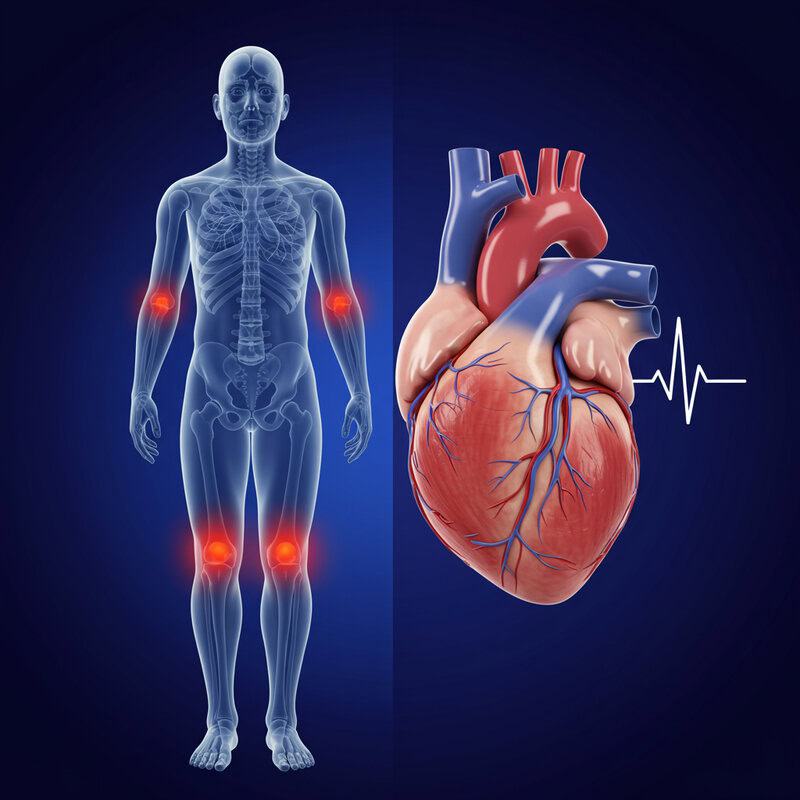
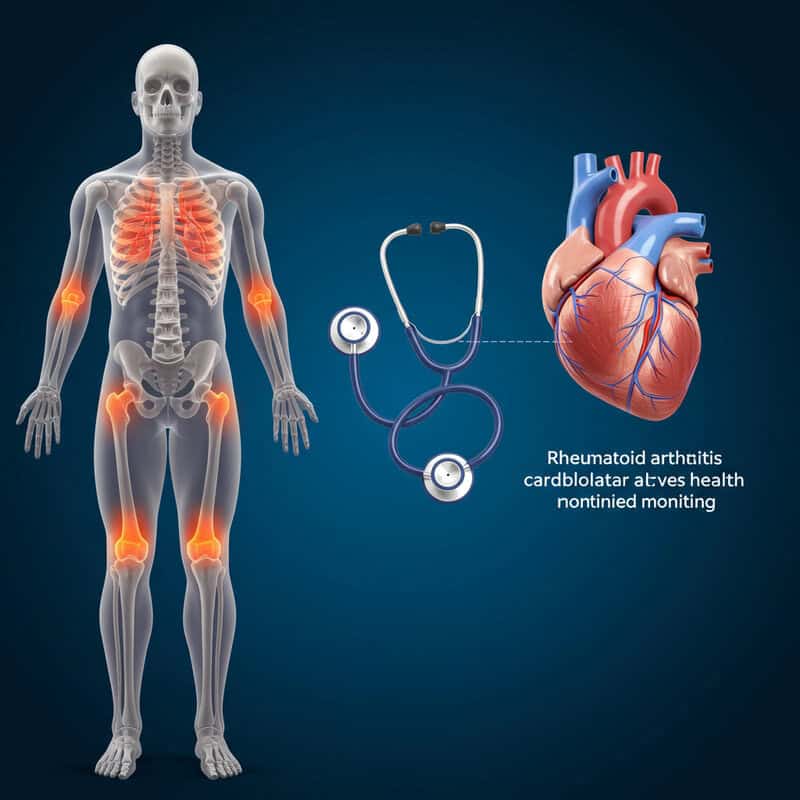
The Link Between Rheumatoid Arthritis and Heart Health
Rheumatoid arthritis (RA) affects approximately 1.3 million Americans, while heart disease remains the leading cause of death in the United States, with over 697,000 fatalities annually (CDC – RA Statistics, CDC – Heart Disease Facts). The cardiovascular system, responsible for circulating blood throughout the body, is directly impacted by both conditions. However, recognizing the link between RA and cardiovascular disease is challenging, as symptoms often emerge late, complicating early diagnosis and timely intervention for at-risk individuals.
1. Inflammation as a Common Denominator
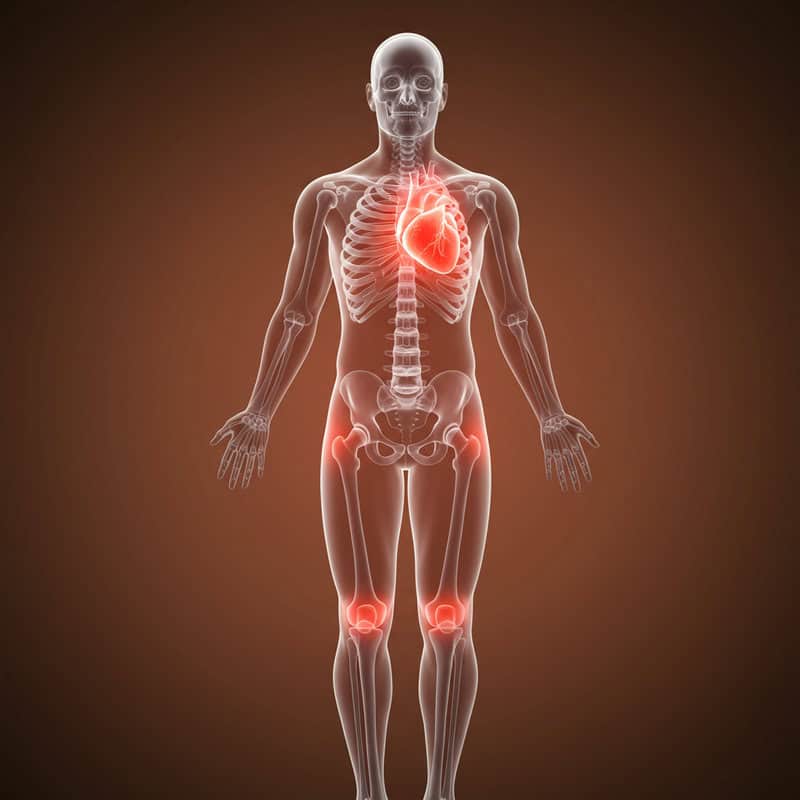
Chronic inflammation is central to both rheumatoid arthritis (RA) and heightened cardiovascular risk. In RA, the immune system mistakenly attacks the body’s own tissues, leading to persistent joint inflammation. This inflammatory process doesn’t remain confined to the joints; it extends throughout the body, damaging blood vessels and contributing to the development of atherosclerosis, or hardening of the arteries (NIH – Inflammation and Cardiovascular Risk). Similarly, other chronic inflammatory conditions such as lupus and psoriasis have been associated with increased rates of heart disease. The underlying mechanism in these diseases is the prolonged elevation of pro-inflammatory cytokines, which can harm the heart and blood vessels over time. Therefore, monitoring inflammation markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) is crucial for patients with RA. These markers help clinicians assess the degree of inflammation and the effectiveness of therapies designed to reduce it. Effective management of inflammation not only alleviates joint symptoms but may also play a pivotal role in mitigating cardiovascular risk, underscoring the importance of integrated care for individuals with RA (Arthritis Foundation – Inflammation and Heart Risk).
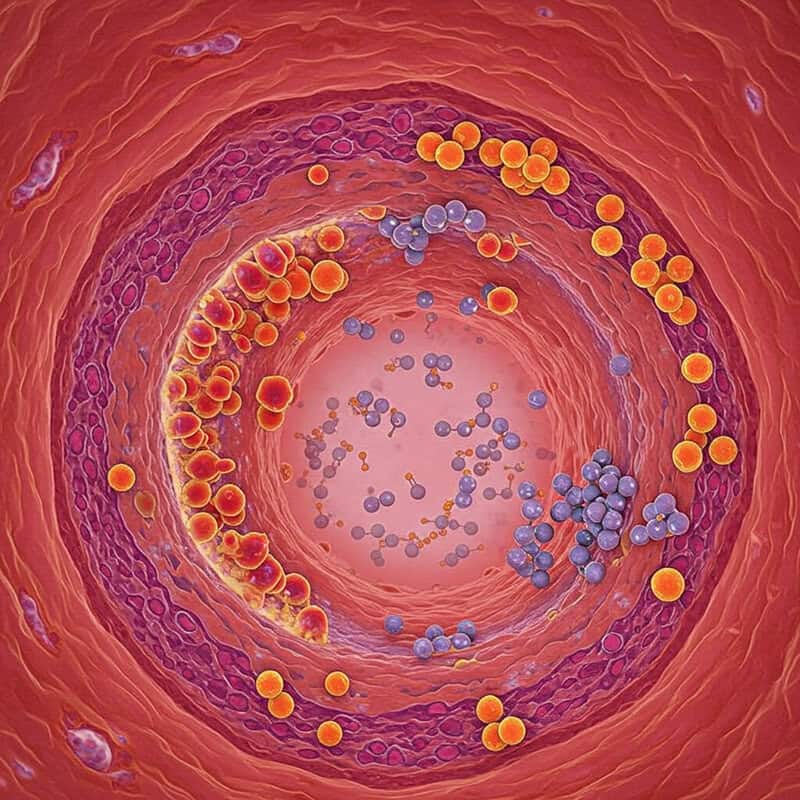
2. Autoimmune Attack and Blood Vessels
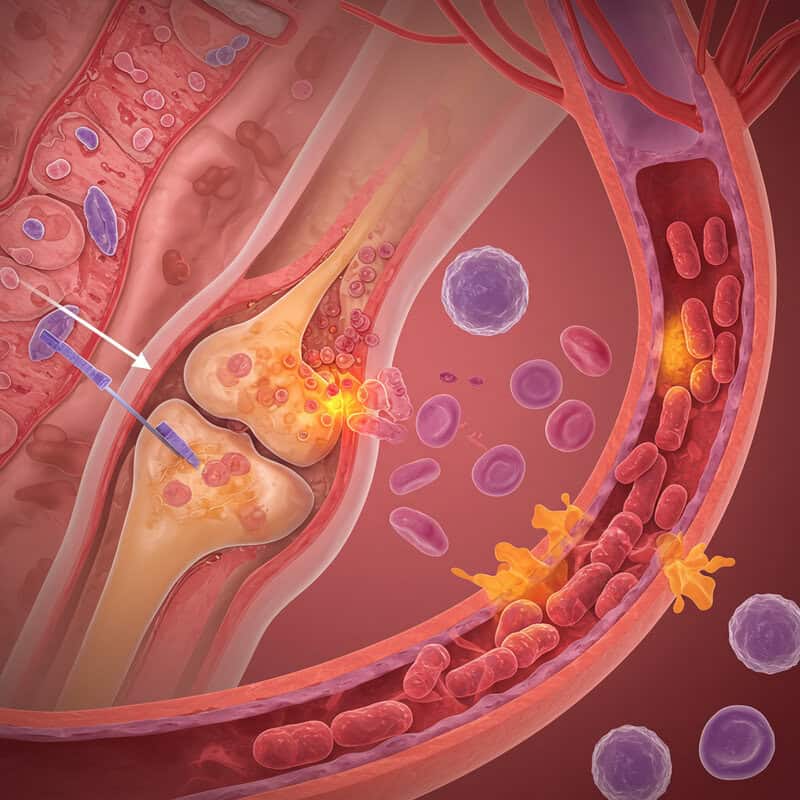
In rheumatoid arthritis (RA), the immune system’s misguided attack is not limited to the joints; it can also target blood vessels, a phenomenon known as vasculitis. This inflammation of the blood vessels can cause them to weaken, narrow, or even become blocked, reducing blood flow to vital organs and tissues (Johns Hopkins Vasculitis Center). While rheumatoid vasculitis is uncommon, it is a serious complication, most often affecting small and medium-sized arteries. The consequences can range from skin ulcers to nerve damage and, in severe cases, organ failure. People with RA should be vigilant for signs of vasculitis, such as unexplained pain, persistent ulcers, or unusual skin changes like red or purple spots. Early detection is essential, as prompt medical intervention can prevent further vascular damage and improve outcomes. Clinicians may use blood tests and imaging studies to diagnose vasculitis and monitor disease progression. Understanding the potential for autoimmune attack on blood vessels highlights the importance of regular check-ups and communication with healthcare providers for individuals with RA (American College of Rheumatology – Vasculitis).
3. Elevated C-Reactive Protein (CRP)

