The Real Reason You Wake Up Tired — And It’s Not Sleep
Every morning, millions wake up feeling drained despite spending hours in bed. Recent data reveals that 63% of adults in the US and 55% in the UK report frequent morning fatigue (Sleep Foundation, BBC). While lack of sleep is often blamed, emerging research points to the pivotal roles of the endocrine and nervous systems in regulating morning energy. Misattributing tiredness to poor sleep alone overlooks these complex biological systems, making true solutions elusive for many.
1. Blood Sugar Fluctuations

Unstable blood sugar levels during the night can significantly impact how rested you feel upon waking. Even if you get adequate sleep, dips and spikes in glucose can leave you feeling groggy and fatigued. Overnight, your body relies on stored glucose to fuel vital functions, and if these reserves are depleted or poorly regulated, the brain and muscles may not receive the energy they need. This process is closely tied to the metabolic system and is especially pronounced in people with diabetes, but even non-diabetics can experience milder forms of nocturnal hypoglycemia.
Warning signs include waking up with headaches, excessive sweating, shakiness, or feeling unusually irritable or anxious. If you notice cravings for sugary foods or caffeine first thing in the morning, your body may be trying to quickly rebalance glucose levels. Monitoring your diet, avoiding high-sugar snacks before bed, and eating complex carbohydrates in the evening can help stabilize overnight blood sugar. For a deeper dive into this topic, the American Diabetes Association offers guidance on managing morning blood sugar, while the Sleep Foundation explains the interplay between nutrition and sleep quality.
2. Poor Sleep Quality (Not Quantity)

Many people believe that spending more hours in bed guarantees feeling refreshed, but sleep quality is often more important than duration. True restorative sleep depends on the body’s ability to cycle through distinct sleep stages, including light, deep, and REM sleep. Disruptions—such as frequent awakenings, restlessness, or an inability to reach deeper sleep stages—can leave you feeling exhausted, even after a full night’s rest.
Individuals with sleep disorders like sleep apnea or insomnia frequently report this phenomenon. They may clock sufficient hours in bed, but interruptions prevent their bodies from reaping the benefits of restorative sleep cycles. You can assess your sleep quality by tracking how often you wake during the night, how quickly you fall asleep, and how rested you feel in the morning. Wearable devices and sleep trackers can provide valuable insights, but keeping a sleep diary is also effective.
The Sleep Foundation provides comprehensive tips on improving sleep quality, while the CDC highlights the importance of sleep hygiene practices. Focusing on consistency, environment, and relaxation routines can help enhance sleep quality beyond mere duration.
3. Chronic Stress Hormones

The body’s stress response system releases hormones like cortisol and adrenaline, which can seriously disrupt restful sleep. Normally, cortisol levels peak in the morning and drop at night, helping you wake up and wind down appropriately. However, chronic stress—from work, personal life, or even excessive screen time—can keep cortisol elevated at night, making it hard to achieve deep, restorative sleep. Adrenaline, the body’s “fight or flight” hormone, can cause sudden awakenings and a racing heart, even in the absence of real danger.
Shift workers provide a compelling case study: irregular schedules and high stress often lead to persistent sleep disturbances and morning fatigue. Research shows that shift workers have higher baseline cortisol and are at increased risk for insomnia and metabolic disorders (NCBI). This demonstrates how stress hormones, when chronically elevated, sabotage the body’s natural sleep/wake cycle.
Managing stress through practices like mindfulness, breathing exercises, and regular physical activity is vital for restoring hormonal balance. Resources from APA and CDC offer guidance on understanding and coping with stress to support better sleep and reduce morning fatigue.
4. Hidden Sleep Apnea

Undiagnosed sleep apnea is a common but often overlooked reason for waking up tired, even after what seems like a full night’s sleep. This condition involves repeated pauses in breathing throughout the night, which can briefly jolt the body out of deep sleep without fully waking you. Unlike simple snoring—which may be harmless—sleep apnea disrupts the restorative functions of sleep, leaving you feeling unrefreshed and sluggish in the morning.
While loud, chronic snoring is a well-known sign, the symptoms of sleep apnea can be subtle. You might experience morning headaches, dry mouth, difficulty concentrating, or unexplained daytime sleepiness. Partners may notice episodes where your breathing stops and restarts, but many sufferers remain unaware. The risk is especially high in those who are overweight, have high blood pressure, or have a family history of the condition.
If you suspect sleep apnea, it’s important to seek medical evaluation. The Sleep Foundation and the CDC provide comprehensive resources on symptoms, diagnosis, and treatment options. Early recognition and intervention can dramatically improve sleep quality and overall health.
5. Dehydration Overnight

Mild dehydration is a surprisingly common cause of morning fatigue. Overnight, the body loses water through breathing, sweating, and even minor movements, all while you’re not actively replenishing fluids. This lack of hydration can make you feel sluggish, unfocused, and irritable upon waking. In fact, the grogginess and cognitive fog linked to dehydration can be similar to the symptoms of jet lag, where the body’s internal balance is temporarily thrown off.
Research shows that even a 1-2% reduction in body water can impair mood, alertness, and physical performance (NCBI). Dehydration also thickens the blood, forcing the heart to work harder and reducing oxygen delivery to muscles and the brain—further amplifying feelings of tiredness. Signs of overnight dehydration include a dry mouth, darker urine, headache, and feeling faint when standing up.
To optimize hydration, try drinking a glass of water before bed (but not so much that it disrupts sleep with bathroom trips), and keep water nearby for the morning. Limiting caffeine and alcohol in the evening can also help, as both are diuretics. For more hydration tips, visit the CDC’s guide on healthy hydration.
6. Vitamin D Deficiency

Vitamin D plays a crucial role in maintaining healthy muscle and nerve function, both of which are essential for feeling energized in the morning. This nutrient helps regulate calcium absorption and supports neuromuscular communication, impacting how your body transitions from rest to wakefulness. When vitamin D levels are low, you may experience muscle weakness, aches, and persistent fatigue, making mornings particularly difficult.
The phenomenon of winter fatigue—when people feel more sluggish and tired during the colder, darker months—is often linked to decreased sun exposure and subsequently lower vitamin D production. Studies have found that individuals with vitamin D deficiency are more likely to report symptoms of sleep disturbances and daytime sleepiness (NCBI).
If you suspect vitamin D deficiency, simple blood tests can confirm your levels. Warning signs include frequent illness, bone or back pain, and low mood in addition to tiredness. To improve vitamin D status, aim for moderate sun exposure, consume fortified foods, or consider supplements after consulting a healthcare provider. For more information, visit the NIH Office of Dietary Supplements for guidelines on vitamin D intake and testing.
7. Poor Air Quality in Bedroom

