Subtle Signs You May Need Hormone Therapy
Recent studies reveal that up to 47% of women and 39% of men in the United States, and nearly 41% of adults in the UK, experience symptoms of hormonal imbalance (NIH, 2023; British Menopause Society, 2023). The endocrine system governs vital processes, including metabolism and mood, yet subtle symptoms often lead to late detection and delayed treatment.
1. Persistent Fatigue

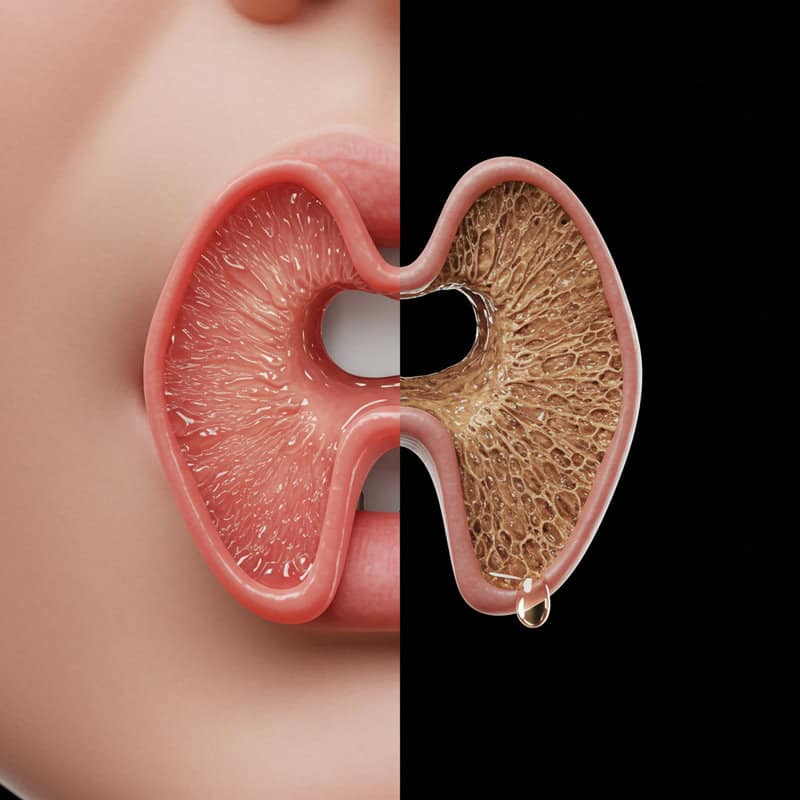
One of the most overlooked indicators of hormonal imbalance is persistent fatigue. Unlike normal tiredness that follows a busy day or insufficient sleep, this kind of exhaustion can be relentless and unrelieved by rest. Hormonal fluctuations, particularly involving the thyroid, adrenal glands, and reproductive hormones, can significantly disrupt energy production and regulation within the body. For example, undiagnosed hypothyroidism—a condition where the thyroid gland does not produce enough hormones—can leave individuals feeling chronically sluggish, mentally foggy, and unable to complete routine tasks.
It is crucial to differentiate between common fatigue and persistent exhaustion that could signal a deeper issue. While lifestyle factors such as stress and lack of sleep certainly play a role, fatigue that persists for several weeks or interferes with daily function warrants medical attention. According to the NHS, chronic fatigue should not be ignored, as it may be an early sign of hormonal dysfunction. Recognizing this subtle but impactful symptom can help individuals seek appropriate evaluation and, if necessary, hormone therapy to restore balance and vitality.
2. Unexplained Weight Changes

Hormones play a pivotal role in regulating body weight, with thyroid hormones and insulin being among the most influential. When these hormones are imbalanced, it can lead to unexplained weight gain or loss that is not attributable to changes in diet, exercise, or lifestyle. For instance, hypothyroidism (underactive thyroid) often causes weight gain due to a slowed metabolism, while insulin resistance or uncontrolled diabetes can result in weight loss as the body struggles to regulate glucose.
It is normal for body weight to fluctuate slightly from day to day due to factors like hydration, sodium intake, or menstrual cycles. However, gradual and unexplained weight changes—especially if they persist over several weeks or months—may indicate a hormonal imbalance rather than typical variation. The NHS recommends paying close attention to weight trends that cannot be explained by lifestyle factors. Monitoring your weight and being alert to subtle shifts can be crucial for early detection of underlying endocrine issues that may require professional evaluation and treatment.
3. Sleep Disturbances

Hormones such as melatonin and cortisol are fundamental in regulating your sleep-wake cycle. Melatonin, produced by the pineal gland, signals your body that it’s time to sleep, while cortisol, released by the adrenal glands, helps wake you up and manage daily stress. Disruptions in the balance of these hormones can lead to difficulty falling asleep, staying asleep, or waking up feeling unrefreshed. For example, elevated nighttime cortisol levels due to chronic stress or adrenal dysfunction can make it challenging to relax and fall asleep, according to the Sleep Foundation.
Another common example is night sweats and insomnia experienced during menopause, largely due to fluctuating estrogen and progesterone levels. These hormonal changes can cause sudden awakenings, leaving individuals feeling unrested. The NHS highlights that persistent sleep disturbances, especially when accompanied by other symptoms, may indicate the need for medical assessment. If you notice ongoing difficulty with sleep that lasts for several weeks or is accompanied by symptoms like night sweats, it’s important to track these issues and discuss them with a healthcare provider, as they may reflect underlying hormonal imbalances.
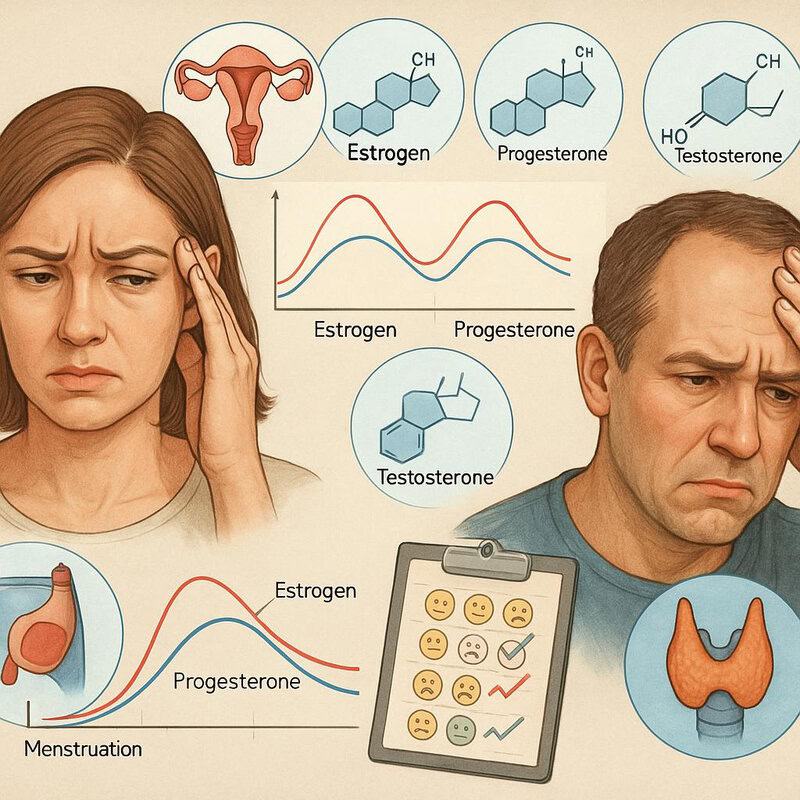
4. Mood Swings

