The Tiny Evening Habit That’s Quietly Ruining Your Insulin Sensitivity
Insulin resistance now affects over 1 in 3 adults worldwide, contributing to rising rates of metabolic disorders such as type 2 diabetes and obesity, according to the CDC and International Diabetes Federation. The endocrine system, which governs hormone balance and glucose regulation, often suffers quietly before symptoms appear. Early warning signs—like mild fatigue or cravings—can be subtle and easily overlooked. Understanding these signals and the impact of daily habits is crucial for safeguarding long-term metabolic health.
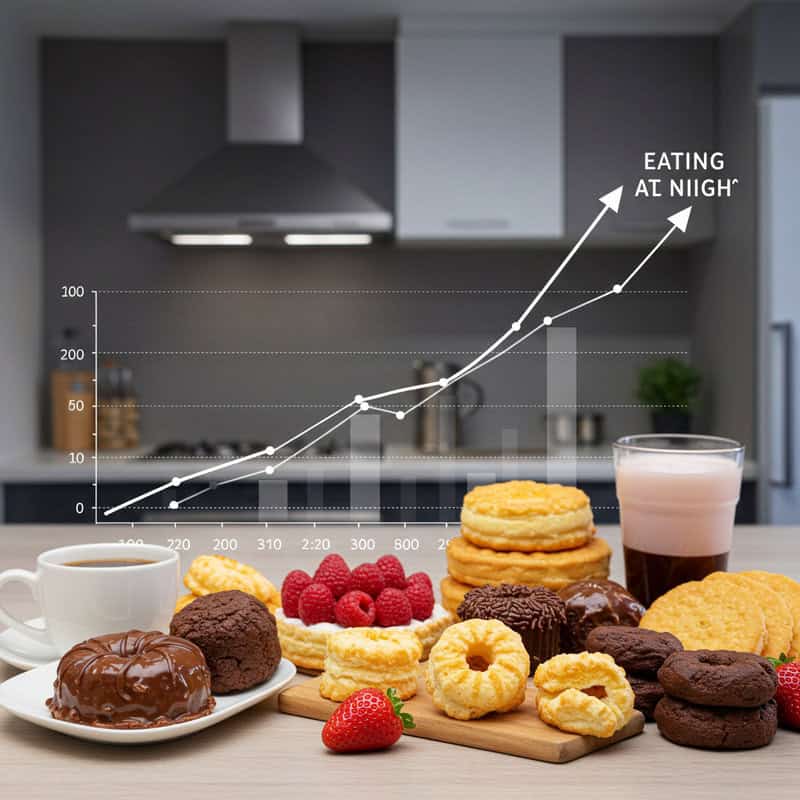
1. Late-Night Snacking

Consuming snacks late in the evening can quietly undermine your metabolic health by disrupting your body’s natural insulin response. Our circadian rhythm, the internal clock that regulates sleep and hormone cycles, causes insulin sensitivity to decline at night. When you eat close to bedtime, your pancreas must work harder to process glucose, leading to elevated blood sugar levels that persist into the night. Over time, this can promote insulin resistance and increase the risk of developing type 2 diabetes, as highlighted by recent research from the National Institutes of Health.
Consider a common scenario: after dinner, you unwind by watching television and reach for a bowl of ice cream or chips. While this comfort food may seem harmless, it prompts a late surge of insulin production at a time when your body is least prepared to handle it. This repeated pattern can gradually erode your metabolic resilience. Avoiding late-night snacking gives your endocrine system a chance to reset overnight, supporting better blood sugar regulation and overall health. For more tips on meal timing and metabolic health, visit the Harvard T.H. Chan School of Public Health.
2. Excessive Screen Time Before Bed

Spending too much time on digital devices in the evening exposes your eyes to blue light, which can significantly disrupt your circadian rhythms and, in turn, your insulin sensitivity. Blue light from screens suppresses melatonin production, a hormone essential for sleep regulation. According to the Sleep Foundation, disrupted sleep patterns have been linked to impaired glucose tolerance and higher levels of insulin resistance.
Unlike natural light, which gradually diminishes as evening approaches, artificial screen light remains intense and constant, sending mixed signals to your brain about when it’s time to wind down. This confusion can delay the onset of deep sleep, a critical phase when the body repairs itself and optimizes hormone function. In contrast, exposure to natural evening light allows the body’s internal clock to synchronize properly, promoting better metabolic outcomes.
To minimize these negative effects, experts recommend limiting screen use at least one hour before bedtime. Consider switching to dim, warm lighting in the evening and using features like night mode or blue light filters on your devices. For further strategies to manage screen exposure, consult resources from the Centers for Disease Control and Prevention.
3. Evening Alcohol Consumption

Drinking alcohol in the evening can have a disruptive effect on insulin signaling and overall metabolic health. Alcohol interferes with the liver’s ability to regulate glucose, leading to erratic blood sugar levels and reduced insulin sensitivity. Research from the National Institute on Alcohol Abuse and Alcoholism highlights that even moderate evening drinking can impair insulin action, especially when combined with high-carbohydrate foods often consumed during social gatherings.
A common scenario is the after-work happy hour, where friends or colleagues unwind with a few drinks and appetizers. While this ritual may seem harmless, it places additional strain on the endocrine system during a time when the body is naturally preparing for rest and cellular repair. Alcohol not only increases the risk of late-night snacking but also disrupts sleep cycles, further compounding insulin resistance issues.
Adopting moderation strategies can help protect your metabolic health. Try limiting alcohol intake to one standard drink per day for women and two for men, as recommended by the Centers for Disease Control and Prevention. Alternating alcoholic beverages with water, choosing lower-sugar options, and setting a “last call” at least two hours before bedtime can also aid in minimizing the metabolic impact.
4. Skipping Dinner

While intermittent fasting and meal-skipping trends have gained popularity for potential weight loss benefits, skipping dinner can actually backfire when it comes to blood sugar control and insulin sensitivity. Going for extended periods without food may cause blood glucose to drop, prompting the body to release stress hormones such as cortisol and adrenaline, which can spike blood sugar unpredictably. According to research published in the National Library of Medicine, irregular meal patterns are linked to poorer glycemic control and increased risk of metabolic syndrome.
Many people who skip dinner in an attempt to “save calories” often find themselves ravenous later in the evening or the next morning, leading to overeating or craving high-sugar foods. This cycle can place unnecessary stress on the pancreas and disrupt the body’s natural insulin response. Balanced meal timing, rather than skipping meals, is crucial for steady blood glucose levels and optimal metabolic health.
If you’re considering fasting, it’s important to do so under medical guidance and with a focus on consistent, nutrient-dense meals during eating windows. For practical advice on healthy meal timing and the science behind fasting, visit the Harvard T.H. Chan School of Public Health.
5. Binge-Watching TV Shows

Engaging in prolonged periods of sedentary activity, such as binge-watching TV shows in the evening, can significantly decrease insulin sensitivity. When the body remains inactive for hours at a time, glucose uptake by muscles slows down, leading to higher blood sugar levels and increased insulin resistance. A study published in Diabetologia found that each additional hour of television viewing was associated with a higher risk of developing type 2 diabetes due to inactivity’s metabolic impact.
In contrast, active forms of relaxation—like taking a walk after dinner, gentle stretching, or even standing while reading—help lower post-meal glucose spikes and enhance insulin efficiency. These activities promote muscle contractions that aid in glucose transport and metabolism, supporting healthier blood sugar regulation. The difference between passive and active evening routines can be profound for metabolic health over time.
To minimize the risks associated with sedentary habits, try setting reminders to stand up and move every 30 minutes, incorporate short walks, or practice yoga or light resistance exercises in the evening. For more evidence-based ideas to reduce sedentary time and boost metabolic health, refer to resources from the Centers for Disease Control and Prevention.
6. High-Sugar Desserts After Dinner