The air you breathe while sleeping can significantly impact how rested you feel upon waking. Allergens such as dust mites, pet dander, and mold spores are common in bedrooms and can trigger low-level inflammation, nasal congestion, and even micro-awakenings throughout the night. These subtle disruptions often go unnoticed but accumulate to reduce overall sleep quality. Additionally, low oxygen levels—caused by poor ventilation or a tightly sealed room—can impair the body’s ability to recover and recharge overnight.
The effects of poor indoor air quality can be as detrimental as exposure to outdoor air pollution, leading to headaches, morning grogginess, and persistent fatigue. Research highlights that people who sleep in environments with higher particulate matter or allergens are more likely to experience non-restorative sleep (NCBI).
To improve bedroom air quality, consider using high-efficiency particulate air (HEPA) filters, regularly washing bedding, and keeping pets out of the bedroom. Ensuring proper ventilation by opening windows or using an air purifier can also make a significant difference. For further air quality tips, visit the EPA’s Indoor Air Quality resource.
8. Iron Deficiency (Anemia)
Iron is a vital mineral that enables red blood cells to transport oxygen from the lungs to tissues throughout the body. When iron levels are low—a condition known as iron deficiency anemia—your blood cannot efficiently deliver oxygen, causing persistent fatigue and making it especially hard to feel energized in the morning. This lack of oxygen affects not only physical stamina but also cognitive performance and mood.
Athletes are particularly familiar with the effects of low iron, as their bodies require more oxygen during physical exertion. Even mild anemia can lead to reduced endurance, slower recovery, and a general sense of exhaustion. For non-athletes, morning tiredness that doesn’t improve with adequate sleep can be a red flag for iron deficiency.
Common signs include pale skin, frequent headaches, brittle nails, shortness of breath, and an increased heart rate. Women, vegetarians, and those with certain digestive conditions are especially at risk. Blood tests can confirm iron levels and guide appropriate supplementation or dietary changes. The CDC provides detailed information on iron and anemia, while the American Society of Hematology outlines symptoms and treatment options.
9. Blue Light Device Exposure

Modern lifestyles are filled with screens—phones, tablets, and laptops—that emit blue light, a wavelength proven to suppress the production of melatonin, the hormone responsible for regulating sleep-wake cycles. When melatonin release is delayed by evening screen use, your circadian rhythms become disrupted, making it harder to fall asleep and reducing the overall quality of your rest.
Consider the common scenario of scrolling through your phone in bed. Studies have shown that even brief exposure to blue light before sleep can delay melatonin secretion by up to an hour, leading to later sleep onset and increased morning grogginess (NCBI). Over time, this disruption can contribute to chronic tiredness, even if you think you’re getting enough hours of sleep.
To counteract these effects, establish a screen-free wind-down period at least 30-60 minutes before bed. Try reading a physical book, listening to calming music, or practicing gentle stretches instead. Adjusting device settings to “night mode” or using blue light-blocking glasses can also help, but limiting exposure remains most effective. Visit the Sleep Foundation’s guide for more strategies on managing blue light and protecting your circadian health.
10. Evening Alcohol Consumption

Alcohol is often mistaken for a sleep aid, but its effects on sleep architecture can leave you feeling even more tired in the morning. While alcohol may initially promote relaxation and help you fall asleep faster, it actually fragments sleep by disrupting the natural progression through sleep cycles. After metabolizing the alcohol, your body spends less time in restorative deep and REM sleep, resulting in frequent micro-awakenings and lighter, less restful slumber.
This disruption is comparable to the effects of caffeine, which delays sleep onset and reduces total sleep time. However, alcohol’s impact tends to be more insidious, as it masks its disruptive qualities by making you feel drowsy up front. Research shows that even moderate evening drinking can increase sleep disturbances and reduce next-day alertness (Sleep Foundation).
If you notice waking up groggy, dehydrated, or with headaches after a night of drinking, it may be time to reconsider your evening habits. Opt for non-alcoholic alternatives, set a drinking cut-off several hours before bedtime, or reserve alcoholic beverages for earlier in the day. More advice can be found at the CDC’s alcohol use resource.
11. Depression and Low Mood

Mood disorders like depression often have a profound effect on sleep patterns, frequently leading to persistent tiredness in the morning. Depression can disrupt the body’s internal clock, cause fragmented or shallow sleep, and trigger early morning awakenings that leave you feeling unrefreshed. Even after sufficient time in bed, people with depression may experience low energy, difficulty concentrating, and a lack of motivation to start the day.
Anxiety, while also disruptive, tends to cause difficulty falling asleep or staying asleep due to racing thoughts and heightened arousal. In contrast, depression is more likely to cause hypersomnia (excessive sleeping) or insomnia, often cycling between the two. Both conditions can create a vicious cycle where poor sleep worsens mood, and low mood further impairs sleep quality.
If you notice persistent sadness, loss of interest in activities, changes in appetite, or sleep disturbances lasting more than two weeks, it’s important to seek support from a healthcare provider or mental health professional. Early intervention can make a significant difference. The National Institute of Mental Health and the Mental Health Foundation offer resources for understanding symptoms and finding help.
12. Inconsistent Sleep Schedule

Maintaining irregular bedtimes and wake times can seriously disrupt your circadian rhythms, the internal clock that regulates your sleep-wake cycle. When you go to bed and wake up at different times each day, your body struggles to know when to release hormones like melatonin and cortisol, leading to morning grogginess and difficulty feeling refreshed. This disruption is remarkably similar to the experience of jet lag, where rapid time zone changes throw the body’s rhythms out of sync and leave you fatigued until you adjust.
The negative effects of an inconsistent sleep schedule are not limited to shift workers or frequent travelers. Even small variations from night to night can impact mood, cognitive sharpness, and physical health (Sleep Foundation). Tools that help regularize routines include setting alarms not just for waking up, but also for going to bed; using sleep tracking apps to monitor patterns; and creating a wind-down ritual to signal it’s time for sleep.
Experts recommend sticking to the same sleep and wake times, even on weekends, to anchor your circadian rhythm. For practical tips, visit the CDC’s sleep hygiene guide and the SleepHealth Foundation.
13. Thyroid Imbalance
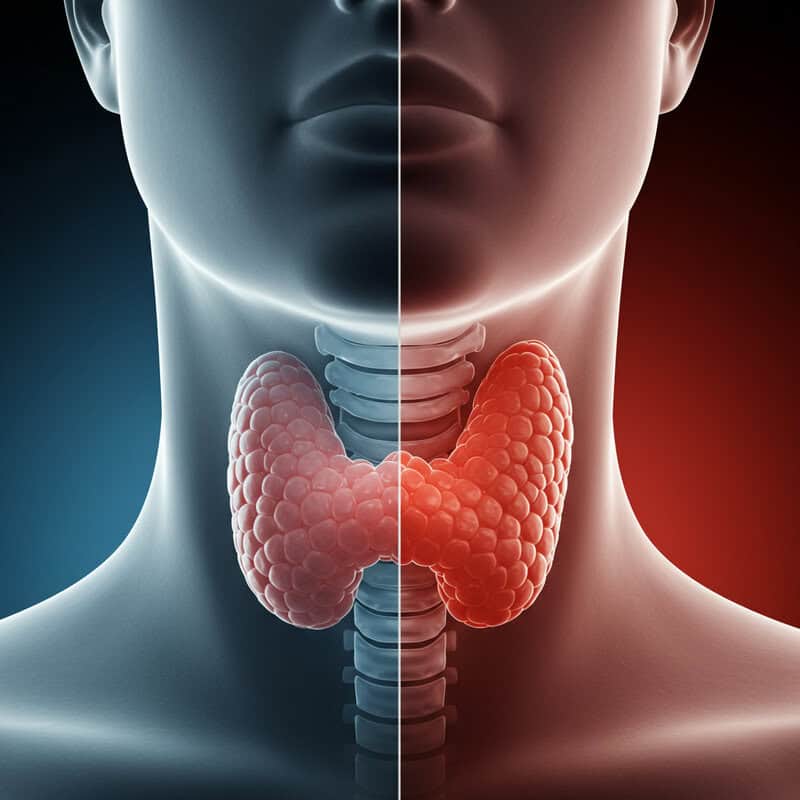
The thyroid gland, located at the base of the neck, regulates metabolism and significantly influences energy levels. When the thyroid is underactive (hypothyroidism), the body’s processes slow down, often resulting in persistent tiredness, weight gain, sensitivity to cold, and sluggishness in the morning. Conversely, an overactive thyroid (hyperthyroidism) can lead to restlessness, difficulty sleeping, increased heart rate, and feeling wired but exhausted.
Thyroid imbalance affects energy regulation in a way that’s similar to hormonal shifts during menopause, where fluctuations can cause fatigue, mood changes, and disrupted sleep. Both conditions involve changes in hormone production that impact the nervous system and metabolic rate, making mornings particularly challenging.
Common symptoms indicating potential thyroid problems include unexplained weight changes, hair loss, dry skin, constipation (in hypothyroidism), or increased sweating and anxiety (in hyperthyroidism). If you notice persistent fatigue along with any of these signs, it’s important to consult a healthcare professional for blood tests and evaluation. The National Institute of Diabetes and Digestive and Kidney Diseases and the American Thyroid Association provide comprehensive information about symptoms, diagnosis, and management of thyroid disorders.
14. Restless Leg Syndrome

