Tips on How To Prevent Colorectal Cancer
Colorectal cancer is a significant health concern, with over 150,000 new cases annually in the US and more than 42,000 in the UK, according to the American Cancer Society and Cancer Research UK. This cancer affects the colon and rectum, vital parts of the digestive system responsible for processing waste. A key challenge is that symptoms often appear late, making early detection and prevention critically important for improving outcomes.
1. Know Your Family History

Understanding your family’s medical background is essential in assessing your risk for colorectal cancer. Genetic factors play a significant role, with individuals who have a first-degree relative (parent, sibling, or child) diagnosed with colorectal cancer facing up to twice the risk compared to those without such a history. According to the Centers for Disease Control and Prevention (CDC), about 1 in 3 people who develop colorectal cancer have family members who have also been affected.
To accurately gauge your risk, gather detailed family medical records, including information about relatives who have had colorectal polyps or related cancers, and the ages at which diagnoses occurred. This information should be regularly updated and shared with your healthcare provider, as it can influence screening recommendations and preventive strategies. For more guidance on collecting and documenting your family’s health history, consult resources such as the National Human Genome Research Institute. Open and honest communication about hereditary risks empowers both you and your healthcare team to take proactive, personalized steps in colorectal cancer prevention.
2. Get Screened Regularly

Routine screening is one of the most effective ways to detect colorectal cancer early, when treatment is most successful. Screening tests such as colonoscopy, flexible sigmoidoscopy, and stool-based tests can identify precancerous polyps or early-stage cancers before symptoms develop. Much like regular health checkups help catch other conditions early, colorectal screenings play a vital role in preventive healthcare. The CDC and NHS both emphasize the proven benefits of these tests in reducing colorectal cancer incidence and mortality.
Current guidelines recommend that people at average risk begin screening at age 45, although those with higher risk factors—such as a family history or certain genetic conditions—may need to start earlier. Speak with your healthcare provider to determine the most appropriate screening schedule and method for you. Early detection through regular screening not only increases the likelihood of successful treatment but can also prevent cancer altogether by removing polyps before they become malignant. For more details on screening options, visit the American Cancer Society.
3. Maintain a Healthy Weight

Research has established a strong connection between obesity and an increased risk of developing colorectal cancer. Individuals with a higher body mass index (BMI) face a greater likelihood of being diagnosed with this disease compared to those in a healthy weight range. According to the American Cancer Society, people with obesity are 30% more likely to develop colorectal cancer than individuals with a normal BMI.
Maintaining a healthy weight not only lowers cancer risk but also supports overall health and well-being. Simple, realistic strategies include incorporating regular physical activity, such as brisk walking or cycling, into your daily routine and making gradual dietary changes—like increasing fruit, vegetable, and whole grain intake while reducing processed foods and sugary beverages. Even modest weight loss can have significant health benefits. Setting achievable goals, tracking progress, and seeking support from healthcare professionals or nutritionists can greatly enhance your success. For guidance on healthy weight management and its role in cancer prevention, visit the Cancer Research UK website for evidence-based tips and resources.
4. Eat More Fiber

Dietary fiber plays a vital role in supporting colon health and lowering the risk of colorectal cancer. Fiber helps keep the digestive system functioning smoothly by promoting regular bowel movements and reducing the time potentially harmful substances stay in contact with the colon lining. Multiple studies, including findings from the World Cancer Research Fund, have shown that individuals who consume high-fiber diets have a significantly reduced risk of developing colorectal cancer compared to those who eat low-fiber diets.
High-fiber diets are rich in fruits, vegetables, legumes, whole grains, and nuts. For example, foods like beans, lentils, oats, brown rice, apples, pears, broccoli, and carrots are excellent sources of fiber. In contrast, diets low in fiber—often high in processed and refined foods—are linked to higher rates of colorectal cancer. Experts recommend adults aim for at least 25 to 30 grams of fiber daily, primarily from food sources. Gradually increasing fiber intake and drinking plenty of water can help your body adjust. For more information on the benefits of fiber and practical ways to add it to your diet, visit the NHS guide to fiber.
5. Limit Red and Processed Meats

There is substantial evidence linking the consumption of red and processed meats to an increased risk of colorectal cancer. According to the Cancer Research UK, eating large amounts of beef, pork, lamb, sausages, bacon, and ham can elevate your risk due to chemicals generated during processing and cooking. In contrast, plant-based diets, which emphasize legumes, whole grains, vegetables, and nuts, are associated with a lower risk of colorectal cancer and offer protective nutrients and fiber.
Experts, including those at the World Health Organization, recommend limiting red meat intake to no more than three portions per week (about 350-500g cooked weight) and minimizing processed meat as much as possible. Practical alternatives include swapping red or processed meats for poultry, fish, beans, lentils, tofu, and other plant proteins. Grilling a salmon fillet, preparing a chickpea salad, or opting for a vegetable stir-fry are delicious and nutritious ways to reduce meat consumption. Gradual dietary shifts make it easier to adopt healthier habits for long-term colorectal health.
6. Exercise Regularly

Regular physical activity plays a significant role in protecting against colorectal cancer. Exercise helps regulate digestion, reduces inflammation, and supports a healthy immune system, all of which contribute to lowering cancer risk. According to the American Cancer Society, people who maintain active lifestyles have a considerably lower risk of developing colorectal cancer compared to those who lead sedentary lives.
Sedentary behavior, such as prolonged sitting or lack of regular movement, is associated with increased colorectal cancer risk and other chronic health issues. In contrast, even moderate activity such as brisk walking, cycling, or gardening for at least 150 minutes per week can provide substantial protective benefits. To fit more exercise into your daily routine, consider walking or biking to work, taking the stairs instead of the elevator, or scheduling regular movement breaks during the day. Engaging in activities you enjoy, like dancing, swimming, or playing sports, makes it easier to stay consistent. The NHS exercise guide offers practical tips and routines to help you get started and stay motivated on your journey to better health.
7. Quit Smoking

Smoking is a well-established risk factor for many cancers, including colorectal cancer. Chemicals found in tobacco can damage the cells lining the colon and rectum, increasing the likelihood of cancerous changes over time. According to the National Cancer Institute, smokers are about 18% more likely to develop colorectal cancer compared to non-smokers, and the risk increases with the duration and intensity of smoking.
Quitting smoking significantly reduces your risk, not only for colorectal cancer but for numerous other health conditions. Effective strategies for quitting include setting a quit date, seeking support from friends, family, or a healthcare provider, and utilizing evidence-based resources such as nicotine replacement therapies or prescription medications. Behavioral counseling and support groups, both in-person and online, can greatly increase your chances of success. The Smokefree.gov website offers free tools, expert advice, and a supportive community for individuals looking to quit tobacco. Remember, it’s never too late to benefit from quitting—your body begins to heal almost immediately, and your risk of colorectal cancer decreases with every smoke-free year.
8. Limit Alcohol Consumption

Alcohol consumption is a recognized risk factor for colorectal cancer. When alcohol is metabolized in the body, it breaks down into acetaldehyde, a toxic compound that can damage the lining of the colon and rectum and interfere with DNA repair processes. According to the National Cancer Institute, the risk of colorectal cancer rises with the amount of alcohol consumed, and even moderate drinking can elevate risk compared to abstaining.
Moderate drinking is typically defined as up to one drink per day for women and two for men, while heavy drinking exceeds these limits. Studies show that heavy drinkers face a significantly higher risk of colorectal cancer than moderate or non-drinkers. To reduce your risk, consider setting weekly limits, choosing alcohol-free days, and substituting alcoholic beverages with water, herbal teas, or sparkling water. Social support and mindful drinking techniques, such as savoring your drink slowly and not using alcohol to manage stress, can help you cut back. For more practical tips and guidance on reducing alcohol intake, visit the NHS alcohol advice page.
9. Manage Type 2 Diabetes
Type 2 diabetes is associated with a higher risk of developing colorectal cancer. High blood sugar levels and insulin resistance can create an environment that promotes cancer cell growth in the colon and rectum. According to the American Cancer Society, individuals with type 2 diabetes are more likely to be diagnosed with colorectal cancer compared to those without diabetes, even after accounting for other risk factors such as obesity and inactivity.
Effectively managing diabetes can help reduce this risk. Key strategies for blood sugar control include monitoring blood glucose levels, following a balanced diet rich in whole grains, vegetables, and lean proteins, and engaging in regular physical activity. Taking prescribed medications as directed and keeping up with medical appointments are also essential. Weight management and reducing processed foods and sugary beverages further support healthy blood sugar levels. Collaborating with your healthcare team, including a primary care doctor and a registered dietitian, can provide personalized guidance. For more information and resources on managing diabetes, visit the American Diabetes Association Healthy Living page.
10. Pay Attention to Symptoms