Hormones such as estrogen, progesterone, and testosterone have a profound impact on emotional regulation and mental well-being. Fluctuations in these hormones can influence neurotransmitter activity in the brain, affecting mood and emotional responses. For instance, decreases in estrogen and progesterone during perimenopause or after childbirth are often linked to irritability, anxiety, and even depression, as discussed by the American Psychiatric Association. Similarly, low testosterone levels in men can contribute to increased feelings of sadness, lack of motivation, and irritability.
Everyone experiences natural emotional ups and downs due to stress, life events, or fatigue. However, hormonal mood swings tend to be more intense, frequent, and unpredictable, often occurring without any obvious external trigger. These emotional changes may significantly impact relationships, work performance, or overall quality of life. According to the NHS, if mood fluctuations are persistent, severe, or accompanied by other physical symptoms such as changes in sleep or appetite, consulting a healthcare professional is recommended. Early intervention can help identify underlying hormonal imbalances and provide appropriate support or therapy.
5. Low Libido
Sexual desire is primarily regulated by hormones such as testosterone, estrogen, and progesterone. These hormones play crucial roles in maintaining a healthy libido in both men and women. Testosterone, in particular, is strongly linked to sexual desire, and a decline in its levels—due to aging, stress, or underlying endocrine disorders—can lead to a noticeable reduction in interest in sexual activity. According to the Johns Hopkins Medicine, low testosterone is a common cause of diminished libido in men, while fluctuating levels of estrogen and progesterone can similarly affect women, especially during menopause or after childbirth.
It is normal for libido to fluctuate due to factors such as stress, fatigue, or relationship changes. However, a persistent and unexplained loss of interest in sex—especially when it lasts for several months or is accompanied by other symptoms like mood changes or fatigue—may point to a deeper hormonal imbalance. The NHS advises that ongoing low libido, particularly if it causes distress or impacts relationships, should be discussed with a healthcare provider to explore potential hormonal or medical causes and appropriate treatments.
6. Hair Loss or Thinning
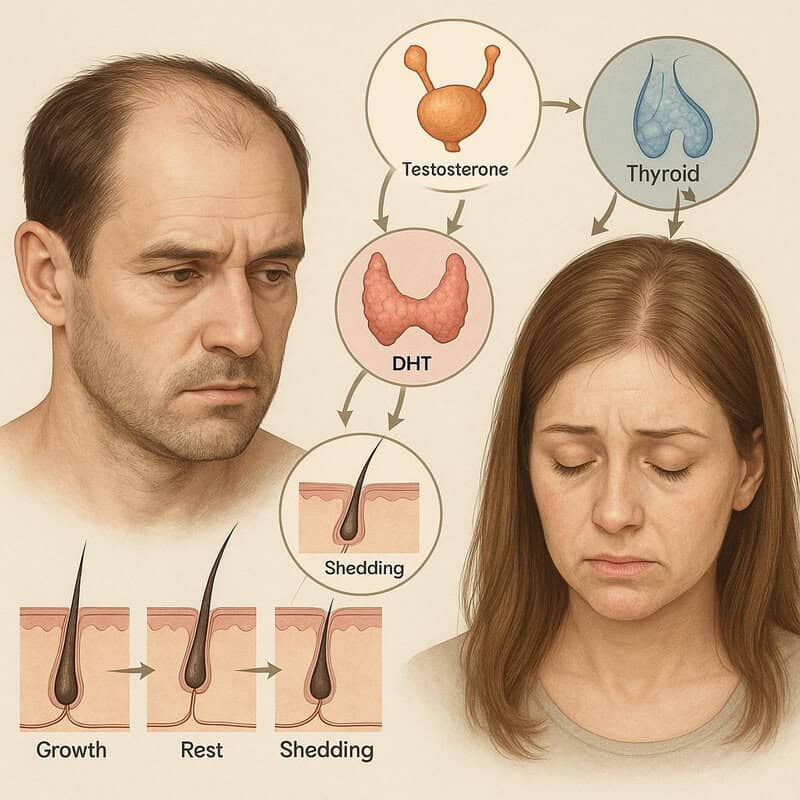
Hair growth is intricately controlled by hormones, particularly androgens such as testosterone and dihydrotestosterone (DHT), as well as thyroid hormones. These hormones influence the hair growth cycle, determining when hair enters growth, rest, and shedding phases. When hormonal imbalances occur—such as with thyroid disorders, polycystic ovary syndrome (PCOS), or menopause—they can disrupt this cycle and lead to hair loss or thinning. According to the American Academy of Dermatology, both men and women may experience diffuse thinning or patchy hair loss due to these imbalances.
Pattern hair loss, such as male-pattern baldness, is typically hereditary and progresses in a predictable manner. In contrast, hormonal hair loss is often more sudden, can be diffuse, and may be accompanied by other symptoms like changes in skin texture or menstrual irregularities. The NHS advises that if you notice rapid hair thinning, widening part lines, or significant shedding—especially when combined with other signs of hormonal changes—it’s important to seek medical advice. Timely evaluation can help identify underlying endocrine issues and guide appropriate treatment to prevent further hair loss.
7. Irregular Menstrual Cycles

The menstrual cycle is tightly regulated by the interplay between estrogen and progesterone, two key reproductive hormones. These hormones orchestrate the timing of ovulation and menstruation, helping to maintain regular monthly cycles. When their balance is disrupted, periods can become unpredictable, unusually heavy or light, or even absent for months at a time. One common cause of such disruptions is polycystic ovary syndrome (PCOS), a hormonal disorder that affects approximately 6% to 12% of women of reproductive age according to the CDC.
While occasional irregularities can be caused by factors like stress, travel, or significant weight changes, persistent or sudden alterations in menstrual cycles may be a sign of underlying hormonal imbalance. The NHS recommends tracking your cycle over several months to detect patterns or changes. If cycles become consistently irregular, excessively long or short, or are missed entirely without another explanation, it’s important to consult a healthcare professional. Early identification of hormonal issues can allow for more effective management, especially when related to conditions like PCOS, thyroid dysfunction, or perimenopause.
8. Hot Flashes or Night Sweats

Vasomotor symptoms such as hot flashes and night sweats are classic signs of hormonal changes, particularly involving estrogen. These symptoms occur when hormonal fluctuations affect the body’s ability to regulate temperature, resulting in sudden sensations of intense heat, sweating, and sometimes chills. The National Institute on Aging states that over 75% of women experience hot flashes during menopause, often accompanied by night sweats that disrupt sleep and quality of life.
While hot flashes and night sweats are most commonly associated with menopause, they can also occur due to thyroid disorders or other hormonal imbalances in both men and women. The NHS notes that these symptoms can vary in frequency and severity, ranging from mild occasional warmth to multiple intense episodes each day or night. It is important to keep track of how often these symptoms occur and how much they interfere with daily activities or sleep. Persistent or severe vasomotor symptoms warrant a discussion with a healthcare provider, as they could indicate an underlying endocrine issue that may benefit from targeted hormone therapy or other medical interventions.
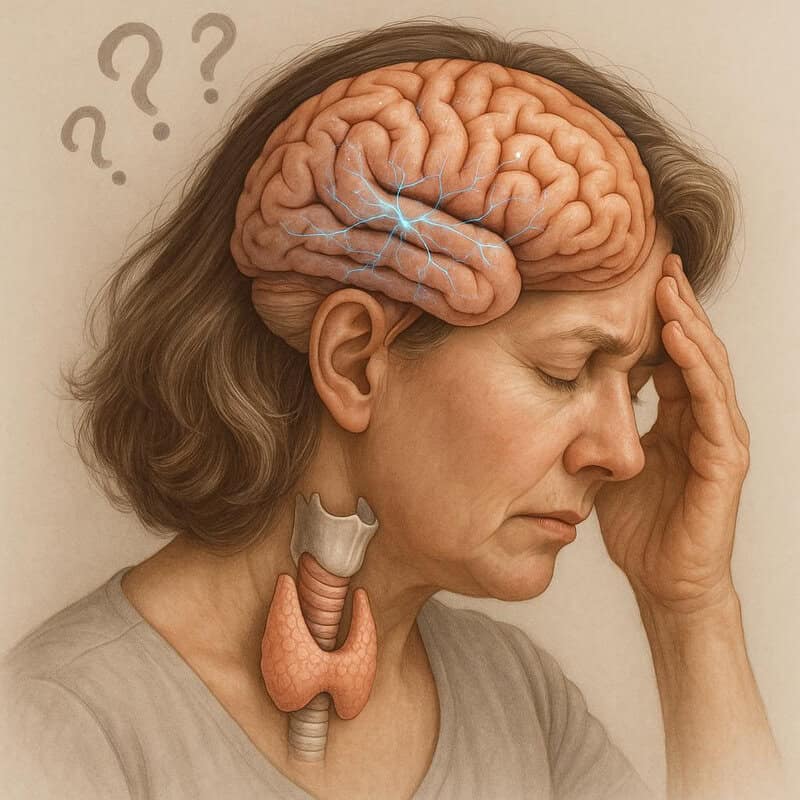
9. Difficulty Concentrating

Hormones such as thyroid hormones and cortisol play a critical role in supporting cognitive function, including memory, attention, and mental clarity. When thyroid hormone levels are either too low (hypothyroidism) or too high (hyperthyroidism), individuals often report problems with focus, forgetfulness, and mental sluggishness—commonly referred to as “brain fog.” Similarly, chronic elevation of cortisol, the body’s main stress hormone, can impair concentration and interfere with the formation of new memories, as highlighted by the National Institutes of Health.
While occasional lapses in concentration are normal, especially during periods of high stress or lack of sleep, hormone-related cognitive issues tend to be more persistent and pronounced. Unlike typical brain fog caused by temporary stress or fatigue, hormonal causes may present alongside other physical symptoms such as fatigue, mood changes, or unexplained weight shifts. The NHS suggests documenting the frequency, duration, and context of cognitive difficulties. Keeping a journal of these symptoms can help healthcare providers identify patterns and differentiate between stress-related brain fog and underlying hormonal imbalances, leading to more accurate diagnosis and targeted treatment options.
10. Dry Skin

