What Drinking Electrolytes Really Does to Your Heart
Cardiovascular disease remains the leading cause of death globally, accounting for nearly 18 million fatalities each year according to the World Health Organization. The heart, central to the body’s circulatory system, relies on a delicate balance of nutrients and minerals to function optimally. However, early symptoms of heart problems are often subtle and easily missed, complicating timely diagnosis and intervention. Understanding how dietary components like electrolytes influence heart health is critical as we seek to improve prevention and overall well-being.
1. Electrolytes: What Are They?
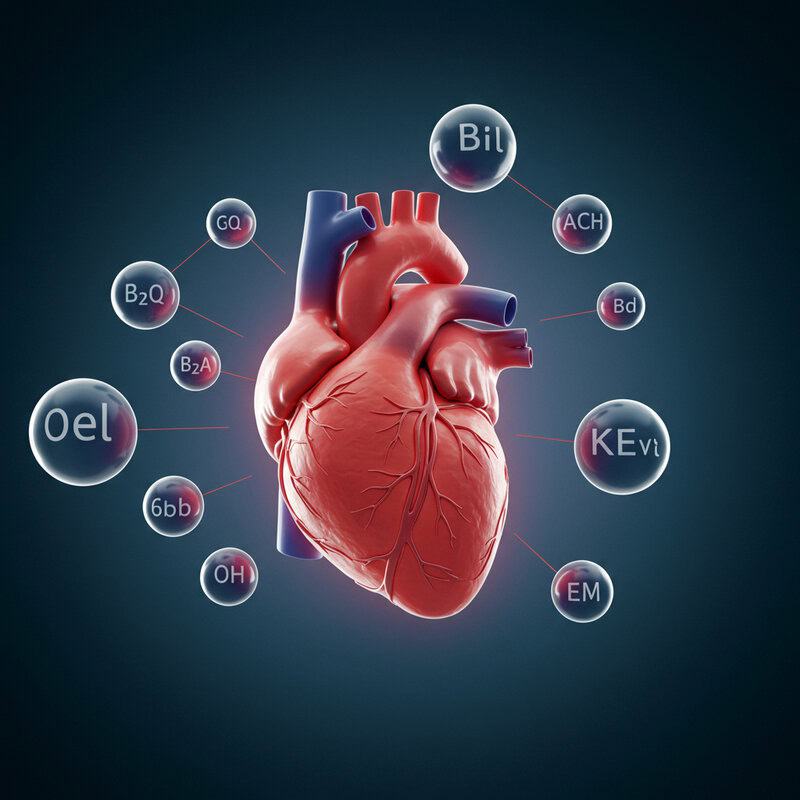
Electrolytes are minerals found in your blood and bodily fluids that carry an electric charge. The most common electrolytes include sodium, potassium, calcium, magnesium, chloride, bicarbonate, and phosphate. These minerals are essential because they help regulate a wide array of bodily functions—most notably, fluid balance, nerve signaling, and muscle contraction. Without the correct balance of electrolytes, cells cannot function properly, and crucial physiological processes can be disrupted.
Electrolytes are especially important for the heart because the cardiac muscle relies on electrical impulses to maintain a stable rhythm and contract effectively. For instance, potassium and sodium play a critical role in generating and transmitting the electrical signals that prompt heartbeats. Imbalances in these minerals can lead to arrhythmias—abnormal heart rhythms—which may be life-threatening in severe cases. Calcium and magnesium are also involved in the contraction and relaxation of the heart muscle, further linking electrolyte levels to cardiovascular health. To learn more about how electrolytes function in the body, visit the Centers for Disease Control and Prevention and the National Center for Biotechnology Information.
2. The Heart’s Electrical System

The heart depends on a precise electrical system to regulate each beat and maintain a steady rhythm. Specialized cells in the heart, known as pacemaker cells, generate electrical impulses that cause the heart muscles to contract and pump blood. This process, called the cardiac conduction system, is carefully orchestrated by the movement of electrolytes—primarily sodium, potassium, and calcium—across the membranes of heart cells.
During each heartbeat, sodium ions rush into the cardiac cells, triggering an electrical impulse. Potassium ions then flow out, helping the cells reset and prepare for the next beat. Calcium ions enter the cells as well, enabling the muscle fibers to contract with each signal. The delicate balance and movement of these electrolytes ensure the heart beats in a synchronized, efficient manner. Even minor disturbances can result in arrhythmias, such as atrial fibrillation or ventricular tachycardia, potentially leading to serious complications (American Heart Association).
Because electrolytes are so crucial to the heart’s electrical activity, maintaining their proper levels is vital to heart health and rhythm stability. This relationship underpins the importance of understanding how what you drink influences your cardiovascular system.
3. Sodium’s Role in Blood Pressure

Sodium is a vital electrolyte that helps regulate fluid balance in the body, but it also plays a significant role in controlling blood pressure. When you consume sodium, typically in the form of salt, it causes the body to retain water. This extra fluid increases the volume of blood circulating through your blood vessels, which can raise blood pressure. Over time, consistently high sodium intake puts extra strain on the heart and arteries, increasing the risk of hypertension, heart disease, and stroke.
According to the Centers for Disease Control and Prevention, most Americans consume far more sodium than the recommended daily limit of 2,300 mg, often unknowingly through processed and restaurant foods. Elevated blood pressure, or hypertension, is a well-established risk factor for heart attacks and heart failure, as it forces the heart to work harder to circulate blood. Reducing sodium intake can help lower blood pressure and protect heart health, especially in those who are salt-sensitive or have existing cardiovascular concerns. Understanding sodium’s impact is crucial for making informed dietary choices that support long-term heart wellness (American Heart Association).
4. Potassium: The Heart Protector

Potassium is a crucial electrolyte that plays a significant role in maintaining normal heart function and protecting against dangerous arrhythmias. It works in tandem with sodium to help regulate the heart’s electrical activity, ensuring that each heartbeat occurs in a controlled and rhythmic manner. Potassium achieves this by helping to reset the electrical charge in heart muscle cells after each contraction, preventing abnormal rhythms that can lead to complications like atrial fibrillation or even sudden cardiac arrest.
Adequate dietary potassium intake has been linked to a lower risk of high blood pressure and stroke. Foods rich in potassium, such as bananas, oranges, spinach, and sweet potatoes, not only support heart rhythm but also help counteract some of sodium’s negative effects on blood pressure. According to the National Institutes of Health, most people do not consume enough potassium in their daily diet, which can leave them vulnerable to heart issues, especially if sodium intake is high.
Ensuring an appropriate balance of potassium through dietary choices or supplements, as recommended by a healthcare provider, is essential for maintaining optimal heart health and reducing the risk of arrhythmias (American Heart Association).
5. Calcium’s Cardiac Influence
Calcium is widely recognized for its role in building strong bones, but it is equally critical for heart health. In the heart, calcium ions are essential for initiating and coordinating each muscle contraction, enabling the heart to pump blood efficiently throughout the body. When an electrical impulse travels along the heart muscle, calcium rushes into the cells, triggering the contractile machinery that produces a heartbeat. This process, known as excitation-contraction coupling, is fundamental to the heart’s ability to function as an effective pump.
An imbalance in calcium levels can have serious consequences. Hypocalcemia (low calcium) can impair heart muscle contraction, potentially leading to irregular heartbeats or decreased cardiac output. Hypercalcemia (high calcium), on the other hand, can cause the heart to beat abnormally fast or even stop altogether in severe cases. Maintaining a balanced calcium level is thus vital for the heart’s electrical and muscular activities. The National Center for Biotechnology Information highlights that proper calcium intake through diet—such as dairy products, leafy greens, and fortified foods—supports cardiac health, especially when paired with other electrolytes like magnesium for optimal function.
For more information, visit the American Heart Association.
6. Magnesium and Heart Rhythm