Recognizing the early warning signs of colorectal cancer can greatly improve your chances of early detection and effective treatment. Common symptoms include blood in the stool, persistent changes in bowel habits (such as diarrhea, constipation, or narrowing of the stool), unexplained weight loss, abdominal pain or cramping, and fatigue. According to the American Cancer Society, being alert to these symptoms and seeking prompt evaluation can lead to earlier diagnosis, which is closely linked to higher survival rates.
Many people may dismiss mild or occasional symptoms, but awareness and timely action are crucial. Studies have shown that individuals who recognize and act upon warning signs are diagnosed at earlier stages, when colorectal cancer is more treatable. If you notice blood in your stool, ongoing changes in bowel habits, or any unexplained symptoms lasting more than a few weeks, it is important to consult your healthcare provider without delay. Do not self-diagnose or wait for symptoms to worsen. For more information on symptoms and when to seek medical help, visit the NHS bowel cancer symptoms page.
11. Increase Calcium Intake

Calcium plays a crucial role in maintaining colon health and may help protect against colorectal cancer. Research cited by the National Cancer Institute suggests that adequate calcium intake can reduce the growth of abnormal cells in the colon and bind to potentially harmful substances in the digestive tract, thus lowering cancer risk. Studies indicate that people who consume recommended levels of calcium have a lower risk of developing colorectal cancer compared to those with insufficient intake.
While dairy products such as milk, yogurt, and cheese are traditional sources of calcium, many non-dairy options are also available. Leafy green vegetables (like kale and bok choy), fortified plant-based milks, almonds, tofu, and canned salmon with bones all provide significant amounts of calcium. For those unable to meet their needs through diet alone, supplementation may be considered. However, excessive calcium intake can pose health risks, so it’s important to follow recommended guidelines—generally 1,000-1,200 mg per day for most adults. Consult your healthcare provider before starting supplements to ensure they are appropriate for your individual needs. For more information on calcium sources and safe supplementation, see the NIH Calcium Fact Sheet.
12. Add More Vitamin D

Vitamin D is vital for maintaining colon health and may play a protective role against colorectal cancer. Research highlighted by the American Cancer Society suggests that adequate vitamin D levels help regulate cell growth and reduce inflammation in the colon, potentially lowering cancer risk. People with lower vitamin D levels have been shown to be at higher risk for developing colorectal cancer in comparison to those with sufficient levels.
The primary natural source of vitamin D is sunlight exposure, as the skin synthesizes this vitamin when exposed to UV rays. However, factors such as location, season, skin tone, and sunscreen use can affect how much vitamin D your body produces. Dietary sources include fatty fish (like salmon and mackerel), fortified foods, and egg yolks. For those unable to get enough vitamin D through sunlight or diet, supplementation is an option, but it’s important to avoid excessive intake. To determine your vitamin D status, a simple blood test ordered by your healthcare provider can help. For more guidance on vitamin D sources, supplementation, and testing, visit the NHS vitamin D page.
13. Eat More Fruits and Vegetables

Fruits and vegetables are packed with antioxidants and phytochemicals—natural compounds that help protect cells from damage and may reduce the risk of colorectal cancer. According to the World Cancer Research Fund, diets high in plant-based foods are associated with lower rates of colorectal cancer compared to diets that are low in produce and high in processed foods. Antioxidants like vitamin C, vitamin E, and beta-carotene, as well as fiber and a variety of phytochemicals, work together to neutralize harmful free radicals and support healthy digestion.
To increase your intake, aim to fill at least half your plate with a colorful variety of fruits and vegetables at every meal. Snack on raw carrots, bell peppers, or fruit, add spinach or tomatoes to sandwiches, and include salads or vegetable soups with lunch and dinner. Frozen and canned options (without added sugars or salt) are convenient and nutritious alternatives to fresh produce. Gradually increasing your servings makes the transition easier and helps you discover new flavors and textures. For additional ideas and serving suggestions, visit the NHS 5 A Day guide.
14. Avoid Sedentary Behavior

Prolonged sitting and sedentary behavior are linked to an increased risk of colorectal cancer, independent of overall physical activity levels. Extended periods of inactivity slow down metabolism, reduce circulation, and may contribute to weight gain and inflammation—all factors that can elevate cancer risk. According to the National Cancer Institute, individuals with predominantly desk-based or sedentary jobs face higher rates of colorectal cancer compared to those who are regularly on their feet or engaged in active work.
To reduce these risks, it’s important to break up long periods of sitting throughout the day. Simple strategies include standing or walking during phone calls, setting reminders to get up every 30 to 60 minutes, and using a standing desk if available. Incorporating short walks, stretching sessions, or light exercises during breaks can also make a significant difference. At home, limit screen time by engaging in household chores, gardening, or recreational activities. Even small changes can help counteract the negative effects of sitting and promote better overall health. For more tips on reducing sedentary time, visit the NHS Sitting Less page.
15. Reduce Stress