Restless Leg Syndrome (RLS) is a neurological condition characterized by uncomfortable sensations in the legs, often described as creeping, crawling, or tingling. These sensations typically worsen at night and are temporarily relieved by movement, leading to involuntary leg movements that disrupt sleep without the person always being fully aware. As a result, individuals with RLS may spend hours tossing and turning, significantly reducing the quality of their rest and causing persistent morning fatigue.
RLS is closely related to Periodic Limb Movement Disorder (PLMD), another sleep disorder involving repetitive, involuntary leg (and sometimes arm) movements during sleep. While PLMD occurs exclusively during sleep and may not cause noticeable discomfort, it can similarly fragment sleep architecture, leaving sufferers feeling unrefreshed upon waking (Sleep Foundation).
If you suspect RLS or PLMD, monitoring your symptoms is key. Keep a sleep diary noting the frequency and severity of symptoms, and ask a partner if they notice frequent leg movements during the night. Video recordings or wearable sleep trackers can provide additional evidence. For more guidance on symptoms, diagnosis, and treatment, visit the National Institute of Neurological Disorders and Stroke resources.
15. Chronic Pain

Chronic pain conditions significantly interfere with the body’s ability to achieve restorative deep sleep. When pain is persistent—whether from arthritis, fibromyalgia, or back problems—it can cause frequent awakenings, make it difficult to shift into the deeper stages of sleep, and reduce overall sleep quality. This results in waking up feeling fatigued and unrefreshed, even after a full night in bed.
Arthritis serves as a prime example: joint stiffness and discomfort often worsen at night, leading to tossing, turning, and difficulty getting comfortable. Studies show that people with arthritis are much more likely to report insomnia and daytime sleepiness (Arthritis Foundation). The cycle of pain disrupting sleep and poor sleep amplifying pain sensitivity creates a challenging feedback loop.
Effective pain management strategies for better rest include using supportive mattresses and pillows, practicing gentle stretching or relaxation exercises before bed, and working with healthcare providers to optimize medication timing. Cognitive-behavioral therapy for insomnia (CBT-I) and mindfulness techniques can also help manage both pain and sleep disturbances. For more tips, explore resources from the CDC’s arthritis management guide.
16. Caffeine Timing

Caffeine is a widely used stimulant found in coffee, tea, chocolate, and many sodas and energy drinks. While it can boost alertness and improve focus when consumed in moderation, having caffeine too late in the day can significantly interfere with your ability to fall asleep and achieve restful sleep. Caffeine blocks adenosine, a neurotransmitter that promotes sleep, and its effects can linger for hours—sometimes staying in the body for up to eight hours or more.
Consuming caffeine in the late afternoon or evening can delay sleep onset, reduce total sleep time, and decrease the amount of deep sleep you get. This is similar to the effects of certain stimulant medications used for conditions like ADHD, which also increase alertness and may disrupt nighttime rest if taken too late (Sleep Foundation). The result is often morning grogginess and a sense of “sleep debt” that accumulates over time.
For better sleep, experts recommend limiting caffeine intake to the morning or early afternoon, ideally stopping consumption at least 6 hours before bedtime. Consider switching to decaffeinated beverages or herbal teas in the evening. For more information, see the CDC’s guide to sleep hygiene.
17. Room Temperature Extremes

The temperature of your bedroom plays a crucial role in regulating sleep cycles. When the environment is too hot or too cold, your body struggles to maintain its optimal core temperature, leading to frequent awakenings and disrupted sleep stages. Being too warm can cause excessive sweating, tossing, and shallow sleep, while a chilly room may increase muscle tension and make it harder to fall or stay asleep. Both extremes prevent you from reaching the deep, restorative stages of sleep necessary for morning energy.
This effect can be clearly observed during outdoor camping, where people often find themselves waking up more frequently due to fluctuating nighttime temperatures. Research shows that thermal discomfort is a leading cause of sleep disturbance, regardless of whether the source is a heatwave or a cold snap (Sleep Foundation).
Experts recommend keeping the bedroom temperature between 60 and 67 degrees Fahrenheit (15 to 19 degrees Celsius) for optimal sleep. Using breathable bedding, adjusting layers, and considering fans or space heaters can help maintain this range. For more advice on creating a sleep-friendly environment, visit the CDC’s bedroom environment guide.
18. Gut Health Imbalance

The gut microbiome—a diverse community of bacteria living in your digestive tract—plays a surprisingly influential role in sleep regulation. The gut produces and regulates neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), both of which are essential for initiating and maintaining restful sleep. When the balance of gut bacteria is disrupted, these neurotransmitter levels can be affected, leading to sleep disturbances and persistent fatigue upon waking.
Conditions like Irritable Bowel Syndrome (IBS) provide a clear example of this connection. People with IBS often report fragmented sleep and morning tiredness, which research has linked to altered gut flora and inflammation (NCBI). Gut health imbalances can also cause bloating, cramping, and discomfort at night, further reducing sleep quality.
Supporting gut health involves consuming a varied diet rich in fiber, prebiotics, and probiotics. Fermented foods like yogurt, kefir, sauerkraut, and kimchi can help restore balance. Managing stress and staying hydrated are also key factors. For more information on the relationship between the gut microbiome and sleep, visit the Sleep Foundation’s guide to gut health and sleep.
19. Sleep Environment Noise