C-Reactive Protein (CRP) is a substance produced by the liver in response to inflammation. In rheumatoid arthritis (RA), CRP levels often rise significantly, reflecting the ongoing inflammatory process. Elevated CRP is not only a marker for active RA but is also independently associated with an increased risk of cardiovascular events such as heart attacks and strokes (CDC – C-Reactive Protein). For example, a CRP reading above 3.0 mg/L is considered high and may indicate substantial inflammation, whereas healthy individuals usually have CRP levels below 1.0 mg/L. High CRP levels have been linked to a greater likelihood of developing atherosclerosis, as the protein contributes to the inflammation of arterial walls (NCBI – CRP and Cardiovascular Disease). Therefore, regular blood tests to monitor CRP are essential for individuals with RA. These tests help healthcare providers assess disease activity and cardiovascular risk, allowing for timely adjustments in treatment plans. By keeping a close watch on CRP levels, both patients and clinicians can better manage inflammation and reduce the long-term risk of heart complications associated with RA.
4. Accelerated Atherosclerosis
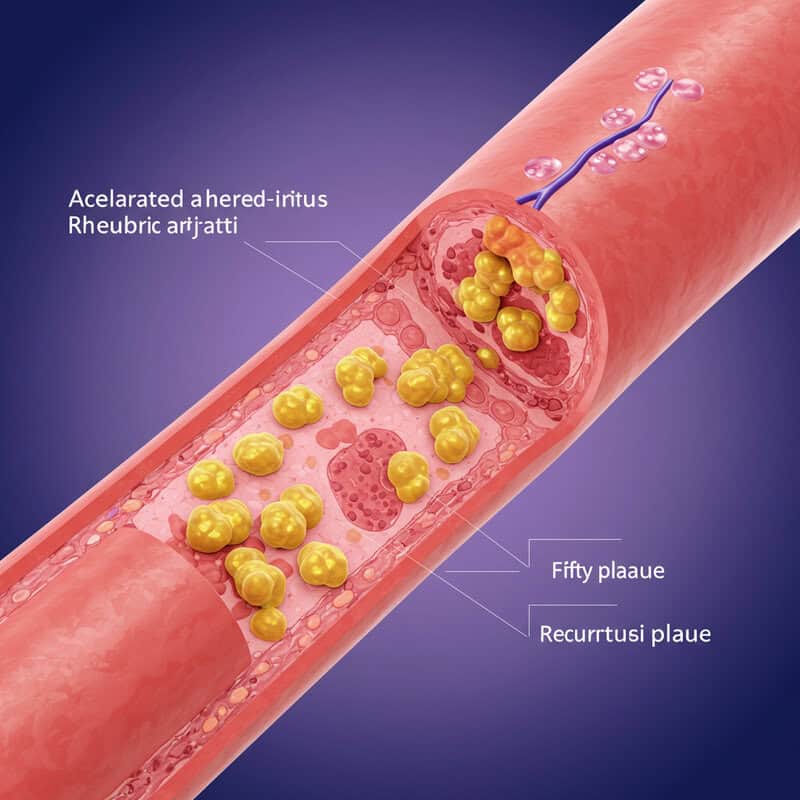
Individuals with rheumatoid arthritis (RA) face a heightened risk of developing atherosclerosis, the buildup of fatty plaques within the arteries. Chronic inflammation in RA accelerates this process, causing arterial walls to become inflamed and more susceptible to damage. Over time, cholesterol and other substances accumulate at these sites of injury, forming plaques that narrow and stiffen the arteries (AHA Journals – Inflammation and Atherosclerosis). Compared to people without RA, those with the condition often develop atherosclerosis earlier and progress more rapidly, leading to an increased risk of heart attack, stroke, and other cardiovascular complications (NIH – RA and Cardiovascular Disease). This difference persists even when traditional risk factors such as age, smoking, and high blood pressure are accounted for. Because of the accelerated nature of atherosclerosis in RA, regular cholesterol screening is vital. Monitoring cholesterol levels allows for early identification of lipid abnormalities and timely intervention, such as dietary modifications, exercise, and medication when necessary. Proactive management of cholesterol, alongside inflammation control, is essential for reducing cardiovascular risks in people living with RA.
5. Endothelial Dysfunction
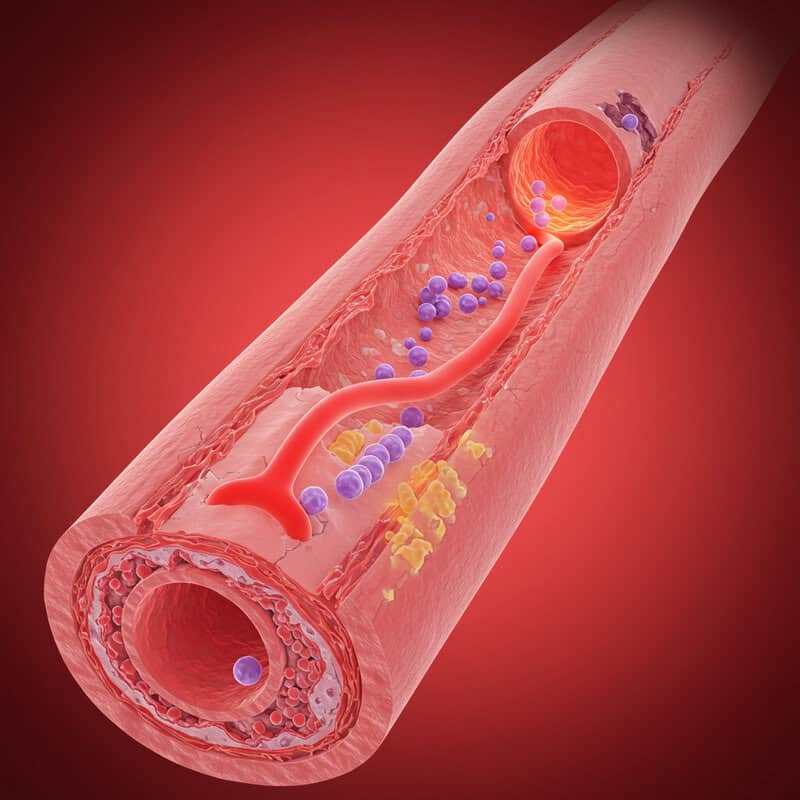
The endothelium is the thin, delicate lining on the inside of blood vessels, playing a crucial role in maintaining vascular health by regulating blood flow, clotting, and immune function. In rheumatoid arthritis (RA), persistent inflammation damages the endothelium, leading to a condition known as endothelial dysfunction (NIH – Endothelial Dysfunction in RA). This dysfunction is one of the earliest indicators of heart disease, as it impairs the vessels’ ability to dilate, increases the risk of clot formation, and promotes the buildup of atherosclerotic plaques. Even before overt cardiovascular symptoms arise, endothelial dysfunction can silently contribute to the progression of heart disease in people with RA. Research shows that RA patients display worse endothelial function than healthy individuals, independent of traditional cardiovascular risk factors (AHA Journals – Endothelial Dysfunction and RA). To support vascular health, individuals with RA are encouraged to adopt lifestyle changes such as regular physical activity, a balanced diet rich in fruits and vegetables, smoking cessation, and stress management. These measures, combined with effective RA treatment, can help preserve endothelial function and reduce cardiovascular risk.
6. Increased Risk of Heart Attack
People living with rheumatoid arthritis (RA) are at a significantly increased risk of myocardial infarction, commonly known as a heart attack. Studies have shown that individuals with RA are up to twice as likely to experience a heart attack compared to those in the general population, even after accounting for traditional risk factors like high blood pressure and smoking (AHA Journals – RA and Increased Cardiovascular Risk). Chronic inflammation accelerates the formation of atherosclerotic plaques, which are more likely to rupture and cause blood clots that block coronary arteries. Additionally, the inflammatory environment in RA can make these heart attacks more severe and harder to treat (NIH – Cardiovascular Disease in RA). Because symptoms of heart attack may sometimes be atypical in RA patients—such as shortness of breath, fatigue, or discomfort rather than classic chest pain—it is crucial for both patients and healthcare providers to respond promptly to any concerning symptoms. Rapid medical attention can be life-saving, and education about heart attack warning signs should be an integral part of RA management strategies.
7. Stroke Risk and RA
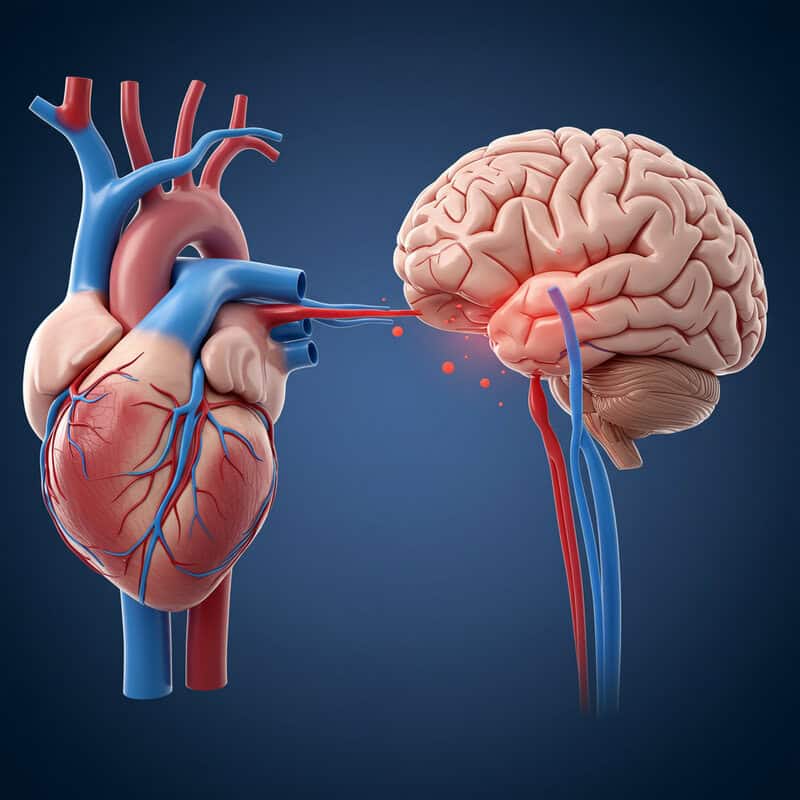
Rheumatoid arthritis (RA) not only increases the risk of heart attack but is also associated with a heightened likelihood of stroke. Research indicates that individuals with RA have a 30-60% higher risk of stroke compared to the general population, especially ischemic strokes caused by blocked blood vessels in the brain (NIH – Stroke and RA). Chronic systemic inflammation in RA accelerates atherosclerosis and contributes to other stroke risk factors, including high blood pressure and atrial fibrillation. A population-based study in Sweden found that people with RA had a significantly higher incidence of stroke than those without RA, underscoring the importance of targeted prevention and management (Annals of the Rheumatic Diseases – Stroke in RA). Regular monitoring and control of blood pressure are essential for reducing stroke risk in RA patients. Blood pressure should be checked at every medical visit, and individuals are encouraged to use home blood pressure monitors for ongoing assessment. Collaborative care between rheumatologists and primary care physicians ensures comprehensive risk management and early intervention, which can help minimize stroke risk in this vulnerable population.
8. Heart Failure Concerns
Patients with rheumatoid arthritis (RA) are at an elevated risk for developing heart failure, which occurs when the heart is unable to pump blood effectively to meet the body’s needs. Chronic inflammation in RA contributes to changes in the heart muscle and blood vessels, leading to both systolic and diastolic dysfunction (Cleveland Clinic – RA and Heart Failure). For example, a middle-aged woman with long-standing RA may present with increasing fatigue, swelling in the legs, and shortness of breath upon exertion. Upon evaluation, she is diagnosed with heart failure, despite having no prior history of coronary artery disease. This scenario illustrates how RA can independently promote heart failure, even in the absence of traditional cardiac risk factors (NIH – Heart Failure in RA). The symptoms of heart failure—including shortness of breath, fatigue, and swelling—should never be ignored by RA patients. Early recognition and reporting of these symptoms are crucial, as prompt intervention can slow disease progression and improve quality of life. Regular cardiovascular assessment is recommended to monitor heart function in individuals with RA.
9. Traditional Risk Factors Compound
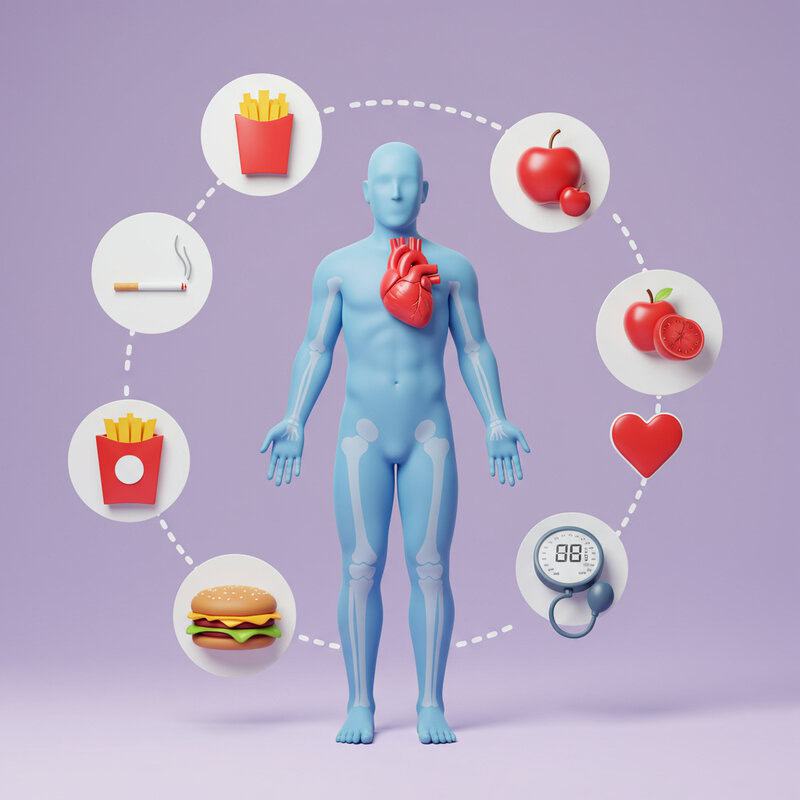
While rheumatoid arthritis (RA) itself heightens cardiovascular risk, traditional factors such as smoking, obesity, and hypertension further amplify this danger. Studies show that the combined presence of RA and these modifiable risks can lead to a disproportionately higher rate of heart disease compared to people without RA (NIH – Cardiovascular Risk Factors in RA). For example, a smoker with RA faces a much greater risk of heart attack than a smoker without RA, as inflammation from both sources damages blood vessels synergistically. Obesity exacerbates inflammation and strains the cardiovascular system, while high blood pressure directly injures arteries, enhancing plaque buildup. Research underscores that the prevalence of these risk factors is often higher among individuals with RA than in the general population (AHA Journals – Traditional Risk Factors in RA). Addressing modifiable risks is crucial: quitting smoking, achieving a healthy weight, and maintaining blood pressure within target ranges can all lower the risk of heart complications. Integrating lifestyle changes and medical management offers the best chance to reduce compounded cardiovascular threats in those living with RA.
10. Role of RA Medications
Medications used to treat rheumatoid arthritis (RA) can have varying effects on heart health. Biologic drugs, such as tumor necrosis factor (TNF) inhibitors, have been shown to reduce systemic inflammation and may lower the risk of cardiovascular events in some patients (American College of Rheumatology – Biologics and Heart Risk). In contrast, long-term use of corticosteroids, while effective in controlling RA flares, can increase blood pressure, raise cholesterol, and elevate blood sugar, all of which contribute to higher cardiovascular risk (Verywell Health – RA Medications and Heart Risk). Nonsteroidal anti-inflammatory drugs (NSAIDs) may also pose additional risks for heart disease, particularly when used over extended periods. Methotrexate, a commonly prescribed disease-modifying antirheumatic drug (DMARD), has been associated with a reduction in cardiovascular events, likely due to its anti-inflammatory properties. Because medication effects can differ greatly between individuals, it is essential to discuss all options with a healthcare provider. Together, patients and providers can weigh the benefits and risks of each medication, aiming for optimal RA control while minimizing negative impacts on cardiovascular health.
11. Corticosteroids and Cardiovascular Effects