Magnesium is a vital electrolyte that plays a key role in maintaining a stable heart rhythm. It facilitates the movement of calcium and potassium into and out of cells, which is necessary for generating and propagating the electrical signals that control the heartbeat. Magnesium acts as a natural calcium channel blocker, helping to relax the heart muscle after each contraction and prevent abnormal electrical activity that could lead to arrhythmias.
A deficiency in magnesium can disrupt the balance of other electrolytes, increasing the risk of irregular heartbeats, palpitations, and more severe arrhythmias. Low magnesium levels are also associated with higher risk of hypertension, cardiovascular disease, and even sudden cardiac death (National Institutes of Health). Symptoms of magnesium deficiency may include muscle cramps, fatigue, and, in severe cases, dangerous changes in heart rhythm.
Most people can maintain adequate magnesium levels through a balanced diet that includes nuts, seeds, whole grains, leafy greens, and legumes. However, certain conditions—such as gastrointestinal disorders, diabetes, or excessive alcohol use—can increase the risk of deficiency and warrant extra attention to magnesium intake (NIH Office of Dietary Supplements).
7. Dehydration: The Hidden Trigger

Dehydration occurs when the body loses more fluids than it takes in, leading to an imbalance of essential electrolytes such as sodium, potassium, and magnesium. This disruption can have significant consequences for heart health. When dehydrated, the blood volume decreases, causing the heart to work harder to pump oxygen and nutrients throughout the body. This extra strain can result in increased heart rate, lower blood pressure, and, in severe cases, even shock (American Heart Association).
Moreover, dehydration can alter the concentration of electrolytes in the bloodstream. Fluctuations in sodium, potassium, or magnesium levels can disrupt the heart’s electrical activity and rhythm, increasing the risk of arrhythmias and other cardiac complications. Athletes, older adults, and individuals with certain medical conditions are especially susceptible to the dangers of dehydration (Centers for Disease Control and Prevention). Ensuring adequate fluid intake and electrolyte replenishment is therefore essential for maintaining a healthy, steady heartbeat and preventing undue cardiovascular stress—especially during periods of intense physical activity, hot weather, or illness.
8. Overhydration and Heart Stress
While staying hydrated is critical for health, excessive fluid intake—especially when paired with high electrolyte consumption—can be harmful to the heart. Overhydration, also known as water intoxication, occurs when the body’s fluid balance is overwhelmed and sodium levels in the blood become dangerously diluted. This condition, called hyponatremia, can cause cells to swell and places significant strain on the heart and other organs.
When sodium concentration drops, the heart may struggle to maintain normal electrical activity, leading to arrhythmias or even cardiac arrest in severe cases (National Institutes of Health). Overconsumption of electrolyte drinks, particularly those high in sodium or potassium, can further exacerbate this imbalance. For people with underlying heart or kidney problems, the risk is even greater, as their bodies may be less capable of excreting excess fluids or electrolytes efficiently (American Heart Association).
It is crucial to balance fluid and electrolyte intake according to individual needs, physical activity, and environmental conditions. Monitoring for symptoms such as swelling, confusion, or irregular heartbeat can help prevent overhydration-related heart complications, especially in vulnerable populations.
9. Arrhythmias from Electrolyte Imbalance

Arrhythmias, or abnormal heart rhythms, often stem from imbalances in key electrolytes such as sodium, potassium, calcium, and magnesium. The heart’s electrical system depends on precise concentrations of these minerals to transmit signals effectively. When electrolyte levels are too high or too low, the electrical impulses that regulate heartbeats can become erratic, resulting in arrhythmias (American Heart Association Journals).
For example, hyperkalemia (excess potassium) can cause the heart to beat too slowly or even stop, while hypokalemia (low potassium) can trigger rapid or irregular heartbeats. Similarly, high calcium levels may lead to dangerous tachycardia, whereas low calcium can result in a slowed heart rate and muscle weakness. Sodium imbalances can also disrupt the normal rhythm, with hyponatremia leading to confusion and, in severe cases, seizures and cardiac arrest (National Center for Biotechnology Information).
Early detection and management of electrolyte imbalances are critical for preventing arrhythmias and related heart complications. Regular monitoring, especially for individuals with chronic health conditions or those taking certain medications, can help maintain cardiac stability and overall health.
10. Sudden Cardiac Arrest and Electrolytes

Sudden cardiac arrest (SCA) is a life-threatening event in which the heart unexpectedly stops beating, often triggered by severe electrolyte imbalances. Electrolytes such as potassium, sodium, calcium, and magnesium are essential for maintaining the heart’s electrical stability. When these minerals fall outside their normal ranges—either from excessive loss (as can happen with intense exercise and heavy sweating) or overconsumption—dangerous arrhythmias can develop and, in extreme cases, progress to cardiac arrest (Mayo Clinic).
Athletes are particularly vulnerable because they may lose large amounts of electrolytes through sweat or attempt rapid rehydration with electrolyte-rich drinks, both of which can disrupt the delicate balance required for normal heart function. Conditions such as hypokalemia (low potassium), hyperkalemia (high potassium), hypocalcemia (low calcium), and severe hyponatremia (low sodium) can all precipitate lethal arrhythmias leading to SCA (National Institutes of Health).
Prompt recognition and correction of electrolyte disturbances are vital for preventing cardiac emergencies, particularly in high-risk groups like athletes. Awareness of symptoms such as palpitations, dizziness, or fainting should prompt immediate medical evaluation to prevent catastrophic outcomes.
11. Sports Drinks: Friend or Foe?

Sports drinks are widely marketed as essential for hydration and optimal performance, especially during intense exercise. These beverages typically contain a blend of electrolytes—primarily sodium, potassium, and sometimes magnesium and calcium—along with sugar and artificial flavors. While sports drinks can help replenish lost electrolytes and fluids during prolonged or vigorous activity, their routine consumption is not always necessary and can even pose risks if overused (Centers for Disease Control and Prevention).
One concern is the high sugar content found in many commercial sports drinks, which can contribute to weight gain, metabolic issues, and dental problems. Additionally, for individuals who are not engaging in strenuous activity, the extra sodium and other electrolytes may lead to imbalances and increase blood pressure or stress the kidneys. Overconsumption can also result in electrolyte overload, heightening the risk of arrhythmias and other heart-related problems (American Heart Association).
While sports drinks can be beneficial in specific scenarios, such as endurance sports or extreme heat, water is generally adequate for most people. Awareness of the ingredients and moderation are key to ensuring these beverages support, rather than harm, heart health.
12. Caffeine and Electrolyte Drinks