Indulging in high-sugar desserts after dinner can lead to significant blood sugar spikes at a time when your body’s ability to process glucose is already diminished. When you consume sweets like ice cream, cakes, or cookies late in the evening, your pancreas must produce more insulin to manage the sudden influx of sugar. This pattern, especially when repeated nightly, can wear down insulin sensitivity over time and increase the risk for insulin resistance and type 2 diabetes. According to the Harvard T.H. Chan School of Public Health, refined sugars and simple carbohydrates contribute to sharp rises and falls in blood glucose.
Even seemingly innocent treats such as chocolate bars or sweetened yogurts can have similar effects if consumed post-dinner. These sugar surges disrupt the body’s overnight metabolic processes, preventing proper hormone balance and cellular repair. To protect your insulin sensitivity, opt for healthier alternatives like fresh fruit, Greek yogurt, or a small handful of nuts when you crave something sweet after dinner. These options contain fiber, protein, and healthy fats, which help slow the absorption of sugar and maintain steadier glucose levels. For more guidance on healthy dessert swaps, visit the Centers for Disease Control and Prevention.
7. Drinking Caffeinated Beverages at Night

Consuming caffeinated beverages such as coffee, tea, or energy drinks late in the evening can disrupt both glucose metabolism and sleep quality, leading to a reduction in insulin sensitivity. Caffeine stimulates the release of adrenaline, which can raise blood sugar levels by promoting glucose release from the liver. According to a study published in the Journal of Clinical Nutrition, caffeine intake in the evening impairs insulin’s ability to regulate blood glucose, making it harder for your body to maintain stable levels overnight.
Many people enjoy a cup of coffee with dessert or a caffeinated soda while watching TV, not realizing that the stimulant effect can linger for hours. This not only makes it more difficult to fall asleep but also interferes with deep, restorative sleep cycles that are essential for healthy metabolic function. Poor sleep further compounds insulin resistance and increases cravings for high-sugar foods the next day.
Experts generally recommend setting a caffeine cut-off time at least 6 hours before bedtime to minimize these effects. For most people, this means avoiding caffeinated drinks after 2 or 3 p.m. For more information on caffeine’s impact and tips for better sleep hygiene, visit the Sleep Foundation.
8. Emotional Eating After Dark

Emotional eating in the evening, often triggered by stress, fatigue, or anxiety, is a common habit that can quietly contribute to insulin resistance. When stress levels are high—such as after a difficult day at work—many people turn to comfort foods like chocolate, chips, or pastries late at night. This pattern combines the negative effects of both stress hormones, like cortisol, and high-calorie foods, leading to elevated blood sugar and diminished insulin sensitivity. According to the National Institutes of Health, chronic stress and emotional eating are closely linked to an increased risk of metabolic syndrome and type 2 diabetes.
Imagine coming home after a stressful meeting or missed deadline, seeking solace in a pint of ice cream or a bag of cookies. While this may provide temporary relief, it sets up a cycle of emotional eating and metabolic imbalance. The body’s stress response already increases blood sugar, and adding high-sugar or high-fat foods exacerbates the strain on insulin regulation.
To break this cycle, try adopting healthier coping mechanisms such as journaling, deep breathing, or going for a short walk. For more strategies on managing stress and emotional eating, explore resources from the HelpGuide.
9. Eating Large, Heavy Dinners

Consuming oversized, calorie-dense dinners can put significant strain on your body’s insulin response, particularly when eaten late in the evening. When you have a large meal—such as a multi-course restaurant dinner featuring appetizers, creamy pasta, bread, and dessert—your pancreas is forced to release a substantial amount of insulin to manage the sudden influx of carbohydrates and fats. This excessive demand can lead to higher post-meal blood glucose levels and, over time, diminish the body’s insulin sensitivity. Studies, including those published by the National Institutes of Health, show that high-calorie evening meals are associated with greater risk for metabolic syndrome and type 2 diabetes.
Heavy dinners also interfere with quality sleep and overnight metabolic repair, compounding the negative effects on hormonal balance and glucose regulation. In contrast, lighter evening meals that are balanced in protein, healthy fats, and complex carbohydrates support steadier blood sugar and improved metabolic health.
Nutrition experts suggest making lunch the largest meal of the day and opting for smaller, portion-controlled dinners. Aim to fill half your plate with vegetables, a quarter with lean protein, and a quarter with whole grains. For more practical meal size guidance, visit the Harvard T.H. Chan School of Public Health.
10. Skipping Evening Physical Activity

Forgoing any form of physical activity in the evening can negatively impact glucose control and insulin sensitivity. Even light movement after dinner—such as a brisk walk, gentle stretching, or a short yoga session—promotes glucose uptake by muscles and helps regulate blood sugar levels. According to research from the National Institutes of Health, post-meal activity can significantly reduce postprandial glucose spikes, supporting better metabolic health over time.
In contrast, entirely sedentary evenings—spent sitting on the couch, working at a computer, or lying in bed—deprive the body of the muscle contractions necessary for optimal glucose transport. This lack of movement allows blood sugar to remain elevated for longer, increasing the risk of developing insulin resistance and related conditions such as type 2 diabetes.
Simple routines can make a substantial difference: try taking a 10- to 20-minute walk after dinner, practicing a short bodyweight exercise circuit, or following a gentle evening yoga video. These activities not only support healthy glucose metabolism but also aid digestion and improve sleep quality. For more ideas on easy evening movement routines, visit the Centers for Disease Control and Prevention.
11. Eating Dinner Too Close to Bedtime

Eating dinner too close to bedtime can significantly disrupt overnight glucose regulation and compromise insulin sensitivity. When a meal is consumed late in the evening, the body’s ability to efficiently process and store glucose is reduced due to the natural circadian decline in metabolic activity. Research from the National Institutes of Health shows that late-night eating is associated with higher nocturnal blood sugar and impaired overnight fat metabolism, increasing the risk for metabolic syndrome and type 2 diabetes.
Consider two household routines: one family consistently eats dinner by 6:00 p.m., allowing for several hours of digestion and activity before sleep, while another frequently sits down to dinner at 9:00 p.m., heading to bed soon after. The first routine enables optimal insulin response and overnight metabolic repair, while the latter leads to persistent elevated blood glucose into the night, contributing to long-term metabolic stress.
Experts generally recommend finishing dinner at least 2-3 hours before bedtime to allow for proper digestion and hormone regulation. Adopting this cut-off can help stabilize blood sugar, support restful sleep, and protect insulin sensitivity. For more on optimal meal timing, visit the Sleep Foundation.
12. Relying on Takeout or Fast Food

Frequent reliance on takeout or fast food for dinner can undermine insulin sensitivity due to the typically high fat, sugar, and calorie content of these meals. Many drive-thru and delivery options—such as burgers, fries, fried chicken, or sugary beverages—are loaded with refined carbohydrates, saturated fats, and hidden sugars. This combination can cause rapid blood sugar spikes and increased insulin demand, which, over time, contributes to insulin resistance and higher risk for metabolic disorders. The Centers for Disease Control and Prevention notes that regular consumption of fast food is associated with increased incidence of type 2 diabetes and obesity.
Picture a typical evening: after a long workday, grabbing takeout from a drive-thru or ordering a pizza seems convenient, but these foods often offer little nutritional value and are packed with ingredients that challenge your body’s metabolic balance. The lack of fiber and essential nutrients in many fast food options further exacerbates blood sugar management issues.
To make healthier choices, try selecting menu items that emphasize grilled proteins, vegetables, and whole grains, and avoid sugary drinks. Preparing simple meals at home, even a few nights a week, can dramatically improve nutritional quality. For more tips on making smart takeout choices, visit the American Heart Association.
13. Overeating Out of Boredom