Long-term use of corticosteroids, such as prednisone, is common in the management of rheumatoid arthritis (RA) flares but comes with significant cardiovascular risks. Corticosteroids can induce hypertension by promoting sodium and water retention, and they may also elevate cholesterol and triglyceride levels, both of which are key contributors to atherosclerosis (NIH – Glucocorticoid Effects on Cardiovascular Risk). Research comparing RA patients who use corticosteroids with those who do not consistently finds higher rates of high blood pressure and adverse lipid profiles among long-term steroid users (Annals of the Rheumatic Diseases – Steroid Use and Heart Risk). These side effects compound the already increased risk of cardiovascular disease in RA, making careful medication management essential. Clinical guidelines recommend using the lowest effective corticosteroid dose for the shortest duration possible to control symptoms. Regular monitoring of blood pressure and cholesterol is advised for anyone taking these medications. By minimizing exposure and focusing on alternative therapies when appropriate, healthcare providers can help patients achieve RA control while reducing the risk of serious cardiovascular complications.
12. Methotrexate and Heart Protection

Methotrexate, a cornerstone disease-modifying antirheumatic drug (DMARD) for rheumatoid arthritis (RA), offers benefits that may extend beyond joint protection. Evidence suggests that methotrexate is associated with a reduced risk of cardiovascular events in RA patients. A major meta-analysis published in the American Journal of Cardiology found that methotrexate use was linked to a 21% lower risk of cardiovascular disease among individuals with RA compared to those not taking the drug (American Journal of Cardiology – Methotrexate and Cardiovascular Risk). This protective effect is believed to result from methotrexate’s ability to lower systemic inflammation, which is a key driver of both joint and cardiovascular damage in RA. Methotrexate may also improve endothelial function and decrease levels of harmful inflammatory cytokines. Adhering to prescribed methotrexate regimens is essential for maximizing these benefits. Patients should take the medication as directed and attend regular follow-up appointments to monitor for side effects and assess treatment effectiveness. Open communication with healthcare providers can ensure that methotrexate therapy is optimized for both joint health and cardiovascular protection.
13. Biologic Therapies and Cardiac Outcomes

