning beds significantly increases the risk of developing skin cancer, including melanoma, the deadliest form. Artificial tanning emits concentrated ultraviolet (UV) radiation, often at levels much higher than natural sunlight, causing DNA damage to skin cells and accelerating the aging process. According to the Centers for Disease Control and Prevention, people who use tanning beds before age 35 increase their melanoma risk by 59%. Numerous case studies, such as those published by the National Institutes of Health, have documented young adults developing aggressive skin cancers linked to indoor tanning.
Beyond cancer, tanning beds can cause premature wrinkles, eye damage, and immune suppression. Many countries and states have imposed age restrictions or outright bans on indoor tanning for minors due to these dangers. Safer alternatives exist, such as sunless tanning lotions, sprays, or creams, which provide a bronzed appearance without UV exposure. These products are widely available and do not carry the same health risks. For more information about the dangers of tanning beds and healthy alternatives, visit the Skin Cancer Foundation: Tanning Risks and the FDA: Indoor Tanning Risks.
21. Safe Outdoor Activities

Enjoying outdoor activities like sports, gardening, and recreation is important for physical and mental health, but it’s essential to minimize UV exposure to reduce skin cancer risk. Plan activities for early morning or late afternoon when the sun’s rays are less intense, typically before 10 a.m. or after 4 p.m. Wear lightweight, long-sleeved clothing, wide-brimmed hats, and UV-blocking sunglasses for protection. Use a broad-spectrum sunscreen with at least SPF 30 on all exposed skin, and remember to reapply every two hours, or more often if swimming or sweating.
Seek shade whenever possible, especially during peak UV hours, and take regular breaks under trees, umbrellas, or canopies. When gardening, wear gloves and consider using a sun-protective face shield. For sports, look for gear designed with built-in UPF (ultraviolet protection factor) fabrics. Encourage children to play in shaded areas and instill sun-safe habits from a young age. Even on cloudy days or in cooler weather, UV rays can still cause damage. For more tips on safely enjoying time outdoors while protecting your skin, visit the CDC: Skin Cancer Prevention and the American Academy of Dermatology: Outdoor Safety.
22. Monitoring for Recurrence

Vigilant monitoring after skin cancer removal is crucial because there is always a risk of recurrence or the development of new cancers, particularly in individuals with a previous history. Regular self-examinations and follow-up visits with a dermatologist enable early detection of any suspicious changes. The skin should be checked monthly for new growths, changes in existing moles, or the reappearance of lesions near the original treatment site. Pay close attention to areas previously affected, as well as the rest of your body, since skin cancer can develop anywhere.
Warning signs include the return of a sore that doesn’t heal, new or changing moles, or persistent redness and swelling. Documenting your skin’s appearance with photographs can help track subtle shifts over time. Your dermatologist may recommend a tailored follow-up schedule based on your cancer type and risk factors, often involving more frequent exams during the first few years after treatment. Early intervention is vital for successful outcomes if recurrence is detected. For more information about post-removal vigilance and what to watch for, visit the American Cancer Society: Follow-up Care for Skin Cancer and the Skin Cancer Foundation: Follow-Up Care.
23. Scar Care After Removal

Proper scar care after skin cancer removal is key to promoting optimal healing and minimizing visible scarring. Immediately following surgery or treatment, it’s important to keep the wound clean and follow your healthcare provider’s instructions for dressing changes and cleaning. Moisturizing the area with petroleum jelly or silicone gel sheets can help keep the skin hydrated and reduce scar formation. Avoid picking at scabs or crusts, as this can increase the risk of infection and worsen scarring. Protecting the healing skin from sun exposure is critical—UV rays can darken scars and make them more noticeable, so cover the area or apply sunscreen once the wound has closed.
If redness, swelling, increased pain, discharge, or fever develops, seek medical advice promptly, as these could be signs of infection or other complications. Over time, most scars will fade, but persistent thickening, itching, or keloid formation may warrant evaluation by a dermatologist. Some patients benefit from treatments like laser therapy or steroid injections for problematic scars. For more details on wound and scar care after skin cancer removal, visit the American Academy of Dermatology: Post-Surgery Care and Skin Cancer Foundation: Scar Care Tips.
24. Psychological Impact and Support