Noise pollution is a significant disruptor of healthy sleep, often causing micro-awakenings and preventing the brain from cycling through the full spectrum of restorative sleep stages. Even if you don’t become fully conscious, environmental sounds like traffic, sirens, or loud neighbors can fragment your sleep, resulting in increased fatigue and grogginess upon waking. Chronic exposure to noise at night has been linked to higher rates of insomnia, cardiovascular stress, and impaired daytime performance.
Comparing urban and rural sleep patterns reveals the impact of environmental noise: urban dwellers are more likely to report poor sleep quality, frequent awakenings, and higher rates of morning tiredness due to constant background noise. In contrast, those living in quieter, rural settings often experience more consolidated and restorative sleep (NCBI).
To minimize noise disruption, consider using white noise machines, earplugs, or heavy curtains to dampen outside sounds. Arranging your bed away from windows and sealing gaps can further reduce noise intrusion. For more detailed strategies, visit the Sleep Foundation’s guide on noise and sleep environment management.
20. Nighttime Hypoglycemia

Nighttime hypoglycemia refers to drops in blood sugar levels that occur during sleep, leading to early morning fatigue, irritability, and a lack of mental clarity upon waking. This phenomenon is not limited to people with diabetes—anyone can experience mild nocturnal hypoglycemia, especially if they skip meals, eat unbalanced dinners, or engage in intense evening exercise. During sleep, the body continues to use glucose for essential functions, and if stores are depleted, the brain’s energy supply becomes compromised, resulting in grogginess and sluggishness in the morning.
For individuals with diabetes, hypoglycemic episodes at night can be more severe and may cause symptoms such as sweating, nightmares, confusion, or even waking up suddenly with a pounding heart. However, even those without diabetes may notice milder signs like headaches, mood swings, or an intense craving for carbohydrates upon waking (American Diabetes Association).
To maintain stable nighttime nutrition, opt for balanced dinners that include complex carbohydrates, healthy fats, and protein. Avoid excessive simple sugars and late-night snacking on sweets. Eating a small, balanced snack before bed may help some people. For more guidance, see the Sleep Foundation’s resource on blood sugar and healthy sleep.
21. Medication Side Effects

Many prescription and over-the-counter medications can disrupt normal sleep architecture, leading to unrefreshing rest and persistent morning fatigue. Medications for high blood pressure, depression, allergies, and asthma often alter neurotransmitter levels or interact with the nervous system, causing lighter sleep, frequent awakenings, or even vivid dreams. These effects reduce the amount of time spent in deep and REM sleep—the stages most critical for physical and mental restoration.
Even over-the-counter sleep aids, which are commonly used to help people fall asleep, can backfire by producing next-day grogginess or “sleep hangovers.” They may help initiate sleep but often disrupt its natural structure, leading to poor quality. Other medications to review with a doctor include beta-blockers, corticosteroids, selective serotonin reuptake inhibitors (SSRIs), certain antihistamines, and stimulant medications (Sleep Foundation).
If you suspect your medication is affecting your sleep, do not stop it abruptly. Instead, consult with your healthcare provider to discuss alternative options, timing adjustments, or additional strategies for minimizing side effects. For a comprehensive list and more information, visit the CDC’s medication and sleep resource.
22. Hormonal Fluctuations

Hormonal fluctuations throughout life—particularly those associated with the menstrual cycle, pregnancy, and menopause—can significantly impact sleep quality and morning energy. During different phases of the menstrual cycle, shifts in estrogen and progesterone can lead to insomnia, restless sleep, or more vivid dreams. Many women report increased fatigue and poorer sleep quality in the days leading up to menstruation due to these hormonal changes.
Pregnancy introduces additional hormonal shifts, often leading to disrupted sleep from increased urination, discomfort, and vivid dreams. Menopause, marked by declining estrogen and progesterone, frequently causes hot flashes and night sweats, which fragment sleep and result in morning tiredness. Hormonal therapy, such as birth control pills or hormone replacement therapy (HRT), can also affect sleep—sometimes improving it, but in some cases, causing further disruption (Sleep Foundation).
Tracking your symptoms in relation to your menstrual cycle, pregnancy progression, or hormone therapy regimen can help identify patterns and triggers. Journaling sleep quality, mood, and physical symptoms provides valuable data for you and your healthcare provider. For more detailed information, see the NICHD’s resource on women and sleep.
23. Nighttime Anxiety

Nighttime anxiety is a common culprit behind delayed sleep onset and unrefreshing mornings. When your mind races with worries, to-do lists, or intrusive thoughts at bedtime, it becomes difficult to transition into a restful state. This overactivity of the brain not only prolongs the time it takes to fall asleep but also increases the likelihood of waking up during the night, leading to fragmented and light sleep. The result is waking up tired, irritable, and mentally drained, even after spending enough hours in bed.
This phenomenon is closely related to generalized anxiety disorder (GAD), where persistent worry and tension can make both falling and staying asleep much harder. People with GAD often report chronic insomnia and frequent early morning awakenings, compounding their fatigue (Sleep Foundation).
To calm nighttime anxiety, try relaxation techniques such as deep breathing, progressive muscle relaxation, or mindfulness meditation before bed. Establishing a soothing bedtime routine—such as gentle stretching, reading, or listening to calming music—can help signal to your body that it’s time to unwind. For more strategies and professional guidance, visit the Anxiety.org resource on anxiety and sleep problems.
24. Undiagnosed Allergies
Allergies to dust mites, pets, or pollen often go undiagnosed, yet they can significantly impair sleep quality by affecting nighttime breathing. Even mild allergic reactions can cause nasal congestion, sneezing, postnasal drip, and itchy eyes, all of which disrupt sleep and contribute to morning fatigue. These symptoms may not be severe enough to notice during the day but can worsen when lying down, making it harder to breathe freely at night.
Hay fever (allergic rhinitis) serves as a clear example: people with hay fever often experience restless sleep and increased awakenings due to airway irritation and sinus congestion (Sleep Foundation). Over time, these disturbances prevent the body from reaching the deep stages of restorative sleep, leading to persistent tiredness and grogginess.
To allergen-proof your bedroom, use hypoallergenic mattress and pillow covers, wash bedding frequently in hot water, and keep pets out of sleeping areas. Consider using a HEPA air purifier and regularly vacuuming carpets and curtains to reduce dust and pollen buildup. For more practical advice and information, see the CDC’s healthy bedroom guide.
25. Overeating or Eating Too Late

Consuming large or heavy meals late at night can overload the digestive system and significantly disrupt sleep quality. When you eat shortly before bedtime, your body remains active digesting food instead of winding down for restorative sleep. This can lead to discomfort, acid reflux, bloating, and increased body temperature, all of which make it harder to fall and stay asleep.
In contrast, some people practice fasting or avoid eating several hours before bed, which allows the digestive system to rest and can promote deeper, more refreshing sleep. Research highlights that late-night eating is linked to fragmented sleep and higher rates of insomnia, while earlier, lighter dinners support normal sleep cycles (Sleep Foundation).
To improve sleep and morning energy, aim to finish your last meal at least two to three hours before going to bed. Focus on balanced meals with lean proteins, complex carbohydrates, and plenty of vegetables. Avoid heavy, spicy, or fatty foods late in the evening. For more tips on healthy meal timing and its effects on sleep, review the CDC’s sleep and nutrition resource.
26. Poor Mattress or Pillow Support