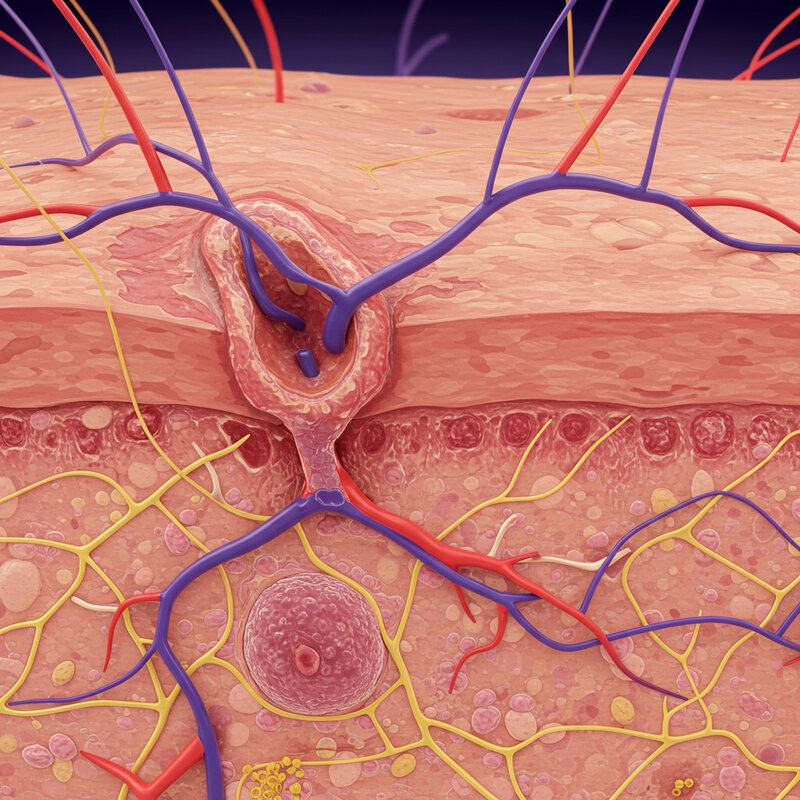
Hormones are essential for maintaining the skin’s moisture balance and overall health. Estrogen and thyroid hormones play particularly important roles by supporting the production of natural oils and regulating skin cell turnover. When hormone levels drop—such as during menopause, with thyroid dysfunction, or certain adrenal imbalances—the skin can become noticeably drier, rougher, and more prone to irritation. The American Academy of Dermatology points out that menopausal women frequently experience persistent dryness due to declining estrogen levels.
While environmental factors like cold weather, low humidity, or overuse of harsh soaps can also lead to temporary dry skin, hormone-related dryness tends to be more stubborn, widespread, and resistant to standard moisturizers. It may be accompanied by other symptoms, such as thinning hair or brittle nails. The NHS advises that if dry skin persists for several weeks despite environmental changes and proper skincare, it may signal an underlying hormonal problem. Noting the duration, severity, and accompanying symptoms can be valuable in guiding a healthcare provider toward the root cause and appropriate treatment options.
11. Increased Sensitivity to Cold or Heat
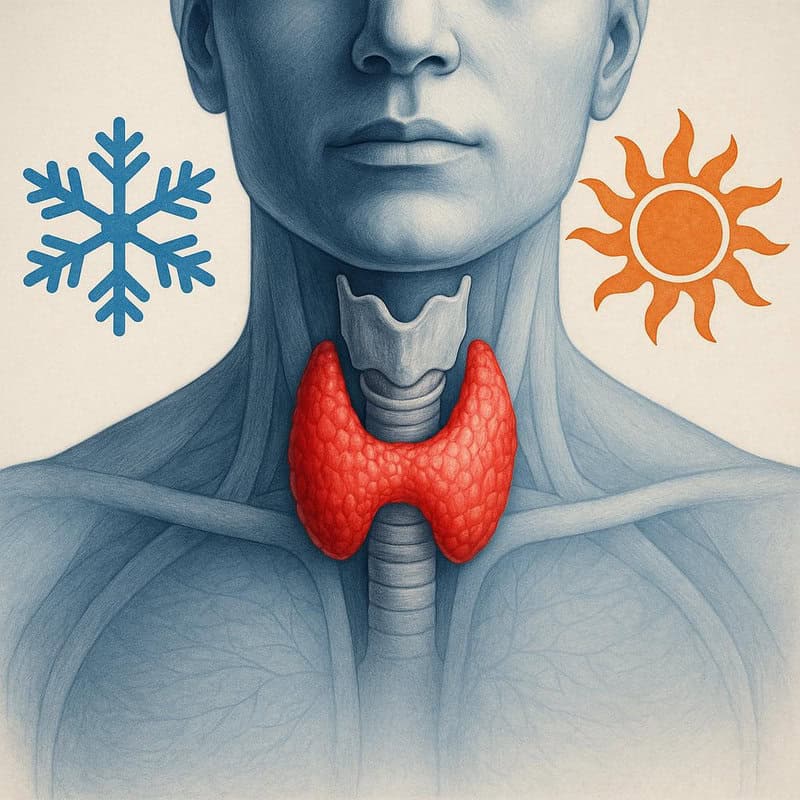
Thyroid hormones are integral to the body’s ability to regulate temperature. They influence the metabolic rate, which in turn affects how much heat the body produces and how effectively it dissipates warmth. When thyroid function is disrupted—either through hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid)—individuals can develop an increased sensitivity to cold or heat. According to the National Institute of Diabetes and Digestive and Kidney Diseases, hypothyroidism often causes people to feel unusually cold, while hyperthyroidism can make them more sensitive to heat and prone to excessive sweating.
It is normal for body temperature preferences to shift slightly with seasonal changes or during exercise. However, persistent or pronounced intolerance to cold or heat—especially when it interferes with daily activities or is accompanied by other symptoms like fatigue, weight changes, or hair loss—deserves medical attention. The NHS suggests that ongoing temperature sensitivity may be a subtle but important sign of a hormonal imbalance. If you notice these changes are consistent and unexplained by environmental factors, seeking an evaluation from a healthcare professional is recommended to rule out thyroid or other endocrine conditions.
12. Frequent Headaches

Headaches can be influenced by many factors, but hormonal fluctuations—particularly changes in estrogen—are a common and sometimes overlooked cause. Estrogen affects blood vessels in the brain and can modulate pain sensitivity, which is why women may notice more headaches at specific points in their menstrual cycle. For example, menstrual migraines often occur just before or during menstruation, when estrogen levels drop sharply. The Migraine Trust explains that these hormonally linked headaches are typically more severe and difficult to treat than other types.
While occasional headaches are normal and may be triggered by dehydration, stress, or lack of sleep, frequent or severe headaches that coincide with hormonal changes—such as menstruation, pregnancy, or perimenopause—may indicate a deeper endocrine imbalance. The NHS advises that if headaches occur regularly, are unusually intense, or are accompanied by other symptoms like visual changes, confusion, or weakness, they should not be ignored. Documenting the timing and severity of headaches can provide valuable information for healthcare providers and help determine if hormone therapy or other interventions are necessary.
13. Digestive Issues
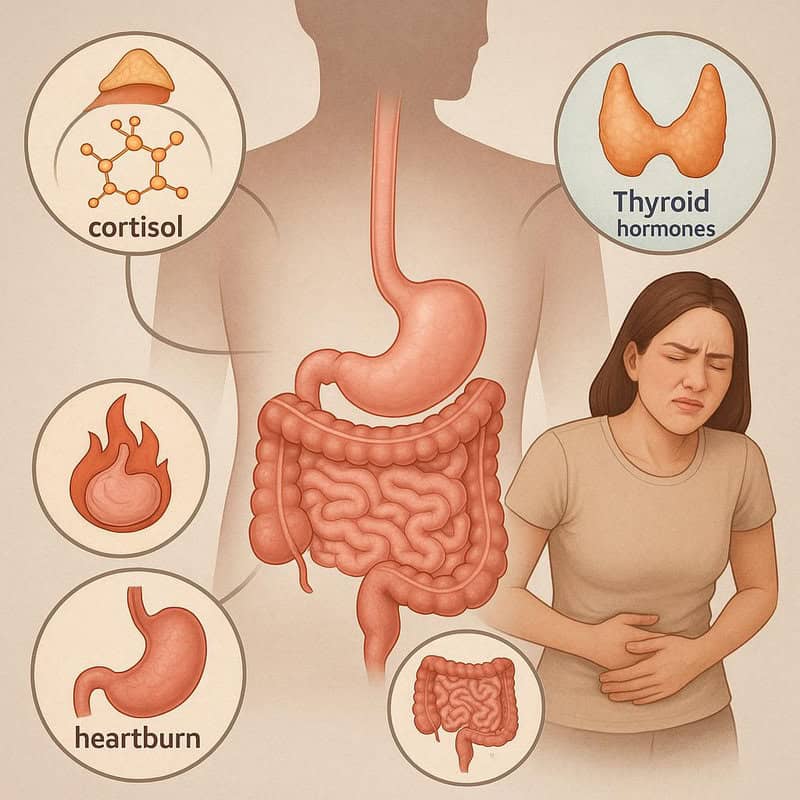
Hormones such as cortisol and thyroid hormones have a direct impact on digestive health and gut function. Cortisol, the primary stress hormone, can influence gut motility, the balance of gut bacteria, and the integrity of the intestinal lining. Chronic elevation of cortisol levels due to prolonged stress may result in symptoms like heartburn, bloating, or irritable bowel syndrome (IBS), as described by the National Institutes of Health. Similarly, thyroid hormones play a crucial role in regulating the speed at which food moves through the digestive tract. Hypothyroidism (underactive thyroid) can cause constipation, while hyperthyroidism (overactive thyroid) may lead to diarrhea or frequent bowel movements (NHS).
Although many people experience occasional digestive discomfort during periods of acute stress or dietary changes, persistent or unexplained symptoms may point to a hormonal cause. If digestive issues are ongoing, severe, or associated with other signs of hormonal imbalance such as fatigue or weight changes, it’s important to track the frequency, duration, and circumstances. Keeping a record can help healthcare professionals determine whether hormonal testing or therapy may be necessary for resolving these gastrointestinal concerns.
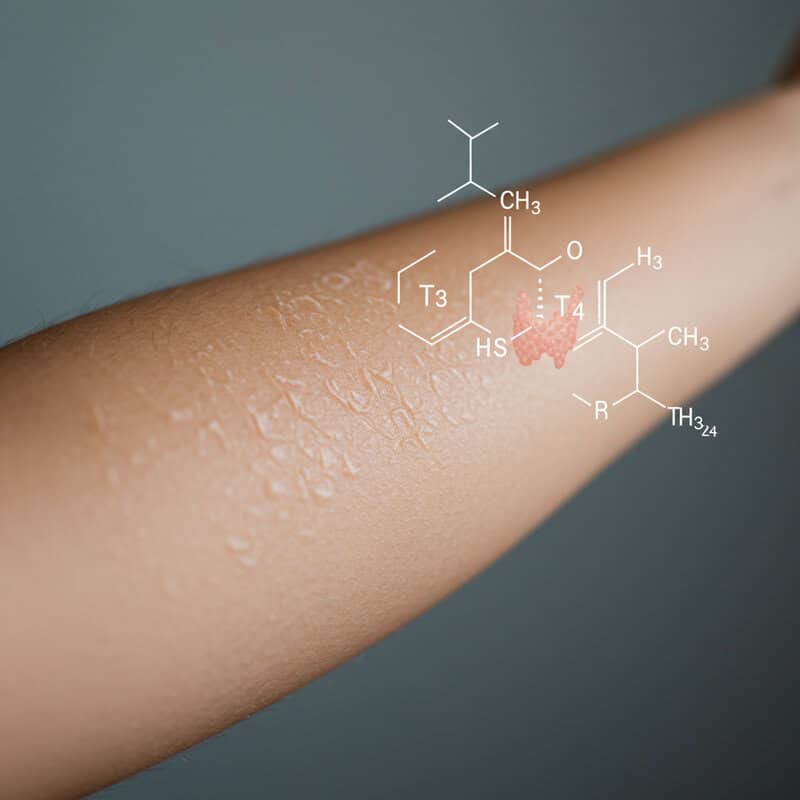
14. Unusual Sweating