Receiving a skin cancer diagnosis and undergoing treatment can have significant psychological and emotional effects. Patients may experience anxiety, depression, fear of recurrence, and concerns about physical appearance or scarring. These feelings are common, especially if the cancer was detected at an advanced stage or involved visible areas such as the face or hands. The stress of medical appointments, procedures, and the uncertainty of outcomes can also impact a patient’s well-being and daily life.
Support from family, friends, and mental health professionals is crucial during this time. Many find comfort in joining support groups, where sharing experiences with others facing similar challenges helps reduce feelings of isolation. Online communities and organizations like the American Cancer Society: Emotional Aspects of Skin Cancer and the Cancer Support Community offer counseling, educational resources, and peer support. Some hospitals also provide psycho-oncology services specializing in the mental health needs of cancer patients. Seeking help is a sign of strength, and emotional recovery is just as important as physical healing. Talking openly about your feelings with loved ones and professionals can greatly aid the journey to recovery.
25. Pediatric Skin Cancer
Skin cancer is rare in children, but cases do occur, particularly among those with genetic predispositions, compromised immune systems, or a history of significant sunburns. The most common types in pediatric patients are melanoma and, less frequently, basal cell carcinoma. Unique warning signs in children may include rapidly growing, oddly shaped, or multi-colored moles, new lesions that bleed or do not heal, or changes in existing birthmarks. Pediatric melanoma, in particular, can look different from adult cases—it may be pink, red, or flesh-colored rather than dark brown or black.
Prevention strategies should start early and include regular use of broad-spectrum sunscreen, protective clothing, and hats for outdoor activities. Children should be taught to seek shade, especially during peak sun hours, and to avoid tanning beds entirely. Parents should perform routine skin checks on their children and consult a dermatologist if any suspicious spots or changes are noticed. Early detection is vital, as pediatric skin cancers can be aggressive. For more information on skin cancer in children and how to protect young skin, visit the Skin Cancer Foundation: Children’s Skin Cancer and the American Cancer Society: Childhood Skin Cancer.
26. Skin Cancer in Older Adults

Older adults face a significantly increased risk of developing skin cancer due to cumulative sun exposure over their lifetimes and age-related changes in skin resilience and immune function. Basal cell carcinoma and squamous cell carcinoma are particularly common in seniors, while melanoma rates also rise with age. Age-related risks are compounded by factors such as a history of sunburns, weakened immune systems, and thinning skin, which may be less able to repair DNA damage from ultraviolet (UV) radiation. In seniors, skin cancers may present as non-healing sores, rapidly growing bumps, or changes in existing lesions.
Treatment in older adults may differ from younger patients due to underlying health conditions, medications, or concerns about wound healing. Less invasive treatments, such as topical therapies or targeted radiation, may be preferred for those with limited mobility or comorbidities. Prevention remains essential—regular use of sunscreen, sun-protective clothing, and routine skin checks can reduce risk and promote early detection. Family members and caregivers play a vital role in monitoring for new or changing skin lesions. For more detailed guidance on skin cancer risk, treatment, and prevention in seniors, visit the American Cancer Society: Skin Cancer in Older Adults and the Skin Cancer Foundation: Age as a Risk Factor.
27. Occupational Hazards

Certain occupations place individuals at a higher risk for skin cancer due to prolonged sun exposure. Outdoor workers such as construction workers, farmers, landscapers, lifeguards, and postal workers are particularly vulnerable to the harmful effects of ultraviolet (UV) radiation. These jobs often require long hours in direct sunlight, increasing the cumulative damage to skin cells and the risk of developing basal cell carcinoma, squamous cell carcinoma, and melanoma.
To mitigate these risks, many organizations have implemented workplace protection policies. These may include providing broad-brimmed hats, UV-protective clothing, sunglasses, and easy access to sunscreen. Scheduling outdoor tasks outside peak UV hours and ensuring shaded rest areas can further reduce exposure. Employers are encouraged to educate workers on the importance of regular skin checks and sun safety practices. The National Institute for Occupational Safety and Health (NIOSH) and the Occupational Safety and Health Administration (OSHA) provide guidelines and resources for sun protection in the workplace. By prioritizing these measures, employers can help safeguard their workforce against occupational skin cancer and promote a culture of health and safety on the job site.
28. Skin of Color: Unique Challenges