The quality of your mattress and pillow directly affects your spinal alignment, comfort, and overall restfulness. Inadequate bedding that is too soft, too firm, or uneven can cause poor posture during sleep, leading to muscle tension, back or neck pain, and frequent tossing and turning throughout the night. This not only prevents you from reaching the deepest, most restorative stages of sleep but also leaves you waking up with aches, stiffness, and persistent fatigue.
Using a well-designed, ergonomic setup—similar to how office chairs are chosen for support—can make a noticeable difference in sleep quality. A mattress that supports the natural curve of your spine and a pillow that keeps your head and neck in alignment help reduce pressure points and encourage uninterrupted sleep (Sleep Foundation).
Signs that your mattress or pillow needs replacing include visible sagging, lumps, waking up with new or worsening pain, or being unable to find a comfortable position. Experts recommend replacing mattresses every 7-10 years and pillows every 1-2 years. For more advice on choosing supportive bedding and recognizing when it’s time for an upgrade, see the CDC’s sleep environment guide.
27. Lack of Morning Light Exposure

Natural morning light plays a pivotal role in resetting your circadian rhythms, the internal clock that governs sleep-wake cycles and hormone release. Exposure to sunlight in the early hours signals your brain to suppress melatonin (the sleep hormone) and boost alertness-promoting chemicals like cortisol and serotonin. Without this daily cue, your body’s clock may drift, making it hard to feel fully awake in the morning and potentially leading to ongoing fatigue.
This phenomenon is clearly seen in shift workers, who often struggle with irregular sleep patterns and persistent tiredness due to a lack of consistent morning light exposure (Sleep Foundation). The absence of natural light in the morning delays circadian alignment, much like experiencing perpetual jet lag.
To maximize morning light, open curtains immediately upon waking, spend time outdoors during the first hour of your day, or consider using a light therapy lamp if natural sunlight is limited. Even a brief walk outside or sitting by a sunny window can help anchor your biological clock. For more practical strategies, review the CDC’s circadian health resource.
28. Undiagnosed Heart Issues
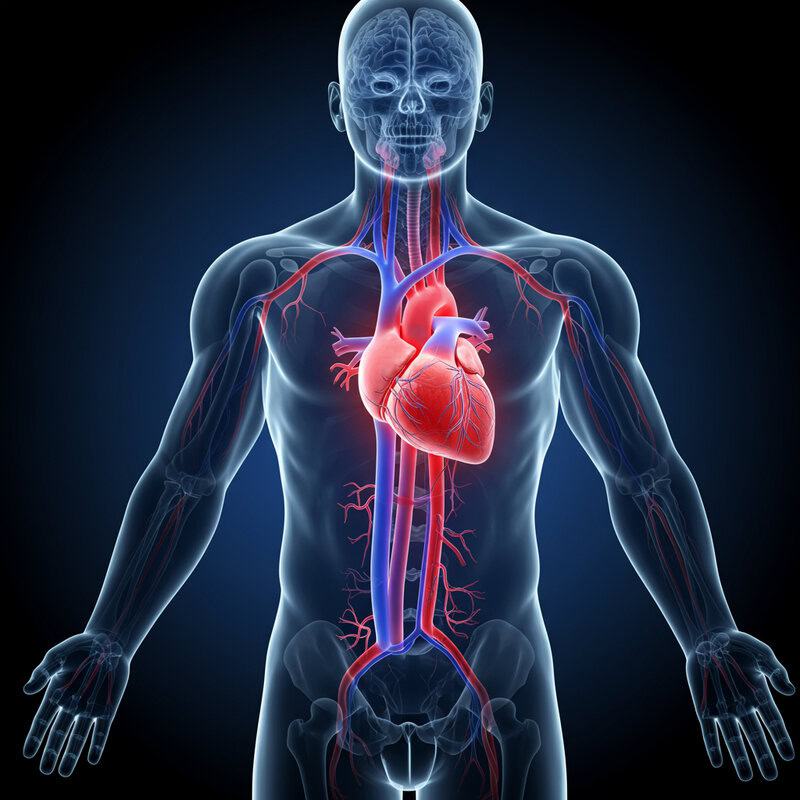
Underlying heart conditions can be a hidden cause of persistent morning fatigue, even when classic symptoms like chest pain or palpitations are absent. The heart is responsible for delivering oxygen-rich blood throughout the body, and when it isn’t functioning efficiently due to issues like arrhythmias, heart failure, or valve disorders, tissues and organs—including the brain—receive less oxygen. This can lead to subtle, ongoing tiredness that’s most noticeable upon waking, as the body hasn’t fully recuperated overnight.
Similar to sleep apnea, which causes intermittent drops in blood oxygen levels and fragmented sleep, undiagnosed heart problems can cause nonrestorative sleep and unexplained daytime sleepiness. The difference is that heart-related fatigue often persists despite improvements in sleep habits or environment (American Heart Association).
Warning signs to watch for include unexplained shortness of breath, swelling in the legs or ankles, frequent nighttime urination, or difficulty lying flat. If you experience persistent fatigue, especially with any of these symptoms or a family history of heart disease, seeking a medical evaluation and heart screening is essential. For more information, visit the CDC’s heart disease resource.
29. Hidden Infections

Low-grade or hidden infections—such as urinary tract infections, sinusitis, or even lingering viral illnesses—can quietly tax the body’s resources and sap energy overnight. These infections may not produce dramatic symptoms, but the immune system remains active as you sleep, diverting energy away from cellular repair and rest. As a result, you may wake up feeling unusually tired, achy, or mentally foggy, despite getting enough hours of sleep.
This experience shares similarities with chronic fatigue syndrome (CFS), where ongoing immune activation leads to profound exhaustion and unrefreshing sleep. While CFS is a complex disorder with multiple triggers, silent infections are thought to play a role in its development and persistence (CDC).
Symptoms to monitor include unexplained low-grade fever, night sweats, swollen lymph nodes, mild chills, muscle aches, or a persistent sore throat. If you notice these signs, especially alongside lasting fatigue, it’s important to consult a healthcare provider for proper testing and diagnosis. For more information on chronic fatigue and the subtle impacts of infections, review the NHS resource on CFS.
30. Narcolepsy or Rare Sleep Disorders
Narcolepsy and other rare sleep disorders can cause profound unrefreshing sleep, regardless of how many hours you spend in bed. Narcolepsy is a neurological disorder that disrupts the brain’s ability to regulate sleep-wake cycles, leading to excessive daytime sleepiness, sudden “sleep attacks,” and sometimes episodes of muscle weakness (cataplexy). People with narcolepsy may experience vivid dreams, hallucinations when falling asleep or waking, and fragmented nighttime sleep, resulting in persistent fatigue and difficulty functioning during the day.
These rare disorders differ from more common issues like sleep apnea, in which breathing interruptions fragment sleep and reduce its restorative quality. However, both conditions result in chronic tiredness and an inability to feel fully rested. While sleep apnea often responds to lifestyle changes or CPAP therapy, narcolepsy and similar disorders require specialized diagnosis and management (Sleep Foundation).
If you consistently wake up tired despite practicing good sleep hygiene, or experience symptoms such as sudden muscle weakness, hallucinations at sleep transitions, or uncontrollable daytime sleepiness, it’s important to consult a sleep specialist. A formal sleep study (polysomnography) and daytime testing can help identify the underlying cause. For more details, visit the NINDS narcolepsy resource.
31. Overtraining or Excessive Exercise
While regular physical activity is essential for healthy sleep, too much intense exercise—especially without adequate recovery—can backfire and leave you waking up tired. Overtraining taxes the body’s muscles, joints, and nervous system, increasing inflammation and stress hormone levels overnight. Instead of allowing for cellular repair during sleep, the body remains in a heightened state of recovery, which can fragment sleep cycles and reduce time spent in deep, restorative stages.
In contrast, incorporating rest days into your exercise routine allows the body to heal, replenish energy stores, and optimize sleep quality. Research indicates that athletes who overtrain or fail to schedule rest are more likely to experience insomnia, increased fatigue, and even mood disturbances (Sleep Foundation).
Signs of overexertion to watch for include persistent muscle soreness, irritability, elevated resting heart rate, frequent illness, and a noticeable drop in performance or motivation. If you’re experiencing these symptoms alongside poor sleep, consider scaling back your workout intensity and prioritizing rest and recovery. For more guidance on balancing exercise and sleep, visit the CDC’s physical activity resource.
32. Low Magnesium Levels