Chronic stress can negatively impact immune function and overall health, potentially influencing the risk of colorectal cancer. Research, including studies from the National Cancer Institute, suggests that persistent high stress levels may weaken the immune system, promote inflammation, and contribute to unhealthy behaviors such as poor diet, physical inactivity, or increased smoking and alcohol use. People with high-stress lifestyles often experience more frequent illnesses and slower recovery compared to those who manage stress effectively.
Those with lower stress levels tend to maintain healthier routines and have stronger immune responses. To reduce stress, consider incorporating relaxation techniques such as deep breathing exercises, meditation, or progressive muscle relaxation into your daily routine. Physical activity, time in nature, social connections, and hobbies can also provide relief and boost mood. Establishing a consistent sleep schedule and seeking professional support from a counselor or therapist when needed are valuable strategies. Mindfulness apps and guided relaxation resources can further support stress management efforts. For evidence-based relaxation techniques and more information on coping with stress, visit the NHS Relaxation Tips for Stress page.
16. Get Enough Sleep
Emerging research links poor sleep quality and insufficient rest to an increased risk of various cancers, including colorectal cancer. Disrupted sleep patterns can impair immune function, heighten inflammation, and affect the body’s ability to regulate hormones and cellular repair. A study published by the National Institutes of Health (NIH) suggests that people who consistently get less than six hours of sleep per night may have a greater risk of developing colorectal polyps, a precursor to cancer, compared to those who regularly achieve seven to eight hours.
Good sleep habits, or sleep hygiene, can make a significant difference. Individuals with healthy routines—such as keeping regular bedtimes, limiting screen use before bed, and creating a comfortable, quiet sleep environment—tend to enjoy better quality rest and reduced cancer risk. To improve sleep hygiene, avoid caffeine late in the day, maintain a cool and dark bedroom, and establish a relaxing pre-sleep routine like reading or gentle stretching. If sleep problems persist, consult a healthcare professional for evaluation. For more science-backed tips and guidance on healthy sleep practices, visit the NHS Sleep Guide.
17. Know About Lynch Syndrome
Lynch syndrome is a hereditary condition that significantly increases the risk of developing colorectal cancer and several other cancers. Caused by inherited mutations in genes responsible for DNA repair, Lynch syndrome affects about 1 in 300 people, according to the National Cancer Institute. Individuals with Lynch syndrome have a lifetime risk of up to 80% for colorectal cancer, compared to a risk of about 4% in the general population. This syndrome can also lead to earlier onset of cancer, often before age 50.
Recognizing the signs and risk factors for Lynch syndrome is crucial, especially if you have a strong family history of colorectal, endometrial, or related cancers. Consider genetic counseling and testing if multiple family members have had these cancers, particularly at younger ages, or if you have a known Lynch syndrome-associated cancer yourself. Early identification can lead to personalized screening plans, preventive measures, and risk-reducing strategies for you and your relatives. For more detailed information on Lynch syndrome, who should consider genetic testing, and the benefits of early detection, visit the American Cancer Society Lynch Syndrome Guide.
18. Be Aware of Inflammatory Bowel Disease (IBD)
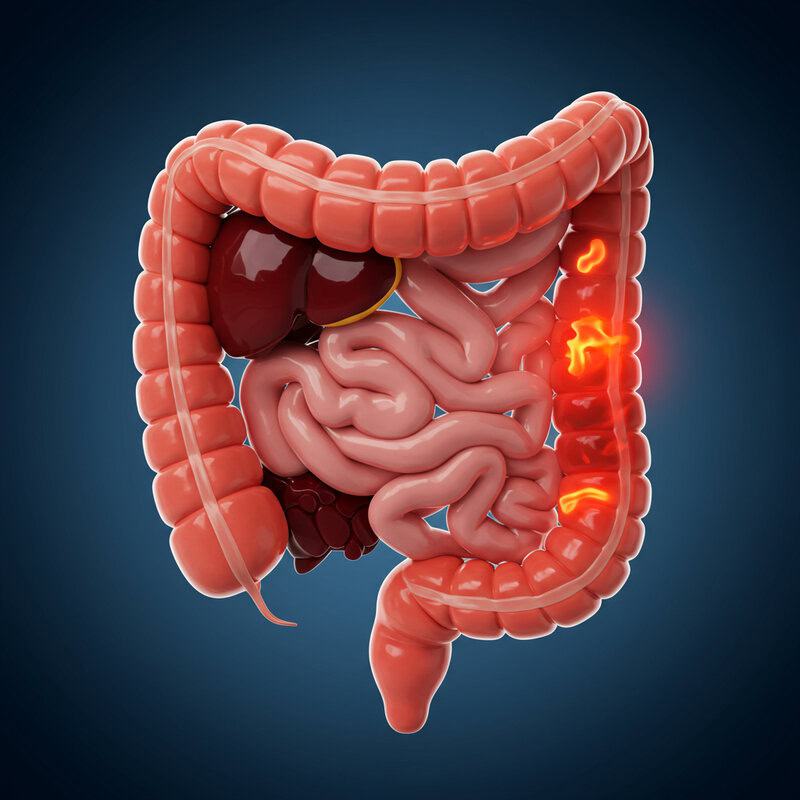
Inflammatory Bowel Disease (IBD), which includes ulcerative colitis and Crohn’s disease, is a significant risk factor for colorectal cancer due to chronic inflammation of the colon lining. According to the Crohn’s & Colitis Foundation, people with IBD have a higher risk of developing colorectal cancer than the general population, especially after living with the disease for more than 8-10 years. The risk increases with the extent and duration of inflammation.
Ulcerative colitis typically involves continuous inflammation of the colon and rectum, while Crohn’s disease can affect any part of the gastrointestinal tract and often presents with patchy inflammation. Both conditions require vigilant monitoring because persistent inflammation can trigger cellular changes that may lead to cancer. Regular colonoscopic surveillance with biopsies is strongly recommended for individuals with IBD. Early and effective management of inflammation through medication, lifestyle changes, and routine checkups can reduce cancer risk. If you have IBD, work closely with your gastroenterologist to develop a personalized monitoring plan. For more information on IBD and cancer prevention strategies, visit the American Cancer Society’s risk factors page.
19. Limit Sugary Beverages

High consumption of sugary beverages—such as sodas, energy drinks, and sweetened teas—has been linked to increased obesity, a well-known risk factor for colorectal cancer. Excessive sugar intake contributes to weight gain, insulin resistance, and systemic inflammation, all of which may promote cancer development. According to the National Cancer Institute, studies suggest that individuals who consume large amounts of sugary drinks have a higher risk of colorectal cancer, particularly among younger adults.
Water-based drinks, such as plain water, herbal teas, and unsweetened infused waters, are healthier alternatives that support hydration without the added calories and risks associated with sugar-laden beverages. Replacing just one sugary drink per day with water can significantly reduce overall sugar intake and help manage weight. For added flavor, try adding slices of lemon, cucumber, or berries to your water. Gradually decreasing the frequency of sugary drink consumption can make the transition easier and more sustainable. For more information on the impact of sugary beverages and practical tips for healthier hydration, visit the NHS guide to sugar in diet.
20. Avoid Charred or Burnt Foods

Cooking foods at high temperatures—such as grilling, barbecuing, or frying—can produce carcinogenic compounds like heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs). These substances form when meat is cooked over an open flame or to the point of charring, and have been shown to damage DNA, potentially increasing colorectal cancer risk. According to the National Cancer Institute, people who frequently consume charred or burnt meats may face a higher cancer risk compared to those who use gentler cooking methods.
Steaming, poaching, or baking foods at lower temperatures minimizes the formation of these harmful compounds. In contrast, grilling, broiling, and pan-frying—especially when foods become blackened—create more carcinogens. To cook safely, avoid direct exposure of meat to an open flame, trim visible fat to reduce flare-ups, and marinate meats to lower HCA formation. Flip meat frequently and remove charred portions before eating. Incorporating more plant-based foods, which do not produce HCAs or PAHs, is another protective step. For further information and practical tips on safer cooking methods, see the American Cancer Society’s cooked meats guidance.
21. Practice Safe Food Handling

Proper food handling is essential for preventing foodborne illnesses, which can cause acute or chronic inflammation in the colon. Persistent or repeated gastrointestinal infections may contribute to colon damage, potentially increasing vulnerability to colorectal cancer over time. According to the Centers for Disease Control and Prevention (CDC), practicing safe food handling dramatically reduces the risk of harmful bacterial contamination and related colon inflammation.
Unsafe practices—such as consuming undercooked meats, cross-contaminating raw and cooked foods, or neglecting handwashing—heighten the risk of infections like Salmonella, E. coli, and Campylobacter. In contrast, safe practices include thorough handwashing with soap and water before and after food preparation, using separate cutting boards for raw meats and vegetables, cooking foods to recommended internal temperatures, and refrigerating leftovers promptly. Regularly cleaning kitchen surfaces and utensils also helps prevent the spread of bacteria. By consistently following these steps, you can protect your digestive health and reduce the risk of inflammation-related complications. For comprehensive food safety guidelines and additional tips, visit the NHS Food Safety and Hygiene page.
22. Monitor Your Bowel Habits
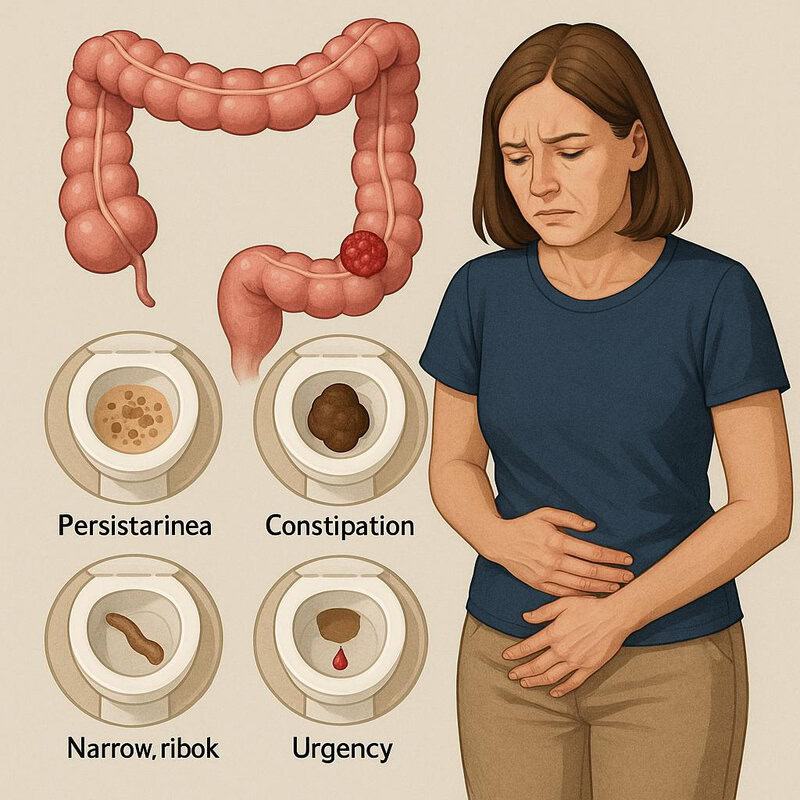
Tracking changes in your bowel habits can provide important early clues about your colon health. While everyone’s digestive system varies, significant or persistent changes may signal underlying problems, including colorectal cancer. According to the American Cancer Society, symptoms such as persistent diarrhea, constipation, narrow or ribbon-like stools, or a sudden urge to have a bowel movement can be cause for concern if they last more than a few weeks.
Typical bowel patterns differ from person to person, but generally, regularity and consistency are signs of a healthy digestive tract. Occasional minor fluctuations—such as mild constipation after travel or dietary changes—are usually not worrisome. In contrast, concerning symptoms include sustained alterations in frequency or form, blood in the stool, unexplained weight loss, or abdominal pain. If you experience any of these symptoms, especially in combination or if they persist, consult your healthcare provider promptly. Early evaluation can help identify and address issues before they become serious. For more information on what to watch for and when to seek help, visit the NHS bowel cancer symptoms page.
23. Avoid Unnecessary Antibiotics
Antibiotics are invaluable for treating bacterial infections, but their overuse can disrupt the balance of beneficial bacteria in the gut, a factor increasingly linked to colorectal cancer risk. Research published by the National Cancer Institute suggests that frequent or unnecessary antibiotic use may reduce microbial diversity, alter immune responses, and increase inflammation in the colon.
While antibiotics are essential for treating specific, confirmed bacterial infections, overuse—such as for viral illnesses like the common cold—can be harmful. Preserving gut health involves only taking antibiotics when prescribed by a healthcare provider and completing the full course as directed. To support healthy gut bacteria, focus on a diet rich in fiber from fruits, vegetables, and whole grains, and consider incorporating fermented foods like yogurt, kefir, or sauerkraut. If you must take antibiotics, ask your doctor about ways to maintain digestive health during and after treatment. For more information on antibiotic stewardship and maintaining a healthy gut microbiome, refer to the NHS antibiotics advice page.
24. Get Vaccinated Against Hepatitis B