Biologic therapies, particularly tumor necrosis factor (TNF) inhibitors, have revolutionized the treatment of rheumatoid arthritis (RA) and may also influence heart health. TNF inhibitors, such as etanercept and adalimumab, target specific inflammatory pathways, reducing systemic inflammation that contributes to both joint damage and cardiovascular disease. Several studies suggest that TNF inhibitors are associated with a decreased risk of heart attacks and strokes in RA patients compared to those not using these medications (BMJ – TNF Inhibitors and Cardiovascular Risk). Other biologic classes, like interleukin-6 (IL-6) inhibitors and B-cell depleting agents, are also used in RA management, but their long-term cardiac effects are less well understood. Some research indicates that these agents may provide similar cardiovascular benefits, though more studies are needed for definitive conclusions (JACC – Biologics and Cardiovascular Outcomes). Regardless of the biologic class, regular cardiovascular monitoring is essential for all RA patients. This includes routine assessments of blood pressure, cholesterol, and heart function to promptly identify any emerging cardiac issues. Collaboration between rheumatologists and cardiologists ensures optimal management of both RA and heart health.
14. NSAIDs—Relief but Risks
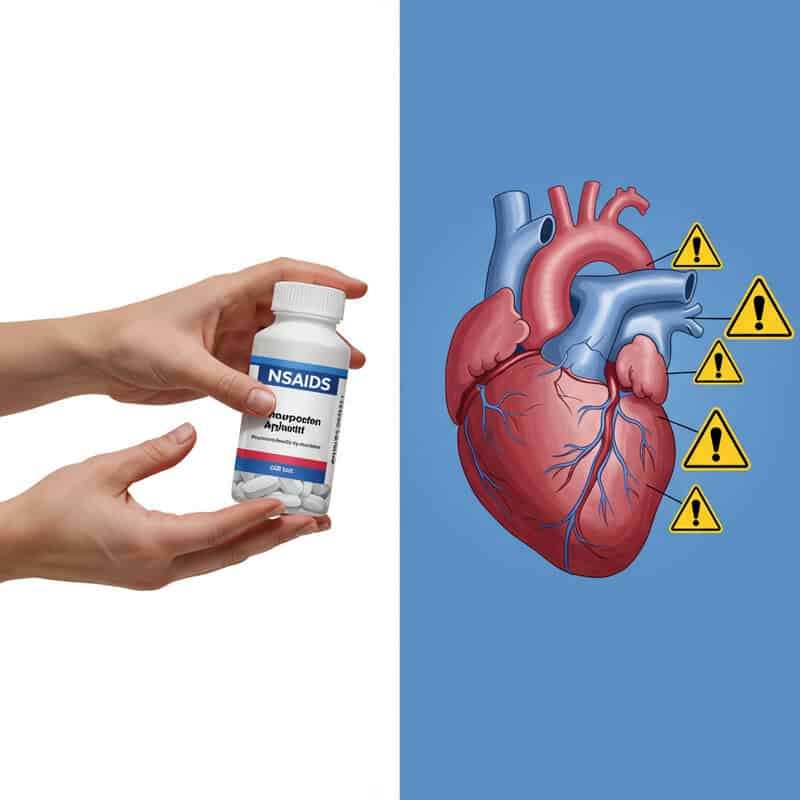
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are commonly used to relieve pain and inflammation in rheumatoid arthritis (RA). However, frequent or long-term NSAID use is associated with an increased risk of cardiovascular events, including heart attack and stroke (FDA – NSAID Heart Risk Warning). A high-profile example involved the withdrawal of rofecoxib (Vioxx) from the market in 2004 after studies revealed a significant increase in heart attacks among its users (NIH – Vioxx Withdrawal and Cardiovascular Risk). NSAIDs may raise blood pressure, cause fluid retention, and adversely affect the lining of blood vessels, compounding pre-existing cardiovascular risks in RA patients. Because of these concerns, healthcare providers recommend that NSAIDs be used at the lowest effective dose for the shortest possible duration. Patients with a history of cardiovascular disease or risk factors should discuss alternatives for pain management with their healthcare providers. Regular monitoring and open communication are crucial to balance the benefits of symptom relief with the potential for serious heart-related side effects.
15. Lipid Profile Changes in RA
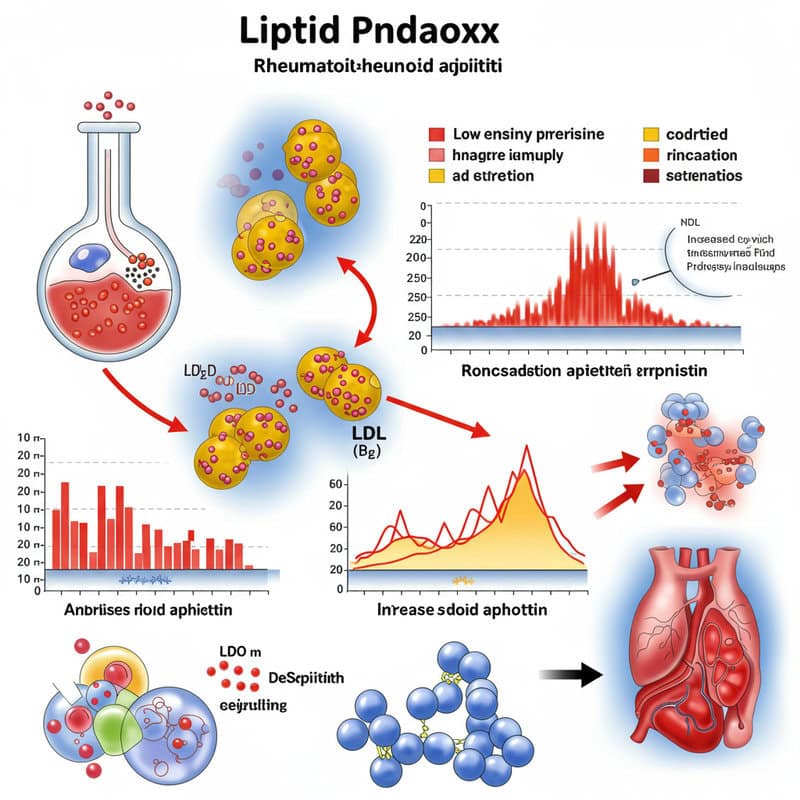
Rheumatoid arthritis (RA) can significantly alter lipid profiles, contributing to a unique cardiovascular risk known as the “lipid paradox.” During active inflammation, RA patients often have lower total cholesterol and low-density lipoprotein (LDL) levels, but these changes do not equate to reduced heart risk. Instead, the composition and function of cholesterol particles may become more atherogenic, increasing cardiovascular risk despite seemingly favorable numbers (NIH – Lipid Paradox in RA). For example, a patient with RA may see their LDL drop from 120 mg/dL to 90 mg/dL during a disease flare, while high-density lipoprotein (HDL) also falls, and inflammation makes LDL particles more likely to promote plaque buildup. As inflammation subsides with effective treatment, cholesterol values often return to pre-RA levels, but heart risk may remain elevated. For these reasons, annual lipid panels are strongly recommended for people with RA, regardless of their apparent cholesterol status (Arthritis Foundation – Cholesterol and RA). Regular monitoring enables timely intervention, such as lifestyle changes or statin therapy, to address evolving cardiovascular risks in this population.
16. Homocysteine and Vascular Damage
Homocysteine is an amino acid found in the blood, and elevated levels have been linked to an increased risk of cardiovascular disease. In individuals with rheumatoid arthritis (RA), studies reveal that homocysteine levels are frequently higher than in healthy populations, contributing to blood vessel injury and promoting atherosclerosis (NIH – Homocysteine in RA and Cardiovascular Risk). Elevated homocysteine damages the endothelium, the delicate lining of blood vessels, and encourages the formation of blood clots—both critical factors in the development of heart disease and stroke. Comparatively, RA patients may have mean homocysteine values of 15 micromoles/L, while healthy individuals typically have values below 10 micromoles/L. Some RA medications, such as methotrexate, can further increase homocysteine, making monitoring especially important. B-vitamin supplementation, particularly folic acid and vitamin B12, has been shown to lower homocysteine levels and may help mitigate vascular damage (Arthritis Foundation – B Vitamins and RA). Healthcare providers often recommend regular screening and appropriate supplementation as part of a comprehensive cardiovascular prevention strategy for people with RA.
17. Anemia and Heart Strain
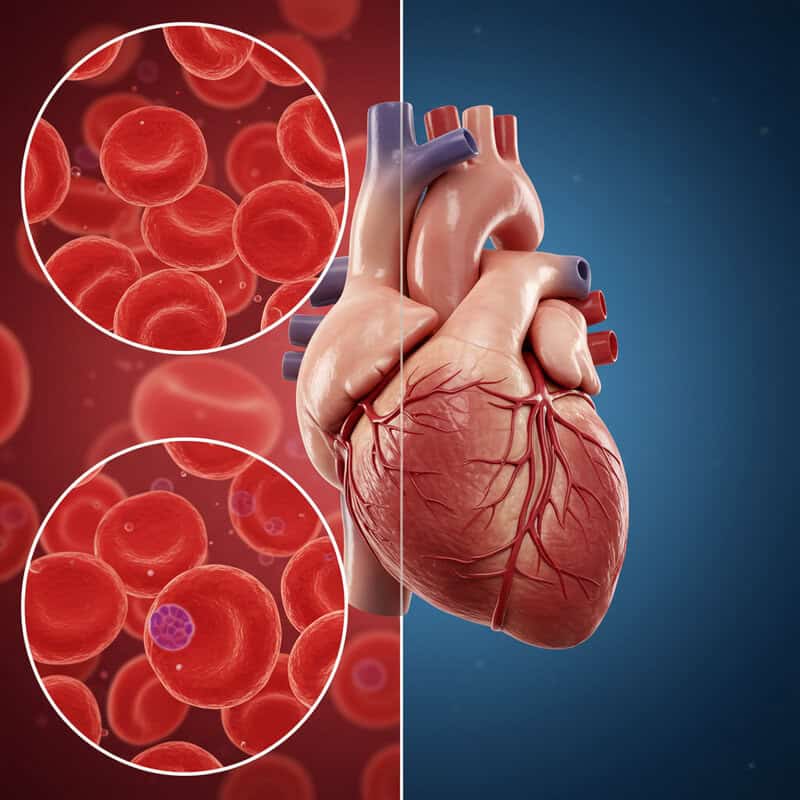
Anemia, characterized by a low red blood cell count or reduced hemoglobin, is a frequent complication in rheumatoid arthritis (RA) due to chronic inflammation and, occasionally, medication side effects. This condition reduces the oxygen-carrying capacity of the blood, forcing the heart to pump harder and faster to meet the body’s oxygen demands (NIH – Anemia in RA). Over time, this extra strain can contribute to enlargement of the heart and exacerbate existing cardiovascular problems. For example, an individual with RA may notice increasing fatigue and shortness of breath with minimal activity. Upon evaluation, their hemoglobin is found to be 9 g/dL, well below the normal range, suggesting anemia as a contributing factor to their symptoms. Persistent anemia not only worsens quality of life but can also accelerate heart failure and increase the risk of cardiac events. It is essential for people with RA to report new or worsening fatigue, dizziness, or palpitations to their healthcare providers. Regular blood tests to monitor for anemia, coupled with appropriate treatment, can help protect heart health and improve overall well-being in RA patients (Arthritis Foundation – Anemia and Arthritis).
18. RA Flares and Acute Cardiac Events
Rheumatoid arthritis (RA) flares are characterized by sudden increases in joint pain, swelling, and overall inflammation throughout the body. Research has demonstrated that these acute flare-ups are linked to a significantly higher short-term risk of cardiac events, such as heart attacks and strokes, compared to periods of disease remission (NIH – RA Flares and Cardiovascular Events). During a flare, the body’s inflammatory markers, including C-reactive protein (CRP) and interleukins, spike dramatically, increasing the likelihood of plaque rupture and blood clot formation. Comparatively, the risk of acute cardiac events is much lower during remission, when inflammation is well-controlled and the cardiovascular system is under less stress. For example, a patient experiencing a severe flare may develop chest pain or shortness of breath, symptoms that could signify a heart attack precipitated by the inflammatory surge. Prompt recognition and management of RA flares—using medications, rest, and other interventions—are critical for reducing both joint damage and cardiovascular complications. Individuals with RA should report flare symptoms to their healthcare team immediately to facilitate timely treatment and minimize short-term heart risks (Arthritis Foundation – RA Flares).
19. Stress and Heart Rate Variability
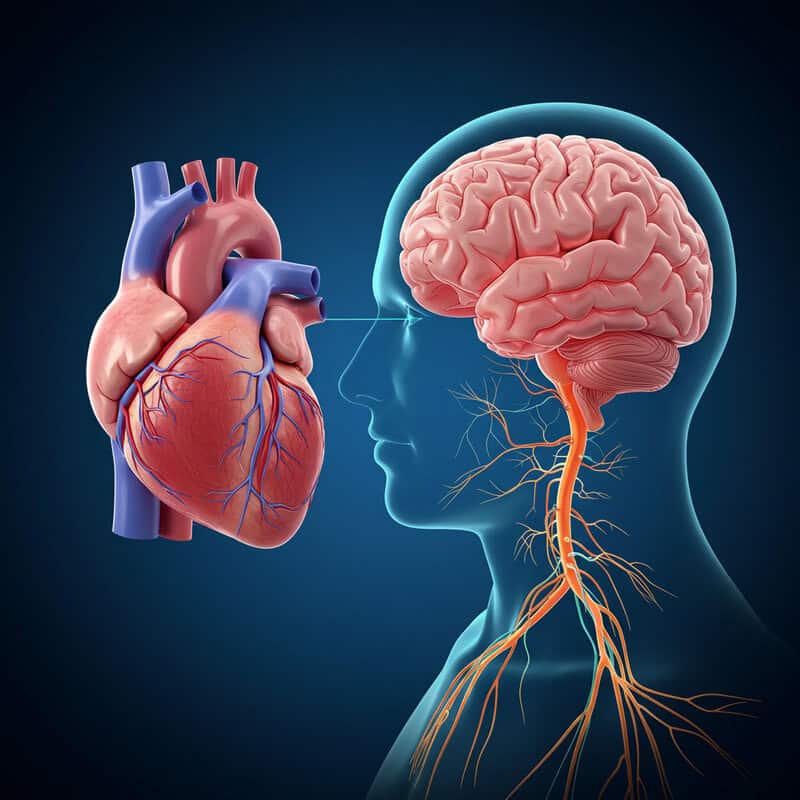
Chronic stress is a common experience for individuals living with rheumatoid arthritis (RA), arising from ongoing pain, disability, and life adjustments. This persistent psychological burden has measurable effects on heart health, particularly heart rate variability (HRV)—a marker of the heart’s ability to adapt to changing demands. Lower HRV, often seen in people with RA, indicates reduced autonomic nervous system flexibility and is associated with higher cardiovascular risk (NIH – Stress, HRV, and RA). In contrast, individuals in stress-free or well-managed states generally exhibit higher HRV, reflecting better cardiovascular resilience and lower risk for adverse events. Chronic stress in RA leads to sustained elevations in stress hormones such as cortisol and adrenaline, which can negatively affect heart rate patterns, blood pressure, and inflammation. To counteract these effects, healthcare professionals recommend mindfulness practices—including meditation, deep breathing, and yoga—which have been shown to improve HRV and reduce stress in RA patients (Arthritis Foundation – Mindfulness Meditation). Incorporating stress management techniques into daily routines can enhance not only emotional well-being but also heart health in those living with RA.
20. Physical Inactivity in RA