Many modern electrolyte drinks, especially those marketed as energy or performance beverages, contain caffeine in addition to minerals like sodium and potassium. While caffeine can enhance alertness and temporarily boost physical performance, its presence in electrolyte-rich drinks may compound potential heart risks (U.S. Food and Drug Administration).
Caffeine is a stimulant that increases heart rate and blood pressure, placing extra stress on the cardiovascular system. When combined with high doses of electrolytes, especially sodium, the risk of arrhythmias and elevated blood pressure may be amplified. This is particularly concerning for individuals with underlying heart conditions, hypertension, or sensitivity to stimulants. The combination can also mask signs of dehydration, prompting overconsumption of both fluids and caffeine, further disrupting electrolyte balance (American Heart Association).
Young people and athletes are at increased risk of adverse effects due to aggressive marketing of caffeinated electrolyte drinks. Symptoms such as palpitations, dizziness, or chest pain should not be ignored, and moderation is strongly advised. Consulting with a healthcare professional before using such products is recommended for those with cardiovascular concerns.
13. Kidney Function and Electrolyte Processing

The kidneys play a pivotal role in maintaining electrolyte balance by filtering the blood, removing excess minerals and waste, and regulating fluid levels. This process is essential for keeping the concentrations of sodium, potassium, calcium, and magnesium within narrow ranges—crucial for normal heart and muscle function. When the kidneys work efficiently, they help prevent dangerous spikes or drops in electrolyte levels, thus protecting the heart’s electrical stability (National Institute of Diabetes and Digestive and Kidney Diseases).
If kidney function is compromised due to chronic kidney disease, dehydration, or excessive intake of fluids and electrolytes, the body’s ability to regulate these minerals diminishes. This can lead to imbalances such as hyperkalemia (high potassium) or hypernatremia (high sodium), which place additional strain on the heart and may provoke arrhythmias or exacerbate hypertension. The heart must then work harder to compensate, increasing the risk of cardiovascular events (National Kidney Foundation).
Supporting kidney health through proper hydration, balanced nutrition, and regular medical checkups is vital for maintaining electrolyte harmony and reducing unnecessary stress on the heart and circulatory system.
14. Medications That Alter Electrolytes

Many widely prescribed medications can significantly affect electrolyte levels, with direct implications for heart health. Diuretics, commonly used to treat high blood pressure and heart failure, promote the excretion of sodium and water but may also deplete potassium and magnesium. This can increase the risk of arrhythmias and muscle weakness. Conversely, potassium-sparing diuretics may lead to elevated potassium levels, which can also disrupt normal heart rhythms (U.S. Food and Drug Administration).
Other medications that may shift electrolyte balance include certain blood pressure drugs (ACE inhibitors and angiotensin receptor blockers), laxatives, some antibiotics, and chemotherapy agents. These drugs can alter sodium, potassium, calcium, or magnesium levels, creating a risk for both hypo- and hyper-electrolyte states. Cardiac glycosides, used for heart failure and arrhythmias, are particularly sensitive to potassium fluctuations, which can amplify their effects and increase toxicity (National Center for Biotechnology Information).
Patients taking these medications should have their electrolyte levels regularly monitored and report symptoms such as palpitations, weakness, or confusion to their healthcare provider. Proper management can help prevent medication-induced cardiac complications.
15. Heart Disease and Electrolyte Sensitivity
Individuals with existing heart disease, such as heart failure, coronary artery disease, or arrhythmias, are often more sensitive to fluctuations in electrolyte levels. When the heart is already compromised, even minor changes in sodium, potassium, calcium, or magnesium can have pronounced effects on cardiac function. For example, a slight drop in potassium can trigger arrhythmias in someone with atrial fibrillation, while small increases in sodium can exacerbate fluid retention and worsen heart failure symptoms (American Heart Association).
This heightened sensitivity stems from the heart’s reduced ability to compensate for electrical disturbances and the body’s decreased resilience to stress. Additionally, underlying structural changes or impaired pumping capacity make the heart more vulnerable to electrolyte-driven disruptions in rhythm or contractility. People with heart disease are also more likely to be on medications that further affect electrolyte balance, amplifying the risk of complications (National Institutes of Health).
Regular monitoring of electrolyte levels, careful dietary management, and prompt attention to symptoms such as palpitations, swelling, or fatigue are essential strategies for protecting heart health in those with preexisting cardiovascular conditions.
16. Diabetes and Electrolyte Fluctuations

Diabetes, particularly when blood sugar levels are poorly controlled, can lead to significant fluctuations in electrolyte levels, thereby increasing the risk of heart complications. High blood glucose causes the body to excrete excess sugar through urine, which is often accompanied by the loss of water and essential electrolytes such as sodium, potassium, and magnesium. This mechanism can result in dehydration and imbalances that stress the cardiovascular system (Centers for Disease Control and Prevention).
People with diabetes are especially susceptible to both hyperkalemia (high potassium) and hypokalemia (low potassium), conditions that may trigger dangerous arrhythmias or exacerbate existing heart disease. Insulin, a key hormone in diabetes management, also influences the movement of potassium into cells, and changes in insulin therapy can further alter electrolyte balance. Diabetic ketoacidosis, a serious complication of uncontrolled diabetes, is notorious for causing severe shifts in sodium and potassium, sometimes leading to life-threatening cardiac events (National Center for Biotechnology Information).
Careful monitoring of blood sugar and electrolytes, as well as prompt management of dehydration and metabolic disturbances, are essential for individuals with diabetes to minimize heart risks associated with electrolyte fluctuations.
17. Age and Electrolyte Needs

As people age, their bodies undergo physiological changes that affect how electrolytes are processed and utilized. Kidney function naturally declines with age, reducing the body’s ability to filter excess electrolytes and maintain fluid balance. This makes older adults more susceptible to both dehydration and electrolyte imbalances, conditions that can significantly impact heart function (National Institute on Aging).
Additionally, the aging heart becomes less adaptable to stress and more vulnerable to rhythm disturbances caused by fluctuations in sodium, potassium, calcium, and magnesium. Medications commonly prescribed to seniors, such as diuretics and heart drugs, can further influence electrolyte levels, increasing the risk of arrhythmias or heart failure exacerbation (National Institutes of Health).
Older adults may also have a diminished sense of thirst, leading to inadequate fluid intake and a higher risk of dehydration. Regular monitoring, individualized fluid and electrolyte recommendations, and prompt attention to symptoms like dizziness, weakness, or palpitations are critical for protecting heart health in the aging population. Proper management can help prevent hospitalizations and improve quality of life for seniors.
18. Gender Differences in Heart Response

Research suggests that men and women can respond differently to changes in electrolyte balance, affecting their risk for heart-related complications. Hormonal differences, particularly the influence of estrogen and progesterone in women, impact how electrolytes such as sodium and potassium are regulated. For example, estrogen is thought to enhance renal sodium excretion, potentially making women less susceptible to sodium-induced hypertension before menopause (American Heart Association Journals).
Women are also more likely to experience certain types of arrhythmias, such as long QT syndrome, which can be triggered or worsened by electrolyte imbalances—especially low potassium or magnesium. Men, on the other hand, may be at increased risk for sudden cardiac arrest associated with high potassium levels (National Institutes of Health).
Additionally, fluid and electrolyte needs may vary based on body composition, hormonal cycles, and life stages such as pregnancy or menopause. These differences underscore the importance of personalized hydration and electrolyte management strategies. Awareness and monitoring of symptoms in both genders can help prevent cardiac events linked to electrolyte disturbances.
19. Heat, Sweat, and Electrolyte Loss
Exposure to high temperatures and intense physical activity significantly increases sweating, which is the body’s natural mechanism to cool itself. However, with sweat comes the loss of critical electrolytes such as sodium, potassium, and chloride. These losses can lead to dehydration and disrupt the delicate electrolyte balance necessary for optimal heart function (Centers for Disease Control and Prevention).
As electrolyte levels drop, the risk of arrhythmias, muscle cramps, and cardiovascular stress rises. Rapid or excessive loss of sodium through sweat can lead to hyponatremia, which impairs nerve and muscle function, including the heart’s electrical system. Potassium depletion is also concerning, as it can cause weakness, fatigue, and potentially dangerous heart rhythm disturbances (National Center for Biotechnology Information).
Athletes, outdoor workers, and individuals in hot climates should be especially vigilant about replacing both fluids and electrolytes. Relying solely on water during periods of heavy sweating may not be sufficient; replenishing lost electrolytes through balanced drinks or dietary sources is crucial for maintaining heart health and preventing complications from heat-related electrolyte loss.
20. Alcohol’s Effect on Electrolytes