Hepatitis B virus (HBV) is primarily known for its impact on liver health, but emerging research indicates that chronic HBV infection may also increase the risk of colorectal cancer. Chronic hepatitis B can contribute to systemic inflammation and immune system changes, which may promote cancer development in other organs, including the colon. According to studies referenced by the National Institutes of Health (NIH), individuals with hepatitis B infection have a higher risk of developing colorectal cancer compared to those who are uninfected.
Vaccination against hepatitis B is a highly effective preventive measure. Those who are vaccinated have a much lower risk of infection and its long-term complications, while unvaccinated individuals are more vulnerable, especially if exposed to the virus through blood, bodily fluids, or unprotected sex. The CDC recommends universal vaccination for infants, unvaccinated children and adolescents, and adults at increased risk for HBV infection. If you are unsure of your vaccination status, consult your healthcare provider about getting tested and vaccinated if necessary. For more information on hepatitis B vaccination and its benefits, visit the NHS hepatitis B vaccination page.
25. Avoid Environmental Toxins

Exposure to environmental toxins, such as pesticides, industrial chemicals, and heavy metals, has been associated with an increased risk of various cancers, including colorectal cancer. These substances can enter the body through contaminated water, air, soil, or food, potentially leading to cellular damage and inflammation. According to the National Cancer Institute, both rural and urban populations face risks, though the nature and sources of exposure may differ. Rural communities may encounter higher pesticide exposure due to agricultural activities, while urban environments might have greater air pollution or industrial contaminants.
To reduce environmental toxin exposure, wash fruits and vegetables thoroughly, choose organic produce when possible, filter drinking water, and avoid using chemical-based pesticides and cleaners at home. Be mindful of local air quality advisories, and consider using air purifiers indoors. Limiting consumption of high-mercury fish and avoiding unnecessary contact with industrial chemicals also helps decrease risk. Staying informed about environmental hazards in your area and supporting policies that reduce pollution can protect both personal and community health. For more details on environmental cancer risks and protective tips, visit the Cancer Research UK pollution and cancer page.
26. Choose Whole Grains Over Refined Grains

Whole grains offer significant benefits for colon health and colorectal cancer prevention. Rich in fiber, vitamins, minerals, and phytochemicals, whole grains support regular bowel movements, feed beneficial gut bacteria, and may help reduce inflammation in the digestive tract. According to the World Cancer Research Fund, diets high in whole grains are associated with a lower risk of colorectal cancer, while refined grains—stripped of their bran and germ—lack these protective nutrients.
Refined products like white bread, white rice, and traditional pasta are digested quickly, causing rapid spikes in blood sugar and offering little fiber. In contrast, whole grain options such as brown rice, whole wheat bread, oats, barley, and quinoa provide sustained energy and contribute to a healthier gut. Practical swaps include choosing whole wheat over white bread, brown or wild rice instead of white rice, and whole grain pasta or cereals. Gradually increasing your intake of whole grains can help your digestive system adjust and make the transition easier. For more guidance on the health benefits of whole grains and how to incorporate them into your meals, visit the NHS Wholegrains Guide.
27. Stay Hydrated
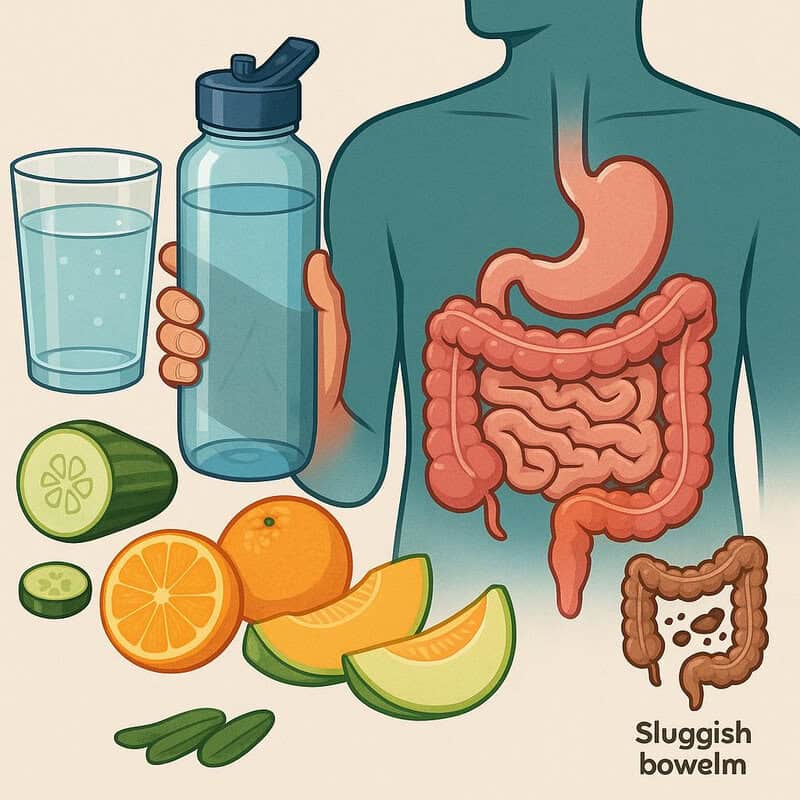
Staying well-hydrated is essential for optimal colon function and overall digestive health. Water helps soften stool, supports regular bowel movements, and dilutes waste products in the colon, which may reduce the risk of irritation and inflammation. According to the American Cancer Society, proper hydration helps the colon work efficiently and may lower the likelihood of constipation and related complications, which are important factors for colorectal health.
Dehydration, on the other hand, can lead to hard stools and sluggish bowel movements, increasing the risk of constipation and straining, which over time may contribute to colon issues. Chronic dehydration can also impair the removal of toxins from the digestive tract, potentially raising cancer risk. To maintain adequate hydration, aim to drink water regularly throughout the day—about 6-8 glasses for most adults, though individual needs vary based on activity, climate, and health status. Carry a reusable water bottle, set reminders to sip water, and include hydrating foods like cucumbers, oranges, and melons in your diet. For more tips and information on proper hydration, visit the NHS Water, Drinks and Your Health page.
28. Avoid Excessive Salt Intake