Rheumatoid arthritis (RA) often causes pain, stiffness, and fatigue, making regular physical activity challenging for many patients. As a result, limited mobility frequently leads to a sedentary lifestyle, which is a known risk factor for both cardiovascular disease and worsening joint function (NIH – Physical Activity in RA). Studies show that people with RA are significantly less active than the general population, with lower participation in both moderate and vigorous exercises. This inactivity not only increases the risk of heart disease but can also contribute to muscle loss, reduced range of motion, and further joint deterioration. Comparatively, individuals without RA are more likely to meet recommended guidelines for physical activity, benefiting from better cardiovascular and musculoskeletal health. Healthcare professionals strongly encourage gentle forms of exercise—such as walking, swimming, or yoga—for those with RA. These low-impact activities can help maintain joint flexibility, reduce inflammation, and improve heart health without exacerbating joint pain. Customizing exercise plans to individual abilities and flare status ensures safety and maximizes benefits. Regular, gentle movement is a crucial component of comprehensive RA care, supporting both joint function and cardiovascular well-being (Arthritis Foundation – Physical Activity).
21. Obstructive Sleep Apnea Prevalence

Obstructive sleep apnea (OSA) is notably more prevalent among individuals with rheumatoid arthritis (RA) compared to the general population. Studies estimate that up to 30% of RA patients may experience some form of sleep-disordered breathing, which is significantly higher than rates seen in healthy cohorts (NIH – Sleep Apnea and RA). OSA is characterized by repeated interruptions in breathing during sleep, leading to drops in oxygen levels and fragmented rest. This condition is strongly linked to the development of heart arrhythmias, high blood pressure, and other cardiovascular complications. In people with RA, OSA can worsen inflammation and further elevate heart risk. Persistent daytime fatigue, morning headaches, and loud snoring are common symptoms that may go overlooked or be attributed to RA itself. For those experiencing ongoing fatigue despite well-controlled RA, healthcare providers recommend sleep studies to evaluate for OSA (Arthritis Foundation – Arthritis and Sleep). Early diagnosis and treatment—such as with continuous positive airway pressure (CPAP) therapy—can improve sleep quality, reduce cardiovascular risk, and enhance overall quality of life for people with RA.
22. Gender Differences in Risk
Women constitute the majority of rheumatoid arthritis (RA) patients and experience unique cardiovascular risks compared to men. Research indicates that women with RA have a higher relative risk of heart disease than women without RA, and the increase in risk is often greater than that seen in men with the disease (NIH – Gender Differences in Cardiovascular Risk in RA). Factors such as hormonal differences, age at disease onset, and the increased prevalence of other autoimmune conditions in women may contribute to this disparity. Furthermore, women are more likely than men to present with atypical symptoms of heart disease, such as fatigue, shortness of breath, or indigestion, rather than classic chest pain. These subtler presentations can lead to delayed diagnosis and treatment. Men with RA also face elevated cardiovascular risk, but the relative impact of RA on heart health is especially pronounced in women. This underscores the need for tailored cardiovascular screening and preventive care for women with RA, including regular monitoring of blood pressure, cholesterol, and heart function. Clinicians should maintain a high index of suspicion for heart disease in female RA patients, even when symptoms are nonspecific (Arthritis Foundation – Heart Disease in Women with RA).
23. Age and Cumulative Risk
The cumulative impact of rheumatoid arthritis (RA) on cardiovascular health increases with age and disease duration. The longer an individual lives with RA, the greater the lifetime exposure to systemic inflammation, which steadily raises the risk of heart disease and stroke (NIH – Age and Cardiovascular Risk in RA). Studies show that older adults with RA have a substantially higher incidence of cardiovascular events compared to both younger RA patients and age-matched individuals without RA. For example, people over 65 with longstanding RA may experience heart attack and stroke rates similar to or higher than those of the general population a decade older. In contrast, younger individuals with early RA still face elevated risk, but it is not as pronounced as in older age groups. This highlights the importance of early and proactive prevention strategies—such as aggressive inflammation control, heart-healthy lifestyle modifications, and regular risk factor screening—from the time of diagnosis. Initiating preventive measures early in the RA disease course can help slow the progression of cumulative cardiovascular risk and improve long-term outcomes (Arthritis Foundation – Heart Disease and Arthritis).
24. Family History and Genetics
Genetics play a significant role in the development of both rheumatoid arthritis (RA) and heart disease. Certain genetic markers, such as HLA-DRB1 alleles, are associated with increased susceptibility to RA and may also contribute to a higher risk of cardiovascular disease (NIH – Genetics of RA and Heart Disease). Family history often reveals patterns where multiple relatives are affected by RA, heart disease, or both. For example, consider a family in which a mother and daughter both have RA and a strong history of early heart attacks among close relatives. Such clustering suggests an inherited predisposition to inflammation and vascular problems. Research confirms that first-degree relatives of RA patients have an elevated risk for both autoimmune and cardiovascular conditions compared to the general population. For families with a pronounced history, genetic counseling can provide valuable insights into individual and familial risk, helping guide early screening and tailored preventive strategies (American College of Rheumatology – Genetics and RA). Understanding genetic risk empowers families to engage in proactive health management, including lifestyle changes and regular cardiovascular assessments for at-risk members.
25. Ethnic and Racial Disparities

Significant disparities exist in the prevalence, severity, and outcomes of rheumatoid arthritis (RA) and related cardiovascular disease across different ethnic and racial groups. Research shows that African American, Hispanic, and Native American populations not only have higher rates of RA but also experience worse cardiovascular outcomes compared to White patients (NIH – Racial Disparities in RA). For example, a study found that African American individuals with RA are more likely to develop heart failure and have higher mortality rates from cardiovascular disease than their White counterparts. Hispanic patients often face barriers to early diagnosis and treatment, leading to advanced disease at presentation and greater heart risk. Native American populations demonstrate some of the highest rates of both RA and heart disease, compounded by challenges in healthcare access and socioeconomic factors. These disparities are influenced by genetics, environmental exposures, healthcare access, and cultural factors. Addressing them requires culturally sensitive education, improved access to rheumatology and cardiology services, and targeted outreach programs (Arthritis Foundation – Arthritis in Minority Populations). Tailored interventions are crucial to reducing the disproportionate burden of RA and cardiovascular disease among minority groups.
26. Diet Trends and Heart Health in RA

Dietary patterns play a pivotal role in influencing both rheumatoid arthritis (RA) activity and cardiovascular risk. The Mediterranean diet, rich in fruits, vegetables, whole grains, fish, olive oil, and nuts, has been shown to reduce inflammation and lower the risk of heart disease in people with RA (NIH – Mediterranean Diet and RA). Studies demonstrate that RA patients following this eating pattern experience improved joint function and reduced cardiovascular events compared to those consuming a Western diet, which is typically high in red meat, processed foods, sugar, and saturated fats. The Western diet is associated with increased systemic inflammation, higher cholesterol, and a greater risk of atherosclerosis, all of which compound heart risk for RA patients. Anti-inflammatory foods—such as fatty fish (salmon, sardines), leafy greens, berries, and nuts—help reduce inflammatory markers and support vascular health. Conversely, minimizing intake of processed and fried foods, refined sugar, and trans fats is recommended. Adopting a heart-healthy, anti-inflammatory diet can be a powerful adjunct to medical therapy for RA, improving both joint symptoms and long-term cardiovascular outcomes (Arthritis Foundation – Anti-Inflammatory Diet).
27. Omega-3 Fatty Acids Benefits