Boredom-driven eating is a common evening pitfall that can quietly undermine insulin sensitivity. When you’re home alone at night, perhaps watching TV or scrolling through your phone, it’s easy to reach for snacks—not out of hunger, but to fill the void of inactivity. This type of mindless eating typically involves high-sugar or high-fat foods, which cause unnecessary blood sugar spikes and place extra demands on insulin regulation. According to the Harvard T.H. Chan School of Public Health, eating without awareness can lead to overeating, weight gain, and increased risk of metabolic syndrome.
Imagine a quiet evening at home, boredom sets in, and suddenly you find yourself finishing a bag of chips or a carton of ice cream. This cycle of eating for entertainment rather than nourishment drives repeated insulin surges, which over time can dull the body’s response to insulin and disrupt healthy glucose metabolism.
Practicing mindful eating can help break the link between boredom and overeating. Try pausing to assess your hunger cues before reaching for a snack, focusing on portion sizes, and savoring each bite. For practical mindful eating exercises and strategies, visit the Centers for Disease Control and Prevention.
14. Consuming Sugary Drinks at Night

Drinking sugary beverages such as sodas, fruit juices, or sweetened teas in the evening can have a pronounced negative effect on blood glucose regulation and insulin sensitivity. These drinks contain high amounts of added sugars, which are rapidly absorbed and cause swift spikes in blood sugar levels. The Centers for Disease Control and Prevention warns that consuming sugary drinks is a major contributor to insulin resistance and an increased risk for type 2 diabetes, especially when consumed regularly at night.
Consider a typical family dinner scenario: along with the meal, glasses of soda or sweetened juice are poured for everyone. While this may seem like a harmless tradition, the glycemic load of these beverages can tax the pancreas and disrupt overnight glucose control. Repeated exposure to high sugar intake at night can dull the body’s natural insulin response and exacerbate metabolic problems over time.
Healthier beverage alternatives include water, sparkling water with a splash of lemon or lime, herbal teas, or unsweetened iced tea. Making these swaps not only supports better blood sugar management but also reduces overall calorie intake. For more ideas on healthy drinks, visit the Harvard T.H. Chan School of Public Health.
15. Eating While Distracted
Eating while distracted—such as browsing your phone, watching TV, or working at your computer—can significantly impair your body’s natural satiety cues and disrupt insulin control. When attention is divided, the brain receives weaker signals of fullness, often leading to overeating and erratic blood sugar responses. Research from the National Institutes of Health indicates that distracted eating is associated with higher calorie intake, poorer meal satisfaction, and an increased risk of metabolic disturbances.
Picture a common scenario: you sit down for dinner with your smartphone in hand, scrolling through messages or social media. Without realizing it, you consume larger portions and eat more quickly, making it difficult for your body to gauge hunger and fullness. This pattern can result in post-meal blood sugar spikes and greater insulin demand, gradually undermining metabolic health over time.
To foster mindful eating, try creating a dedicated mealtime environment free from screens and other distractions. Focus on the flavors, textures, and aromas of your food, chew slowly, and pause between bites to check in with your hunger cues. For additional mindful eating strategies and their benefits for metabolic health, visit the Harvard T.H. Chan School of Public Health.
16. Frequent Small Evening Meals

Constant grazing on small meals or snacks throughout the evening can lead to persistent elevations in insulin levels, ultimately lowering insulin sensitivity. Each time you eat, even a small amount, your pancreas releases insulin to manage the incoming glucose. When this cycle repeats several times during the evening—such as nibbling on crackers, cheese, fruit, and sweets between dinner and bedtime—your body never gets a chance to allow insulin levels to drop and reset. Research published by the National Institutes of Health has shown that frequent eating patterns, especially in the evening, can be detrimental to metabolic health compared to structured meals.
In contrast, consuming balanced, well-timed meals spaced several hours apart gives your body the opportunity to process nutrients efficiently and maintain a healthy insulin rhythm. This structured approach supports better blood sugar control and reduces the risk of developing insulin resistance.
To optimize metabolic health, aim to finish your last meal or snack at least two to three hours before bedtime and avoid unnecessary grazing in the evening. Establishing a set meal schedule and practicing mindful eating can help break the cycle of constant snacking. For more on meal timing and spacing, visit the Harvard T.H. Chan School of Public Health.
17. Skipping Fiber at Dinner
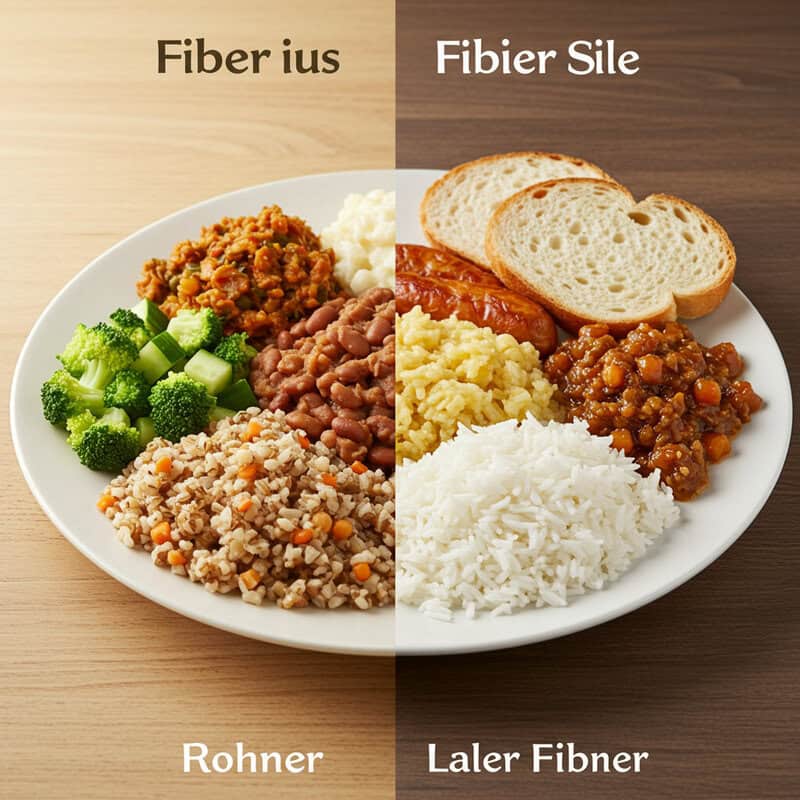
Neglecting to include fiber in your evening meal can have a substantial impact on glucose moderation and insulin sensitivity. Fiber slows the absorption of carbohydrates, leading to more gradual increases in blood sugar and reduced demand for insulin. Without enough fiber, easily digested carbs—like those in white bread, white rice, or sugary sides—can cause rapid spikes in blood glucose. The Harvard T.H. Chan School of Public Health emphasizes that fiber is essential for steady glucose regulation and long-term metabolic health.
Consider this comparison: a dinner of white-bread sandwiches and chips versus a grilled chicken salad loaded with leafy greens, beans, and roasted vegetables. The former provides little fiber, resulting in a quick blood sugar surge, while the latter’s fiber content ensures slower digestion, greater satiety, and a more stable insulin response.
For optimal metabolic health, make fiber-rich foods a consistent part of your dinner routine. Incorporate vegetables, whole grains, beans, lentils, nuts, and seeds into your meals, and aim to fill at least half your plate with produce. For practical tips on boosting fiber intake and meal planning, visit the Centers for Disease Control and Prevention.
18. Not Drinking Enough Water in the Evening