Magnesium is a vital mineral that plays a key role in muscle relaxation, nerve function, and the regulation of sleep. It helps activate neurotransmitters that calm the nervous system and promotes the transition to deep sleep by supporting the body’s natural circadian rhythms. When magnesium levels are low, you may experience muscle cramps, restless legs, and frequent nighttime awakenings, all of which contribute to unrefreshing sleep and persistent morning fatigue.
Calcium is another important mineral for muscle function, but unlike magnesium—which relaxes muscles—calcium is involved in muscle contraction. An imbalance, with too little magnesium and relatively high calcium, can lead to increased muscle tension and difficulty winding down at night. Studies have shown that magnesium supplementation can improve sleep quality, especially in older adults and those with insomnia (Sleep Foundation).
Signs of magnesium deficiency include muscle twitches, cramps, irritability, fatigue, and even irregular heart rhythms. To boost magnesium intake, incorporate foods like leafy green vegetables, nuts, seeds, whole grains, and legumes into your diet. For more information on magnesium’s role in sleep and how to recognize a deficiency, visit the NIH Office of Dietary Supplements.
33. Insufficient Protein Intake

Protein is essential for muscle repair, hormone production, and maintaining steady energy levels. During sleep, the body relies on protein to rebuild tissues and synthesize important neurotransmitters that influence alertness and mood. If your diet is low in protein, your ability to recover from daily physical activity is diminished, and you may wake up feeling sore, weak, or persistently tired. Additionally, insufficient protein can lead to unstable blood sugar levels, which further disrupt restful sleep and morning energy.
Vegetarian and vegan diets can be especially prone to protein deficiencies if not carefully planned, as plant-based sources may contain less complete proteins compared to animal products. However, with mindful choices—such as combining legumes, grains, nuts, and seeds—it’s possible to meet protein needs and support muscle repair (Sleep Foundation).
Signs of low protein intake include frequent muscle soreness, slow wound healing, hair thinning, and feeling fatigued despite adequate rest. To boost protein, incorporate foods like eggs, dairy, fish, poultry, tofu, beans, lentils, quinoa, and Greek yogurt. For more information on protein’s role in sleep and energy, visit the Harvard T.H. Chan School of Public Health’s protein guide.
34. Unresolved Grief or Trauma

Emotional distress from unresolved grief or trauma can profoundly disrupt sleep and leave you feeling persistently tired, even after a full night’s rest. Unlike acute stress reactions—which may cause temporary sleeplessness, increased heart rate, or anxiety—longstanding grief or trauma can lead to chronic sleep disturbances, nightmares, and frequent awakenings. The body remains in a heightened state of alertness, making it difficult to reach deep, restorative stages of sleep.
This persistent fatigue is not just psychological; it is rooted in the ongoing activation of the nervous system and stress hormones, which can affect immune function and overall health. Unresolved emotional pain may also contribute to feelings of depression, apathy, or a lack of motivation, further compounding morning tiredness (Sleep Foundation).
If you notice ongoing sadness, intrusive memories, difficulty sleeping, or a sense of emotional numbness that persists for weeks or months, it may be time to seek counseling or professional support. Early intervention with therapy, support groups, or trauma-informed care can promote healing and improve both sleep quality and daytime energy. For more resources, visit the U.S. Department of Veterans Affairs’ sleep and trauma guide.
35. Sleep Partner Disturbances

Sharing a bed with a partner can often lead to sleep disruptions, even if you’re not fully aware of them. A partner’s movements, snoring, talking, late-night phone use, or differing sleep schedules can cause micro-awakenings and prevent you from reaching deep, restorative stages of sleep. These subtle disturbances accumulate over the night, leading to morning grogginess, fatigue, and irritability.
In comparison, solo sleepers generally experience fewer interruptions and more consistent sleep quality. Studies have shown that sharing a bed with a partner who snores or has restless sleep can significantly reduce overall sleep efficiency (Sleep Foundation).
Strategies to improve shared sleep include using white noise machines to mask sounds, investing in a larger mattress for more personal space, and considering separate blankets to minimize movement transfer. If snoring is a persistent issue, encourage your partner to seek medical evaluation for conditions like sleep apnea. Establishing compatible bedtime routines and communicating openly about sleep needs can also enhance sleep for both partners. For more tips, visit the CDC’s guide to optimizing your sleep environment.
36. Overuse of Sleep Medications

Relying excessively on sleep medications—whether prescription or over-the-counter (OTC)—can actually worsen sleep quality over time. While these drugs may initially help you fall asleep faster, long-term use often leads to tolerance, dependency, and “rebound insomnia,” where sleep becomes even more difficult without the medication. Both prescription sleep aids (such as benzodiazepines and Z-drugs) and OTC remedies (like antihistamines) can disrupt natural sleep cycles, reduce time spent in deep and REM sleep, and cause next-day grogginess.
Prescription medications tend to be more potent and can lead to stronger dependency and withdrawal symptoms, whereas OTC sleep aids may be less addictive but still carry risks of hangovers and cognitive impairment, especially in older adults (Sleep Foundation). Over time, overuse of these medications can mask underlying sleep issues without addressing the root cause.
Weaning off sleep medications should be done gradually and under medical supervision to minimize withdrawal effects. Incorporating behavioral strategies—such as cognitive-behavioral therapy for insomnia (CBT-I), improving sleep hygiene, and using relaxation techniques—can restore natural sleep rhythms. For more guidance, visit the CDC’s resource on sleep and medications.
37. Undiagnosed Autoimmune Disease
Autoimmune diseases such as lupus and rheumatoid arthritis can be hidden culprits behind persistent fatigue, especially in the morning. These conditions occur when the immune system mistakenly attacks the body’s own tissues, leading to chronic inflammation and impaired cellular repair during sleep. Unlike acute viral infections, which typically cause a sudden onset of tiredness, autoimmune diseases produce ongoing, fluctuating fatigue that often does not improve with rest.
The fatigue experienced in autoimmune disorders is frequently accompanied by other symptoms, such as joint pain, morning stiffness, mild fever, unexplained rashes, or swelling. The persistent inflammatory response also disrupts normal sleep architecture, making it difficult to achieve restorative deep sleep (Sleep Foundation).
Early warning signs to watch for include symmetrical joint pain, unexplained muscle aches, chronic low-grade fevers, lingering mouth ulcers, or marked changes in energy levels. If you experience these symptoms along with persistent tiredness, it is important to consult a healthcare provider for evaluation and possible autoimmune screening. For more information on autoimmune fatigue and its impact on sleep, visit the Lupus Foundation of America’s sleep resource.
38. Poor Evening Routine