Omega-3 fatty acids are well-recognized for their dual role in reducing inflammation and supporting cardiovascular health, making them especially beneficial for individuals with rheumatoid arthritis (RA). These healthy fats, primarily found in fatty fish such as salmon, sardines, and mackerel, help decrease the production of inflammatory cytokines and lower levels of C-reactive protein (CRP), a marker of both RA activity and heart risk (NIH – Omega-3s and RA). Clinical trials have shown that regular intake of omega-3s leads to reduced joint pain and stiffness in RA patients, along with improvements in cholesterol profiles and reduced risk of arrhythmias and atherosclerosis. For example, eating two servings of salmon per week or adding chia seeds and walnuts to the diet can significantly boost omega-3 intake. Supplements containing EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are also effective options, especially for those who cannot consume enough omega-3-rich foods. Experts recommend incorporating these sources into the daily diet to maximize anti-inflammatory and heart-protective benefits (Arthritis Foundation – Omega-3 Fatty Acids). Consistent omega-3 consumption is a simple, evidence-based strategy for improving both joint and cardiovascular health in RA.
28. Fiber Intake and Cholesterol
Dietary fiber is essential for heart health, particularly in individuals with rheumatoid arthritis (RA), who are at increased risk for elevated cholesterol and cardiovascular disease. High-fiber diets help lower cholesterol levels by binding to cholesterol in the digestive system and promoting its excretion, thus reducing the buildup of plaque in arteries (NIH – Dietary Fiber and Cholesterol). RA patients who regularly consume fiber-rich meals—such as oatmeal with berries, lentil soups, and salads featuring beans and leafy greens—tend to have lower total and LDL cholesterol compared to those eating low-fiber diets heavy in processed foods and refined grains. For example, a breakfast of whole-grain cereal and fruit provides significantly more fiber than a breakfast of white bread and sugary pastries. In addition to cholesterol-lowering effects, fiber supports gut health and may help lower systemic inflammation, further benefiting people with RA. Health experts recommend a daily fiber intake of at least 25 grams for women and 38 grams for men (Arthritis Foundation – Fiber and Arthritis). Incorporating a variety of whole grains, fruits, vegetables, and legumes into the daily diet can help RA patients achieve these goals and protect both joint and cardiovascular health.
29. Vitamin D and Cardiovascular Risk
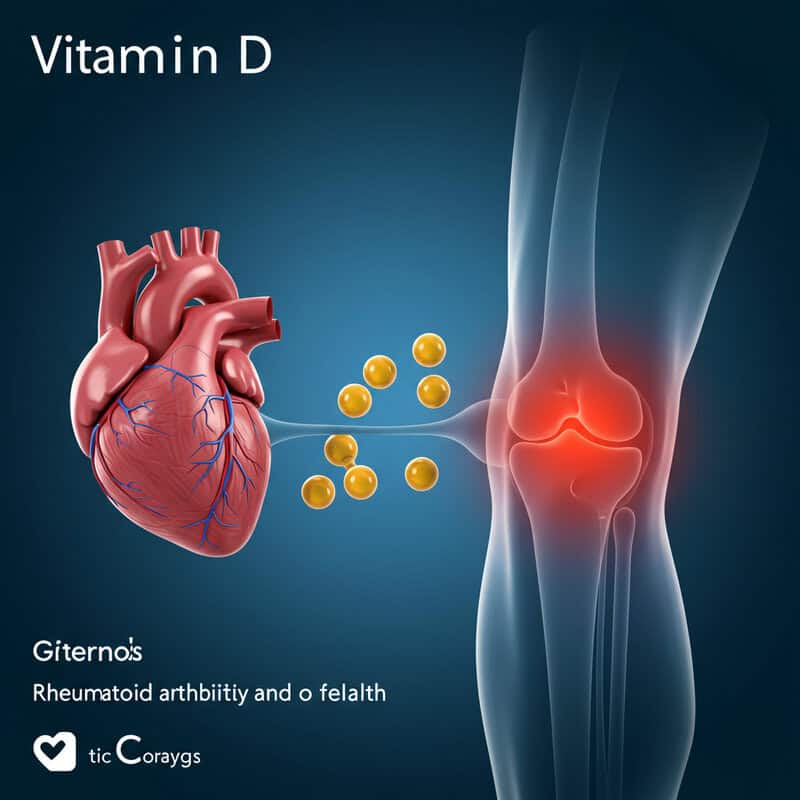
Vitamin D plays a crucial role in both immune regulation and cardiovascular health, and deficiency is common among people with rheumatoid arthritis (RA). Research indicates that low vitamin D levels are associated with increased inflammation, higher disease activity, and a greater risk of cardiovascular events in RA patients (NIH – Vitamin D and Cardiovascular Disease in RA). Vitamin D deficiency can contribute to endothelial dysfunction, hypertension, and atherosclerosis, further compounding existing risks in those with RA. For example, a patient with consistently low vitamin D levels may be advised to take a daily supplement of 1,000 to 2,000 IU or more, depending on their baseline blood levels and physician recommendations. Sun exposure and dietary sources, such as fortified dairy products and fatty fish, can also help maintain adequate vitamin D status. Experts recommend regular blood tests to monitor vitamin D, aiming for levels above 30 ng/mL for optimal health benefits (Arthritis Foundation – Vitamin D and Arthritis). Routine checks and appropriate supplementation are simple yet effective strategies to reduce inflammation and support cardiovascular health in individuals with RA.
30. Alcohol Consumption Patterns
Alcohol consumption has complex effects on both heart health and rheumatoid arthritis (RA) outcomes. Moderate alcohol intake—typically defined as up to one drink per day for women and two for men—has been associated with a lower risk of certain cardiovascular events in the general population and may even have a mild anti-inflammatory effect in some RA patients (NIH – Alcohol, Cardiovascular Disease, and RA). However, heavy or chronic alcohol use reverses these benefits, increasing blood pressure, contributing to abnormal heart rhythms, and raising triglyceride levels. Excessive drinking can also interfere with RA medications, particularly methotrexate, and worsen liver function, compounding health risks. For example, a patient who enjoys a glass of red wine with dinner may experience no adverse effects, while someone who consumes several drinks per day faces heightened risk for both heart complications and RA flare-ups. Health experts consistently advise moderation, emphasizing that individuals with RA should discuss safe alcohol limits with their healthcare provider (Arthritis Foundation – Alcohol and Arthritis). Thoughtful consumption and regular medical guidance can help individuals balance social habits with optimal heart and joint health.
31. Smoking and Double Jeopardy
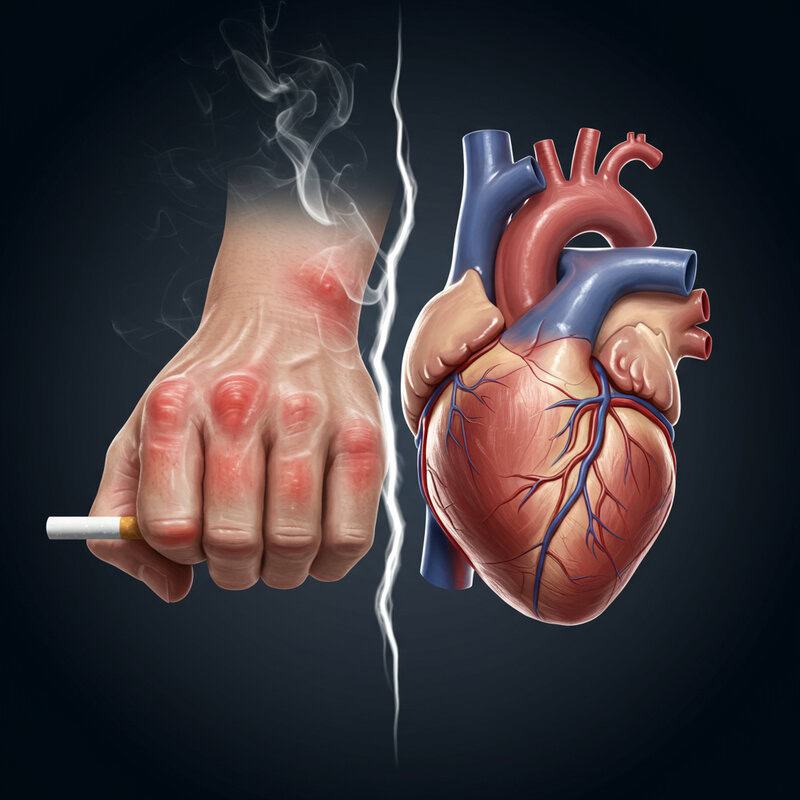
Smoking is a major risk factor for both rheumatoid arthritis (RA) development and progression, as well as for cardiovascular disease. In people with RA, smoking amplifies inflammation, increases disease severity, and reduces the effectiveness of key medications such as methotrexate and biologics (NIH – Smoking, RA, and Cardiovascular Risk). Smokers with RA are significantly more likely to experience heart attacks, strokes, and accelerated atherosclerosis compared to non-smokers. For instance, studies show that RA patients who smoke have up to double the risk of cardiovascular events relative to their non-smoking counterparts, even after adjusting for other risk factors. Smoking also promotes the formation of rheumatoid factor and anti-CCP antibodies, making both RA onset and progression more aggressive. The combination of RA and smoking truly represents a “double jeopardy” for heart health. Healthcare providers strongly urge all individuals with RA to quit smoking and offer support through counseling, medications, and cessation programs. Resources such as the Smokefree.gov website provide valuable tools and guidance. Quitting smoking is one of the most powerful steps RA patients can take to improve both joint and cardiovascular outcomes.
32. Hypertension in RA

Hypertension, or high blood pressure, is notably more prevalent among individuals with rheumatoid arthritis (RA) than in the general population. Studies have found that up to 50% of people with RA develop hypertension, compared to about one-third of adults without RA (NIH – Hypertension in RA). The increased risk is attributed to chronic inflammation, certain RA medications (such as corticosteroids and NSAIDs), and the presence of other cardiovascular risk factors. Unfortunately, blood pressure control rates are often lower in RA patients, with many individuals remaining above target ranges despite treatment. This lack of control further elevates the risk of heart attack, stroke, and heart failure. In comparison, individuals without RA are more likely to achieve blood pressure targets through lifestyle modification and medication adherence. To address this issue, experts recommend regular home blood pressure monitoring for RA patients, in addition to routine checks at medical appointments (Arthritis Foundation – Arthritis and High Blood Pressure). Home monitoring allows for early detection of rising blood pressure and timely adjustments to treatment, helping to reduce the overall cardiovascular burden in people living with RA.
33. Diabetes and Metabolic Syndrome
Rheumatoid arthritis (RA) is associated with a higher risk of developing diabetes and metabolic syndrome—a cluster of conditions including abdominal obesity, high blood pressure, abnormal cholesterol, and elevated blood sugar. Chronic inflammation in RA contributes to insulin resistance, making it more difficult for the body to regulate blood glucose levels (NIH – RA and Diabetes Risk). Studies have shown that people with RA are up to 50% more likely to develop type 2 diabetes compared to those without the disease. Metabolic syndrome is also more prevalent in RA, with research pointing to overlapping inflammatory pathways and shared genetic risk factors. For example, a patient with RA may present with high triglycerides, increased waist circumference, and elevated fasting glucose—hallmarks of metabolic syndrome—raising their cardiovascular risk exponentially. These disease clusters pose a significant challenge, as they mutually reinforce each other’s negative effects on vascular health. Annual blood sugar screening and regular metabolic assessments are recommended for all individuals with RA (Arthritis Foundation – Arthritis and Diabetes). Early identification and treatment of metabolic imbalances are crucial for preventing heart complications and improving long-term outcomes in RA.
34. Obesity’s Dual Burden
Obesity presents a dual challenge for individuals with rheumatoid arthritis (RA), amplifying both joint symptoms and cardiovascular risk. Excess body weight increases systemic inflammation, making RA harder to control and often leading to more severe disease activity (NIH – Obesity and RA). Additionally, obesity is a well-established risk factor for heart disease, contributing to high blood pressure, abnormal cholesterol, and diabetes, all of which are prevalent among RA patients. For example, a person with RA who loses 5-10% of their body weight through a combination of healthier eating and increased physical activity may experience reduced joint pain, improved mobility, and lower blood pressure and cholesterol levels. Gradual weight loss—at a rate of one to two pounds per week—is recommended to ensure sustainable results and to minimize muscle loss. Even modest reductions in weight can significantly lower inflammation and cardiovascular risk. Healthcare professionals advise that weight management programs for RA patients be individualized, accounting for mobility limitations and flare status (Arthritis Foundation – Weight Loss and Arthritis). Achieving and maintaining a healthy weight is a key strategy for improving both joint and heart health in RA.
35. Cholesterol Medications and RA