Adrenaline and thyroid hormones are major regulators of the body’s sweat response. Adrenaline, released during times of stress or anxiety, can trigger sudden and intense episodes of sweating as part of the “fight or flight” response. Meanwhile, excessive production of thyroid hormones—as seen in hyperthyroidism—can increase metabolism to the point where the body generates more heat, leading to persistent or unexplained sweating even in cool environments. The Endocrine Society notes that unusual or excessive sweating can be an early sign of an underlying endocrine disorder.
It is normal to sweat in response to exercise, hot weather, or emotional stress. However, sweating that is excessive, occurs without a clear trigger, or is accompanied by other symptoms like weight loss, fatigue, or heart palpitations should be taken seriously. Distinguishing between normal, situational sweating and persistent, unexplained episodes is important for early detection. If you experience ongoing unusual sweating, especially alongside other subtle hormonal symptoms, it is advisable to consult a healthcare provider for evaluation and possible hormone testing.
15. Breast Changes
Breast tissue is highly sensitive to hormonal fluctuations, especially those involving estrogen and progesterone. These hormones can cause cyclical changes such as tenderness, swelling, or the formation of benign lumps, particularly in the days leading up to menstruation. This phenomenon, known as cyclical breast pain, is a common and generally harmless result of the menstrual cycle, as noted by the NHS. However, when breast tenderness or lumps persist outside of your normal cycle, increase in severity, or are accompanied by other symptoms such as nipple discharge or skin changes, they may warrant further investigation.
It’s important to distinguish between typical, hormonally-driven breast changes and those that are persistent or unusual. Non-cyclical pain or new lumps that do not resolve after your period may signal an underlying hormonal imbalance or, in rare cases, a more serious condition. The American Cancer Society recommends regular breast self-exams and prompt reporting of any changes to a healthcare professional. Early evaluation can help differentiate between benign hormonal effects and conditions that require further attention or intervention.
16. Joint or Muscle Pain

Hormones such as estrogen play a significant role in maintaining joint and muscle health. Estrogen has anti-inflammatory properties and helps protect joint tissues, which is why many women notice increased joint stiffness or muscle pain as estrogen levels decline during menopause or perimenopause. According to the Versus Arthritis organization, reduced estrogen can lead to more pronounced aches, pains, and even swelling, especially in the hands, knees, and shoulders.
While occasional muscle soreness or joint discomfort is normal, particularly after physical activity or aging, hormonally-driven pain tends to be more persistent and widespread. It may arise without any clear injury or overuse and can be accompanied by other hormonal symptoms like hot flashes or mood changes. The NHS suggests that if joint or muscle pain becomes chronic, unexplained, or interferes with daily life, it should be evaluated by a healthcare professional. Keeping a record of when symptoms occur and any associated changes can help identify patterns linked to hormonal fluctuations and guide appropriate management, including the potential need for hormone therapy.
17. Changes in Appetite
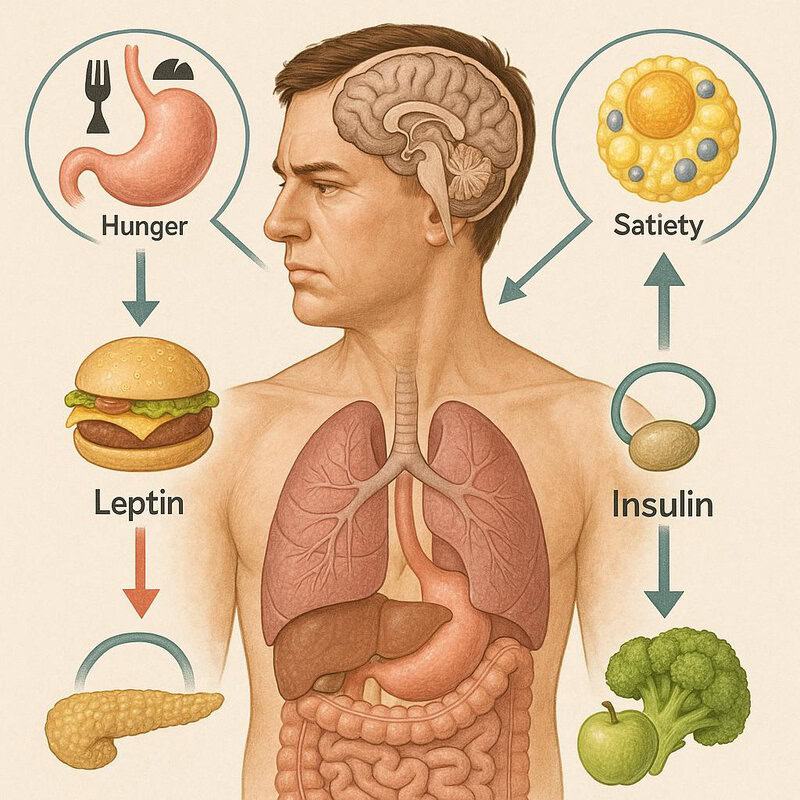
Hunger and satiety are regulated by a complex interplay of hormones, including leptin, ghrelin, and insulin. Leptin, produced by fat cells, signals the brain to reduce appetite when energy stores are sufficient, while ghrelin, released in the stomach, stimulates hunger. Insulin also plays a role in managing blood sugar and influencing when and how much we eat. When these hormones are out of balance—due to factors such as chronic stress, thyroid dysfunction, or insulin resistance—individuals may experience persistent changes in appetite, ranging from intense cravings to a sudden lack of interest in food (NIH).
It’s normal for appetite to fluctuate with emotional stress, physical activity, or changes in routine—sometimes leading to “stress-eating” or loss of appetite during difficult periods. However, ongoing and unexplained shifts in hunger or fullness may signal a deeper hormonal issue. The NHS suggests monitoring appetite changes that last several weeks, especially if they are accompanied by weight changes, fatigue, or digestive symptoms. Tracking when these changes occur and any related factors can help a healthcare provider determine if hormonal testing or intervention is necessary.
18. High Blood Pressure

Adrenal hormones, particularly aldosterone and cortisol, play a vital role in regulating blood pressure by controlling fluid balance and vascular tone. When the adrenal glands produce excessive amounts of these hormones—such as in conditions like Cushing’s syndrome or Conn’s syndrome—it can lead to persistent high blood pressure (hypertension) that does not respond well to typical lifestyle modifications like diet and exercise. The Blood Pressure UK organization highlights that hormonal causes of hypertension are often overlooked, yet treatable.
While most cases of high blood pressure are linked to factors such as obesity, high sodium intake, or lack of physical activity, hormonal hypertension tends to be more resistant and may be accompanied by symptoms like muscle weakness, headaches, or unexplained weight gain. Regular blood pressure monitoring is key, as recommended by the NHS. If consistently high readings are found and lifestyle changes don’t help, it’s important to ask your healthcare provider about possible hormonal evaluations to identify or rule out endocrine-related causes.
19. Acne in Adulthood

Androgens, a group of hormones that includes testosterone, are closely linked to the development of acne. These hormones stimulate the sebaceous (oil) glands in the skin, which can lead to increased oil production, clogged pores, and the growth of acne-causing bacteria. While acne is commonly associated with adolescence, many adults—especially women—experience persistent breakouts due to hormonal fluctuations related to menstrual cycles, polycystic ovary syndrome (PCOS), pregnancy, or menopause (American Academy of Dermatology).
It’s normal to have an occasional breakout due to stress, diet, or changes in skincare routines. However, stubborn, cystic, or recurring acne that appears primarily along the jawline, chin, or lower cheeks in adulthood may be a sign of an underlying hormonal imbalance. The NHS recommends consulting a dermatologist if adult acne is persistent, severe, or resistant to over-the-counter treatments. A healthcare professional can help determine if hormone testing or therapy is appropriate, as well as recommend customized skincare and medications to effectively manage hormonally driven acne.
20. Thinning Eyebrows