Skin cancer can affect individuals of all racial and ethnic backgrounds, though detection and outcomes in people with skin of color often present unique challenges. While those with darker skin have more melanin, offering some natural protection against ultraviolet (UV) damage, they are not immune to skin cancer. In fact, skin cancers in people of color are frequently diagnosed at later stages, when they are more difficult to treat and have poorer outcomes. Melanoma, for example, is more likely to appear on less sun-exposed areas—such as the palms, soles, and under the nails—in these populations, contributing to delayed recognition.
Barriers to early detection include a lack of awareness, misconceptions about risk, and less frequent skin cancer screenings. Healthcare professionals and patients alike may overlook or misdiagnose suspicious lesions. Tailored advice includes performing regular self-exams, paying close attention to non-traditional sites, and seeking dermatologic care for any persistent, changing, or unusual spots regardless of location or skin tone. For more information on skin cancer in diverse populations and resources for detection and prevention, visit the American Academy of Dermatology: Skin Cancer in Skin of Color and the Skin Cancer Foundation: Skin of Color.
29. The ABCDEs of Melanoma

Early detection of melanoma is crucial, and the ABCDE rule provides a simple, effective way to identify suspicious moles or lesions. Each letter stands for a key warning sign:
A – Asymmetry: One half of the mole or spot is unlike the other half in shape, color, or texture.
B – Border: The edges are irregular, scalloped, or poorly defined, rather than smooth and even.
C – Color: The mole contains multiple shades of brown, tan, black, red, white, or blue, or the color is unevenly distributed.
D – Diameter: The spot is larger than 6 millimeters (about the size of a pencil eraser), although melanomas can sometimes be smaller.
E – Evolving: The mole is changing in size, shape, color, elevation, or another trait—or new symptoms such as bleeding or itching develop.
Regular self-examination using these criteria can help detect melanoma early, when it is most treatable. For detailed visuals and further guidance on the ABCDEs of melanoma, visit the American Cancer Society: Melanoma Detection and the Skin Cancer Foundation: Melanoma Warning Signs.
30. When to Seek a Second Opinion

Seeking a second medical opinion can be valuable at various stages of a skin cancer journey. Consider consulting another specialist if you have doubts about your diagnosis, if your cancer is rare or complex, or if you are presented with multiple treatment options that differ in risk, recovery, or cosmetic outcome. A second opinion may also be beneficial if your initial provider has limited experience with your specific cancer type, or if you simply want reassurance before starting a significant procedure or therapy.
Receiving input from another dermatologist, oncologist, or surgeon can help clarify your diagnosis, confirm the recommended treatment plan, or introduce additional options—sometimes leading to less invasive or more advanced therapies. This process often provides peace of mind, ensuring you make informed decisions about your care. Most doctors welcome a second opinion and may even recommend it for complicated cases. For tips on how and when to seek a second opinion, visit the American Cancer Society: Second Opinions and the American Society of Clinical Oncology: How to Get a Second Opinion. Empowering yourself with knowledge leads to greater confidence in your treatment choices.
31. Advances in Skin Cancer Detection

Recent advances in skin cancer detection are revolutionizing early diagnosis and improving patient outcomes. Technologies such as artificial intelligence (AI) and dermoscopy are now widely used to enhance the accuracy of skin cancer screening. AI-powered tools analyze high-resolution images of skin lesions, comparing them to vast databases to identify suspicious characteristics often missed by the human eye. This technology assists dermatologists in distinguishing benign from malignant growths and can streamline the decision for further biopsy or monitoring.
Dermoscopy, a non-invasive imaging technique, uses a handheld device to magnify and illuminate skin lesions, allowing for better visualization of subsurface features. This increases diagnostic accuracy, particularly for melanoma and atypical moles. In addition, teledermatology enables patients to send images of their skin to specialists for rapid evaluation, expanding access to expert care, especially in underserved regions. These advances help detect cancers at earlier stages, when treatment is most effective and less invasive. For more information on new detection technologies and their impact on skin cancer diagnosis, visit the National Cancer Institute: AI and Skin Cancer Detection and the Skin Cancer Foundation: New Technologies.
32. Teledermatology Options

Teledermatology is transforming access to skin cancer screening and dermatological care, particularly for people in rural or underserved areas. This innovative approach allows patients to consult with dermatologists remotely, using secure platforms to send high-quality photos or videos of suspicious moles, lesions, or skin changes. These photo consultations can provide rapid expert evaluation, helping to determine whether an in-person visit or biopsy is needed. Teledermatology reduces wait times for appointments and makes it easier for individuals to receive timely advice without the barriers of travel or limited local specialists.
Many healthcare systems and private practices now offer teledermatology services, often integrated with electronic health records for seamless follow-up. Some telehealth platforms even use artificial intelligence to assist in the initial review of submitted images, further improving triage and accuracy. However, while teledermatology is highly effective for initial assessment and monitoring, in-person visits remain crucial for procedures like biopsies or treatments. For more information on teledermatology, how to prepare for a remote skin check, and its benefits for improving skin cancer outcomes, visit the American Academy of Dermatology: Teledermatology and the National Cancer Institute: Teledermatology and Skin Cancer.
33. Sun Safety for Children