Proper hydration is a vital but often overlooked factor in maintaining healthy insulin function. Water supports efficient circulation, aids in the transport of glucose and insulin throughout the body, and helps the kidneys flush out excess sugar. When you don’t drink enough water in the evening, dehydration can set in, making it harder for your body to regulate blood sugar levels and potentially contributing to insulin resistance. A study highlighted by the National Institutes of Health demonstrates that even mild dehydration impairs glucose metabolism and increases the concentration of blood sugar.
Consider the difference between sipping water with your evening meal and throughout the night versus going hours without drinking, leading to dry mouth and sluggishness by bedtime. Chronic dehydration can trigger the release of stress hormones like vasopressin, which in turn can raise blood sugar and strain insulin regulation.
To optimize hydration and support metabolic health, aim to consume water consistently with your dinner and in the hours leading up to sleep. Avoid sugary sodas or caffeinated beverages late at night. For more guidance on optimal daily fluid intake and the link between hydration and metabolic health, visit the Centers for Disease Control and Prevention.
19. Eating High-Glycemic Foods at Night

Consuming high-glycemic foods—such as white pasta, white rice, potatoes, or sugary snacks—in the evening can trigger rapid spikes in blood sugar and force the pancreas to produce large amounts of insulin. These starchy or sugary foods are quickly digested and absorbed, leading to abrupt increases in glucose levels that challenge insulin regulation and can, over time, erode insulin sensitivity. The Harvard T.H. Chan School of Public Health notes that frequent consumption of high-glycemic foods is linked to a greater risk of type 2 diabetes and metabolic dysfunction.
Picture a typical dinner of a large bowl of white pasta or a plate of white rice and bread. While satisfying in the moment, these choices can cause blood sugar to surge, especially when eaten late in the day when the body’s natural insulin sensitivity is already declining. Repeated patterns like this in the evening can quietly undermine metabolic health.
To support better glucose control, opt for low-glycemic swaps such as whole grain pasta, brown rice, quinoa, lentils, or roasted non-starchy vegetables. These alternatives are digested more slowly, resulting in steadier blood sugar and a more balanced insulin response. For a comprehensive list of low-glycemic foods, visit the American Diabetes Association.
20. Ignoring Portion Sizes

Overlooking proper portion sizes during evening meals can have a significant impact on insulin sensitivity and metabolic health. Eating oversized portions, especially of calorie-dense or carbohydrate-rich foods, floods the bloodstream with glucose and places excessive demands on the pancreas to produce insulin. This phenomenon, often referred to as “portion distortion,” is increasingly common in settings like buffet-style dinners or family gatherings, where it’s easy to lose track of how much food is being consumed. The Centers for Disease Control and Prevention highlights that large portion sizes are strongly linked to overeating and higher risks of insulin resistance and weight gain.
Consider a buffet dinner where multiple servings of pasta, bread, and desserts are freely available. Without mindful attention to portion sizes, it’s easy to pile up your plate and eat well past satiety, leading to elevated blood sugar long after the meal is over. Consistently eating more than your body needs, especially at night, undermines insulin regulation and sets the stage for metabolic dysfunction.
To keep portions in check, use smaller plates, serve food in the kitchen rather than at the table, and pay close attention to hunger and fullness cues. For practical portion control strategies, visit the Harvard T.H. Chan School of Public Health.
21. Eating Out of Habit, Not Hunger

Engaging in habitual evening eating—snacking simply because it’s part of your nightly routine rather than due to true hunger—can quietly impair insulin sensitivity over time. When you eat out of habit, such as grabbing a snack every time you sit down to watch TV in the evening, your body is prompted to release insulin unnecessarily. This constant, low-level stimulation of insulin release increases the risk of developing insulin resistance, as highlighted by research from the National Institutes of Health.
For instance, many people associate TV time with snack time, reaching for popcorn, chips, or sweets even if they had a satisfying dinner just an hour before. This mindless habit trains your body to expect food at certain times, regardless of energy needs, contributing to excessive calorie intake and erratic blood sugar patterns.
To break this cycle, learn to distinguish between real hunger and habitual cravings. Before reaching for a snack, pause to check for physical signs of hunger, such as a growling stomach or low energy. If you aren’t truly hungry, try drinking water, engaging in a non-food-related activity, or practicing mindful distraction. For more on recognizing hunger cues, visit the Centers for Disease Control and Prevention.
22. Opting for Highly Processed Foods

Regularly choosing highly processed foods for evening snacks or meals can significantly disrupt insulin function and overall metabolic health. These foods—such as chips, cookies, packaged pastries, and microwave dinners—are often loaded with refined carbohydrates, added sugars, unhealthy fats, and artificial additives. Such ingredients are rapidly digested, resulting in quick blood sugar spikes and heavy insulin demands. According to the Harvard T.H. Chan School of Public Health, frequent consumption of processed foods is closely linked to increased risk of insulin resistance, obesity, and type 2 diabetes.
Consider the scenario of reaching for a bag of chips or a sleeve of cookies during a quiet evening at home. While convenient and satisfying in the moment, these snacks offer little nutritional value and prompt repeated glucose surges that challenge your body’s insulin regulation. Over time, this pattern can dull metabolic response and promote chronic disease.
To protect your insulin sensitivity, swap highly processed foods for whole, minimally processed alternatives. Choose snacks like raw vegetables with hummus, a handful of unsalted nuts, or fresh fruit. Emphasizing whole foods supports steadier blood sugar levels and provides essential nutrients. For more ideas on healthy swaps, visit the Centers for Disease Control and Prevention.
23. Eating Alone and Unmindfully

Eating alone and without mindfulness can negatively influence both your eating behaviors and your body’s insulin response. Social and mindful eating tend to promote slower, more deliberate food consumption, which helps regulate appetite hormones and supports more stable blood sugar levels. According to the Harvard T.H. Chan School of Public Health, mindful eating practices can reduce overeating and improve metabolic outcomes by enhancing awareness of hunger and fullness cues.
In contrast, solitary and unmindful eating—such as eating quickly in front of the TV or while distracted by work—often leads to larger portion sizes and rapid consumption. Without social cues or conscious attention to your meal, it’s easier to miss signals of satiety, resulting in unnecessary insulin spikes and increased risk of insulin resistance.
To make dinners more mindful, try setting the table and removing digital distractions, even if you’re dining solo. Take time to notice the flavors, textures, and presentation of your food. If possible, share meals with family or friends, as conversation naturally slows the pace of eating. For more mindful eating techniques and their benefits for metabolic health, visit the Centers for Disease Control and Prevention.
24. Relying on Quick-Fix Energy Foods

Turning to quick-fix energy foods, such as energy bars, sports drinks, or sugary snacks, can significantly spike blood sugar levels and disrupt insulin sensitivity—especially when consumed in the evening. Many of these products are marketed for convenience or as workout fuel, but they often contain high amounts of refined sugars, syrups, and processed carbohydrates. The Harvard T.H. Chan School of Public Health cautions that energy bars and similar snacks can cause rapid glucose surges, which place unnecessary demands on the pancreas and may undermine metabolic health over time.
Imagine finishing an evening workout and reaching for a sports drink or a packaged energy bar loaded with sugar. While these options may provide a quick energy boost, they can also lead to post-exercise blood sugar spikes, followed by crashes that promote cravings and disrupt recovery.
Instead, opt for whole-food snacks that offer a balance of nutrients and support steady glucose metabolism. Good choices include a banana with a small handful of nuts, plain Greek yogurt with berries, or a slice of whole grain toast with nut butter. For more advice on choosing healthy snacks, visit the Centers for Disease Control and Prevention.
25. Eating to Soothe Anxiety