Thyroid hormones are essential for the normal growth and maintenance of hair, including the eyebrows. One classic but often subtle sign of thyroid dysfunction—particularly hypothyroidism (underactive thyroid)—is the thinning or loss of the outer third of the eyebrows, a phenomenon known as Queen Anne’s sign. This occurs because insufficient thyroid hormone disrupts the hair growth cycle, leading to slower growth and increased shedding. According to the British Thyroid Foundation, eyebrow thinning can be an early indicator of thyroid problems, even before other symptoms develop.
While eyebrow thinning can also result from over-plucking, aging, or certain skin conditions like eczema, it’s important to watch for persistent or progressive changes, especially if accompanied by other signs such as fatigue, weight gain, or dry skin. The NHS advises seeking medical advice if you notice ongoing eyebrow loss along with other symptoms of hormonal imbalance. Early recognition and evaluation can help identify thyroid issues and allow for timely treatment, often reversing hair loss and restoring normal growth when hormone levels are corrected.
21. Infertility or Difficulty Conceiving
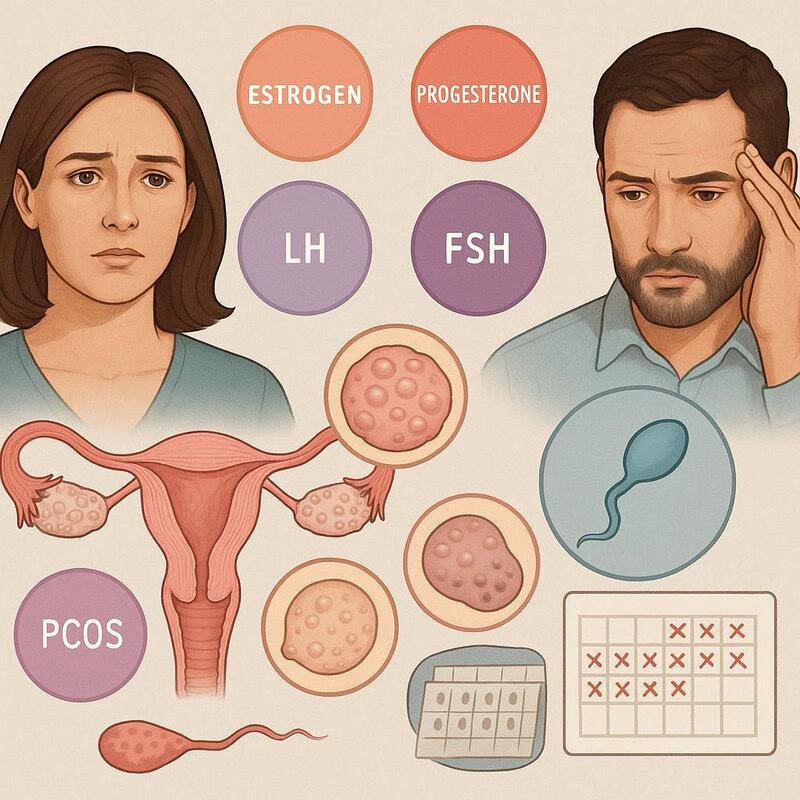
Hormones play a fundamental role in regulating fertility for both women and men. The coordinated actions of estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) govern ovulation, menstrual cycles, and the ability to conceive. Disruptions in this hormonal balance can interfere with regular ovulation or sperm production, leading to challenges with conception. One of the most common hormone-related causes of infertility is polycystic ovary syndrome (PCOS), a condition affecting up to 12% of women of reproductive age in the United States according to the CDC. PCOS is characterized by irregular cycles, excess androgens, and often, cysts on the ovaries, all of which can hinder fertility.
Experiencing occasional irregular cycles or delays in conception can be normal, especially with age or lifestyle changes. However, the NHS recommends seeking medical evaluation if you have been trying to conceive for 12 months or more without success (or 6 months if over age 35). Early assessment can identify underlying hormonal imbalances and help guide appropriate interventions, which may include hormone therapy, fertility treatments, or lifestyle modifications.
22. Changes in Voice
Hormones have a significant influence on the structure and function of the vocal cords. Estrogen, progesterone, and thyroid hormones help maintain the flexibility and lubrication of the vocal tissues. When hormone levels fluctuate or decline—such as during menopause or with thyroid dysfunction—they can cause subtle but noticeable changes in voice quality. For example, women in menopause may experience a deeper, hoarser, or less stable voice due to reduced estrogen’s impact on the mucous membranes and collagen in the vocal folds (NIH).
Similarly, hypothyroidism can cause swelling of the vocal cords, resulting in a raspy or weak voice. According to the British Thyroid Foundation, these changes may develop gradually and may be accompanied by other symptoms like fatigue, dry skin, or weight gain. While temporary voice changes are common after illness or overuse, persistent or progressive changes—especially if not linked to a clear cause—should be evaluated by a healthcare provider. Monitoring your voice over time can help identify hormonal issues early and support timely intervention.
23. Reduced Bone Density
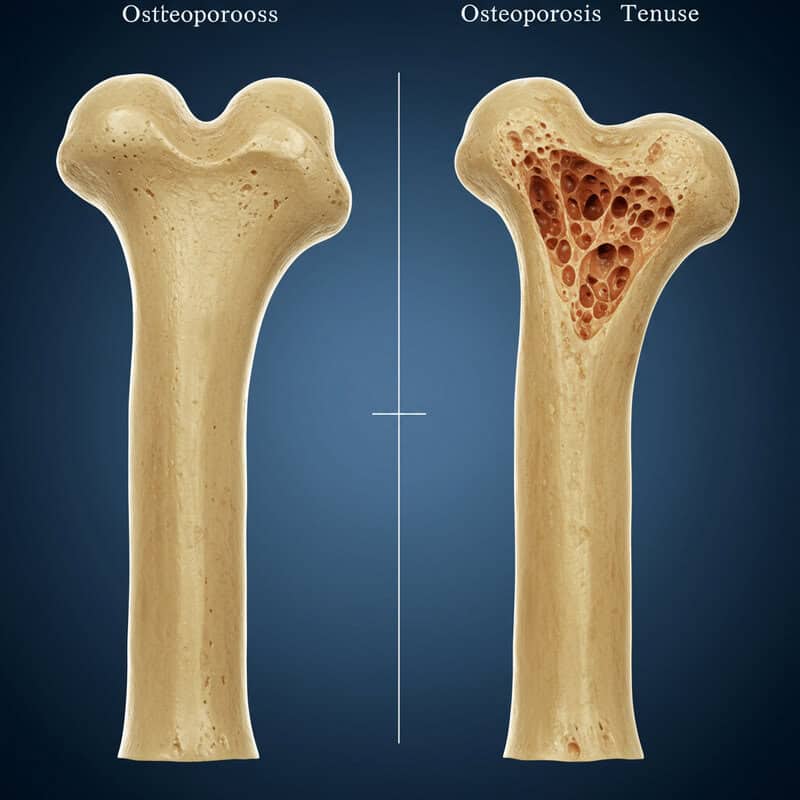
Hormones such as estrogen and testosterone are vital for maintaining strong, healthy bones. Estrogen helps slow the natural breakdown of bone tissue, while testosterone supports bone formation and density. When levels of these hormones decline—particularly during menopause in women or andropause in men—the rate of bone loss accelerates, increasing the risk of osteoporosis and fractures. The NHS notes that postmenopausal women are especially vulnerable, as the sharp drop in estrogen that occurs after menopause can lead to significant reductions in bone density within just a few years.
While some bone loss with age is normal, excessive or accelerated loss can result in brittle bones and a higher likelihood of breaks, even from minor falls. Groups at higher risk include women over 50, men with low testosterone, those with a family history of osteoporosis, and individuals taking certain medications or with other endocrine disorders. Regular screening—such as bone density scans—is recommended for these at-risk populations. Early detection of reduced bone density can prompt preventative measures, including hormone therapy, calcium and vitamin D supplements, and lifestyle changes to support bone health.
24. Frequent Urination
Hormonal imbalances, particularly those involving insulin (as seen in diabetes) and adrenal hormones such as aldosterone, can significantly impact urinary patterns. In diabetes, either a lack of insulin or the body’s inability to use it effectively leads to high blood glucose levels. The kidneys work harder to filter and excrete this excess glucose, resulting in frequent urination—one of the earliest symptoms of both type 1 and type 2 diabetes (CDC). Adrenal hormones like aldosterone help regulate the body’s fluid and electrolyte balance; imbalances can cause both increased urination and changes in thirst (NHS).
It is normal to urinate more often with increased fluid intake, caffeine consumption, or cold temperatures. However, a sudden or persistent increase in urination—especially if unrelated to lifestyle factors or accompanied by symptoms such as excessive thirst, fatigue, or unexplained weight loss—may indicate an underlying hormonal issue. Noting changes in frequency, urgency, and associated symptoms is important for early detection and should be discussed with a healthcare provider if the pattern continues for more than a few days.
25. Blurred Vision

Hormonal imbalances can have a direct impact on vision, most notably through fluctuations in blood sugar and thyroid hormones. High blood sugar levels, as seen in uncontrolled diabetes, can cause the lens of the eye to swell, leading to blurred vision or rapid changes in prescription. Prolonged hyperglycemia can also damage blood vessels in the retina, increasing the risk of diabetic retinopathy, according to the CDC. Similarly, both hyperthyroidism and hypothyroidism can cause eye changes, such as dryness, swelling, or double vision, due to inflammation or tissue buildup behind the eyes (NHS).
While temporary blurred vision is commonly caused by eye strain, fatigue, or excessive screen time, persistent or unexplained changes in vision—especially when accompanied by other symptoms such as increased thirst, weight fluctuations, or eye discomfort—may signal a hormonal issue. The NHS advises that any sudden or continuous visual disturbances should prompt timely evaluation by a healthcare professional. Keeping track of when vision changes occur and any related symptoms can help in identifying the root cause and preventing further complications.
26. Decreased Muscle Mass

Testosterone and growth hormone are essential for building and maintaining muscle mass throughout life. Testosterone promotes protein synthesis and muscle repair, while growth hormone stimulates tissue growth and regeneration. As people age, natural declines in these hormones can lead to a gradual loss of muscle mass, a condition known as sarcopenia. According to the National Institutes of Health, age-related hormonal changes are among the primary drivers of this process, but decreased muscle mass can also result from untreated hormone deficiencies at any age.
While some muscle loss is a normal part of aging, significant or rapid decreases—especially in the absence of changes to physical activity or diet—may indicate an underlying hormonal imbalance. This is particularly relevant for men experiencing low testosterone or those with pituitary disorders affecting growth hormone production. The NHS suggests noting persistent weakness, reduced strength, or visible loss of muscle bulk. Monitoring these changes over time and discussing them with a healthcare provider can help identify hormonal deficiencies early, enabling targeted interventions like hormone therapy, dietary adjustments, or resistance exercise programs.
27. Numbness or Tingling

Hormonal imbalances, especially those involving the thyroid gland and adrenal glands, can lead to neurological symptoms such as numbness, tingling, or “pins and needles” sensations in the hands, feet, or other extremities. Hypothyroidism, for instance, can slow nerve signal transmission and contribute to peripheral neuropathy—a condition characterized by persistent numbness or tingling (British Thyroid Foundation). Adrenal insufficiency, such as in Addison’s disease, can also affect electrolyte balance and nerve function, causing similar symptoms (NHS).
A real-world example includes individuals with untreated hypothyroidism reporting progressive numbness in their fingers and toes, sometimes accompanied by muscle weakness or cramping. While occasional tingling from sitting awkwardly or temporary pressure on a nerve is harmless, persistent or unexplained symptoms can signal an underlying hormonal problem or even more serious neurological conditions. The NHS recommends seeking prompt medical evaluation if numbness or tingling occurs frequently, worsens over time, or is associated with other signs of hormonal imbalance. Early detection is important for preventing further nerve damage and ensuring appropriate treatment.
28. Puffy Face or Eyes