Instilling sun protection habits early in life is vital for reducing the lifetime risk of skin cancer. Children’s skin is more sensitive to ultraviolet (UV) radiation, and just a few severe sunburns during childhood can greatly increase their risk of developing skin cancer later. Parents and caregivers should teach children to apply broad-spectrum sunscreen with at least SPF 30 before going outdoors, reapplying every two hours, and after swimming or sweating. Wearing wide-brimmed hats, UV-protective sunglasses, and long-sleeved shirts further shields young skin from harmful rays. Seeking shade during peak sunlight hours (10 a.m. to 4 p.m.) and encouraging play in covered or shaded areas are also key strategies.
Schools play an important role in sun safety education and implementation. Many schools now allow students to bring and apply sunscreen, wear hats, and access shaded areas during recess or outdoor events. Educational programs and skin cancer awareness campaigns can reinforce sun-safe behaviors and empower children to protect themselves. Collaboration between parents, teachers, and community organizations ensures a consistent message and safer environments for children. For more information on teaching sun safety to children and school-based prevention efforts, visit the CDC: Sun Safety for Children and the Skin Cancer Foundation: Children and Sun Safety.
34. Diet and Skin Health

Nutrition plays an important role in maintaining healthy skin and supporting the body’s defenses against skin cancer. Diets rich in antioxidants—such as vitamins C and E, beta-carotene, and selenium—help protect skin cells from oxidative damage caused by ultraviolet (UV) radiation. Foods like leafy greens, berries, citrus fruits, carrots, nuts, and seeds are excellent sources of these protective compounds. Omega-3 fatty acids, found in fatty fish like salmon, walnuts, and flaxseeds, may also reduce inflammation and support skin repair.
Staying well-hydrated by drinking plenty of water helps maintain skin elasticity and function, aiding in recovery from sun exposure or minor injuries. While no single food can prevent skin cancer, a balanced diet that emphasizes whole, unprocessed foods supports the immune system and overall skin health. Some research suggests that limiting processed meats, excessive sugar, and alcohol may further enhance skin resilience. For more information on the link between diet and skin cancer prevention, including recommended foods and recipes, visit the American Cancer Society: Eat Healthy and the Skin Cancer Foundation: Nutrition and Skin Health. A healthy diet, combined with sun protection, forms a comprehensive approach to skin cancer prevention.
35. Vitamin D Versus Sun Safety

The body relies on sunlight to produce vitamin D, a nutrient essential for bone health, immune function, and overall well-being. However, unprotected sun exposure increases the risk of skin cancer, leading to a common dilemma: how to balance vitamin D needs with effective sun safety. Dermatologists and health organizations agree that it is possible—and preferable—to maintain adequate vitamin D levels without excessive UV exposure. Short periods of incidental sun exposure, such as walking outside with arms exposed for a few minutes, can help, but deliberate tanning or skipping sunscreen is not recommended.
Vitamin D can also be obtained safely through dietary sources like fortified milk, cereals, fatty fish, and egg yolks, as well as with supplements if needed. Blood tests can determine if you have a deficiency, allowing for personalized advice from a healthcare provider. The American Cancer Society and the Centers for Disease Control and Prevention recommend prioritizing sun protection and consulting your doctor about vitamin D supplementation if you are at risk for low levels. This approach allows you to benefit from vitamin D while minimizing skin cancer risk.
36. Medication-Related Risks