Excessive salt intake has been linked to gastrointestinal problems, including inflammation and damage to the lining of the digestive tract. While the association between salt and colorectal cancer is still being studied, evidence suggests that high-salt diets may contribute to an unhealthy gut environment and raise the risk of other digestive cancers. According to the World Cancer Research Fund, reducing salt consumption is an important step toward protecting digestive health.
Salty snacks like chips, processed meats, instant noodles, and canned soups often contain high levels of sodium, while fresh fruits, vegetables, whole grains, and unsalted nuts are naturally low in salt. Replacing processed, salty foods with fresh, home-cooked meals allows you to better control sodium intake. Aim for less than 2,300 mg of sodium per day, as recommended by the Centers for Disease Control and Prevention (CDC). Read nutrition labels, use herbs and spices instead of salt for flavoring, and rinse canned foods to reduce sodium content. For more guidance on lowering salt intake and making heart- and colon-healthy food choices, visit the NHS Salt Nutrition page.
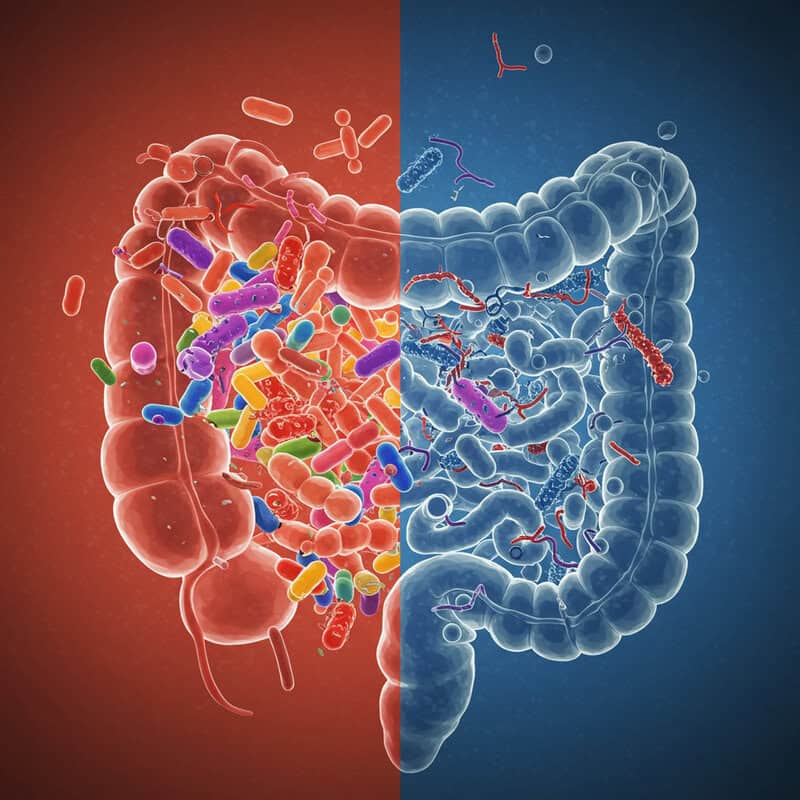
29. Mind Your Gut Microbiome
The gut microbiome—a complex community of trillions of bacteria and other microorganisms in your digestive tract—plays a crucial role in maintaining colon health and may influence colorectal cancer risk. A diverse and balanced microbiome supports digestion, regulates inflammation, and helps protect against harmful pathogens. According to the National Cancer Institute, research has found that certain gut bacteria can produce substances that either suppress or promote cancer development.
Individuals with a diverse microbiome, fostered by a varied diet rich in fiber and plant-based foods, tend to have a lower risk of colon inflammation and cancer. In contrast, an imbalanced microbiome—often resulting from poor diet, overuse of antibiotics, or chronic stress—can create an environment where harmful bacteria thrive, increasing cancer risk. To support your gut health, include probiotic-rich foods such as yogurt with live cultures, kefir, sauerkraut, kimchi, and miso in your diet. Also, consume prebiotic foods like onions, garlic, bananas, and whole grains to nourish beneficial bacteria. For more information on the link between gut health and colorectal cancer, visit the NHS Probiotics Guide.
30. Limit Artificial Additives

Artificial additives, including food dyes, preservatives, and flavor enhancers, are commonly found in processed foods and have raised concerns about their long-term effects on health. Some studies have suggested a possible link between certain additives and an increased risk of gastrointestinal issues, inflammation, and potentially colorectal cancer, although more research is needed. According to the American Cancer Society, minimizing processed foods and artificial additives may help reduce unnecessary exposure to substances that could pose health risks.
Processed foods—such as packaged snacks, ready meals, and sugary drinks—often contain a variety of artificial colors, flavors, and preservatives, while whole foods like fresh fruits, vegetables, and unprocessed grains do not. Choosing whole foods reduces your intake of additives and provides essential nutrients that support colon health. To limit artificial additives, read ingredient labels carefully and avoid products with long lists of unfamiliar or chemical-sounding names. Opt for foods labeled as “no artificial colors or preservatives” when possible. Preparing meals at home from fresh ingredients is another effective way to control what you eat. For more information on food additives and how to make informed choices, visit the NHS Food Additives Guide.
31. Get Regular Medical Checkups

Routine medical checkups are a cornerstone of preventive health and play a critical role in the early detection of colorectal cancer. Regular visits to your healthcare provider allow for ongoing risk assessment, timely screening recommendations, and the identification of subtle warning signs that may otherwise go unnoticed. According to the National Cancer Institute, individuals who receive periodic checkups and screenings are more likely to detect colorectal cancer at an earlier, more treatable stage compared to those who only seek medical attention when symptoms arise.
Outcomes are significantly better among people who adhere to regular care; early detection increases survival rates and often leads to less aggressive treatment options. Your provider can also monitor other health conditions that may increase your risk, such as type 2 diabetes or inflammatory bowel disease. Adults should generally aim for an annual checkup, although your provider may recommend more frequent visits based on age, personal and family history, and specific risk factors. Be proactive in discussing any new symptoms or concerns, and make sure to keep up with recommended cancer screenings. For more advice on the importance of checkups and screening schedules, visit the NHS GP services page.
32. Know Your Personal Risk Factors
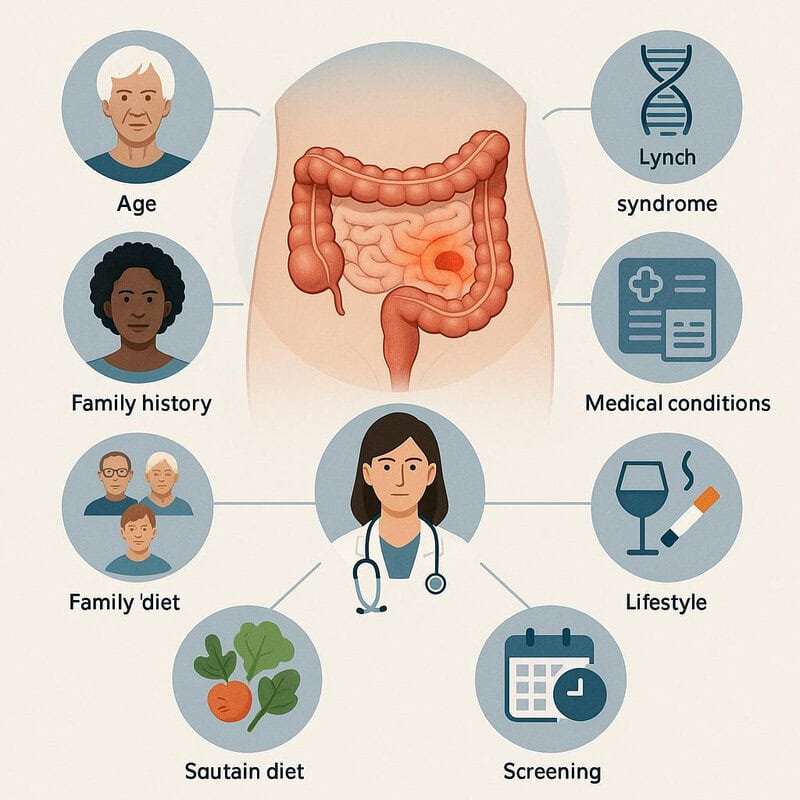
Understanding your personal risk factors for colorectal cancer is key to effective prevention and tailored health strategies. Risk assessment involves evaluating elements such as age, ethnicity, family history, genetic predispositions (like Lynch syndrome), lifestyle choices, and underlying medical conditions such as inflammatory bowel disease or type 2 diabetes. The American Cancer Society emphasizes that individuals with multiple or significant risk factors may need earlier or more frequent screenings compared to those at average risk.
High-risk individuals—such as those with a close relative who had colorectal cancer, or a history of certain genetic syndromes—should work closely with their healthcare provider to develop a personalized prevention plan. This may include earlier screening, genetic counseling, or more intensive lifestyle modifications. Low-risk individuals can often follow standard screening recommendations and focus on general preventive measures, such as maintaining a healthy diet and staying active. To assess your risk, gather detailed family health information, be aware of your medical history, and discuss these factors with your doctor. For additional guidance on risk assessment and personalized prevention, visit the NHS Bowel Cancer Causes page.
33. Use Aspirin Only as Directed