Hypothyroidism, or an underactive thyroid, can cause fluid retention and swelling in various parts of the body, most noticeably in the face and around the eyes. This puffiness—sometimes referred to as myxedema—is a result of reduced thyroid hormone levels slowing down metabolism and altering fluid balance. The NHS lists facial swelling as a classic sign of hypothyroidism, often appearing alongside other symptoms like fatigue, weight gain, and dry skin.
It is normal to occasionally experience mild facial puffiness, especially after consuming salty foods, crying, or not getting enough sleep. However, swelling caused by hormonal imbalances is typically more persistent and cannot be easily explained by lifestyle or dietary factors. Puffiness from hypothyroidism may also be accompanied by swelling in the hands, feet, or lower legs. If facial or periorbital swelling occurs frequently, lasts for several days, or is associated with other symptoms of thyroid dysfunction, the British Thyroid Foundation recommends consulting a healthcare provider. Early diagnosis and treatment of hypothyroidism can reverse swelling and prevent complications.
29. Slow Heart Rate
Thyroid hormones, particularly triiodothyronine (T3) and thyroxine (T4), play an essential role in maintaining the heart’s rhythm and speed. In cases of hypothyroidism, reduced hormone levels can slow the heart rate—a condition known as bradycardia. This occurs because thyroid hormones help regulate the heart’s electrical activity and the force of each contraction. The British Thyroid Foundation notes that a persistently slow heart rate, especially when accompanied by fatigue, cold intolerance, or weight gain, may signal underlying thyroid dysfunction.
While a low resting heart rate (often below 60 beats per minute) can be healthy and normal in well-conditioned athletes, abnormal bradycardia in non-athletes—particularly if it is associated with other symptoms—should prompt further evaluation. Symptoms of concern include dizziness, weakness, chest pain, or fainting. The NHS recommends monitoring your pulse regularly and seeking medical advice if you notice persistent slowness or episodes of unexplained fatigue. Early detection of thyroid-related bradycardia allows for timely intervention and can help restore normal heart function.
30. Irregular Heartbeat
Hormonal imbalances, particularly involving the thyroid gland and adrenal hormones, can significantly affect heart rhythm and lead to arrhythmias—irregular, too fast, or too slow heartbeats. Hyperthyroidism (overactive thyroid) can cause the heart to beat erratically or rapidly, resulting in palpitations, skipped beats, or atrial fibrillation. According to the NHS, these disruptions occur because excess thyroid hormones increase the sensitivity of the heart’s electrical system. Similarly, high levels of adrenaline and cortisol during periods of extreme stress or adrenal gland disorders can also trigger abnormal heart rhythms.
A real-world example is the development of atrial fibrillation in individuals with untreated hyperthyroidism, which may present as a fluttering sensation in the chest, dizziness, or shortness of breath. While occasional palpitations can be harmless—often related to caffeine, anxiety, or dehydration—persistent or worsening irregular heartbeats, especially when accompanied by chest pain or fainting, require prompt medical attention. The British Heart Foundation recommends tracking the frequency and circumstances of these symptoms to assist healthcare providers in diagnosis and treatment, potentially including hormone evaluation and therapy.
31. Frequent Infections
Hormones such as cortisol—the body’s primary stress hormone—and thyroid hormones play a crucial role in regulating the immune system. Chronic elevation of cortisol, as seen in prolonged stress or Cushing’s syndrome, can suppress immune function, making the body more susceptible to infections. Similarly, both hypothyroidism and hyperthyroidism can impair the immune response, reducing the body’s ability to fight off viruses and bacteria. The National Institutes of Health highlights that individuals with hormonal imbalances may notice an increased frequency of illnesses, such as colds, respiratory infections, or skin infections.
While catching a cold or mild infection occasionally is normal—especially during certain seasons or in crowded environments—repeated or lingering infections may signal a weakened immune system due to underlying hormonal problems. The NHS advises being vigilant if you experience recurrent infections, slow healing, or unusual illnesses. Keeping track of how often you become ill and the severity of each episode can help healthcare providers determine whether hormonal testing or therapy is needed to restore immune balance and protect long-term health.
32. Feeling Depressed
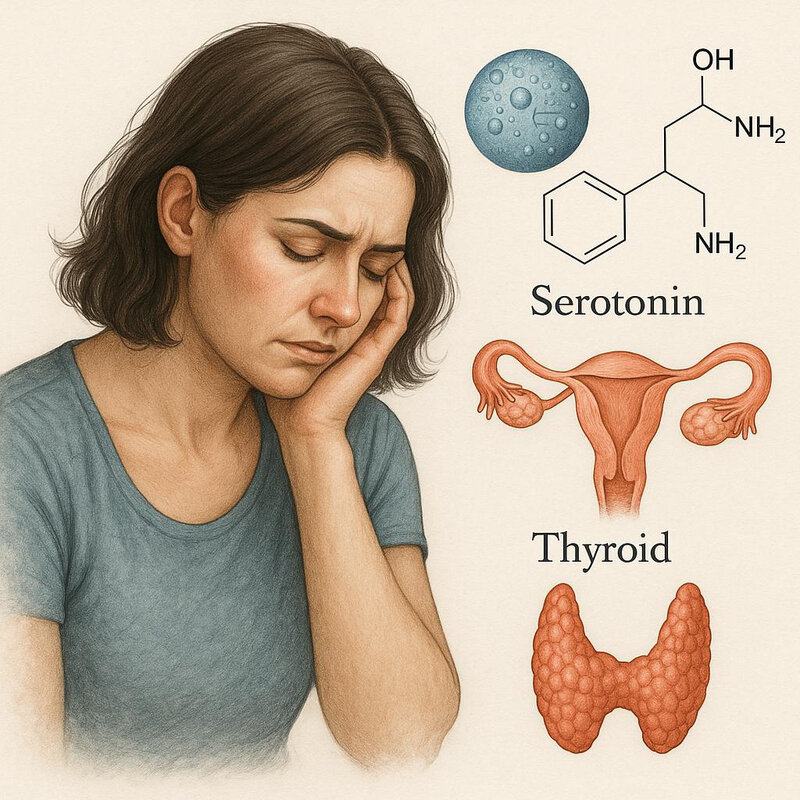
Hormones play a profound role in regulating mood, with serotonin, estrogen, and thyroid hormones among the most influential. Serotonin is a neurotransmitter often called the “feel-good” chemical, and its production is closely linked to hormonal activity. Low levels of thyroid hormones (hypothyroidism) can cause or worsen depression, fatigue, and apathy, as noted by the British Thyroid Foundation. Similarly, fluctuations in estrogen and progesterone can contribute to mood swings and persistent sadness, particularly during perimenopause, postpartum, or following significant hormonal shifts (American Psychiatric Association).
It’s normal to experience brief periods of sadness or low mood in response to stressful events, loss, or major life transitions. However, persistent feelings of hopelessness, loss of interest in activities, or ongoing low energy may indicate a deeper hormonal or medical issue. The NHS encourages seeking support from a healthcare provider if low mood lasts for more than two weeks or is accompanied by changes in sleep, appetite, or concentration. Addressing hormonal imbalances can be a key part of an effective treatment plan for depression.
33. Loss of Height