Alcohol consumption can significantly disrupt electrolyte balance, leading to increased strain on the heart and heightened risk of cardiovascular complications. Alcohol acts as a diuretic, promoting increased urine output, which accelerates the loss of essential electrolytes such as sodium, potassium, and magnesium from the body (National Center for Biotechnology Information). This loss is often compounded by the fact that alcohol impairs the body’s ability to properly reabsorb fluids and minerals in the kidneys.
As electrolyte levels drop, the heart becomes more vulnerable to arrhythmias, palpitations, and even sudden cardiac events. Chronic alcohol use can also contribute to persistent magnesium deficiency, which is particularly concerning for heart rhythm stability. Furthermore, binge drinking can result in rapid, severe shifts in electrolytes and fluid balance, greatly increasing the risk for acute complications such as atrial fibrillation or “holiday heart syndrome” (American Heart Association).
To protect heart health, it’s important to consume alcohol in moderation, stay hydrated with non-alcoholic fluids, and be mindful of symptoms like dizziness, muscle cramps, or irregular heartbeat, which could signal an imbalance requiring medical attention.
21. Fasting, Diets, and Heart Risks

Extreme diets and prolonged fasting can significantly disrupt electrolyte balance, posing potential risks to heart health. Diets that severely restrict food groups—such as very low-carbohydrate, low-calorie, or juice cleanses—may lack adequate sources of sodium, potassium, magnesium, and calcium. During fasting, the body continues to lose electrolytes through urine, sweat, and respiration, but without regular intake, these essential minerals are not replenished (National Center for Biotechnology Information).
These electrolyte shifts can result in symptoms ranging from muscle cramps and weakness to life-threatening arrhythmias and cardiac arrest. Rapid weight loss, commonly seen with crash diets, can also cause sudden drops in potassium and magnesium, heightening the risk for abnormal heart rhythms (American Heart Association). Individuals with preexisting heart conditions or those taking medications that affect electrolytes are at even greater risk for complications.
Before embarking on extreme diets or fasting regimens, it is essential to consult a healthcare professional. A balanced diet that provides sufficient electrolytes—along with regular monitoring and gradual adjustments—can help prevent dangerous shifts and support both heart and overall health.
22. High-Performance Athletes’ Heart Hazards

High-performance athletes face unique cardiovascular risks due to the rapid loss and sometimes excessive replacement of electrolytes during intense training or competition. Strenuous exercise increases sweat production, which can deplete key electrolytes such as sodium, potassium, and magnesium at a much faster rate than in less active individuals. If these losses are not adequately replenished, athletes may experience muscle cramps, fatigue, and dangerous arrhythmias (National Institutes of Health).
Conversely, overzealous rehydration with water or electrolyte-rich beverages can lead to imbalances such as hyponatremia (low sodium) or hyperkalemia (high potassium). Both conditions are associated with impaired heart rhythm and, in extreme cases, sudden cardiac arrest. The risk is particularly pronounced during endurance events like marathons or triathlons, where the combination of prolonged exertion, high fluid turnover, and variable electrolyte intake can create a perfect storm for cardiac events (American Heart Association).
To minimize risks, athletes should tailor their hydration and electrolyte strategies to their individual needs, accounting for sweat rate, environmental conditions, and duration of activity. Regular monitoring and consultation with sports health professionals are vital for peak performance and heart safety.
23. Children and Electrolyte Drinks

The use of electrolyte drinks in children has grown increasingly common, but their safety and effects on heart health warrant careful consideration. While these beverages are sometimes necessary for treating dehydration due to vomiting, diarrhea, or prolonged physical activity, routine consumption is generally unnecessary for healthy children. Most sports drinks contain high levels of sugar and sodium, which can promote unhealthy weight gain, dental issues, and potentially increase blood pressure (American Academy of Pediatrics).
Children’s bodies are more sensitive to shifts in electrolyte balance than adults. Overconsumption of electrolyte drinks can lead to excessive sodium or potassium levels, putting strain on the heart and increasing the risk of arrhythmias or high blood pressure, especially in those with underlying health conditions. The American Heart Association advises that water is sufficient for most children, except in cases of illness-related dehydration or intense exercise lasting longer than an hour.
Parents should read labels carefully and consult healthcare providers before giving children electrolyte drinks. Encouraging a balanced diet and proper hydration with water remains the best approach for supporting healthy growth and heart function in kids.
24. Electrolyte Supplements: Pros and Cons

Electrolyte supplements are available in various forms, including tablets, powders, and liquids, and are often marketed for hydration, athletic recovery, or to counteract deficiencies. These supplements can be beneficial for individuals with increased needs, such as those experiencing heavy sweating, gastrointestinal illness, or certain medical conditions. In such cases, supplements can help prevent dehydration, muscle cramps, and support normal heart rhythm (Mayo Clinic).
However, indiscriminate or excessive use of electrolyte supplements may do more harm than good. Over-supplementation can lead to dangerous imbalances, such as hyperkalemia (high potassium) or hypernatremia (high sodium), both of which can provoke arrhythmias or elevate blood pressure. Some supplements also contain added sugars or artificial ingredients, which may be counterproductive for heart health. Individuals with kidney disease, hypertension, or heart disease are particularly at risk for complications related to improper electrolyte intake (Cleveland Clinic).
For most people, a balanced diet rich in fruits, vegetables, and whole foods provides sufficient electrolytes. Supplements should only be used when medically indicated and under healthcare supervision to ensure optimal heart and overall health.
25. Hospital IV Electrolytes and the Heart

In hospital settings, intravenous (IV) electrolyte solutions are often administered to quickly correct imbalances caused by dehydration, illness, surgery, or certain medical treatments. Common IV electrolytes include sodium chloride, potassium chloride, calcium gluconate, and magnesium sulfate. Because these minerals are delivered directly into the bloodstream, their effects on the heart can be immediate and profound, particularly in critically ill patients (National Center for Biotechnology Information).
IV electrolyte therapy is closely monitored to avoid overcorrection, which can be just as dangerous as deficiency. Continuous cardiac monitoring is standard when administering potassium, magnesium, or calcium, as rapid shifts in these electrolytes can trigger arrhythmias, cardiac arrest, or other life-threatening complications. Dosages are tailored to the patient’s specific needs, underlying conditions, and current laboratory values. The Merck Manual notes that careful adjustment and ongoing assessment are essential for patient safety.
IV electrolyte replacement is a powerful tool in acute care, but it requires skilled oversight to protect the heart and ensure the best possible outcomes for patients with complex medical needs.
26. Diuretics and Heart Strain