Certain medications can increase your skin’s sensitivity to sunlight, a condition known as photosensitivity, which raises the risk of sunburn and, over time, skin cancer. Common drugs that may cause this reaction include some antibiotics (such as tetracyclines and fluoroquinolones), diuretics, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, antifungal medications, retinoids (for acne), and some antihistamines. Additionally, medications for high blood pressure, heart conditions, and certain chemotherapy drugs can make the skin more vulnerable to UV damage.
If you are taking any of these medications, it’s important to adjust your sun protection routines. Avoid direct sun exposure during peak hours, wear broad-brimmed hats and UV-protective clothing, and consistently apply broad-spectrum sunscreen with an SPF of 30 or higher. Inform your healthcare provider or pharmacist of any unusual sun reactions, such as severe burns, rashes, or blistering. Always check medication labels for sun sensitivity warnings and ask your doctor if you need extra precautions. For a comprehensive list of photosensitizing medications and safety tips, visit the American Academy of Dermatology: Photosensitivity and the U.S. FDA: Medication and Sun Sensitivity.
37. Immune System and Cancer Risk
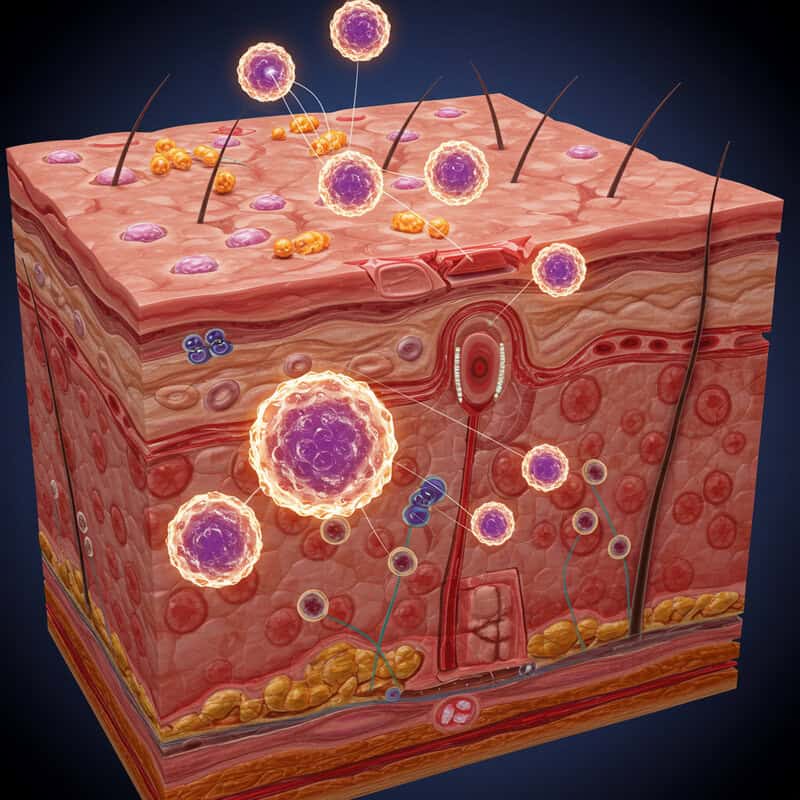
A healthy immune system plays a critical role in identifying and eliminating abnormal cells, including those that can develop into cancer. When immunity is weakened—due to conditions like HIV/AIDS, organ transplantation, certain cancers, or immunosuppressive medications—the body’s ability to fight off early cancerous changes is reduced. People with suppressed immunity are at significantly increased risk for developing skin cancers, particularly squamous cell carcinoma, which can behave more aggressively in these populations. Transplant recipients, for example, have a markedly higher incidence of skin cancer compared to the general public.
Prevention strategies for immunocompromised individuals include rigorous sun protection, frequent skin self-exams, and more regular dermatological screenings. These patients should avoid tanning beds, take extra care with medications that may further increase sun sensitivity, and promptly report any new or changing skin lesions to their healthcare provider. Consulting a dermatologist familiar with the unique risks of immunosuppressed patients is recommended. For more on how immunity impacts skin cancer risk and prevention, visit the American Cancer Society: Skin Cancer Risk Factors and the Skin Cancer Foundation: Immunosuppression and Skin Cancer.
38. Skin Cancer Myths Debunked

There are many persistent myths about skin cancer that can lead to unnecessary risks or delays in detection and treatment. One common misconception is that people with darker skin do not get skin cancer; in reality, while the risk is lower, those with skin of color can and do develop skin cancer, often at more advanced stages due to delayed recognition. Another myth is that tanning—whether outdoors or in a tanning bed—is safe or even healthy. The truth is, any tan is a sign of skin damage, and artificial tanning significantly increases the risk of all types of skin cancer.
Some believe that skin cancer only appears on sun-exposed parts of the body, but it can develop anywhere, including under fingernails, on the soles of the feet, or inside the mouth. Others think that only older adults are at risk; however, skin cancer can affect people of all ages—including children and young adults. Early detection remains crucial, regardless of age or skin type. For more information and to explore more skin cancer myths and facts, visit the American Cancer Society: Skin Cancer Myths and Facts and the Skin Cancer Foundation: Myths Debunked.
39. The Role of Annual Physicals