Recent studies have suggested that regular, low-dose aspirin use may help reduce the risk of colorectal cancer, particularly among individuals with higher risk profiles. Aspirin’s anti-inflammatory properties are believed to inhibit processes that promote cancer cell growth in the colon. According to the National Cancer Institute, long-term aspirin use has shown a modest protective effect, especially for those with a personal or family history of polyps or colorectal cancer.
However, aspirin is not without risks—it can increase the likelihood of gastrointestinal bleeding, ulcers, and other side effects, especially in older adults or those with certain medical conditions. The balance of benefits and risks varies from person to person. Experts, including the U.S. Preventive Services Task Force, recommend that aspirin for cancer prevention should only be considered under medical supervision. Never start, stop, or change your aspirin regimen without talking to your healthcare provider, who can assess your individual risk and advise on the safest course of action. For more detailed guidance, visit the NHS Aspirin Information page.
34. Consider Genetic Counseling

Genetic counseling is a valuable resource for individuals with a personal or family history suggestive of hereditary colorectal cancer syndromes, such as Lynch syndrome or familial adenomatous polyposis. According to the National Cancer Institute, those who have multiple relatives with colorectal or related cancers, early-onset diagnoses, or known genetic mutations should consider genetic counseling to assess their risk and guide prevention strategies.
People who undergo genetic counseling are more likely to receive timely genetic testing, personalized screening recommendations, and preventive interventions compared to those who do not seek this specialized guidance. This proactive approach can lead to earlier detection, improved outcomes, and tailored care for both the individual and their family. During a genetic counseling session, you can expect a thorough review of your family and medical history, discussion of potential genetic testing, and exploration of the implications for your health and your relatives. The counselor will provide information, answer questions, and support decision-making. For more information about genetic counseling, who should consider it, and what to expect, visit the NHS Genetic Counseling page.
35. Watch for Unexplained Weight Loss

Sudden, unexplained weight loss can be an important warning sign of underlying health issues, including colorectal cancer. While gradual weight loss due to intentional lifestyle changes, such as improved diet and increased physical activity, is generally considered healthy, losing a significant amount of weight without trying—typically more than 5% of your body weight over six to twelve months—may signal a medical problem. According to the American Cancer Society, unexplained weight loss is one of the symptoms often reported by individuals diagnosed with colorectal cancer.
Healthy weight changes usually occur in the context of dietary adjustments or exercise programs and are accompanied by other positive health markers. In contrast, concerning weight loss may be rapid, persistent, and accompanied by other symptoms such as fatigue, changes in bowel habits, or abdominal pain. If you experience unexplained weight loss, especially alongside additional gastrointestinal symptoms, consult your healthcare provider promptly for evaluation. Early assessment can help identify the cause and, if necessary, lead to timely intervention. For more guidance on when to seek medical attention for weight changes, visit the NHS Sudden Weight Loss page.
36. Know About Polyps
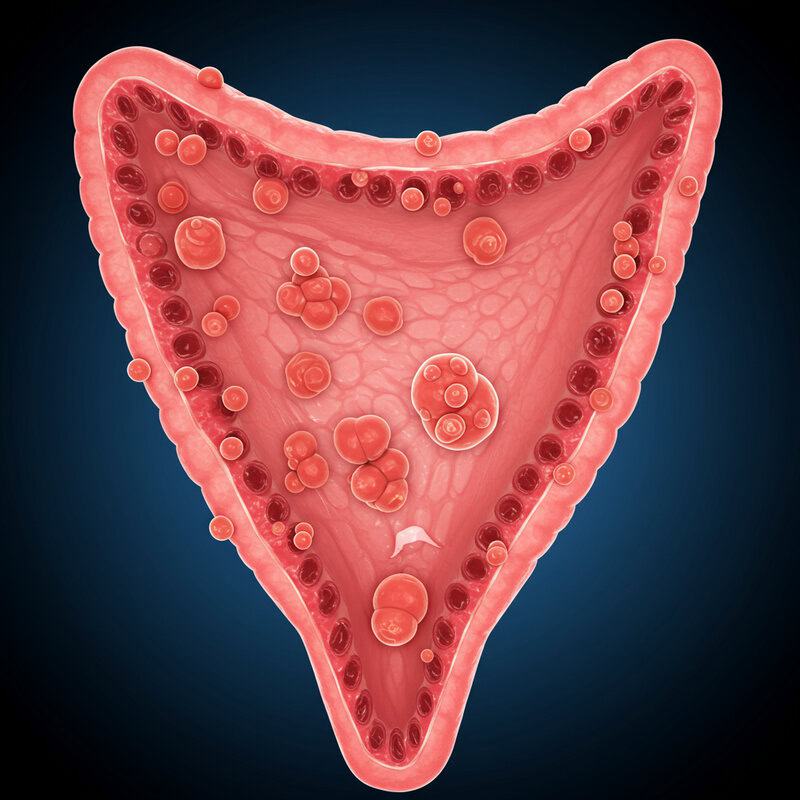
Colon polyps are growths that form on the inner lining of the colon or rectum. While most polyps are benign, some can develop into colorectal cancer over time. According to the American Cancer Society, the majority of colorectal cancers begin as adenomatous polyps, which have the potential to become malignant if not detected and removed early.
There are several types of polyps, with adenomatous (adenomas) and serrated polyps carrying the highest risk for cancer development. Hyperplastic polyps, on the other hand, are generally considered low risk. The likelihood of a polyp turning into cancer depends on its size, type, and number. Regular screening through colonoscopy is essential because it allows for the detection and removal of polyps before they become cancerous—a process known as polypectomy. Removing polyps during screening significantly reduces the risk of colorectal cancer. If you are at increased risk or have previously had polyps, your healthcare provider may recommend more frequent surveillance. For more information about colon polyps and their role in cancer prevention, visit the NHS Bowel Polyp page.
37. Eat Healthy Fats

The types of fats you consume can significantly affect inflammation and overall colon health, influencing your risk for colorectal cancer. Diets high in saturated fats—found in red meat, butter, and many processed foods—may promote inflammation and have been linked to increased cancer risk. In contrast, unsaturated fats, particularly omega-3 fatty acids, are associated with anti-inflammatory effects and may help protect against cancer development. According to the American Cancer Society, replacing saturated fats with healthier unsaturated fats can be a beneficial dietary strategy.
Unsaturated fats are found in foods such as olive oil, avocados, nuts, seeds, and fatty fish like salmon, mackerel, and sardines. These fats support cell health and may help regulate inflammation in the colon and throughout the body. Practical ways to incorporate healthy fats include using olive oil for cooking, adding sliced avocado to salads, and snacking on a handful of walnuts or almonds. Limit your intake of processed snacks, fried foods, and fatty cuts of red meat, which are high in less desirable fats. For more information on the impact of dietary fats and practical swaps, visit the NHS Different Fats Nutrition page.
38. Limit Fast Food

Diets high in fast food are associated with an increased risk of obesity, inflammation, and chronic diseases, including colorectal cancer. Fast foods typically contain high levels of unhealthy fats, salt, sugar, and artificial additives, while being low in fiber, vitamins, and minerals. The American Cancer Society notes that frequent consumption of fast food can promote weight gain and poor gut health, both of which are risk factors for colorectal cancer.
In contrast, home-cooked meals allow for greater control over ingredients, portion sizes, and cooking methods, making it easier to include fiber-rich vegetables, whole grains, and healthy fats. Preparing meals at home also helps reduce your intake of processed meats and artificial additives commonly found in fast food. To dine out more healthily, choose grilled or baked options instead of fried, ask for sauces and dressings on the side, and prioritize salads, whole grains, or vegetable-based dishes. Plan ahead by packing nutritious snacks or meals to avoid the temptation of fast food when you’re on the go. For more healthy eating tips and guidance, visit the NHS Healthy Eating Guide.
39. Engage Your Healthcare Team