Diuretics, commonly known as “water pills,” are medications frequently prescribed to treat high blood pressure, heart failure, and edema by promoting the removal of excess fluid through urine. While diuretics help reduce the workload on the heart by decreasing blood volume, they can also lead to significant changes in electrolyte levels—most notably, sodium, potassium, and magnesium (American Heart Association).
Thiazide and loop diuretics, in particular, may cause the body to lose too much potassium and magnesium, increasing the risk of arrhythmias and muscle weakness. Conversely, potassium-sparing diuretics can sometimes lead to dangerously high potassium levels, especially in those with kidney dysfunction. Both low and high potassium states can disrupt the heart’s electrical activity, leading to irregular heartbeats, palpitations, or even sudden cardiac events (National Center for Biotechnology Information).
Patients taking diuretics should have their electrolyte levels checked regularly and be mindful of symptoms such as muscle cramps, fatigue, or abnormal heart rhythms. Dietary modifications or supplementation may be necessary to maintain a safe electrolyte balance and protect cardiac health while on these medications.
27. Thyroid Issues and Electrolyte Disruption
Thyroid disorders, including both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid), can significantly disrupt electrolyte balance and impact heart rhythms. The thyroid gland produces hormones that regulate metabolism, which in turn influences how the body processes and distributes electrolytes such as sodium, potassium, and calcium (National Center for Biotechnology Information).
In hyperthyroidism, the body’s metabolic rate increases, often leading to greater renal excretion of electrolytes and a higher risk of low potassium (hypokalemia) and low magnesium. These shifts can precipitate arrhythmias, including atrial fibrillation, a rapid and irregular heart rhythm associated with stroke and heart failure. Hypothyroidism, on the other hand, can cause the body to retain more water and sodium, sometimes resulting in low sodium levels (hyponatremia), which may cause fatigue, confusion, or in severe cases, abnormal heart rhythms (American Thyroid Association).
Because thyroid dysfunction can make the heart more sensitive to even minor electrolyte changes, regular monitoring and appropriate management of both thyroid hormone levels and electrolytes are crucial. Timely treatment helps reduce the risk of dangerous cardiac complications and ensures better overall health outcomes.
28. Salt Substitutes and Hidden Risks

Salt substitutes are often marketed as a healthier alternative to regular table salt, especially for individuals seeking to lower their sodium intake and manage blood pressure. These products typically replace some or all of the sodium chloride with potassium chloride. While this substitution can help reduce sodium-related risks, it introduces potential hidden dangers, particularly for people with heart or kidney problems (U.S. Food and Drug Administration).
Excess potassium from salt substitutes can lead to hyperkalemia, a condition characterized by dangerously high potassium levels in the blood. Hyperkalemia can disrupt the electrical conduction system of the heart, resulting in abnormal rhythms (arrhythmias), muscle weakness, or even sudden cardiac arrest. Individuals taking medications such as ACE inhibitors, angiotensin receptor blockers, or potassium-sparing diuretics are at greater risk, as these drugs can also elevate potassium (American Heart Association).
Before using salt substitutes, it is important to consult with a healthcare provider, especially for those with kidney disease or heart conditions. Regular monitoring of potassium levels can prevent unintended complications and support safe dietary changes for heart health.
29. Digestion and Electrolyte Absorption
Gut health plays a fundamental role in maintaining electrolyte balance, as most electrolyte absorption occurs in the digestive tract. Conditions that impair the gut’s ability to absorb nutrients—such as Crohn’s disease, celiac disease, chronic diarrhea, or surgical removal of intestinal segments—can lead to significant deficiencies in sodium, potassium, magnesium, and calcium (National Center for Biotechnology Information).
Malabsorption disorders can cause chronic or acute electrolyte imbalances, heightening the risk for dehydration and triggering heart complications like arrhythmias, palpitations, or even heart failure. Persistent diarrhea or vomiting accelerates the loss of both fluids and minerals, placing extra stress on the cardiovascular system. In severe cases, rapid shifts in electrolytes may lead to dangerous changes in heart rhythm and blood pressure (Mayo Clinic).
Managing gut health through proper diagnosis and treatment of gastrointestinal disorders is essential for restoring and maintaining electrolyte balance. Supplementation, hydration, and tailored medical care can help reduce cardiac risks and improve quality of life for those affected by chronic malabsorption or digestive conditions.
30. Chronic Illness and Ongoing Balance

Managing electrolyte balance is particularly challenging for individuals living with chronic illnesses such as kidney disease, heart failure, or liver cirrhosis. These conditions often impair the body’s ability to regulate fluid and electrolyte levels, increasing the risk of both deficiency and overload. For example, in chronic kidney disease, the kidneys lose their capacity to excrete excess potassium, sodium, and fluid, which can result in dangerous imbalances that threaten heart rhythm and function (National Kidney Foundation).
Heart failure patients may experience fluid retention and are frequently prescribed diuretics to manage swelling and congestion. However, diuretics can further disrupt electrolyte levels, leading to low potassium or magnesium, both of which are critical for heart rhythm stability (American Heart Association). The delicate interplay between medication, diet, and disease progression necessitates regular monitoring and individualized treatment plans.
Ongoing collaboration with healthcare providers, routine blood tests, and symptom tracking are essential for those with chronic illness to maintain a safe electrolyte balance. Proper management not only helps prevent cardiac complications but also improves overall quality of life and disease outcomes.
31. Stress and Electrolyte Shifts
Chronic or acute psychological stress can significantly impact electrolyte balance, thereby increasing pressure on the heart. When the body is under stress, it releases hormones such as cortisol and adrenaline, which promote fluid retention and alter the redistribution of sodium, potassium, and other electrolytes throughout the body (National Institutes of Health). This hormonal response can lead to elevated blood pressure, increased heart rate, and a higher risk of arrhythmias.
High stress levels may also drive behavioral changes, such as poor dietary choices, excessive caffeine or alcohol consumption, and inadequate hydration—all of which can further disrupt electrolyte status. In severe cases, such as during panic attacks or medical emergencies, the body’s rapid fluid and electrolyte shifts can induce palpitations, muscle cramps, or even cardiac events, particularly in individuals with preexisting heart disease (American Heart Association).
To minimize the heart risks associated with stress-induced electrolyte changes, it is important to adopt healthy coping strategies, maintain a balanced diet, and stay hydrated. Regular relaxation practices and medical guidance can help protect cardiovascular health in the face of ongoing stress.
32. Early Signs of Electrolyte Imbalance