Declining levels of estrogen in women and testosterone in men can significantly accelerate bone loss, leading to weakened vertebrae and gradual loss of height. These hormones are essential for maintaining bone density; when they decrease—especially after menopause or during andropause—bones become more susceptible to osteoporosis and compression fractures. The National Osteoporosis Foundation explains that vertebral compression from osteoporosis often results in individuals losing one inch or more in height over time and may cause a stooped posture or back pain.
While minor height changes with aging are common, a noticeable or rapid reduction in height is a red flag for underlying bone loss. Osteoporosis can occur silently, so you may not experience symptoms until a fracture occurs. The NHS recommends regular height checks—especially for postmenopausal women, older adults, and those with risk factors for bone disease. Early identification of height loss can prompt bone density screening and intervention, such as hormone therapy, calcium and vitamin D supplementation, and weight-bearing exercises to help prevent further bone deterioration.
34. Cravings for Salt or Sugar
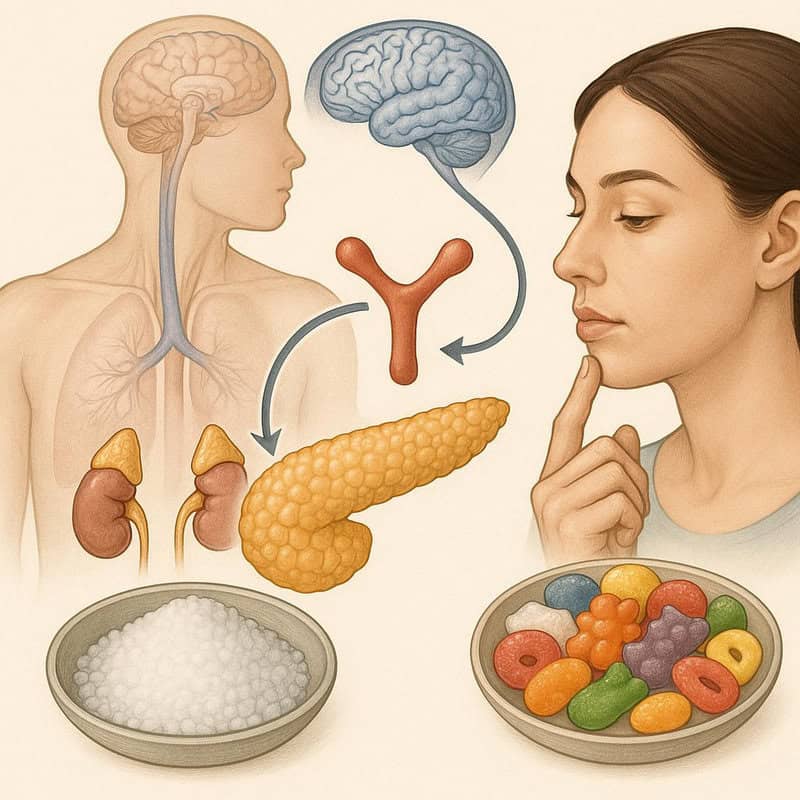
Hormonal imbalances, particularly involving the adrenal glands and insulin, can strongly influence cravings for salt or sugar. The adrenal glands produce hormones like cortisol and aldosterone, which help regulate electrolyte and glucose balance. In conditions such as Addison’s disease, low aldosterone levels can lead to intense salt cravings as the body attempts to compensate for sodium loss (NHS). Similarly, imbalances in insulin, the hormone that controls blood sugar, can trigger frequent sugar cravings or episodes of hypoglycemia, leading to a cycle of seeking quick energy from sweets (CDC).
It’s normal for taste preferences to shift with stress, menstruation, or changes in physical activity. Occasional cravings are usually harmless, but persistent, intense, or unexplained urges for salty or sugary foods may be a subtle signal of an underlying hormonal disorder. The NHS recommends tracking your cravings along with your daily diet to identify patterns and potential triggers. If cravings are ongoing and interfere with your nutrition or health, consulting a healthcare provider is advised to rule out hormonal causes and receive personalized dietary guidance.
35. Decreased Sweating
An underactive thyroid (hypothyroidism) can reduce the body’s ability to produce sweat, a subtle but telling sign of hormonal imbalance. Thyroid hormones—triiodothyronine (T3) and thyroxine (T4)—are crucial for regulating metabolism, which in turn influences body temperature and sweat gland activity. When thyroid hormone levels drop, the metabolic rate slows and sweat production decreases, leading to noticeably dry skin and a reduced ability to cool the body during heat or physical exertion. The NHS lists decreased sweating as a symptom of hypothyroidism, often accompanied by other signs such as fatigue, weight gain, and sensitivity to cold.
Normal sweat patterns vary widely and can be influenced by genetics, climate, hydration, and activity level. However, a persistent reduction in sweating—especially if it develops gradually and is not linked to medication, dehydration, or environmental factors—may indicate a hormonal issue. The British Thyroid Foundation recommends considering thyroid function testing if you notice ongoing changes in sweating, particularly alongside other symptoms of hypothyroidism. Early diagnosis allows for effective management and helps restore normal sweat production and overall well-being.
36. Oily Skin
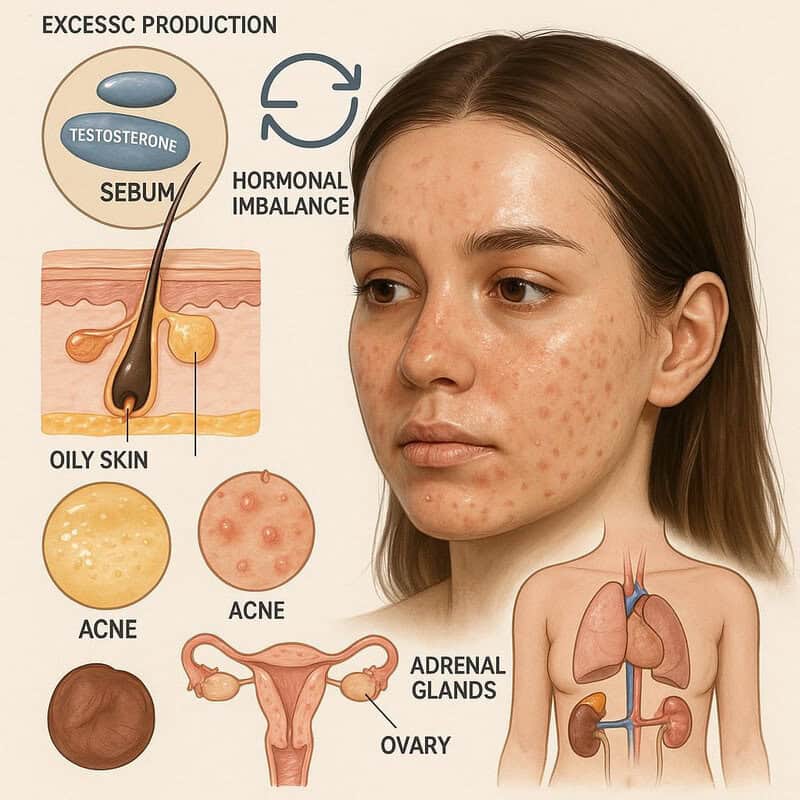
Excess production of androgens—a group of hormones that includes testosterone—can stimulate the sebaceous glands to produce more sebum, resulting in oily skin. This is a common hormonal phenomenon during puberty, when androgen levels naturally rise, causing the skin to appear shiny and increasing the risk of acne. However, in adulthood, persistent oily skin may signal an underlying hormonal imbalance, such as polycystic ovary syndrome (PCOS), adrenal gland disorders, or even hormonal fluctuations related to the menstrual cycle (American Academy of Dermatology).
While temporary oiliness can occur due to hot weather, exercise, or heavy skincare products, ongoing excessive oil production—especially when accompanied by adult acne, irregular periods, or hair changes—warrants closer attention. The NHS suggests using gentle, non-comedogenic cleansers and oil-free moisturizers to help manage oily skin. For persistent or severe cases, particularly if linked to other symptoms of hormonal imbalance, consulting a healthcare provider or dermatologist is recommended. They may suggest hormone testing or targeted treatments to address the root cause and restore balance to your skin.
37. Delayed Wound Healing
Hormonal imbalances, particularly those involving insulin (as seen in diabetes) and thyroid hormones, can significantly impair the body’s ability to heal wounds. In diabetes, high blood sugar levels damage blood vessels and nerves, reducing blood flow and the delivery of essential nutrients to injured tissue. This results in delayed wound healing and an increased risk of infection or complications, especially in the feet and lower legs (CDC). Similarly, hypothyroidism can slow cellular repair and regeneration, causing even minor cuts or bruises to heal more slowly (British Thyroid Foundation).
While some delay in healing is normal with age or certain medications, wounds that persist for weeks, reopen, or become easily infected may suggest an underlying hormonal disorder. The NHS advises monitoring the recovery time of cuts, scrapes, or ulcers—especially if you have a history of diabetes or thyroid issues. Noting patterns of slow healing can help your healthcare provider identify hormonal causes and recommend effective management strategies to support proper tissue repair.
38. Swelling in Hands or Feet

Hormonal imbalances, particularly hypothyroidism and disruptions in cortisol production, can lead to fluid retention and noticeable swelling in the hands or feet. In hypothyroidism, lowered thyroid hormone levels slow metabolism and alter the movement of fluids in the body, resulting in puffiness or swelling—often most visible around the hands, feet, and face. This type of swelling, known as myxedema, can also make the skin appear thicker or doughy (NHS).
Cortisol, produced by the adrenal glands, helps regulate sodium and water balance. Both excessive (Cushing’s syndrome) and insufficient cortisol (Addison’s disease) can disrupt this regulation, causing swelling, especially in the extremities (Endocrine Society). While mild swelling can result from standing for long periods, hot weather, or minor injuries, persistent or unexplained swelling—especially when accompanied by fatigue, weight changes, or skin changes—should prompt further evaluation. Tracking when swelling occurs and whether it improves with rest or elevation can help your healthcare provider determine if hormone testing or intervention is needed to address the underlying cause.
39. Abnormal Body Hair Growth
Excess androgens—male hormones such as testosterone—can lead to abnormal body hair growth, a condition known as hirsutism, particularly in women. Hirsutism is characterized by the appearance of coarse, dark hair in areas where women typically have minimal hair, such as the face, chest, back, or abdomen. One of the most common causes of increased androgen levels in women is polycystic ovary syndrome (PCOS), which disrupts normal hormone balance and affects up to 10% of women of reproductive age, according to the CDC.
While some variation in hair growth is normal and influenced by genetics or ethnicity, the sudden or progressive development of thick, dark hair in a male-pattern distribution is a red flag for hormonal imbalance. The NHS recommends seeking medical advice if you notice new or worsening hair growth on the face, chest, or other atypical areas, particularly when accompanied by other symptoms such as irregular periods, acne, or voice changes. Early evaluation can help identify the underlying hormonal cause and guide appropriate treatment, including hormone therapy or medications to manage symptoms.
40. Frequent Moodiness or Irritability
Hormonal fluctuations—especially changes in estrogen, progesterone, and testosterone—can have a pronounced effect on emotional stability, leading to frequent moodiness or irritability. These cyclical mood changes are commonly reported during premenstrual syndrome (PMS), perimenopause, and menopause, as well as in men experiencing low testosterone levels. The American Psychiatric Association notes that hormonally driven mood swings often arise suddenly and can be more intense than typical emotional responses to daily stressors.
While it’s normal to feel irritable or moody in response to stressful events, lack of sleep, or major life changes, hormone-related irritability tends to follow a pattern related to menstrual cycles, menopause, or other endocrine shifts. You may notice mood changes that recur monthly, worsen at certain points in your cycle, or persist through periods of hormonal transition. The NHS recommends tracking your mood and identifying any correlations with physical symptoms or hormonal milestones. Recognizing these patterns can help you and your healthcare provider distinguish between situational moodiness and symptoms rooted in hormonal imbalance, guiding appropriate treatment and support.
41. Difficulty Losing Weight
Hormonal imbalances, particularly involving the thyroid gland and estrogen levels, can significantly affect metabolism and make weight loss challenging. An underactive thyroid (hypothyroidism) slows metabolic processes, resulting in fewer calories burned at rest and a tendency to gain or retain weight despite healthy eating and exercise habits (NHS). Similarly, declining estrogen during menopause can lead to increased fat storage around the abdomen and a shift in body composition, making it harder to lose weight with standard lifestyle modifications (National Institute on Aging).
While plateauing weight loss can result from inconsistent diet, lack of exercise, or high stress, persistent inability to lose weight—despite sustained, evidence-based efforts—may indicate an underlying hormonal issue. If you experience ongoing struggles with weight loss, particularly when accompanied by fatigue, hair loss, or other symptoms of endocrine imbalance, it’s important to seek medical evaluation. Hormone testing and a thorough review of your health can help pinpoint metabolic slowdowns and guide effective interventions that go beyond diet and exercise alone.
42. Lightheadedness or Dizziness