Incorporating skin examinations into your annual physical is a key strategy for early detection and prevention of skin cancer. During yearly health exams, primary care providers can assess your skin for suspicious moles, lesions, or changes that you may have overlooked. These checks are especially important for individuals with risk factors such as fair skin, a history of sunburns, multiple moles, or a family history of skin cancer. Bringing up any new or changing spots during your appointment ensures that potential problems are addressed promptly.
Annual physicals offer an opportunity to discuss sun safety, review self-exam techniques, and determine if a referral to a dermatologist is necessary for more in-depth evaluation. For those with a personal or family history of skin cancer, your healthcare provider may recommend more frequent screenings. Making skin checks a routine part of your health care helps catch cancers early, when they are most treatable and outcomes are best. For more information on the importance of annual exams and integrating skin health into routine care, visit the American Cancer Society: Skin Cancer Detection and the American Academy of Dermatology: How to Spot Skin Cancer.
40. Travel and Sun Exposure

Traveling, especially to sunny or tropical destinations, can increase your risk of sunburn and skin damage due to higher ultraviolet (UV) exposure. High-altitude regions, areas closer to the equator, and reflective environments like beaches or snowy mountains amplify UV intensity. Before you travel, research the UV index of your destination and pack accordingly. Bring a broad-spectrum sunscreen with at least SPF 30, and remember that travel-size containers may need to be replenished for longer trips. Wide-brimmed hats, UV-blocking sunglasses, and lightweight, long-sleeved clothing are essential for protection during sightseeing, outdoor activities, or water sports.
Plan outdoor excursions for early morning or late afternoon to avoid peak sun hours (10 a.m. to 4 p.m.), and seek shade whenever possible. Remember to reapply sunscreen every two hours and after swimming or sweating. Be vigilant even on overcast days, as UV rays can penetrate clouds. Travelers with increased skin cancer risk should schedule a skin check before and after extended trips. For more tips on staying sun-safe while traveling, visit the CDC: Skin Cancer Prevention During Travel and the Skin Cancer Foundation: Traveler’s Guide to Sun Safety.
41. Tattoos and Skin Cancer Detection

Tattoos can complicate the early detection of skin cancer by masking changes in moles or new lesions. The pigments and colors used in tattoos may obscure variations in size, shape, or color of underlying skin, making it challenging to spot suspicious growths or evolving moles. Melanoma and other skin cancers can develop within or beneath tattooed skin, sometimes resulting in delayed diagnosis and more advanced disease at the time of discovery. Areas with large, dense, or dark tattoos are especially difficult to monitor.
If you have tattoos, it’s important to pay close attention to the skin beneath and around the ink. Look for new lumps, persistent redness, changes in texture, or any lesions that bleed, itch, or fail to heal. Periodically photographing your tattoos can help you recognize subtle changes over time. Inform your dermatologist about all tattooed areas during routine skin checks so they can examine these spots thoroughly. If you notice any unusual skin changes within your tattoos, seek professional evaluation promptly. For more information on tattoos and skin cancer detection, visit the Skin Cancer Foundation: Tattoos and Skin Cancer and the American Academy of Dermatology: Tattoos and Skin Cancer.
42. Allergies and Sunscreens

Some individuals experience allergic reactions to sunscreens, which can manifest as redness, itching, swelling, or a rash where the product was applied. These reactions are often due to certain chemical ingredients such as oxybenzone, fragrances, preservatives, or parabens. Allergic contact dermatitis or photoallergic reactions may occur, particularly in people with sensitive skin or a history of allergies. If you suspect a sunscreen allergy, discontinue use immediately and consult a dermatologist for evaluation and patch testing if necessary.
Hypoallergenic sunscreen options are available, typically formulated with physical (mineral) blockers like zinc oxide or titanium dioxide, which are less likely to cause irritation. Look for products labeled “fragrance-free,” “paraben-free,” or “sensitive skin.” Perform a patch test by applying a small amount to a discreet area and waiting 24 hours to check for a reaction before using it more widely. For those with severe sensitivities, clothing and hats with built-in ultraviolet protection factor (UPF) can provide additional sun safety. For more guidance on sunscreen allergies, ingredient lists, and finding hypoallergenic products, visit the American Academy of Dermatology: Sunscreen Allergy and the Skin Cancer Foundation: Allergic Reactions to Sunscreen.
43. Skin Cancer and Climate Change