Eating to soothe anxiety—often referred to as “comfort eating”—can negatively impact insulin response and overall metabolic health. When stress and anxiety levels are high, the body releases cortisol, a hormone that raises blood sugar levels. Pairing this hormonal response with high-calorie, high-sugar comfort foods such as cookies, chips, or ice cream can lead to even more pronounced spikes in blood glucose and a greater demand for insulin. Research from the National Institutes of Health underscores the close link between emotional eating, stress, and increased risk of insulin resistance.
Consider a scenario where, after a tense day, you find yourself reaching for snacks to calm your nerves. While this pattern may provide temporary emotional relief, it quickly becomes a habit that disrupts metabolic balance and makes it harder for the body to maintain healthy blood sugar levels.
To break the cycle of anxiety-driven eating, experiment with alternative calming routines. Practices such as deep breathing exercises, meditation, gentle stretching, or taking a short walk can help soothe anxiety without triggering unhealthy blood sugar fluctuations. For more ideas on managing stress and emotional eating, visit the HelpGuide.
26. Consuming Artificial Sweeteners

The effects of artificial sweeteners on insulin sensitivity and metabolic health are a topic of ongoing debate among researchers. Some studies suggest that consuming artificial sweeteners—such as aspartame, sucralose, or saccharin, commonly found in diet sodas and sugar-free snacks—may alter gut microbiota and potentially disrupt glucose metabolism. According to the Harvard T.H. Chan School of Public Health, while these sugar substitutes don’t raise blood sugar directly, their long-term impact on insulin response is still being investigated.
For example, you might choose a diet soda with dinner, believing it to be a healthier alternative to regular soda. However, some research, including findings from the National Institutes of Health, indicates that frequent consumption of artificially sweetened beverages could be linked to metabolic disturbances and changes in insulin sensitivity over time.
Current guidance suggests using artificial sweeteners in moderation, rather than relying on them as a primary replacement for sugar. Instead, prioritize water, herbal teas, or naturally flavored sparkling water to reduce your intake of both sugar and artificial additives. For more on the science and recommendations, visit the Centers for Disease Control and Prevention.
27. Skipping Protein at Dinner

Protein plays a crucial role in stabilizing blood sugar levels and supporting healthy insulin function, especially during the evening meal. Including an adequate source of protein slows the absorption of carbohydrates, reduces post-meal glucose spikes, and promotes a feeling of fullness that prevents late-night snacking. According to the Harvard T.H. Chan School of Public Health, protein-rich meals contribute to improved glycemic control and metabolic health.
Contrast this with a dinner that consists only of a simple salad of greens and a light vinaigrette, lacking a significant protein source. While low in calories, such a meal digests quickly, potentially leading to hunger, cravings, and unstable blood sugar throughout the night. This can set the stage for overeating or choosing less healthy snacks later in the evening, which further strains insulin regulation.
To optimize your dinner for metabolic health, incorporate protein-rich foods such as grilled chicken, fish, tofu, beans, lentils, or eggs. Pair these with fiber-rich vegetables and whole grains for a balanced, satisfying meal. For more ideas on building protein into evening meals, visit the Centers for Disease Control and Prevention.
28. Eating in Low Light or in Bed

The environment in which you eat can subtly but significantly influence your eating habits and insulin regulation. Eating in dim lighting or in bed—rather than at a table in a well-lit space—often leads to more distracted eating, larger portion sizes, and less awareness of satiety cues. According to the Harvard T.H. Chan School of Public Health, mindful eating practices are more effective when meals are consumed in a dedicated, well-lit eating area, supporting better blood sugar control and healthier food choices.
Consider a scenario where you’re snacking on chips or cookies in bed while watching television late at night. This environment encourages mindless eating, making it easy to lose track of how much you’ve consumed and often resulting in excessive calorie and sugar intake. Such habits can lead to irregular insulin release and over time contribute to diminished insulin sensitivity and metabolic issues.
To create a more supportive eating environment, try to eat dinner and snacks at a dining table with sufficient lighting. Avoid eating in bed or in front of screens. Set the table, use proper utensils, and take time to savor your food, which encourages mindful eating and improved metabolic health. For more tips, visit the Centers for Disease Control and Prevention.
29. Not Tracking Evening Intake

Lack of awareness about what and how much you eat in the evening can quietly undermine insulin health. Without tracking, it’s easy to underestimate portion sizes, forget about snacks, and overlook the total amount of sugar or carbs consumed. This “hidden” intake can lead to unintended blood sugar spikes and increased insulin demand. The Centers for Disease Control and Prevention emphasizes that food awareness and tracking are key strategies for maintaining healthy blood glucose levels and preventing insulin resistance.
For example, you might snack on crackers while cooking, have a few bites of dessert after dinner, and sip a sweetened beverage while watching TV—without realizing the cumulative impact. These forgotten or mindless eating moments can add up, especially in the evening when insulin sensitivity is naturally lower.
To improve awareness, try simple tracking methods like keeping a food journal, using a smartphone app, or taking quick notes about what you eat after dinner. Even brief tracking can reveal patterns and help you make more intentional choices. For more practical tips and tools for food tracking and diabetes prevention, visit the Centers for Disease Control and Prevention.
30. Eating Under Time Pressure

Eating in a rush, especially during evening meals, can negatively impact digestion and insulin efficiency. When meals are consumed quickly—perhaps due to a late work meeting or a packed schedule—the body has less time to signal fullness, leading to overeating and erratic blood sugar responses. Fast eating may also impair digestive processes, resulting in less efficient glucose absorption and greater insulin demand. Research from the National Institutes of Health links hurried eating to an increased risk of insulin resistance and metabolic syndrome.
Imagine the scenario of finishing a late meeting and rushing through dinner in just a few minutes. This hurried approach not only increases the likelihood of larger portion sizes but also reduces enjoyment and disrupts your body’s natural ability to regulate appetite and blood glucose.
To counteract the effects of time pressure, practice mindful eating strategies: take a few deep breaths before your meal, put down utensils between bites, chew slowly, and focus on the sensory experience of eating. Even when time is tight, carving out a few extra minutes to eat mindfully can support better digestion and healthier insulin function. For more mindful eating advice, visit the Harvard T.H. Chan School of Public Health.
31. Not Allowing Digestion Before Sleep

Failing to allow sufficient time for digestion between dinner and bedtime can disrupt your body’s insulin response and overnight glucose regulation. When you eat a meal or snack shortly before lying down, your digestive system is forced to work while your metabolism is naturally slowing for sleep. This can lead to prolonged elevated blood sugar levels and increased overnight insulin production, ultimately undermining insulin sensitivity. Research from the National Institutes of Health highlights that eating close to bedtime is associated with poorer glycemic control and a greater risk for metabolic disturbances.
Consider the example of a late-night snacker who frequently eats just before heading to bed. This habit means the body is still processing food during the early stages of sleep, impairing optimal metabolic repair and hormone balance. Over time, this pattern can contribute to weight gain and reduced insulin effectiveness.
Experts generally recommend finishing your last meal or snack at least two to three hours before bedtime to allow for proper digestion and blood sugar stabilization. Establishing a consistent routine where eating ends well before sleep supports both metabolic health and quality rest. For more timing guidelines and sleep-nutrition insights, visit the Sleep Foundation.
32. Skipping Vegetables at Dinner