An erratic or overly stimulating evening routine can significantly disrupt your ability to wind down and achieve restorative sleep. Engaging in activities such as late-night work, intense exercise, scrolling through social media, or consuming caffeinated beverages can keep your mind and body in a heightened state of alertness. This delays the release of melatonin, the hormone responsible for signaling sleep, and makes it harder to transition into restful slumber.
In contrast, mindful evening routines—such as dimming lights, reading a book, practicing gentle stretches, or engaging in relaxation exercises—promote a gradual wind-down process. These habits help cue your circadian rhythm that it’s time for rest, leading to faster sleep onset and better sleep quality (Sleep Foundation).
To improve your evening routine, establish a consistent bedtime, avoid screens at least 30-60 minutes before sleep, and create a calming environment with soothing music or aromatherapy. Writing down worries or next-day plans can also help clear your mind. For more tips on developing a healthy evening routine, visit the CDC’s sleep hygiene guide.
39. Low Blood Pressure

Low blood pressure, or hypotension, can be an underappreciated cause of morning dizziness, weakness, and fatigue. When blood pressure is low, the heart and blood vessels may struggle to supply enough oxygen and nutrients to the brain and muscles, particularly after rising from bed. This can lead to symptoms such as lightheadedness, blurred vision, and a sense of overwhelming tiredness upon waking.
Much like the effects of dehydration—which also reduces blood volume and can cause similar symptoms—hypotension is often most noticeable in the morning when you first stand up. Common causes include inadequate fluid intake, certain medications, hormonal imbalances, or underlying heart conditions (Mayo Clinic).
Signs to monitor include frequent dizziness, fainting, excessive fatigue, cold or clammy skin, and rapid or irregular heartbeat. If these symptoms persist, especially if they interfere with daily activities, seek medical advice for evaluation and management. Increasing fluid and salt intake, rising slowly from bed, and wearing compression stockings are practical ways to help manage low blood pressure. For more information, visit the CDC’s guide to blood pressure.
40. Chronic Inflammation
Chronic inflammation—an ongoing, low-grade immune response in the body—can have a major impact on sleep cycles and morning energy. Unlike acute infections, which cause short-term symptoms and typically resolve with healing, chronic inflammation is persistent and often subtle. It can disrupt the balance of cytokines, signaling molecules that help regulate sleep and immune function, leading to fragmented sleep, less time in deep sleep stages, and more frequent awakenings throughout the night.
This ongoing disruption prevents the body from undergoing proper repair and restoration during sleep, resulting in morning fatigue, muscle aches, and brain fog. Chronic inflammation is associated with conditions like obesity, diabetes, autoimmune diseases, and even untreated allergies (Sleep Foundation).
To combat chronic inflammation, adopt an anti-inflammatory lifestyle: eat a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats like omega-3s; manage stress through mindfulness or yoga; engage in regular moderate exercise; and prioritize restorative sleep. Avoiding processed foods and excess sugar can also help. For more science-backed tips, visit the CDC’s chronic inflammation resource.
41. Sleep Procrastination (Revenge Bedtime)

Sleep procrastination—often called “revenge bedtime procrastination”—occurs when you intentionally delay going to bed in order to reclaim personal leisure time, usually after a long or stressful day. This habit leads to later bedtimes, reduced total sleep duration, and, ultimately, persistent morning fatigue. Many people scroll through social media, binge-watch shows, or engage in other activities late into the night, sacrificing crucial rest for a sense of autonomy or relaxation.
Unlike time management strategies that prioritize rest and productivity, sleep procrastination undermines both by creating a cycle of sleep deprivation and reduced daytime performance. Research has shown that this behavior is linked to increased stress, mood swings, and difficulty concentrating the next day (Sleep Foundation).
Healthier alternatives include scheduling daily leisure breaks, setting alarms or reminders for bedtime, and creating a relaxing pre-sleep routine that satisfies your need for “me time” without encroaching on sleep hours. Practicing mindful time management and prioritizing self-care can help break the cycle of bedtime procrastination. For more practical tips, visit the CDC’s sleep hygiene resource.
42. Overexposure to Artificial Light

Excessive exposure to artificial light in the evening can significantly disrupt your circadian rhythms—the body’s natural 24-hour clock that regulates sleep and wakefulness. Bright indoor lighting, LED screens, and even streetlights filtering through windows can inhibit the release of melatonin, the hormone that signals it’s time for rest. This confusion makes it harder to fall asleep, delays sleep onset, and leads to lighter, fragmented sleep, resulting in tiredness the next morning.
In contrast, people who spend time camping or in nature—away from artificial lighting—often experience more consistent sleep and earlier bedtimes, as their circadian rhythms align more closely with the natural cycle of daylight and darkness (Sleep Foundation).
To create a sleep-friendly lighting environment, dim household lights at least an hour before bed, use warm-colored bulbs, and consider blackout curtains to block outside light. Avoid exposure to screens or use blue light filters on devices in the evening. Creating a gradual transition to darkness helps cue your body for sleep. For more actionable advice, review the CDC’s guide to optimizing bedroom lighting.
43. Nighttime Technology Use

Using technology such as TVs, smartphones, and tablets before bed can overstimulate the brain and significantly disrupt the natural wind-down process needed for restful sleep. The combination of engaging content and blue light exposure from screens keeps the mind alert, delays the release of melatonin, and makes it harder to transition into the relaxed state necessary for sleep. This often leads to later bedtimes, difficulty falling asleep, and less restorative sleep overall, resulting in morning grogginess and fatigue.
In contrast, reading a physical book under soft, warm lighting promotes relaxation and helps signal to the brain that it’s time to prepare for sleep. Studies have shown that people who adopt screen-free bedtime routines fall asleep faster and report better sleep quality than those who use electronic devices at night (Sleep Foundation).
To foster healthier sleep habits, establish a screen-free wind-down period of 30-60 minutes before bed. Swap technology use for calming activities such as journaling, meditation, gentle stretching, or listening to soothing music. For more screen-free ideas and guidance, visit the CDC’s sleep hygiene resource.
44. Poor Sleep Hygiene

Poor sleep hygiene refers to habits and environmental factors that undermine restful sleep, such as inconsistent bedtimes, excessive bedroom clutter, noise, and frequent disruptions. These conditions can make it challenging for your mind and body to associate the bedroom with relaxation, leading to difficulty falling asleep, lighter sleep, and frequent awakenings. Over time, this results in persistent tiredness and diminished daytime performance.
In comparison, many people find they sleep better in hotel rooms—often because the environment is clean, quiet, dark, and free from distractions. The contrast highlights the importance of a consistent, calming routine and a clutter-free, purpose-built sleep space (Sleep Foundation).
To improve sleep hygiene, establish a regular sleep schedule, use your bed only for sleep and intimacy, and keep the bedroom tidy and free from electronics. Block out light with blackout curtains, minimize noise with white noise machines or earplugs, and keep the room cool and well-ventilated. Limit caffeine and heavy meals before bedtime, and create a soothing wind-down routine. For more actionable strategies, visit the CDC’s sleep hygiene guide.
45. Undiagnosed Diabetes or Prediabetes