Climate change is contributing to rising skin cancer rates through its impact on the earth’s atmosphere, particularly via ozone layer depletion. The ozone layer acts as a natural shield, absorbing the majority of the sun’s harmful ultraviolet (UV) radiation. As human activities have released chlorofluorocarbons (CFCs) and other pollutants, the ozone layer has thinned, allowing more UVB rays to reach the earth’s surface. Increased UV exposure elevates the risk of DNA damage in skin cells, leading to a higher incidence of all types of skin cancer, especially in regions with significant ozone depletion.
Additionally, climate change brings about longer and hotter summers, more outdoor activities, and shifts in UV patterns, all of which may further increase cumulative sun exposure. Public health experts are concerned that these environmental changes will continue to drive up skin cancer rates if sun protection measures are not widely adopted. For more information on the relationship between climate change, ozone depletion, and skin cancer trends, visit the U.S. Environmental Protection Agency: Ozone Layer Depletion Health Effects and the American Cancer Society: Climate Change and Cancer Risk.
44. Community Awareness Campaigns

Community awareness campaigns play a crucial role in educating the public about skin cancer prevention and early detection. Successful campaigns like Australia’s “Slip! Slop! Slap!” and the United States’ “Choose Your Cover” have significantly raised awareness about sun safety and the importance of protective behaviors. These initiatives use memorable slogans, school programs, mass media, and partnerships with local organizations to promote practices such as using sunscreen, wearing hats, seeking shade, and scheduling regular skin checks.
Research shows that such campaigns can lead to measurable behavior change, including increased sunscreen use, reduced tanning bed usage, and more frequent skin self-examinations. They also address misconceptions and barriers by targeting high-risk groups, such as outdoor workers, children, and teens. The impact of these campaigns is reflected in reduced skin cancer rates in targeted populations and improved public knowledge about prevention. For examples of effective community outreach and resources for launching local efforts, visit the CDC: Community Skin Cancer Prevention and the American Cancer Society: Skin Cancer Prevention Campaigns. Grassroots education remains a vital tool in the fight against skin cancer worldwide.
45. Mobile Apps for Skin Monitoring

Mobile apps for skin monitoring have become powerful tools in the early detection and prevention of skin cancer. These applications enable users to photograph, track, and compare moles and skin lesions over time, making it easier to notice subtle changes that may indicate a problem. Some popular apps—such as MoleMapper, Miiskin, and SkinVision—offer features like reminders for self-exams, secure photo storage, and risk assessments using artificial intelligence algorithms.
Many of these apps provide educational resources to help users apply the ABCDE rule for melanoma, and some allow users to share images directly with dermatologists for remote consultations. While these tools are not a replacement for professional medical advice, they can prompt timely visits to a healthcare provider if changes are detected. Choosing an app with strong privacy protections and clear medical disclaimers is important. For more information about mobile health technology and its role in skin cancer detection, visit the American Cancer Society: Skin Self-Exam Apps and the American Academy of Dermatology: Mobile Apps for Skin Monitoring.
46. Insurance and Cost Considerations

Understanding insurance coverage and managing costs are important aspects of skin cancer screening, diagnosis, and treatment. Most health insurance plans, including Medicare, typically cover medically necessary skin cancer screenings, biopsies, and removal procedures, especially when performed due to clinical suspicion of cancer. Coverage may vary for routine, preventive skin checks or cosmetic procedures related to scar revision. It is important to verify specific benefits and any out-of-pocket expenses with your insurance provider prior to scheduling appointments.
For those without insurance or facing high deductibles, financial assistance programs are available through hospitals, community clinics, and nonprofit organizations. Some dermatology practices offer sliding-scale fees or payment plans. Additionally, organizations such as the American Cancer Society and NeedyMeds provide support and resources for finding affordable care. Early detection and timely removal of skin cancer can reduce long-term costs associated with more advanced treatments. If you are concerned about finances, talk openly with your healthcare team or clinic social worker about options for assistance. For more details on insurance and financial support for skin cancer care, visit the American Cancer Society: If You Have Skin Cancer.
47. Cosmetic Concerns After Removal