Statins are the most commonly prescribed cholesterol-lowering medications and are frequently used in individuals with rheumatoid arthritis (RA) who have elevated cholesterol or additional cardiovascular risk factors. Beyond their lipid-lowering properties, statins possess anti-inflammatory effects that may be particularly beneficial for RA patients, helping to reduce systemic inflammation and the risk of atherosclerosis (NIH – Statins in RA). Clinical studies have shown that statin therapy in RA not only lowers LDL cholesterol but may also decrease disease activity and improve vascular health. However, statins can cause side effects, including muscle pain, liver enzyme elevations, and, rarely, increased blood sugar or memory problems. These potential side effects should be weighed against the cardiovascular benefits, especially in RA patients who are already managing multiple medications. Ongoing lipid monitoring—through regular blood tests—is advised to assess treatment effectiveness and detect any adverse reactions early (Arthritis Foundation – Statins and Arthritis). Collaborative care between rheumatologists and primary care providers ensures that statin therapy is optimized for both heart and joint health, with adjustments made as needed based on individual response and tolerability.
36. Aspirin and Cardiovascular Prevention
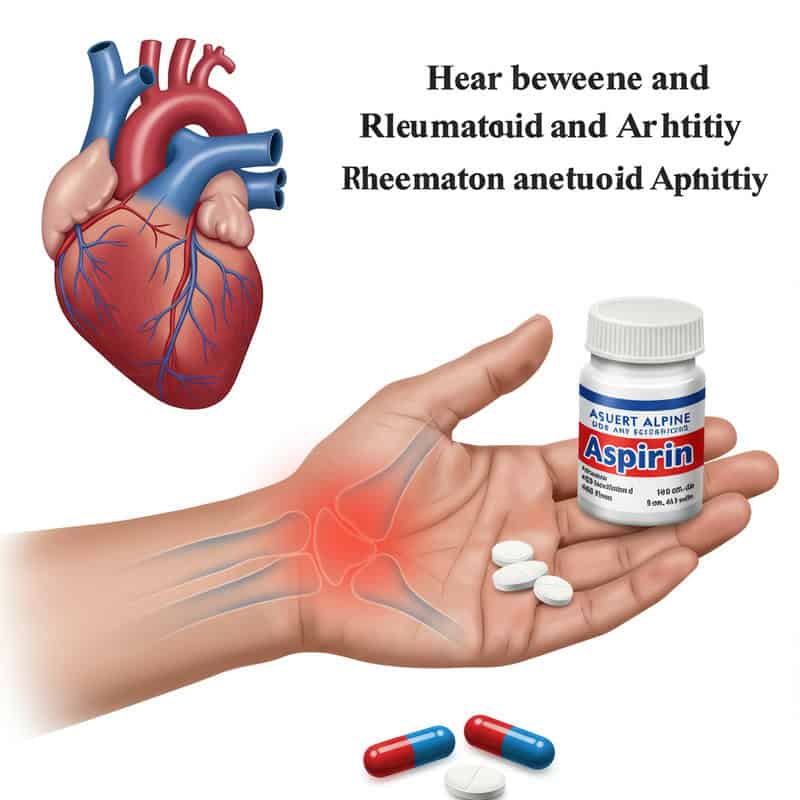
Aspirin has long been used to prevent heart attacks and strokes in high-risk populations, but its role in rheumatoid arthritis (RA) remains debated. While low-dose aspirin can reduce blood clot formation and may lower cardiovascular risk, evidence specific to RA patients is mixed. Some studies suggest that aspirin may provide additional heart protection in RA, particularly for those with a history of cardiovascular events or multiple risk factors (NIH – Aspirin Use in RA). However, other research highlights potential harms, such as gastrointestinal bleeding and increased bleeding risk, especially when combined with corticosteroids or NSAIDs commonly used in RA. Recent guidelines from the American College of Cardiology and American Heart Association recommend aspirin for primary prevention in only select high-risk individuals, while others may not benefit and could be harmed (JACC – 2019 ACC/AHA Guidelines on Aspirin). For RA patients, the decision to use aspirin for cardiovascular prevention should be individualized, taking into account personal and family history, bleeding risk, and concurrent medications. Shared decision-making between patients and healthcare providers ensures that aspirin therapy is tailored to maximize benefits and minimize risks.
37. Blood Clots and Deep Vein Thrombosis
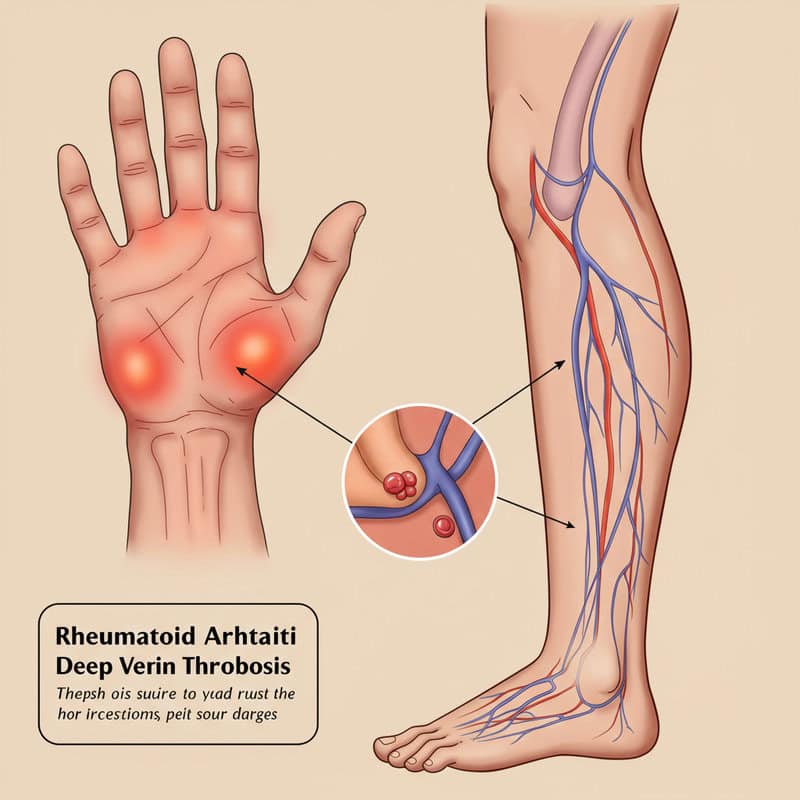
Rheumatoid arthritis (RA) is associated with a heightened risk of developing blood clots, including deep vein thrombosis (DVT) and pulmonary embolism. Chronic inflammation in RA increases the tendency for blood to clot, and certain medications, limited mobility, or recent surgeries can further elevate this risk (NIH – Thrombosis Risk in RA). For example, a patient with RA who experiences prolonged swelling and pain in the calf after a period of immobility may be found to have DVT upon medical evaluation. DVT can lead to life-threatening complications if clots travel to the lungs, causing a pulmonary embolism. Symptoms such as new or unexplained leg swelling, redness, warmth, or pain should prompt immediate medical attention. Because people with RA may not always recognize these signs, healthcare providers emphasize education and vigilance—especially after hospitalization or during periods of decreased physical activity (Arthritis Foundation – Arthritis and Blood Clots). Timely diagnosis and treatment of blood clots, including anticoagulation therapy, are critical to prevent complications and protect cardiovascular health in individuals living with RA.
38. Arrhythmias and Irregular Heartbeats
Rheumatoid arthritis (RA) can increase the risk of developing arrhythmias, or irregular heartbeats, due to persistent inflammation that affects both heart tissue and the electrical conduction system. Studies show that people with RA are more likely to experience atrial fibrillation and other types of arrhythmias than those without the condition (NIH – Arrhythmias in RA). The chronic inflammatory environment in RA can lead to structural changes in the heart, promote fibrosis, and disrupt normal signaling pathways that regulate heart rhythm. For instance, RA patients may have an arrhythmia rate up to 40% higher than age-matched healthy controls. These irregular heartbeats can cause symptoms such as palpitations, dizziness, chest discomfort, or even fainting. Because arrhythmias can increase the risk of stroke and heart failure, it is crucial for individuals with RA to promptly report any new or unusual sensations of rapid, fluttering, or irregular heartbeats to their healthcare provider (Arthritis Foundation – Arthritis and Heart Disease). Early diagnosis and intervention, including medications or rhythm control procedures, can help manage arrhythmias and reduce the risk of complications in RA.
39. Pericarditis in RA
Pericarditis is an inflammation of the pericardium, the thin, protective sac surrounding the heart, and it can occur as an extra-articular manifestation of rheumatoid arthritis (RA). Chronic systemic inflammation in RA may extend to the pericardial lining, leading to fluid accumulation, thickening, and irritation (NIH – Pericarditis in RA). Symptoms of pericarditis include sharp, stabbing chest pain that often worsens with deep breaths or lying down, shortness of breath, and sometimes low-grade fever. Some individuals may feel relief when sitting up or leaning forward. Because chest pain in RA patients can be mistaken for other cardiac or pulmonary conditions, prompt medical evaluation is crucial. Untreated pericarditis may progress to serious complications, such as cardiac tamponade, which is a medical emergency. Diagnosis often involves a physical examination, echocardiography, and other imaging studies to assess pericardial fluid and inflammation. While pericarditis in RA is less common than other heart complications, awareness of its symptoms and risks is essential. Early recognition and treatment—including anti-inflammatory medications or, in severe cases, drainage procedures—can prevent long-term damage and ensure better outcomes (Arthritis Foundation – Pericarditis and Arthritis).
40. Cardiac Imaging in Risk Assessment
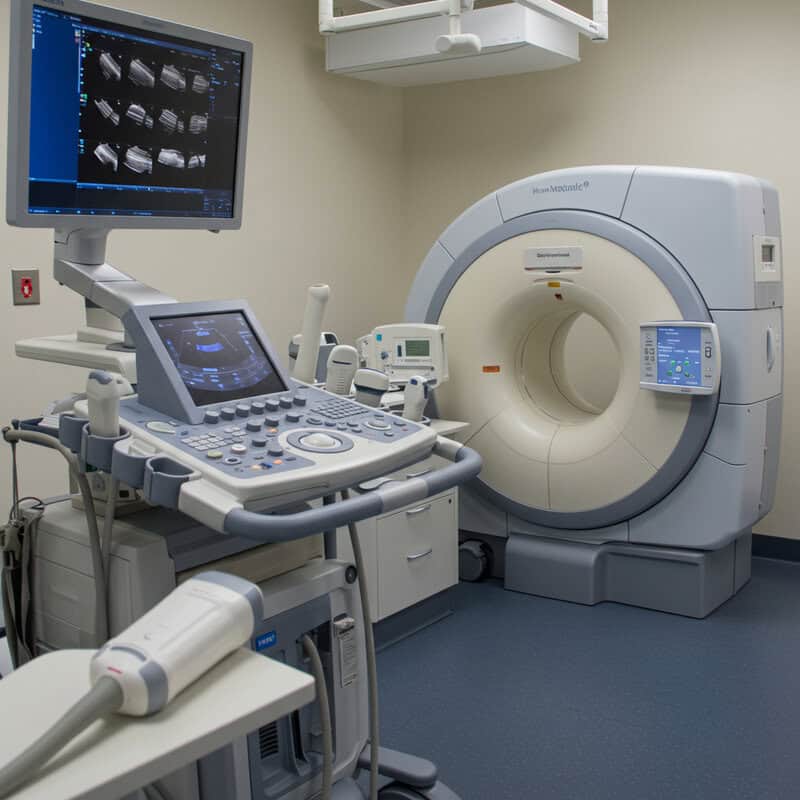
Cardiac imaging plays a vital role in evaluating heart health among individuals with rheumatoid arthritis (RA), who are at increased risk for a variety of cardiovascular complications. Echocardiograms—ultrasound scans that visualize the heart’s structure and function—are commonly used to assess issues such as heart failure, pericarditis, and valve abnormalities in RA patients. In addition to echocardiography, advanced imaging modalities like cardiac MRI and CT angiography provide detailed information about heart tissue, blood flow, and the presence of atherosclerotic plaques (NIH – Cardiac Imaging in RA). These tools are often more sensitive than traditional chest X-rays or electrocardiograms (EKGs) and can detect early or subtle changes that may not yet cause symptoms. For example, cardiac MRI is especially useful for identifying inflammation, fibrosis, or scarring within the heart muscle. Healthcare providers may recommend cardiac imaging for RA patients who develop unexplained symptoms such as chest pain, shortness of breath, palpitations, or persistent fatigue. Early and accurate diagnosis allows for prompt intervention and tailored management of both RA and cardiovascular complications (Arthritis Foundation – Arthritis and Heart Disease).
41. Carotid Ultrasound for Early Detection