Taking a team-based approach to your health significantly enhances prevention and early detection of colorectal cancer. Collaborating with your healthcare providers—including your primary care physician, gastroenterologist, dietitian, and other specialists—ensures that you receive comprehensive, personalized guidance tailored to your unique risk factors and needs. According to the National Cancer Institute, individuals who actively engage their healthcare team are more likely to adhere to screening recommendations, receive timely interventions, and achieve better outcomes compared to those navigating their health alone.
A solo approach may lead to missed opportunities for education, prevention, or early diagnosis. In contrast, a team approach provides multiple perspectives, expertise, and ongoing support. To get the most from your healthcare visits, come prepared with questions such as: Am I due for colorectal cancer screening? What risk factors should I be aware of? How can I improve my diet and lifestyle for colon health? Are there any symptoms I should monitor? Open communication and regular check-ins with your healthcare team empower you to make informed decisions and take proactive steps. For more advice on working with your providers, visit the NHS Working with Your Healthcare Team page.
40. Be Mindful of Hormone Use
Hormone therapy, including treatments such as hormone replacement therapy (HRT) for menopausal symptoms and certain contraceptives, can influence colorectal cancer risk. According to the American Cancer Society, some studies have shown that postmenopausal women who use combined estrogen-progestin HRT may have a slightly lower risk of developing colorectal cancer compared to non-users. However, hormone therapy can also increase the risk of other health issues, such as breast cancer, blood clots, and stroke, making the decision to use hormones complex and highly individual.
Individuals not using hormone therapy avoid these potential risks and benefits, but may experience more severe menopausal symptoms or require alternative treatments for other hormonal conditions. Before starting, stopping, or changing any hormone treatment, it is important to discuss your personal and family history, risk factors, and preferences with your healthcare provider. Regular checkups and open communication can help ensure that hormone use is safe and appropriate for your situation. For more insights on hormone therapy and its impact on cancer risk, visit the NHS Hormone Replacement Therapy Risks page.
41. Avoid Chronic Constipation
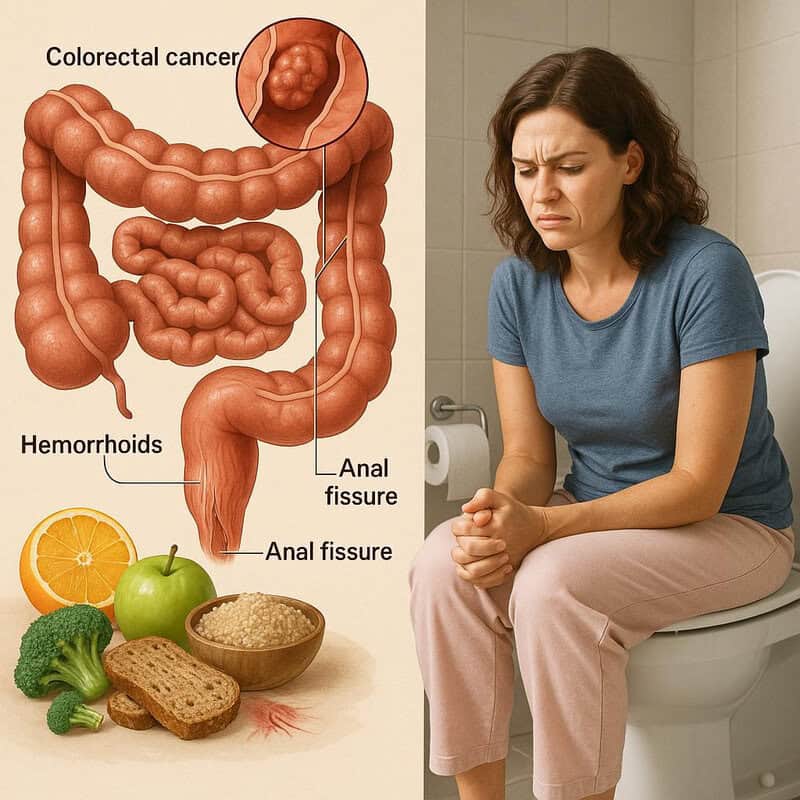
Maintaining regular, healthy bowel movements is important for colon health and may help lower the risk of colorectal cancer. Chronic constipation causes stool to remain in the colon for extended periods, which can lead to irritation, increased contact with potential carcinogens, and discomfort. According to the American Cancer Society, regularity is a sign that your digestive system is functioning well, while persistent constipation may indicate underlying issues that require attention.
Individuals with regular bowel habits are less likely to experience complications such as hemorrhoids, anal fissures, or chronic inflammation. In contrast, ongoing constipation—defined as fewer than three bowel movements per week or difficulty passing stool—should not be ignored. Remedies for chronic constipation include increasing dietary fiber through fruits, vegetables, and whole grains, staying well-hydrated, and engaging in regular physical activity. Establishing a consistent bathroom routine and responding promptly to the urge to have a bowel movement can also help. If constipation persists despite lifestyle changes, consult your healthcare provider, as it could signal a more serious condition. For more advice on managing and preventing constipation, visit the NHS Constipation page.
42. Know the Signs of Iron Deficiency Anemia
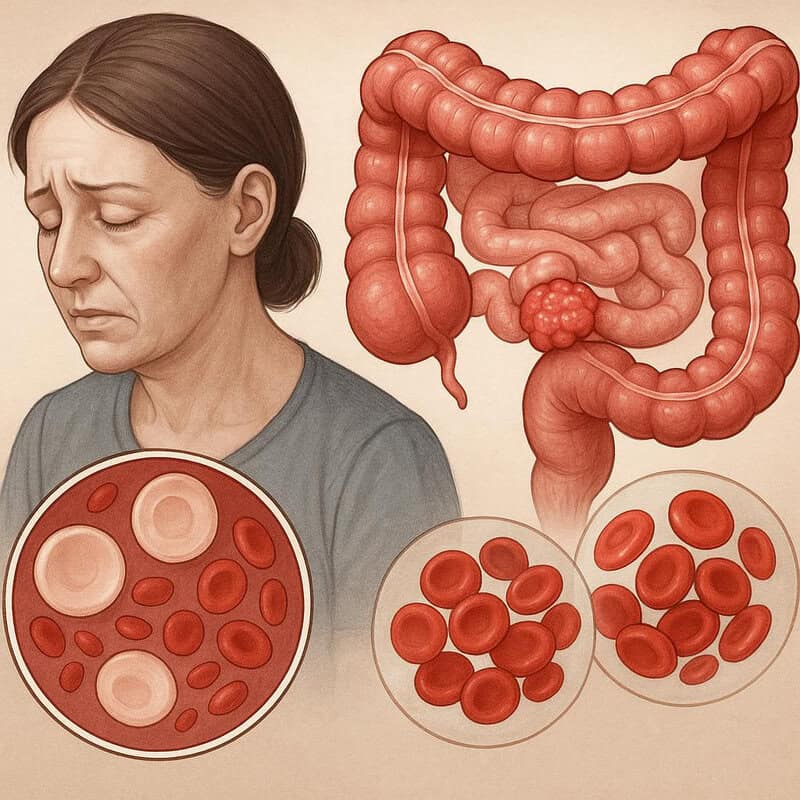
Iron deficiency anemia can be an early warning sign of colorectal cancer, particularly when it develops suddenly or without an obvious cause. This form of anemia occurs when the body lacks enough iron to produce healthy red blood cells, leading to symptoms such as fatigue, weakness, pale skin, shortness of breath, and dizziness. According to the American Cancer Society, unexplained iron deficiency anemia in adults—especially older adults—can be the result of slow, chronic blood loss from the digestive tract due to colon polyps or cancer.
While iron deficiency anemia is often caused by dietary insufficiency, heavy menstrual periods, or other non-cancerous conditions, the sudden onset or persistence of anemia without a clear reason warrants further investigation. Be vigilant for symptoms such as ongoing tiredness, chest pain, rapid heartbeat, or noticeable changes in stamina. If you experience these symptoms or your blood tests reveal low iron levels, consult your healthcare provider for further evaluation. Early testing may include stool tests, colonoscopy, or additional blood work. For more information on the warning signs and causes of anemia, visit the NHS Iron Deficiency Anaemia page.
43. Choose Organic When Possible