Leaving vegetables off your dinner plate can quietly sabotage insulin sensitivity and overall metabolic health. Vegetables provide essential fiber, vitamins, minerals, and phytonutrients that slow carbohydrate absorption, promote satiety, and support steady blood sugar levels. The Harvard T.H. Chan School of Public Health emphasizes that diets rich in vegetables are associated with a lower risk of type 2 diabetes and improved insulin response.
Contrast this with a dinner consisting of steak and mashed potatoes, but no vegetables. Such a meal is likely higher in simple carbohydrates and lower in fiber, resulting in quicker blood sugar spikes and increased insulin demand. Over time, consistently skipping vegetables can make it harder for your body to regulate glucose and may contribute to metabolic syndrome.
Adding vegetables to your dinner doesn’t have to be complicated. Toss a handful of leafy greens into pasta, roast a tray of mixed vegetables with olive oil, or add sliced bell peppers and carrots to stir-fries. Even a simple side salad can make a big difference. For more inspiration and practical ways to include more vegetables in your meals, visit the Centers for Disease Control and Prevention.
33. Eating in Response to Fatigue

Fatigue in the evening can often be mistaken for hunger, leading to unnecessary eating that challenges insulin sensitivity. When you’re tired—perhaps after a long workday or a late night on a project—your body may send signals that mimic true hunger, prompting cravings for quick energy foods like sweets or refined carbs. According to the Centers for Disease Control and Prevention, sleep deprivation and fatigue can disrupt hunger hormones and increase the risk of overeating, particularly in the evening hours.
Imagine finishing a taxing day, feeling exhausted, and automatically reaching for a snack to “perk up.” While this may provide a brief energy boost, it often results in blood sugar spikes and unnecessary insulin release, gradually undermining your metabolic health.
Instead of eating in response to fatigue, try non-food remedies to restore energy and clarity. Take a brisk walk, stretch, listen to music, or practice a few minutes of deep breathing. If you’re routinely tired in the evenings, prioritize improving your sleep schedule and quality. For more information on distinguishing fatigue from hunger and healthy ways to manage tiredness, visit the Sleep Foundation.
34. Skipping Healthy Fats at Dinner

Excluding healthy fats from your evening meal can negatively affect satiety and glucose control, both crucial for maintaining insulin sensitivity. Healthy fats—found in foods like avocados, olive oil, nuts, seeds, and fatty fish—help slow the absorption of carbohydrates, reducing post-meal blood sugar spikes and keeping you fuller for longer. According to the Harvard T.H. Chan School of Public Health, diets that include moderate amounts of unsaturated fats are associated with better metabolic health and improved glycemic response.
Compare this to a low-fat dinner, such as plain steamed vegetables with grilled chicken breast and no added fats. While low in calories, this type of meal may not promote lasting fullness, potentially leading to cravings and late-night snacking on less healthy options, which can disrupt glucose regulation and increase insulin demand.
To enhance both satisfaction and metabolic benefits, incorporate sources of healthy fats into your dinner. Drizzle olive oil over roasted vegetables, add sliced avocado to salads, sprinkle nuts or seeds on grain bowls, or include a serving of salmon or mackerel. For additional guidance on adding healthy fats to your diet, visit the Centers for Disease Control and Prevention.
35. Eating Too Quickly

Eating too quickly during dinner can overwhelm your body’s insulin response and make it harder to regulate blood sugar. When you rapidly consume food, your stomach doesn’t have time to signal fullness to your brain, increasing the risk of overeating and causing a sudden surge in blood glucose. The pancreas is then forced to release a large amount of insulin in a short period, a pattern associated with reduced insulin sensitivity over time. The National Institutes of Health reports that fast eaters are at higher risk for metabolic syndrome and type 2 diabetes than those who eat slowly.
Contrast this with a meal enjoyed at a leisurely pace, where each bite is chewed thoroughly and there are pauses between mouthfuls. Slow eating gives your digestive system time to process food, supports better blood sugar control, and allows you to recognize satiety before overeating occurs.
To slow down your eating, try setting your fork down between bites, chewing each bite at least 20 times, and taking sips of water throughout the meal. Engaging in conversation or focusing on the flavors and textures of your food can also naturally help pace your dining experience. For more mindful eating tips, visit the Harvard T.H. Chan School of Public Health.
36. Ignoring Hunger and Fullness Cues

Many people become disconnected from their natural hunger and fullness cues, especially in the evening when routines or emotions often drive eating habits. Ignoring these body signals can lead to unnecessary calorie intake and erratic blood sugar spikes, putting extra strain on insulin regulation. The Harvard T.H. Chan School of Public Health highlights that mindful recognition of hunger and satiety is key to supporting metabolic health and preventing insulin resistance.
Consider the example of automatically reaching for a snack after dinner simply because it’s part of your nightly routine, not because you’re truly hungry. This pattern often results in eating past fullness, leading to elevated blood sugar and increased insulin demand. Over time, this disconnect can dull your body’s appetite regulation and contribute to weight gain or metabolic dysfunction.
To foster mindful cue recognition, pause and assess your physical sensations before eating—ask yourself if you’re actually hungry or just eating out of habit or boredom. During meals, eat slowly and check in with your body periodically to notice when you begin to feel satisfied. For more guidance on tuning into hunger and fullness cues, visit the Centers for Disease Control and Prevention.
37. Consuming Spicy Foods That Disrupt Sleep

Eating spicy foods late in the evening—such as a hot curry or extra-peppery salsa—can lead to disrupted sleep, which in turn has negative effects on insulin sensitivity. Spicy foods may cause indigestion, heartburn, or increased body temperature, all of which can interfere with falling and staying asleep. The Sleep Foundation notes that poor or fragmented sleep is closely linked to greater insulin resistance and impaired glucose regulation, even after just one restless night.
For example, enjoying a spicy dinner of curry or chili close to bedtime might seem satisfying, but it can cause nighttime discomfort, frequent awakenings, or even insomnia. This lack of restorative sleep leaves the body less able to process glucose efficiently the next day, increasing cravings for high-sugar foods and taxing the pancreas further.
To promote better sleep and metabolic health, opt for milder, easily digestible meals in the evening. Choose lean proteins, whole grains, and steamed or roasted vegetables, and save spicy dishes for earlier in the day. For more advice on sleep-friendly nutrition and the impact of diet on rest, visit the Sleep Foundation.
38. Eating Due to Social Pressure

Evening gatherings with friends or family can create an environment where social pressure leads to overeating and, consequently, places extra strain on insulin sensitivity. At parties, dinners, or celebrations, it’s common to feel compelled to eat more than you need—whether out of politeness, to fit in, or simply because tempting foods are readily available. The Harvard T.H. Chan School of Public Health notes that social eating often results in consuming larger portions and more calorie-dense foods, which can trigger blood sugar spikes and increase insulin demand.
Picture a party scenario where platters of appetizers, desserts, and drinks are constantly within reach. Even if you’re not particularly hungry, you may find yourself grazing throughout the evening or accepting food and drink to avoid seeming rude. This pattern of eating due to social cues rather than genuine hunger can undermine your ability to regulate glucose and maintain metabolic balance.
To navigate social eating, set intentions before events—decide what and how much you’ll eat, and practice politely declining extra servings. Focus on conversation and connection rather than just the food, and try to fill your plate with healthier options when possible. For more social eating strategies, visit the Centers for Disease Control and Prevention.
39. Not Planning Evening Meals