Carotid ultrasound is a non-invasive imaging technique used to detect plaque buildup and narrowing in the carotid arteries, which supply blood to the brain. For individuals with rheumatoid arthritis (RA), this tool is particularly valuable, as they are at increased risk for atherosclerosis and stroke even at younger ages (NIH – Carotid Ultrasound in RA). Unlike routine blood tests or physical exams, carotid ultrasound can visualize early signs of plaque formation before symptoms occur, offering a window into vascular health. Studies show that RA patients are more likely to have carotid plaque and increased intima-media thickness compared to healthy controls, even when they lack conventional cardiovascular risk factors. Routine carotid ultrasound screening is not recommended for the general population, but it may be justified in high-risk RA patients—such as those with longstanding disease, multiple risk factors, or a family history of early cardiovascular events. Detecting subclinical atherosclerosis through carotid ultrasound enables earlier intervention with lifestyle changes or medication, potentially reducing the risk of stroke and other complications (Arthritis Foundation – Arthritis and Stroke).
42. Exercise Prescription in RA

Safe and effective exercise is a cornerstone of comprehensive care for rheumatoid arthritis (RA), offering substantial benefits for both joint and heart health. Inactive RA patients are more likely to experience deconditioning, muscle weakness, reduced range of motion, and increased cardiovascular risk compared to their more active counterparts (NIH – Exercise in RA). Studies consistently show that RA patients who engage in regular, low-impact physical activity—such as walking, swimming, cycling, or gentle yoga—enjoy improved mobility, less pain, better mood, and lower rates of heart disease. In contrast, those who remain sedentary often contend with increased inflammation, weight gain, and higher blood pressure. Exercise prescriptions for RA should be individualized, taking into account the patient’s disease activity, joint status, and overall fitness. A tailored activity plan, developed in collaboration with a physical therapist or exercise specialist, may include aerobic activity, flexibility training, and muscle strengthening exercises. Short, frequent sessions are encouraged, with adjustments during disease flares. The Arthritis Foundation provides resources and guidance for safe exercise routines (Arthritis Foundation – Exercise and RA). With the right approach, most individuals with RA can safely incorporate movement into their daily lives.
43. Stress Management Techniques

Effective stress management is crucial for individuals with rheumatoid arthritis (RA), as chronic stress can worsen inflammation, exacerbate pain, and increase cardiovascular risk. Research shows that RA patients who regularly practice stress reduction techniques enjoy better disease control, less fatigue, and improved heart health compared to those who do not engage in such practices (NIH – Stress Management in RA). Without stress management, patients may experience more frequent flares, higher inflammatory markers, and greater emotional distress. Practical strategies for reducing stress in RA include mindfulness meditation, deep breathing exercises, gentle yoga, tai chi, and progressive muscle relaxation. Engaging in enjoyable hobbies, maintaining social connections, and seeking support from therapists or support groups also play important roles in emotional well-being. Even simple routines—such as taking daily walks in nature or listening to calming music—can provide significant relief. The Arthritis Foundation offers resources and guided exercises for stress management (Arthritis Foundation – Stress Reduction Tips). By incorporating stress reduction into daily routines, individuals with RA can help break the cycle of inflammation and support both joint and cardiovascular health.
44. Sleep Hygiene and Heart Health

Good sleep hygiene is essential for managing rheumatoid arthritis (RA) and reducing cardiovascular risk. People with RA often struggle with sleep disturbances due to pain, stiffness, or medication side effects, which can impair immune function, raise blood pressure, and increase systemic inflammation (NIH – Sleep and RA). Studies show that RA patients with poor sleep quality experience more frequent disease flares, higher levels of fatigue, and worse heart health compared to those who achieve restorative rest. In contrast, individuals who maintain consistent, high-quality sleep routines report less pain, better mood, and improved cardiovascular markers such as lower blood pressure and reduced inflammation. Recommended bedtime routines for RA patients include establishing a regular sleep schedule, limiting screen time before bed, practicing relaxation techniques, and creating a comfortable, quiet sleep environment. Avoiding caffeine and heavy meals in the evening, as well as managing pain symptoms before bedtime, can also promote better sleep. The Arthritis Foundation – Sleep Tips provides additional resources. Prioritizing sleep hygiene is a simple yet powerful way to support joint function, mood, and heart health in people with RA.
45. Regular Health Checkups
Ongoing medical evaluations are fundamental for individuals with rheumatoid arthritis (RA) to effectively manage both joint and cardiovascular health. Regular checkups enable early detection of complications, timely adjustment of therapies, and close monitoring of disease progression. Compared to the general population, RA patients typically require more frequent health assessments—often every three to six months—especially if their disease is active or if they are on immunosuppressive medications (American College of Rheumatology – Regular Monitoring). In contrast, healthy adults without chronic conditions may only need annual exams. During these visits, it’s important to request key laboratory tests, including complete blood counts (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), lipid profiles, liver and kidney function tests, and blood glucose or HbA1c for diabetes screening. Periodic blood pressure checks and, when indicated, electrocardiograms or imaging studies should also be part of comprehensive care. Proactive communication with healthcare providers about new symptoms—such as chest pain, swelling, or unexplained fatigue—ensures prompt evaluation. The Arthritis Foundation – Checkups for Arthritis offers guidance on preparing for appointments. Adhering to a regular checkup schedule is vital for optimizing long-term outcomes in RA.
46. Vaccination and Infection Risk
Infections pose a particular threat to individuals with rheumatoid arthritis (RA), as both the disease and its treatments can weaken the immune system. Infections—including respiratory illnesses like influenza or pneumonia—are known to trigger inflammation surges that may precipitate acute cardiovascular events such as heart attacks and heart failure (NIH – Infection and Cardiovascular Risk in RA). Studies comparing vaccinated and unvaccinated RA populations reveal that those who receive recommended vaccines experience fewer infections and lower rates of infection-related cardiac complications. Vaccination against influenza, pneumococcus, and even shingles can reduce the risk of severe infection and the consequent inflammatory response that stresses the heart. Additionally, COVID-19 vaccination is especially important for RA patients, who may be at higher risk for severe illness and heart complications. Staying up to date on all age- and risk-appropriate vaccines is a cornerstone of preventive care in RA management. The Arthritis Foundation – Vaccines for Arthritis Patients provides comprehensive information. Discussing vaccination schedules with healthcare providers ensures optimal protection and helps reduce the risk of infection-triggered heart events in individuals with RA.
47. Patient Education and Empowerment

Empowering patients through education is vital for effective management of both rheumatoid arthritis (RA) and cardiovascular risk. Informed patients are more likely to adhere to medications, recognize warning signs, make healthy lifestyle choices, and communicate proactively with their healthcare teams. For example, a successful education program at the Hospital for Special Surgery in New York provided RA patients with workshops on disease management, medication safety, diet, exercise, and heart health. Participants in this program demonstrated improved medication adherence, better self-monitoring of symptoms, and a significant reduction in emergency room visits and disease flares (Hospital for Special Surgery – Patient Education Success). Education also fosters self-advocacy, encouraging patients to ask questions, seek second opinions, and participate actively in shared decision-making. Resources such as the Arthritis Foundation – Self-Advocacy Tips offer practical guidance for navigating the complexities of RA care. By staying informed and engaged, patients can better manage their condition, reduce heart risk, and achieve improved quality of life. Ongoing education and self-empowerment are essential components of comprehensive RA and cardiovascular care.
48. Partnering With a Multidisciplinary Team

Collaborative, multidisciplinary care offers significant advantages for individuals with rheumatoid arthritis (RA), especially given the complex interplay between joint and heart health. In a solo care model, patients may only see a single provider, such as a rheumatologist, who might not have the resources or expertise to address all aspects of cardiovascular risk or related complications. In contrast, team-based care brings together rheumatologists, cardiologists, primary care physicians, nurses, physical therapists, dietitians, and mental health professionals to create an integrated care plan tailored to the patient’s unique needs (NIH – Multidisciplinary Approach in Rheumatology). Studies show that patients managed by multidisciplinary teams experience better disease control, lower rates of cardiovascular events, and improved quality of life compared to those receiving fragmented or solo care. For example, a patient with RA, high blood pressure, and high cholesterol may benefit from seamless coordination between specialists, ensuring medication interactions are minimized and lifestyle interventions are reinforced. The Arthritis Foundation – Arthritis Care Team provides information on building a support network. Seeking comprehensive, team-based care ensures all facets of RA and heart health are addressed, resulting in the best possible outcomes for patients.
49. Clinical Trials and New Research

Ongoing research is continuously expanding our understanding of the complex relationship between rheumatoid arthritis (RA) and cardiovascular disease. Scientists are investigating new medications, lifestyle interventions, and diagnostic methods to reduce heart risk in RA patients. Current clinical trials are exploring the effects of advanced biologic agents, statins, and anti-inflammatory therapies specifically on cardiovascular outcomes in RA populations. For example, the TARGET trial (NCT02832254) is a large, multicenter study examining whether different RA treatments can lower the risk of heart attacks and strokes in patients with moderate to high cardiovascular risk (American College of Rheumatology – TARGET Trial). Participation in clinical trials offers access to cutting-edge therapies, contributes to scientific progress, and may provide more intensive monitoring than standard care. Patients interested in joining a study should discuss options with their healthcare team and review eligibility criteria on resources such as ClinicalTrials.gov. By considering participation in research, individuals with RA can help advance knowledge and improve future care for both themselves and the broader patient community.
50. Advocacy and Raising Awareness

Public awareness and advocacy are critical for promoting early detection, improving care, and reducing the burden of heart disease among people with rheumatoid arthritis (RA). Increased awareness helps patients, families, and healthcare providers recognize the signs of cardiovascular involvement sooner and encourages the adoption of preventive strategies. For example, campaigns by the Arthritis Foundation Advocacy have successfully influenced legislation to increase funding for arthritis research, improve access to medications, and mandate coverage for preventive screenings. These efforts have led to earlier diagnoses and better integrated care for thousands of RA patients (Arthritis Foundation – Our Impact). Community involvement—such as participating in awareness walks, sharing personal stories, or supporting social media campaigns—can amplify the message and foster a supportive environment for those affected. Patients and families are encouraged to engage with local and national advocacy organizations to help shape policy, promote education, and expand research funding. By raising awareness and participating in advocacy, the RA community can drive lasting change, improve health outcomes, and ensure that the link between rheumatoid arthritis and heart health receives the attention and resources it deserves.
Conclusion
The connection between rheumatoid arthritis (RA) and heart health demands urgent attention from patients, families, and healthcare providers alike. Early screening for cardiovascular risk factors, proactive management of inflammation, and regular heart health assessments are essential for reducing complications and improving long-term outcomes (CDC – RA Basics). Practical steps such as scheduling routine checkups, monitoring blood pressure and cholesterol, and discussing warning signs with your care team can make a significant difference. By addressing RA-related heart risks early and consistently, individuals with RA can protect both their joints and their cardiovascular system, leading to a better quality of life. Collaborative care and ongoing awareness remain key to optimal management (Arthritis Foundation – Heart Health).
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