Electrolyte imbalances can develop subtly, but certain early symptoms serve as important warning signs of underlying heart stress or impending complications. Common symptoms include muscle cramps, weakness, fatigue, and abnormal sensations like tingling or numbness. More specific to the cardiovascular system, individuals might notice heart palpitations, irregular or rapid heartbeat, dizziness, or unexplained episodes of lightheadedness (Cedars-Sinai).
Additional early signs may include headaches, confusion, nausea, vomiting, and, in severe cases, fainting. These symptoms result from disruptions in the heart’s electrical conduction and impaired nerve signaling, both of which depend on balanced electrolyte levels. In people with preexisting heart disease, even mild electrolyte shifts can quickly escalate to serious problems like arrhythmias or chest pain (Cleveland Clinic).
Recognizing these early indicators is vital for prompt intervention and preventing dangerous cardiac events. Anyone experiencing persistent or severe symptoms should seek medical attention. Routine blood tests and regular monitoring can help detect imbalances before they become life-threatening, especially in high-risk individuals.
33. When to Seek Emergency Care
Certain symptoms of electrolyte imbalance signal a potentially life-threatening problem and require immediate medical attention. Red flag signs include severe or persistent chest pain, sudden onset of palpitations or irregular heartbeat, fainting or loss of consciousness, and difficulty breathing. These symptoms may indicate that electrolyte disturbances are causing dangerous arrhythmias or acute heart failure (Mayo Clinic).
Other urgent warning signs include severe muscle weakness or paralysis, profound confusion or inability to stay awake, uncontrollable vomiting or diarrhea, and seizures. In people with known heart disease, diabetes, or kidney problems, even milder symptoms such as dizziness, swelling, or sudden changes in mental status should prompt a call to emergency services (Centers for Disease Control and Prevention).
Time is critical in these situations, as untreated electrolyte imbalances can rapidly progress to cardiac arrest or other catastrophic outcomes. Do not attempt self-treatment or delay seeking help—call emergency services or go to the nearest emergency room if you or someone you know experiences these red flag symptoms.
34. Lab Tests for Electrolyte Levels
Blood tests are essential tools for assessing electrolyte balance and identifying potential risks to heart health. The most common laboratory evaluations include the basic metabolic panel (BMP) and comprehensive metabolic panel (CMP), both of which measure levels of key electrolytes: sodium, potassium, chloride, bicarbonate (CO₂), calcium, and sometimes magnesium and phosphate. These tests provide a snapshot of how well the body is regulating fluids, acid-base status, and essential minerals (MedlinePlus).
Normal reference ranges are generally:
Sodium: 135-145 mmol/L
Potassium: 3.5-5.0 mmol/L
Chloride: 98-107 mmol/L
Calcium: 8.5-10.2 mg/dL
Magnesium: 1.7-2.2 mg/dL
Values outside these ranges may indicate dehydration, kidney dysfunction, heart problems, or effects from medications and require further investigation. Interpretation of results must consider the patient’s symptoms, medical history, and current medications. Abnormal results often prompt additional tests or treatment adjustments to restore safe electrolyte levels, preventing arrhythmias and other heart complications (Cleveland Clinic).
35. Holistic Hydration Approaches

Balanced hydration goes beyond simply drinking water or consuming electrolyte beverages—it involves a comprehensive approach that includes dietary choices and lifestyle habits. Many fruits and vegetables, such as watermelon, oranges, cucumbers, and leafy greens, are naturally rich in both water and essential electrolytes like potassium and magnesium. Incorporating these foods into daily meals helps maintain optimal fluid and electrolyte balance, supporting both heart and overall health (Harvard T.H. Chan School of Public Health).
Hydration needs vary based on age, activity level, climate, and individual health conditions. Rather than relying solely on sports or electrolyte drinks, experts recommend drinking water regularly throughout the day and eating a variety of nutrient-dense foods. This holistic strategy helps prevent both dehydration and dangerous electrolyte imbalances. Monitoring urine color (pale yellow indicates good hydration) and being attentive to thirst cues are simple yet effective ways to gauge hydration status (Centers for Disease Control and Prevention).
For most people, a diet rich in whole foods and regular water intake is sufficient. Those with increased needs—due to illness, exercise, or climate—should adjust their intake accordingly, ideally under the guidance of a healthcare professional.
36. Electrolyte Drinks vs. Plain Water

Choosing between electrolyte drinks and plain water depends largely on individual needs, activity levels, and underlying health conditions. For most people engaging in everyday activities, plain water is the healthiest choice for hydration. It effectively maintains fluid balance without adding sugars, calories, or excess electrolytes, which is ideal for heart health and overall well-being (Centers for Disease Control and Prevention).
Electrolyte drinks are specifically designed to replace minerals lost through heavy sweating, vomiting, diarrhea, or prolonged intense exercise. In these scenarios, such beverages can prevent dangerous imbalances that might lead to muscle cramps, fatigue, or arrhythmias. However, for people who are not losing high amounts of electrolytes, these drinks may introduce excessive sodium or sugar, which can raise blood pressure, promote weight gain, and strain the heart (American Heart Association).
The key is moderation and appropriateness: water suffices for routine hydration, while electrolyte drinks should be reserved for times when there is a true risk of deficiency. Individuals with heart or kidney issues should consult healthcare professionals before using electrolyte beverages regularly.
37. Reading Labels: Hidden Sodium and Sugar

Reading nutrition labels is crucial for understanding what you’re really consuming in electrolyte drinks, many of which contain surprisingly high levels of sodium and sugar. Excess sodium can elevate blood pressure, increase heart workload, and contribute to long-term cardiovascular disease, while added sugars can lead to weight gain, insulin resistance, and metabolic syndrome—all of which are risk factors for heart problems (Centers for Disease Control and Prevention).
When choosing an electrolyte drink, check the “Sodium” and “Total Sugars” lines on the Nutrition Facts panel. Some sports drinks contain up to 400 mg of sodium and 30 grams of sugar per serving—quantities that can quickly exceed daily recommendations if consumed in large amounts. Ingredient lists may also reveal hidden forms of sugar such as high-fructose corn syrup, sucrose, or dextrose (American Heart Association).
Opting for drinks with lower sodium and sugar content, or making your own diluted versions, can help protect heart health. For most people, water and a balanced diet are the safest choices, with electrolyte drinks reserved for specific, medically indicated situations.
38. Home Monitoring of Heart Health

Advancements in technology have made it easier than ever to monitor heart health from home. Wearable devices such as smartwatches and fitness trackers can continuously track heart rate, rhythm, and even detect irregularities like atrial fibrillation. Many of these devices offer real-time alerts if they detect abnormal heart activity, allowing users to seek prompt medical attention (American Heart Association).
Other home tools include portable ECG (electrocardiogram) monitors, blood pressure cuffs, and pulse oximeters. These devices can provide valuable data on resting heart rate, variability, and blood pressure trends, all of which are influenced by electrolyte balance. Regular home monitoring is especially beneficial for individuals with known heart conditions, those taking medications that affect electrolytes, or people recovering from recent cardiac events (Centers for Disease Control and Prevention).
While these tools do not replace professional medical evaluation, they can help track patterns, detect early warning signs of electrolyte imbalances, and facilitate more informed conversations with healthcare providers. Always consult a physician about concerning changes or persistent symptoms detected through home monitoring.
39. Role of Fiber in Electrolyte Retention

Dietary fiber, found in fruits, vegetables, whole grains, and legumes, plays a crucial role in digestive health and can also aid in maintaining electrolyte balance. Fiber helps regulate the rate at which nutrients, including electrolytes like potassium, magnesium, and calcium, are absorbed in the digestive tract. By slowing gastric emptying and improving gut health, fiber promotes more consistent absorption of these minerals, helping to prevent rapid fluctuations that could impact heart rhythm and function (Harvard T.H. Chan School of Public Health).
Fiber-rich foods also support hydration by holding water in the digestive system, which can be particularly beneficial in preventing dehydration and the associated loss of electrolytes through diarrhea or loose stools. Stable electrolyte levels are essential for proper nerve signaling, muscle contraction, and maintaining a steady heartbeat (National Institutes of Health).
Including a variety of fiber sources in your diet not only supports cardiovascular health directly by lowering cholesterol and blood pressure but also indirectly by enhancing electrolyte retention. This holistic dietary approach is especially important for individuals at risk of heart disease or those experiencing frequent electrolyte disturbances.
40. Travel, Climate, and Heart Risks
Traveling—especially to regions with drastically different climates—can significantly impact hydration and electrolyte needs, thereby influencing heart health. Hot, humid environments increase sweat production and accelerate the loss of sodium, potassium, and other electrolytes, raising the risk of dehydration and heart rhythm disturbances. Conversely, high altitudes or cold climates can also cause fluid shifts, alter thirst perception, and potentially lead to subtle but important electrolyte imbalances (Centers for Disease Control and Prevention).
Air travel itself poses unique challenges, as cabin air is dry, and the body can lose additional fluids through respiration. Long flights or trips with limited access to drinking water may increase the risk of dehydration, particularly in older adults and those with preexisting heart or kidney conditions. Changes in time zones can also disrupt medication schedules for people who rely on diuretics or other drugs that affect electrolytes (American Heart Association).
To protect heart health during travel, it’s important to drink fluids consistently, adjust electrolyte intake based on activity and climate, and monitor for symptoms such as dizziness, weakness, or palpitations. Consulting a healthcare provider before significant travel is recommended for those with heart conditions.
41. Plant-Based Diets and Electrolytes