Hormonal imbalances involving the adrenal glands or thyroid gland can disrupt blood pressure regulation, leading to episodes of lightheadedness or dizziness. Adrenal insufficiency, such as in Addison’s disease, impairs the production of aldosterone and cortisol—hormones that help maintain stable blood pressure and fluid balance. As a result, standing up quickly or prolonged standing can trigger sudden drops in blood pressure (orthostatic hypotension), causing dizziness or even fainting (NHS). Similarly, hypothyroidism can contribute to lower-than-normal blood pressure, further increasing the risk of lightheadedness (British Thyroid Foundation).
Occasional dizziness is common with dehydration, skipping meals, or rapid position changes. However, persistent or unexplained lightheadedness—especially if accompanied by fatigue, salt cravings, or darkening of the skin—may indicate a hormonal cause. Practical advice includes rising slowly from sitting or lying positions, staying hydrated, and documenting when symptoms occur. If dizziness is recurrent or severe, consult a healthcare provider for evaluation and possible hormone testing to identify and address the underlying endocrine issue.
43. Memory Problems
Estrogen and thyroid hormones play a significant role in supporting cognitive function, including memory and information processing. Estrogen helps protect neural pathways and supports neurotransmitter activity in the brain, which is why many women experience increased forgetfulness or “brain fog” during menopause when estrogen levels decline (National Institute on Aging). Similarly, both hyperthyroidism and hypothyroidism can impair concentration and memory, leading to difficulties in recalling names, appointments, or recent events (British Thyroid Foundation).
While occasional lapses in memory are a normal part of aging or can result from stress and lack of sleep, new or worsening memory problems—especially if they develop suddenly or interfere with daily functioning—should not be ignored. Persistent forgetfulness, confusion, or difficulty focusing can be subtle signs of hormonal imbalance. The NHS recommends monitoring when issues arise and noting any associated symptoms. Early recognition and discussion with a healthcare provider can help determine whether hormone testing or therapy is appropriate to restore cognitive clarity and support overall brain health.
44. Changes in Skin Pigmentation

Hormonal imbalances, particularly those involving the adrenal glands, can lead to noticeable changes in skin pigmentation. Addison’s disease, a disorder in which the adrenal glands produce insufficient amounts of cortisol and aldosterone, is a classic example. This condition triggers increased production of adrenocorticotropic hormone (ACTH), which can stimulate melanocytes and cause areas of the skin—especially creases of the hands, elbows, knees, gums, and inside the cheeks—to darken or develop a bronze tint (NHS).
While mild changes in skin color can result from sun exposure, aging, or minor injuries, persistent or progressive darkening, especially in non-sun-exposed areas, may signal an underlying endocrine problem. A real-world example is a person with Addison’s disease noticing dark patches on their knuckles, gums, and scars, along with symptoms such as fatigue, weight loss, and low blood pressure. The Endocrine Society recommends consulting a doctor if you observe unexplained changes in skin pigmentation, particularly when accompanied by other symptoms of adrenal insufficiency. Early diagnosis allows for prompt treatment and can prevent serious complications.
45. Chest Pain
Hormone imbalances can significantly impact cardiovascular health, sometimes manifesting as chest pain. Thyroid disorders, particularly hyperthyroidism, can increase heart rate, elevate blood pressure, and stress the heart, occasionally leading to palpitations or chest discomfort (British Thyroid Foundation). Similarly, fluctuations in estrogen and cortisol can influence blood vessel health and clotting, raising the risk of angina or even heart attack in some individuals (NHS).
While chest pain can also result from benign causes such as muscle strain, indigestion, or anxiety, any new, severe, or unexplained chest pain should always be taken seriously. Hormonal chest pain may be accompanied by symptoms like palpitations, shortness of breath, or dizziness, but it is not always easy to distinguish from other, potentially life-threatening conditions. The NHS urges immediate medical evaluation for sudden or persistent chest pain, especially if it is associated with sweating, nausea, or radiates to the arm or jaw. Early intervention is critical for identifying the underlying cause and preventing complications.
46. Swelling or Enlargement of the Neck
Swelling or visible enlargement of the neck can be a sign of a thyroid disorder, most commonly manifesting as a goiter. A goiter occurs when the thyroid gland becomes enlarged due to hormonal imbalances such as hypothyroidism, hyperthyroidism, or iodine deficiency. According to the NHS, a goiter may appear as a noticeable swelling at the base of the neck, which can be smooth and uniform or nodular with lumps.
While mild thyroid enlargement may not cause symptoms, a larger goiter can lead to discomfort, a tight feeling in the throat, difficulty swallowing, hoarseness, or even breathing problems if it presses against the windpipe. Regular self-checks can help you spot new or increasing swelling. To check, stand in front of a mirror and swallow while observing the lower front area of your neck for movement or bulging. The British Thyroid Foundation advises seeking prompt medical assessment if you notice new neck swelling, rapid enlargement, or associated symptoms. Early evaluation can help determine the underlying cause and guide timely treatment, preventing complications from untreated thyroid disease.
47. Decreased Motivation

Hormonal shifts can profoundly impact psychological well-being, often leading to decreased motivation and a loss of drive to pursue everyday activities or personal goals. Low levels of testosterone, estrogen, and thyroid hormones have all been linked to reduced energy, diminished interest, and apathy. For example, men with testosterone deficiency frequently report a lack of motivation and enthusiasm, while women experiencing perimenopause or menopause may notice a similar decline as estrogen levels fall (Hormone Health Network). Hypothyroidism can also cause slowed thinking and a lack of initiative (British Thyroid Foundation).
It’s normal to experience periods of low motivation during times of stress, illness, or significant life changes. However, persistent or unexplained lack of motivation—especially when accompanied by changes in mood, sleep, or appetite—may indicate an underlying hormonal imbalance. The NHS suggests documenting these changes and noting any patterns or triggers. Bringing this information to your healthcare provider can assist in distinguishing between situational and hormone-driven causes, allowing for targeted treatment and support.
48. Paleness or Anemia

Hormonal disorders involving the thyroid gland or adrenal glands can contribute to anemia, which often presents as paleness of the skin or mucous membranes. Hypothyroidism can reduce the body’s ability to produce red blood cells, resulting in fatigue, weakness, and a noticeably pale complexion (British Thyroid Foundation). Similarly, Addison’s disease can impair adrenal hormone production, affecting the absorption and utilization of nutrients necessary for red blood cell formation (NHS).
A classic example is a person with untreated hypothyroidism who develops persistent tiredness, shortness of breath, and pale skin, along with other symptoms such as weight gain or cold intolerance. While anemia can also result from dietary deficiencies or chronic illness, persistent paleness and related symptoms may signal a hormonal origin. The NHS recommends seeking medical evaluation and bloodwork if you notice ongoing fatigue, pallor, or weakness. Early diagnosis of hormonal anemia is essential, as addressing the underlying endocrine disorder can often reverse anemia and restore normal energy levels.
49. Restless Legs

Restless legs syndrome (RLS) is a neurological condition that causes an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations. Hormonal imbalances—particularly involving dopamine and thyroid hormones—can contribute to the development or worsening of RLS. Dopamine is a neurotransmitter that helps regulate muscle activity, and disruptions in its production or signaling can trigger restless leg symptoms. Additionally, hypothyroidism has been linked to an increased risk of RLS, as thyroid dysfunction may affect nerve and muscle health (Sleep Foundation).
Normal fidgetiness or the urge to stretch after sitting for long periods is common and usually temporary. However, RLS is characterized by persistent, worsening discomfort that is most noticeable at rest or in the evening, often interfering with sleep. According to the NHS, if you experience persistent tingling, crawling, or burning sensations in your legs—especially if symptoms disrupt your sleep or daily life—you should seek medical evaluation. Identifying and treating underlying hormonal imbalances can sometimes alleviate or significantly improve restless leg symptoms.
50. Excessive Thirst
Excessive thirst, also known as polydipsia, is a classic symptom of hormonal imbalances such as diabetes and adrenal disorders affecting cortisol levels. In diabetes, high blood sugar causes the kidneys to excrete more water in an attempt to eliminate excess glucose, leading to dehydration and persistent thirst (CDC). Similarly, cortisol imbalances—such as those seen in Addison’s disease or Cushing’s syndrome—can disrupt the body’s fluid and electrolyte balance, resulting in increased thirst (NHS).
It’s normal to feel thirsty after exercise, eating salty foods, or spending time in warm weather. However, ongoing and unexplained excessive thirst—especially when accompanied by frequent urination, fatigue, or unexplained weight loss—may be a warning sign of a serious hormonal disorder. The NHS recommends seeking medical evaluation and blood tests if you experience persistent polydipsia, as early diagnosis of diabetes or adrenal dysfunction is key to preventing complications and restoring health.
Conclusion

Recognizing the subtle signs of hormonal imbalance is crucial for sustaining long-term health and well-being. Many symptoms—such as fatigue, mood changes, or unexplained weight shifts—are often overlooked or mistaken for everyday stressors, yet they may signal underlying endocrine issues. Early detection through regular self-monitoring, proactive screening, and timely consultation with a healthcare provider can make a significant difference in outcomes. If you notice persistent or unexplained changes in your body, don’t hesitate to discuss them with a professional. For more on hormone health and screening, visit the Hormone Health Network or the NHS Endocrine System Guide.
Medical Disclaimer

This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized guidance. For more, visit the NHS.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