Failing to plan your evening meals can easily result in poor dietary choices that negatively impact insulin sensitivity. Without a plan, you’re more likely to reach for convenient, processed, or high-sugar foods when hunger strikes, especially after a long day. This reactive approach often leads to meals that are low in nutrients and high in refined carbohydrates, causing sharp blood sugar spikes and increased insulin demand. The Centers for Disease Control and Prevention highlights meal planning as a key strategy for preventing diabetes and supporting metabolic health.
Consider the common scenario of arriving home late and realizing there’s nothing prepared for dinner. You might opt for takeout, microwaveable entrees, or snacks like chips and cookies, simply for convenience. While expedient, these choices rarely provide the balance of fiber, protein, and healthy fats needed for stable blood sugar regulation.
To avoid last-minute scrambles, dedicate a little time each week to meal planning and prepping ingredients. Batch-cook grains, chop vegetables, or marinate proteins ahead of time. Keeping healthy staples on hand makes it much easier to assemble a nutritious dinner, even when you’re short on time. For meal prep tips and recipes, visit the Harvard T.H. Chan School of Public Health.
40. Eating Foods High in Trans Fats

Consuming foods high in trans fats can significantly impair insulin function and increase the risk of metabolic disorders. Trans fats, often found in packaged snacks, baked goods, and fried fast foods, promote inflammation and interfere with the body’s ability to regulate glucose. The Harvard T.H. Chan School of Public Health warns that even small amounts of trans fat can raise bad cholesterol, lower good cholesterol, and directly contribute to insulin resistance and type 2 diabetes.
For example, grabbing a few commercially baked cookies or a bag of microwave popcorn while watching TV in the evening may seem harmless, but these snacks often contain partially hydrogenated oils—a primary source of trans fats. Over time, regular intake of such products can quietly erode metabolic health and make it harder for your body to manage blood sugar effectively.
To protect your insulin sensitivity, become a diligent label reader. Look for terms like “partially hydrogenated oils” on ingredient lists and avoid these products whenever possible. Choose snacks made with whole ingredients, such as nuts, seeds, or homemade baked goods using healthy oils. For more information on trans fats and how to avoid them, visit the Centers for Disease Control and Prevention.
41. Overindulging in Dairy at Night

Dairy products have a complex relationship with insulin sensitivity and digestion, particularly when consumed in large amounts during the evening. While moderate dairy intake can provide protein and beneficial nutrients like calcium, overindulging in heavy dairy products—such as large portions of cheese, creamy sauces, or full-fat ice cream—may lead to digestive discomfort and disrupt blood sugar regulation. Some research, including insights from the Harvard T.H. Chan School of Public Health, indicates that certain dairy proteins can trigger a strong insulin response, especially when paired with high glycemic foods or consumed in excess.
For instance, ending your evening with a large bowl of ice cream or cheese-laden pasta can overload your digestive system and promote a rapid insulin surge, potentially affecting overnight glucose balance and sleep quality. In contrast, lighter dairy options—such as a small serving of plain Greek yogurt or a slice of low-fat cheese—are less likely to cause digestive or metabolic issues when eaten in moderation.
To support metabolic health, limit heavy, rich dairy foods at night and stick to modest portions. Combine dairy with fiber-rich foods, like fruit or whole grains, to slow digestion and promote stable blood sugar. For more on dairy’s health effects and serving guidelines, visit the Centers for Disease Control and Prevention.
42. Eating Salty Snacks Late

Consuming salty snacks late in the evening—such as chips, pretzels, or salted nuts—not only contributes to excessive sodium intake but can indirectly affect insulin sensitivity. High salt intake may increase blood pressure and stimulate the release of stress hormones like cortisol and adrenaline, both of which can raise blood sugar levels and impair insulin action. The Harvard T.H. Chan School of Public Health notes that excessive sodium is linked with cardiovascular risk and metabolic disturbances.
For example, reaching for a bag of chips while relaxing at night can set off a cascade of effects: the salt prompts water retention, raises blood pressure, and may trigger hormonal responses that disrupt glucose metabolism. Over time, these patterns can contribute to both insulin resistance and overall poor health.
To reduce risk, be mindful of your salt intake, especially in the evening. Opt for unsalted or lightly salted snacks, and flavor foods with herbs, spices, or lemon instead of salt. Read labels to identify hidden sodium in packaged foods. For more helpful tips on lowering sodium and its impact on health, visit the Centers for Disease Control and Prevention.
43. Choosing Refined Grains for Dinner

Selecting refined grains—such as white bread, white rice, or regular pasta—for your evening meal can prompt rapid spikes in blood glucose and increased insulin demand. Refined grains are stripped of fiber and essential nutrients during processing, causing them to digest and absorb quickly. This leads to a swift rise in blood sugar, which over time can contribute to insulin resistance and metabolic dysfunction. The Harvard T.H. Chan School of Public Health highlights that diets high in refined grains are associated with a greater risk of type 2 diabetes and cardiovascular disease.
For instance, a dinner of white bread with butter or a large serving of white rice offers little to buffer the glucose surge, in contrast to meals that use whole grain alternatives. Whole grains like brown rice, quinoa, whole wheat bread, or barley digest more slowly, promoting gradual rises in blood sugar and supporting better insulin sensitivity.
To make healthier swaps, replace white bread with whole grain varieties, opt for brown or wild rice instead of white, and choose whole wheat or legume-based pasta. For more suggestions and the benefits of whole grains, visit the Centers for Disease Control and Prevention.
44. Eating Because Food Is Available

Environmental cues, such as visible snacks or an open pantry, can strongly influence eating behaviors—even when you’re not truly hungry. This tendency to eat simply because food is present can lead to excess calorie consumption, frequent blood sugar spikes, and chronic insulin overload. The Harvard T.H. Chan School of Public Health highlights that mindless eating driven by external cues rather than internal hunger is a major contributor to weight gain and metabolic issues.
Picture a common scenario: you walk into the kitchen after dinner, see an open bag of cookies or a bowl of candy on the counter, and automatically start snacking. This response bypasses natural hunger and fullness cues and can become a nightly pattern that strains insulin sensitivity over time.
To reduce overeating triggered by food availability, manage your environment by keeping tempting snacks out of sight—store treats in opaque containers or higher cabinets and keep countertops clear of packaged foods. Instead, display healthy options such as fresh fruit or pre-cut vegetables. Practicing mindful eating and asking yourself if you’re truly hungry before reaching for food can also help. For more environment management strategies, visit the Centers for Disease Control and Prevention.
45. Relying on “Healthy” Packaged Foods