Plant-based diets, which emphasize fruits, vegetables, legumes, nuts, seeds, and whole grains, naturally provide an abundance of key electrolytes—particularly potassium and magnesium—while typically being lower in sodium than diets high in processed foods. Increased intake of potassium-rich foods such as bananas, sweet potatoes, spinach, and beans supports healthy blood pressure and reduces the risk of heart disease by helping to counteract the effects of sodium (Harvard T.H. Chan School of Public Health).
Magnesium, found in leafy greens, whole grains, and nuts, is essential for stable heart rhythm and is plentiful in plant-based diets. The reduced sodium content of these diets further protects against hypertension and fluid retention, both of which can strain the heart. However, individuals on strict plant-based or vegan diets should be mindful of consuming enough calcium, as some plant foods contain compounds that may inhibit calcium absorption. Fortified plant milks, tofu, and certain leafy greens can help meet calcium needs (National Institutes of Health).
Overall, a well-balanced plant-based diet supports electrolyte balance and heart health, but careful planning ensures all mineral needs are consistently met for optimal cardiovascular protection.
42. Medically Supervised Rehydration

While mild dehydration can often be corrected by drinking water or oral rehydration solutions at home, certain situations call for medically supervised rehydration and electrolyte replacement. This is especially true for individuals with underlying heart, kidney, or liver disease, as well as for infants, older adults, or those experiencing severe vomiting, diarrhea, or heat-related illness. In these cases, improper rehydration can quickly lead to dangerous electrolyte shifts, putting the heart at significant risk (Mayo Clinic).
Medical professionals are able to assess the severity of dehydration and electrolyte imbalance through physical examination and laboratory testing. They can then tailor intravenous (IV) fluid and electrolyte therapy to individual needs, closely monitoring cardiac status and adjusting treatment as necessary. Professional supervision helps prevent complications such as fluid overload, arrhythmias, or worsening organ dysfunction, which can result from overly rapid or inappropriate electrolyte replacement (National Center for Biotechnology Information).
Anyone with significant symptoms—such as confusion, persistent vomiting, chest pain, rapid heartbeat, or inability to keep fluids down—should seek medical care promptly. Timely intervention is critical for safe recovery and protecting long-term heart health.
43. Myths About Electrolyte Drinks

Electrolyte drinks are often marketed as essential for everyone’s hydration and heart health, but several myths persist around their necessity and safety. One common misconception is that these drinks are needed for all types of physical activity or daily life; in reality, most people meet their hydration and electrolyte needs through a balanced diet and water, unless they engage in prolonged, vigorous exercise, experience severe illness, or are exposed to extreme heat (Centers for Disease Control and Prevention).
Another myth is that electrolyte drinks are always safe and heart-friendly. In truth, many commercial options contain high levels of sugar and sodium, which can contribute to hypertension, weight gain, and increased cardiovascular risk if consumed excessively. Even “zero sugar” or “low calorie” variants may contain artificial additives that offer no heart benefit (American Heart Association).
It’s also falsely believed that more electrolytes are always better; in fact, overconsumption can lead to dangerous imbalances, such as hypernatremia or hyperkalemia, with direct effects on heart rhythm. Informed choices and moderation are key for heart-healthy hydration.
44. Electrolytes and Blood Clotting
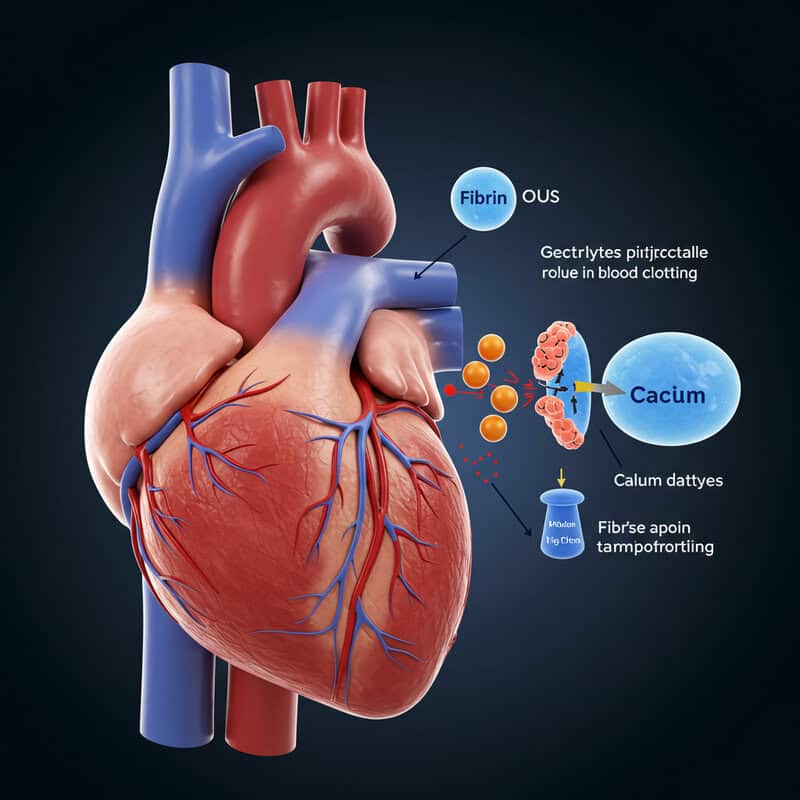
Certain electrolytes, particularly calcium, play a direct role in the blood clotting process, which has important implications for heart health. Calcium is essential for the activation of various clotting factors in the blood, enabling the transformation of fibrinogen to fibrin and ultimately helping to form stable blood clots (National Center for Biotechnology Information). Insufficient calcium can disrupt this cascade, increasing the risk of excessive bleeding, while excessively high calcium levels might contribute to abnormal clot formation.
Sodium and potassium also influence blood vessel tone and overall hemodynamics, indirectly affecting the likelihood of clot formation. For example, high sodium intake can raise blood pressure and promote arterial stiffness, factors that may increase the risk of clot-related events like heart attack or stroke (American Heart Association).
Magnesium, another vital electrolyte, helps regulate vascular tone and platelet function, providing a protective effect against unwanted clotting and supporting overall cardiovascular health. Thus, maintaining balanced electrolyte levels is crucial not only for rhythm and hydration but also for preventing complications from abnormal blood clotting that could endanger the heart.
45. Alcohol Withdrawal and Heart Arrhythmias