Appearance-related concerns are common after skin cancer removal, especially when surgery affects visible areas like the face, neck, or hands. Scarring, changes in skin texture, loss of pigment, or asymmetry can impact self-esteem and social confidence. Many patients worry about how their skin will look after healing and whether others will notice the changes. Fortunately, advances in reconstructive and cosmetic dermatology offer a range of solutions. Options include meticulous surgical closure techniques, skin grafts, local flaps, and later procedures such as laser therapy, dermal fillers, or microneedling to improve the appearance of scars.
Consulting with a dermatologist or plastic surgeon experienced in reconstructive procedures can help tailor a plan that addresses both functional and cosmetic needs. Camouflage makeup and specialized skincare products can also minimize visible changes and restore confidence during healing. Support groups and counseling may help individuals adjust emotionally and embrace their appearance. For more information on managing cosmetic outcomes after skin cancer treatment, visit the Skin Cancer Foundation: Appearance Concerns and the American Academy of Dermatology: Reconstruction After Skin Cancer. Addressing cosmetic worries is an important part of holistic recovery and self-acceptance.
48. Research and Future Treatments

Innovative research in skin cancer continues to drive the development of new therapies and bring hope for more effective prevention and lasting cures. Emerging treatments include targeted therapies that attack specific genetic mutations in melanoma and other cancers, as well as next-generation immunotherapies designed to enhance the body’s immune response with fewer side effects. Scientists are also investigating vaccine-based strategies to prevent skin cancer recurrence and novel topical medications that could treat pre-cancerous lesions without invasive procedures.
Ongoing clinical trials worldwide are testing these breakthroughs, with the goal of improving outcomes for patients at all stages of skin cancer. Advances in non-invasive imaging, artificial intelligence, and personalized medicine promise to refine diagnosis and tailor treatments to each individual’s genetic and molecular profile. Preventive research is also focused on developing more effective sunscreens and public health interventions to reduce UV exposure. For the latest updates on clinical trials and cutting-edge therapies, visit the ClinicalTrials.gov: Skin Cancer Trials and the National Cancer Institute: Skin Cancer Research. These advances inspire optimism for a future where skin cancer is more easily prevented, detected, and treated.
49. Resources and Support Organizations

Accessing accurate information and supportive resources is essential for anyone affected by skin cancer. Several reputable organizations provide educational materials, hotlines, and community support for patients, families, and caregivers. The Skin Cancer Foundation offers comprehensive guides on prevention, detection, and treatment, as well as a searchable database of dermatologists. The American Cancer Society provides a 24/7 helpline at 1-800-227-2345, online chat services, and local support groups. The Cancer Support Community connects individuals with counseling, peer support, and educational workshops.
For those seeking information about clinical trials or financial assistance, ClinicalTrials.gov and NeedyMeds are valuable resources. The American Academy of Dermatology provides guidance on self-exams, sun safety, and finding board-certified specialists. These organizations also offer materials in multiple languages and for diverse communities. Reaching out for help—whether for answers to medical questions, emotional support, or practical guidance—can make a significant difference in navigating the challenges of skin cancer.
50. Lifelong Prevention Strategies

Reducing skin cancer risk is a lifelong commitment that involves consistent, proactive habits. Incorporate daily sun protection into your routine by applying broad-spectrum sunscreen with at least SPF 30, wearing wide-brimmed hats, UV-protective sunglasses, and long-sleeved clothing. Seek shade during peak sunlight hours (10 a.m. to 4 p.m.), and avoid tanning beds entirely. Perform monthly self-examinations to check for new or changing moles and lesions, using the ABCDE method for guidance. Keep a personal skin checklist or photo log to track changes over time, and schedule regular professional skin exams, especially if you have risk factors or a history of skin cancer.
Teach sun-safe habits to children and encourage your family, friends, and coworkers to prioritize skin health as well. Maintain a healthy diet, stay hydrated, and be vigilant about medication-related sun sensitivity. Stay informed about new research and advances in skin cancer prevention. For comprehensive prevention checklists and daily tips, visit the Skin Cancer Foundation: Prevention Strategies and the CDC: Skin Cancer Prevention. By making these practices a permanent part of your lifestyle, you can significantly lower your risk of developing skin cancer—now and in the future.
Conclusion

Early detection and lifelong prevention are essential in the fight against skin cancer. Recognizing warning signs, practicing daily sun protection, and committing to regular self-exams and professional screenings can dramatically improve outcomes and save lives. Whether you have a history of skin cancer or simply want to minimize your risk, proactive care is key. Schedule routine check-ups, stay informed about new advancements, and share sun-safe habits with loved ones. For further guidance and support, explore resources from the Skin Cancer Foundation and the American Cancer Society. Together, these steps empower you to take charge of your skin health for life.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