Many packaged foods marketed as “healthy”—such as granola bars, protein snacks, or low-fat crackers—can be misleading and may still undermine insulin sensitivity. Despite claims like “whole grain,” “natural,” or “low sugar,” these products often contain added sugars, refined flours, artificial sweeteners, and unhealthy fats. The Harvard T.H. Chan School of Public Health cautions that processed and packaged foods can cause rapid blood sugar spikes and contribute to insulin resistance, regardless of their front-of-package health claims.
For example, grabbing a granola bar for an evening snack might seem like a smart choice. However, a closer look at the label may reveal high amounts of added sugars, syrups, or refined grains, all of which prompt a swift insulin response similar to less “healthy” treats. Relying on these foods regularly in the evening can quietly erode metabolic health.
To make truly healthier choices, always read nutrition and ingredient labels—look for high fiber, low added sugar, and minimal processing. Favor whole food snacks like fruit, nuts, or plain Greek yogurt over packaged alternatives whenever possible. For more label reading tips and healthy snacking guidance, visit the Centers for Disease Control and Prevention.
46. Eating to Reward Yourself at Night
Using food as a reward at night—such as indulging in dessert or a favorite snack after a long day—can establish a pattern that disrupts both dopamine regulation and insulin sensitivity. Reward-based eating activates the brain’s pleasure centers, triggering dopamine release, which can reinforce the habit of turning to food for comfort or celebration. Over time, this cycle can lead to overeating, repeated blood sugar spikes, and increased insulin demand. The Harvard T.H. Chan School of Public Health notes that emotional and reward-driven eating is a key driver of weight gain and metabolic dysfunction.
Imagine coming home after a stressful day and automatically reaching for ice cream as a “treat.” While this may provide a fleeting sense of relief, it can quickly become a nightly habit that undermines your body’s ability to regulate glucose and insulin, especially if paired with inactivity or additional late-night snacking.
To break the cycle of food-based rewards, explore alternative self-care practices that support relaxation and well-being without disrupting metabolic health. Consider taking a warm bath, reading a favorite book, practicing gentle yoga, or spending time with loved ones. For more ideas on healthy self-care routines, visit the HelpGuide.
47. Not Prioritizing Evening Relaxation
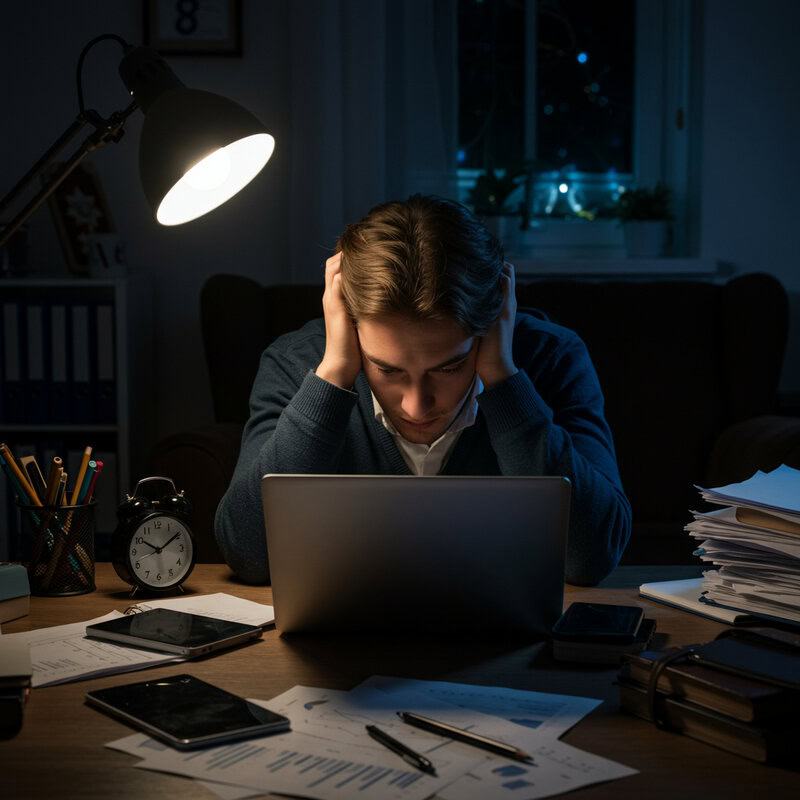
Neglecting relaxation in the evening can have a profound effect on insulin sensitivity and overall metabolic health. Chronic stress triggers the release of cortisol and other stress hormones, which elevate blood glucose levels and, over time, contribute to insulin resistance. According to the Centers for Disease Control and Prevention, managing stress is a critical component of diabetes prevention and healthy glucose regulation.
Consider the scenario of a busy evening routine: juggling chores, checking work emails, or running errands late into the night, leaving little time to decompress. This constant state of stimulation keeps stress hormone levels elevated, making it harder for your body to maintain balanced blood sugar and optimal insulin function.
To foster relaxation and metabolic health, set aside dedicated time each evening for calming activities. Techniques such as deep breathing, progressive muscle relaxation, gentle stretching, meditation, or listening to soothing music can help lower cortisol levels and support a healthy hormonal balance. Even just a few minutes of intentional relaxation can make a difference. For more stress management strategies and their benefits for metabolic health, visit the HelpGuide.
48. Eating While Working at Night

Eating while working at night can quietly disrupt your ability to recognize satiety cues and maintain stable blood glucose levels. The mental distraction of work—such as answering emails, preparing reports, or browsing documents on a laptop—diverts attention from your meal. This often leads to mindless overeating, larger portions, and rapid consumption, which can cause post-meal blood sugar spikes and place additional strain on insulin regulation. The Harvard T.H. Chan School of Public Health highlights that multitasking during meals is associated with poorer metabolic outcomes and increased risk of weight gain.
For example, you might sit at the dining table with your laptop after hours, eating dinner or snacking absentmindedly as you work. This habit makes it difficult to notice when you are full and can result in eating more than intended—potentially leading to insulin resistance over time if practiced regularly.
To foster healthier habits, set clear boundaries between meals and work. Designate a screen-free time and space for eating, and give yourself permission to focus solely on your food. Taking these steps not only supports mindful eating but also allows your body to better regulate blood sugar. For more mindful eating and boundary-setting tips, visit the Centers for Disease Control and Prevention.
49. Ignoring Blood Sugar Monitoring

Regular blood sugar monitoring is a crucial yet often overlooked habit for anyone at risk of insulin resistance, prediabetes, or diabetes. Monitoring allows you to detect trends, understand how different evening habits affect your glucose levels, and make timely adjustments to your routine. For those with risk factors—such as a family history of diabetes, overweight, or a sedentary lifestyle—using a home glucometer can provide valuable insights and early warnings before symptoms become severe. The Centers for Disease Control and Prevention recommends regular screening and self-monitoring to improve outcomes and prevent complications.
Consider a scenario where you have a glucometer at home but rarely use it, or only check your blood sugar when feeling unwell. Without consistent monitoring, it’s easy to miss subtle changes—such as elevated readings after late-night snacking or eating high-glycemic foods—that quietly erode insulin sensitivity over time.
To stay proactive, set a regular schedule for blood sugar checks, especially in the evening or after trying different foods. Keep a log to track patterns and share results with your healthcare provider. For more information on who should monitor and how to use a glucometer effectively, visit the Centers for Disease Control and Prevention.
50. Failing to Seek Support for Habit Change

Attempting to change long-standing evening habits that undermine insulin sensitivity can be challenging without the encouragement and accountability of a support network. Research consistently shows that people are more successful in making and sustaining healthy behavioral changes when they have social support, whether from friends, family, or community groups. The Centers for Disease Control and Prevention emphasizes the value of accountability and connection for managing both diabetes and lifestyle habits.
For example, joining a group challenge—such as a workplace wellness initiative, a family commitment to cook healthy dinners, or an online community aiming to reduce nighttime snacking—can boost motivation and provide practical tips, feedback, and shared victories. Having others to check in with or celebrate milestones makes it easier to stay on track, learn from setbacks, and make sustainable progress.
If you feel stuck or isolated in your efforts, seek out resources like local support groups, registered dietitians, or online forums dedicated to metabolic health. Professional counseling or diabetes education programs can also provide guidance and tools for lasting change. For more ideas on finding support and building accountability, visit the HelpGuide.
Conclusion
Addressing the small, often overlooked evening habits that impact insulin sensitivity is critical for preventing metabolic disorders and safeguarding long-term health. As modern lifestyles introduce countless subtle threats to glucose regulation, reflecting on your nighttime routines can reveal opportunities for positive change. Whether it’s meal timing, snack choices, or stress management, even minor adjustments can yield significant benefits. For those with risk factors such as family history, weight concerns, or persistent fatigue, regular blood sugar screening is highly recommended. Early intervention is key to reversing insulin resistance before it escalates. For more guidance on diabetes prevention and healthy habits, visit the Centers for Disease Control and Prevention.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