Choosing organic foods may offer benefits for colorectal cancer prevention by reducing exposure to certain pesticides and synthetic chemicals. Organic farming practices limit the use of synthetic pesticides and fertilizers, which may help lower the intake of residues that have been linked to cancer risk in some studies. According to National Cancer Institute guidance, while the evidence is not conclusive, opting for organic produce can be part of a precautionary approach to lowering environmental toxin exposure.
Comparatively, conventionally grown foods are more likely to contain traces of pesticides, though regulatory agencies monitor these levels for safety. Some fruits and vegetables—such as strawberries, spinach, and apples—tend to have higher pesticide residues, making them good candidates for organic purchasing. When shopping on a budget, prioritize buying organic versions of foods you eat raw or most often, and wash all produce thoroughly. Incorporating a variety of fruits, vegetables, and whole grains—whether organic or conventional—remains the foundation of a healthy, cancer-preventive diet. For more information on organic foods, potential benefits, and safe produce handling, visit the NHS Organic Foods page.
44. Stay Up to Date with Research

Keeping informed about the latest research on colorectal cancer prevention is vital for making educated decisions about your health. New findings can influence screening recommendations, reveal emerging risk factors, and introduce more effective prevention strategies. Individuals who stay engaged with reputable health news are better equipped to adapt their habits and discuss up-to-date options with their healthcare providers. In contrast, those who do not follow current research may miss important advancements that could impact their risk or care.
Reliable sources for colorectal cancer research updates include the National Cancer Institute News, American Cancer Society News, and Cancer Research UK Latest News. Subscribing to newsletters, setting up alerts for trusted organizations, or regularly checking these websites can help you stay informed. Always consult your healthcare team before making changes based on new studies, as they can help interpret findings in the context of your personal risk factors. Staying engaged with research empowers you to make proactive, evidence-based choices for colorectal cancer prevention and overall health.
45. Advocate for Workplace Wellness

The work environment can significantly influence your risk of colorectal cancer by shaping daily habits around physical activity, diet, and stress management. Supportive workplaces that offer healthy meal options, encourage movement, and foster work-life balance contribute to lower cancer risk and better overall health. In contrast, unsupportive workplaces—characterized by prolonged sitting, limited access to healthy foods, and high stress—can increase risk factors such as obesity, inactivity, and poor dietary choices. According to the Centers for Disease Control and Prevention (CDC) Workplace Health Promotion program, effective wellness initiatives can help employees adopt and maintain cancer-preventive behaviors.
To promote wellness at work, consider advocating for standing desks, regular movement breaks, nutritious cafeteria options, and access to mental health resources. Organize walking meetings, encourage participation in wellness challenges, or request educational workshops on nutrition and cancer prevention. Open communication with management about the importance of a healthy work environment can lead to policy changes that benefit everyone. Even small changes—like keeping fruit in the break room or starting a lunchtime walking group—can make a meaningful difference. For more ideas and resources on workplace wellness, visit the NHS Workplace Health page.
46. Encourage Family Screening

Family-wide prevention is a powerful tool in reducing colorectal cancer risk, especially among those with a history of the disease. Encouraging all eligible family members to undergo regular screening can lead to earlier detection and, ultimately, save lives. Families that prioritize and participate in screening are more likely to catch polyps or early-stage cancers before symptoms arise, resulting in better outcomes and less invasive treatments. In contrast, families that avoid or delay screening miss critical opportunities for early intervention and may face higher rates of advanced cancer diagnoses. The National Cancer Institute strongly recommends discussing screening with relatives, especially if there is a known genetic risk or family history of colorectal cancer.
Starting the conversation can be as simple as sharing your own screening experience or expressing concern for your loved ones’ health. Try statements like, “I recently had my colonoscopy and it was a relief to know everything was okay,” or “Since colorectal cancer runs in our family, it’s important for all of us to get checked regularly.” Share reputable resources, such as the NHS Bowel Cancer Screening page, to help answer questions and address concerns. Open dialogue can empower your family to take proactive steps toward long-term health.
47. Know the Role of Aspirin and NSAIDs

Anti-inflammatory drugs such as aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) have been studied for their potential to reduce colorectal cancer risk. Research, including findings from the National Cancer Institute, shows that regular, long-term use of low-dose aspirin can lower the incidence of colorectal polyps and cancer, particularly in individuals at higher risk. NSAIDs like ibuprofen may also offer protective effects by reducing inflammation that can promote cancerous changes in the colon.
However, the use of these medications is not without risk. Aspirin and NSAIDs can cause gastrointestinal bleeding, ulcers, kidney problems, and other side effects, especially with prolonged or high-dose use. The balance of benefits and risks depends on personal health factors, age, and family history. Current guidelines recommend that anyone considering aspirin or NSAIDs for cancer prevention should first consult their healthcare provider. Your doctor can help assess your individual risk profile and determine whether the potential benefits outweigh the risks in your case. For more information on anti-inflammatory drugs and their role in cancer prevention, visit the NHS Anti-inflammatories Guide.
48. Support Public Health Initiatives

Public health initiatives play a vital role in colorectal cancer prevention by increasing awareness, improving access to screening, and promoting healthy lifestyle choices across communities. Areas with strong public health programs typically see higher rates of early detection, lower incidence of advanced cancer, and better patient outcomes. Programs may include free or subsidized screening events, educational campaigns, and outreach to underserved populations. According to the Centers for Disease Control and Prevention Colorectal Cancer Control Program, community-based interventions have been effective in reducing disparities and ensuring more people benefit from preventive measures.
Getting involved can amplify the impact of these initiatives. You can volunteer with local cancer organizations, participate in awareness campaigns, or advocate for public policies that support cancer screening and healthy environments. Sharing educational materials, encouraging friends and neighbors to get screened, and joining community walks or fundraisers are other ways to contribute. Supporting these efforts helps create a culture of prevention and can lead to lasting improvements in community health. For more information on public health programs and how you can participate, visit the Cancer Research UK Get Involved page.
49. Share Information with Others

Sharing accurate information about colorectal cancer prevention can create a powerful ripple effect, helping to protect not just individuals but entire communities. Informed communities are more likely to engage in preventive behaviors, participate in screenings, and support one another in making healthy choices. In contrast, uninformed communities may experience higher rates of late-stage cancer diagnoses, lower screening uptake, and persistent myths about cancer risk and prevention. According to the National Cancer Institute, effective communication and outreach are essential tools for improving public health outcomes.
To maximize your impact, tailor your message to your audience—use clear language, share personal stories or testimonials, and provide links to reputable resources like the American Cancer Society Colorectal Cancer Screening Guidelines. Host informational sessions at community centers, workplaces, or online, and encourage open discussion to dispel fears or misconceptions. Social media is another powerful tool for spreading awareness quickly and widely. By actively sharing knowledge, you can empower others to take charge of their health and help reduce the burden of colorectal cancer for future generations.
50. Take Action—Don’t Delay

Prompt action is crucial when it comes to preventing colorectal cancer. Individuals who proactively adopt healthy habits, schedule regular screenings, and address symptoms early significantly improve their chances of avoiding serious disease and achieving better health outcomes. In contrast, delaying prevention efforts—such as postponing screenings or ignoring warning signs—can result in late-stage diagnoses, more invasive treatments, and lower survival rates. According to the American Cancer Society, early detection and intervention are key determinants of long-term survival and quality of life.
To get started, assess your personal risk factors, discuss screening options with your healthcare provider, and begin incorporating prevention tips—such as improving your diet, staying active, and limiting alcohol and tobacco use—into your daily routine. Share these steps with family and friends to encourage a collective focus on prevention. Remember, taking small actions now can lead to big health benefits in the future. For more guidance, access resources provided by the NHS Bowel Cancer Prevention page. Don’t wait—taking action today could save your life or the life of someone you love.
Conclusion

Colorectal cancer prevention is urgent and achievable through informed, proactive steps. By adopting a balanced diet, staying physically active, maintaining a healthy weight, limiting alcohol and tobacco, and staying vigilant for symptoms, you can significantly lower your risk. Early and regular screening remains one of the most effective measures, especially for those with additional risk factors. Consulting your healthcare provider for personalized advice and acting on recommended screenings can save lives. Don’t wait for symptoms—prevention and early detection are key. For more information and to take the next step, visit the National Cancer Institute Colorectal Prevention page.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