Alcohol withdrawal is a medically complex process that can lead to sudden and severe electrolyte shifts, significantly increasing the risk of heart arrhythmias. Chronic alcohol use often results in deficiencies of key electrolytes such as potassium, magnesium, and calcium due to poor dietary intake, gastrointestinal losses, and decreased absorption (National Center for Biotechnology Information). When alcohol consumption abruptly stops, the body’s chemistry can change rapidly, causing further imbalances as fluids and electrolytes redistribute.
These rapid shifts can destabilize the heart’s electrical system, precipitating dangerous arrhythmias such as atrial fibrillation, ventricular tachycardia, or even life-threatening ventricular fibrillation. Symptoms may include palpitations, chest pain, shortness of breath, dizziness, or fainting. Individuals with preexisting heart conditions, malnutrition, or liver dysfunction are particularly vulnerable during alcohol withdrawal (American Heart Association Journals).
Medical supervision is essential during withdrawal to monitor and correct electrolyte levels, manage symptoms, and reduce the risk of cardiac complications. Prompt intervention with intravenous fluids, electrolyte replacement, and continuous cardiac monitoring can be life-saving during this critical period.
46. Electrolytes in Popular Diet Trends
Popular diet trends such as keto, paleo, and low-carb regimens can have a profound impact on electrolyte balance, influencing heart health in the process. The ketogenic diet, which involves drastically reducing carbohydrate intake, leads to increased water and sodium loss through urine during the initial adaptation phase, often resulting in symptoms known as the “keto flu” (fatigue, dizziness, palpitations) caused by low sodium, potassium, and magnesium levels (National Institutes of Health).
Paleo and low-carb diets, while emphasizing whole foods and reducing processed salt, may inadvertently lower sodium and potassium intake if not carefully planned. This can increase the risk of dehydration and arrhythmias, particularly for those with underlying cardiovascular conditions. On the other hand, these diets often include ample magnesium and calcium from nuts, seeds, and leafy greens, which can support heart rhythm if consumed in adequate amounts (Harvard T.H. Chan School of Public Health).
To maintain electrolyte and heart health on such diets, individuals should monitor intake of all key minerals, stay hydrated, and consider supplementation if symptoms of imbalance occur. Consulting a healthcare professional before starting restrictive diets can help prevent unintended cardiac risks.
47. Hospital Monitoring: The Cardiac Telemetry Unit

Hospitals use cardiac telemetry units to provide continuous, real-time monitoring of heart rhythm and vital signs for patients at risk of arrhythmias or electrolyte disturbances. In these specialized units, patients are connected to telemetry monitors that record electrical activity from the heart, allowing healthcare teams to promptly detect changes such as abnormal rhythms (arrhythmias), heart rate fluctuations, or conduction abnormalities (American Heart Association Journals).
For individuals with electrolyte imbalances—especially those receiving intravenous electrolyte replacement, taking diuretics, or recovering from surgery or cardiac events—frequent blood tests are performed to assess sodium, potassium, calcium, and magnesium levels. The telemetry system provides immediate feedback, so any dangerous changes can be addressed without delay. Nurses and physicians are trained to interpret both telemetry data and lab results, ensuring that interventions such as medication adjustments or additional monitoring are implemented quickly (National Center for Biotechnology Information).
This vigilant, round-the-clock surveillance is essential for preventing life-threatening complications and improving outcomes for vulnerable cardiac patients. It exemplifies the critical connection between electrolyte status and heart rhythm in acute medical care.
48. Electrolyte Imbalance in Cancer Treatment
Cancer treatments such as chemotherapy, radiation, and certain targeted therapies frequently disrupt electrolyte levels, placing additional strain on the heart. Chemotherapy agents can cause nausea, vomiting, diarrhea, and kidney dysfunction—all of which lead to significant losses of sodium, potassium, magnesium, and calcium. Some medications may also cause the body to retain or excrete electrolytes abnormally, compounding the risk of dangerous imbalances (National Cancer Institute).
When electrolytes are thrown out of balance, patients may experience symptoms such as muscle cramps, weakness, confusion, and, most critically, arrhythmias or heart failure. Hypokalemia (low potassium) and hypomagnesemia (low magnesium) are particularly common in cancer patients and can trigger irregular heart rhythms, which may be life-threatening if not corrected quickly (National Institutes of Health).
Due to these risks, cancer patients receiving aggressive treatments are closely monitored with regular blood tests and cardiac assessments. Proactive management—including electrolyte supplementation, hydration, and medication adjustments—helps reduce the likelihood of cardiac complications and supports safer, more effective cancer care.
49. Pregnancy, Electrolytes, and the Heart

Pregnancy brings significant changes to fluid and electrolyte balance, which can influence heart health for both mother and baby. As blood volume expands to support fetal development, the body’s need for sodium, potassium, calcium, and magnesium increases. Proper electrolyte management is critical, as imbalances can contribute to complications such as high blood pressure (preeclampsia), edema, muscle cramps, and cardiac arrhythmias (American College of Obstetricians and Gynecologists).
Nausea, vomiting, and changes in kidney function during pregnancy may lead to excessive loss of electrolytes, particularly in cases of severe morning sickness (hyperemesis gravidarum). Low potassium or magnesium can provoke heart palpitations or irregular heartbeats, while inadequate calcium intake impacts muscle and nerve function for both mother and fetus. Monitoring and supplementing electrolytes as needed can help prevent these issues and support a healthy pregnancy (National Institutes of Health).
Prenatal care providers typically recommend a balanced diet rich in fruits, vegetables, dairy, and whole grains to meet increased electrolyte needs. Regular blood pressure and electrolyte monitoring ensure early detection and management of any imbalances, safeguarding maternal and fetal heart health.
50. Optimizing Heart Health: Smart Electrolyte Choices

Safely managing electrolyte intake is essential for protecting and optimizing heart health throughout life. A balanced approach begins with a nutrient-rich diet that includes plenty of fruits, vegetables, whole grains, dairy products, and lean proteins—these foods offer natural sources of potassium, magnesium, calcium, and other key electrolytes without excess sodium or sugar (American Heart Association).
For most people, drinking water and consuming a variety of whole foods is sufficient to meet daily electrolyte needs. Electrolyte drinks and supplements should be reserved for situations involving heavy sweating, illness, or medical advice, and always used in moderation. Reading nutrition labels, monitoring portion sizes, and limiting processed foods can help avoid excessive sodium and sugar, both of which can strain the heart.
Regular physical activity, managing chronic conditions, and routine check-ups—including blood tests for electrolytes if indicated—are also crucial. Individuals with heart, kidney, or endocrine disorders should consult healthcare professionals for tailored guidance (Centers for Disease Control and Prevention).
Informed choices, attention to symptoms, and prevention-focused habits are the foundation for lasting heart health through smart electrolyte management.
Conclusion

Monitoring electrolyte intake is crucial for maintaining optimal heart health, as even minor imbalances can have significant cardiovascular consequences. Understanding the connection between hydration, diet, and the heart empowers individuals to make informed choices and recognize early warning signs. Regular health screenings, reading nutrition labels, and adopting balanced hydration habits are effective steps for prevention and well-being. For those with existing medical conditions, personalized advice from healthcare professionals is essential (CDC Heart Disease Prevention). Disclaimer: This article is for informational purposes only and should not replace professional medical advice. Always consult a healthcare provider before making changes to your diet, medication, or hydration practices.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