Undiagnosed diabetes or prediabetes can silently undermine sleep quality and leave you waking up tired, even after a full night’s rest. Elevated blood sugar levels disrupt the body’s ability to repair and restore itself during sleep. High glucose can cause frequent urination, dehydration, and restless sleep, all of which limit your time in deep, restorative sleep stages. Over time, this leads to persistent morning fatigue, increased thirst, and unexplained irritability.
Insulin resistance—the hallmark of prediabetes—prevents cells from efficiently using glucose for energy. This causes blood sugar to remain high overnight, placing additional stress on the kidneys and nervous system. People with undiagnosed diabetes or insulin resistance are more prone to sleep disturbances, including insomnia and obstructive sleep apnea (Sleep Foundation).
Warning signs to watch for include excessive thirst, frequent nighttime urination, unexplained weight changes, and persistent fatigue. If these symptoms are present, or if you have risk factors such as family history or obesity, it’s important to get tested for diabetes. Early detection and management can dramatically improve sleep quality and overall health. For more information, visit the CDC’s diabetes symptoms resource.
46. Nutrient Deficiencies (B12, Folate, etc.)

B vitamins—including B12 and folate—are crucial for energy metabolism, red blood cell production, and nervous system health. Deficiencies in these nutrients can result in inadequate oxygen delivery to tissues, impaired nerve function, and persistent fatigue, even after a seemingly adequate night’s sleep. B12, in particular, is essential for converting food into cellular energy and maintaining myelin, the protective sheath around nerves.
Vegan and vegetarian diets are more likely to be low in B12, as this vitamin is primarily found in animal products. Without careful supplementation or consumption of fortified foods, those following plant-based diets may experience symptoms of deficiency such as weakness, memory problems, tingling in the hands or feet, and chronic tiredness (Sleep Foundation).
To prevent or address deficiencies, consider regular blood tests—especially if you have dietary restrictions or persistent fatigue. Supplementation options include B12 tablets, sprays, or injections, as well as folate-rich foods like leafy greens, beans, and fortified cereals. For comprehensive guidance on B vitamins and supplementation, visit the NIH Office of Dietary Supplements.
47. Asthma or Breathing Disorders

Nocturnal asthma and other breathing disorders can significantly hinder your ability to reach and maintain deep, restorative sleep. During the night, airway inflammation or constriction can worsen, leading to symptoms such as coughing, wheezing, chest tightness, and shortness of breath. These interruptions fragment sleep cycles and make it difficult for the body to enter the deep stages necessary for physical and mental recovery, resulting in persistent morning fatigue.
Similar to allergies, which can cause nasal congestion and airway irritation, asthma often flares up overnight due to reclining posture, cooler air, or increased exposure to indoor allergens. However, breathing disorders like asthma may cause more pronounced and persistent symptoms, including sudden awakenings and the need for rescue inhalers (Sleep Foundation).
To monitor nocturnal breathing problems, keep a symptom diary and note any nighttime awakenings, coughing fits, or difficulty breathing. Using a peak flow meter before bed and upon waking can help track lung function. Consult your healthcare provider about optimizing asthma management, minimizing bedroom allergens, and using air purifiers. For more support, visit the CDC’s asthma resource.
48. Chronic Fatigue Syndrome (CFS/ME)
Chronic Fatigue Syndrome, also known as Myalgic Encephalomyelitis (CFS/ME), is a complex disorder marked by profound, unrelenting fatigue that does not improve with rest or adequate sleep. Individuals with CFS/ME report waking up feeling just as tired as when they went to bed, regardless of the number of hours slept. This persistent exhaustion is often accompanied by brain fog, muscle or joint pain, headaches, and unrefreshing sleep, making daily activities challenging.
CFS/ME shares similarities with fibromyalgia, another condition characterized by widespread pain and sleep disturbances. Both disorders disrupt sleep architecture, reducing the restorative quality of sleep and leading to increased daytime sleepiness and cognitive difficulties (CDC).
Because CFS/ME symptoms can mimic those of other chronic health problems, it’s important to seek specialty care if you experience unexplained, persistent fatigue lasting more than six months, especially if accompanied by memory issues, sore throat, or muscle pain. Diagnosis can be complex and may require consultation with a sleep or fatigue specialist. For more information and support, visit the NHS CFS resource.
49. Overuse of Napping

While napping can provide a quick energy boost, excessive or poorly timed naps can disrupt nighttime sleep and contribute to morning fatigue. Long naps—especially those lasting more than 30 minutes—or napping late in the day can make it harder to fall asleep at bedtime, reduce overall sleep drive, and fragment the natural sleep-wake cycle. This can result in lighter, less restorative sleep at night and persistent grogginess upon waking.
In contrast, power napping—short naps of 10 to 20 minutes taken early in the afternoon—has been shown to enhance alertness and cognitive performance without interfering with nighttime sleep (Sleep Foundation). These brief naps are less likely to cause sleep inertia (the groggy feeling after waking from deep sleep) and are more compatible with healthy sleep habits.
To optimize nap benefits, limit naps to 20-30 minutes and avoid napping after 3 p.m. If you find yourself relying on naps daily or struggling with nighttime sleep, reassess your sleep hygiene and daily schedule. For more guidance on healthy napping, visit the CDC’s napping tips resource.
50. Unmanaged Sleep Disorders

Unmanaged sleep disorders—such as insomnia, parasomnias (like sleepwalking or night terrors), and circadian rhythm disorders—are common but frequently go unrecognized. These conditions disrupt the natural architecture of sleep, leading to frequent awakenings, difficulty falling or staying asleep, and non-restorative rest, regardless of total sleep time. The result is persistent morning fatigue, mood changes, and impaired daytime functioning, often without an obvious cause.
By contrast, individuals who have received a proper diagnosis and management plan for their sleep disorder—through behavioral therapy, medication, or lifestyle changes—often experience dramatic improvements in sleep quality and daytime alertness. Early recognition and treatment are crucial, as untreated sleep disorders can increase the risk for accidents, depression, and chronic health issues (Sleep Foundation).
If you regularly struggle with falling asleep, staying asleep, abnormal nighttime behaviors, or a misaligned sleep-wake schedule, consider keeping a sleep diary and discussing your symptoms with your healthcare provider. Referral to a sleep specialist for evaluation and, if needed, a sleep study can help pinpoint underlying issues and guide effective treatment. For more information, visit the CDC’s sleep disorders resource.
Conclusion

Morning fatigue isn’t always a simple matter of sleep quantity. As explored, a wide range of biological, environmental, and lifestyle factors can undermine how rested you feel, regardless of hours spent in bed. Understanding and addressing these underlying causes is essential for lasting energy and well-being. If persistent tiredness affects your life, start by keeping a detailed sleep diary to track symptoms, habits, and patterns. Don’t hesitate to seek professional evaluation for hidden disorders or chronic fatigue. Early intervention can lead to more effective, personalized solutions. For further guidance on sleep health and fatigue management, visit the Sleep Foundation or the CDC’s Sleep Health resource.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





