When Fatigue Isn’t Just Fatigue — And What It Could Mean
Fatigue affects nearly one in five adults worldwide, with up to 45% of people reporting persistent tiredness at some point in their lives (source). While often dismissed as a normal response to stress or lack of sleep, fatigue can signal deeper issues involving the nervous, endocrine, or immune systems. Early recognition is challenging, as symptoms are often vague and overlap with common daily experiences. Understanding when fatigue may indicate a more serious underlying condition is essential for timely diagnosis and effective management.
1. Anemia
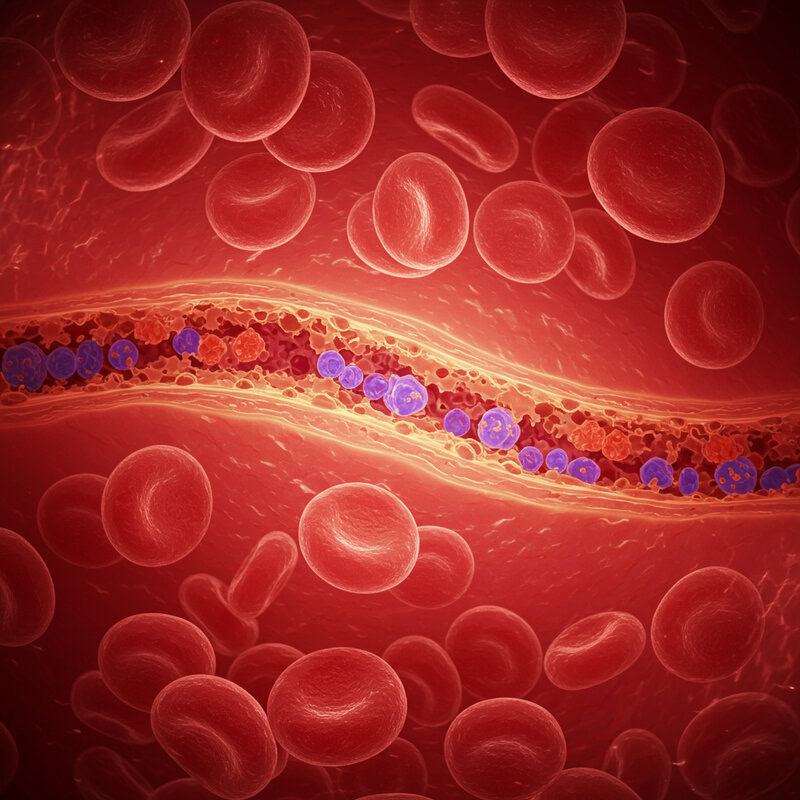
Anemia occurs when the body has a low red blood cell count or insufficient hemoglobin, reducing the blood’s ability to carry oxygen to tissues. This oxygen deficit can cause persistent fatigue, weakness, shortness of breath, and difficulty concentrating. Among the different types, iron deficiency anemia is the most common, arising from inadequate dietary iron, blood loss (such as heavy menstrual periods), or poor absorption. Other types include vitamin B12 or folate deficiency anemia, and chronic disease-related anemia (CDC).
People with anemia often notice that even mild activity leaves them exhausted, and the fatigue does not improve with rest. In some cases, symptoms may be accompanied by pale skin, rapid heartbeat, or dizziness. Because these signs can be subtle or attributed to other causes, many individuals remain undiagnosed. If you experience persistent, unexplained tiredness—especially with additional symptoms like paleness or heart palpitations—it’s important to talk to a healthcare provider about getting a blood test to check for anemia. Early detection and treatment are crucial to restoring energy and preventing complications (Mayo Clinic).
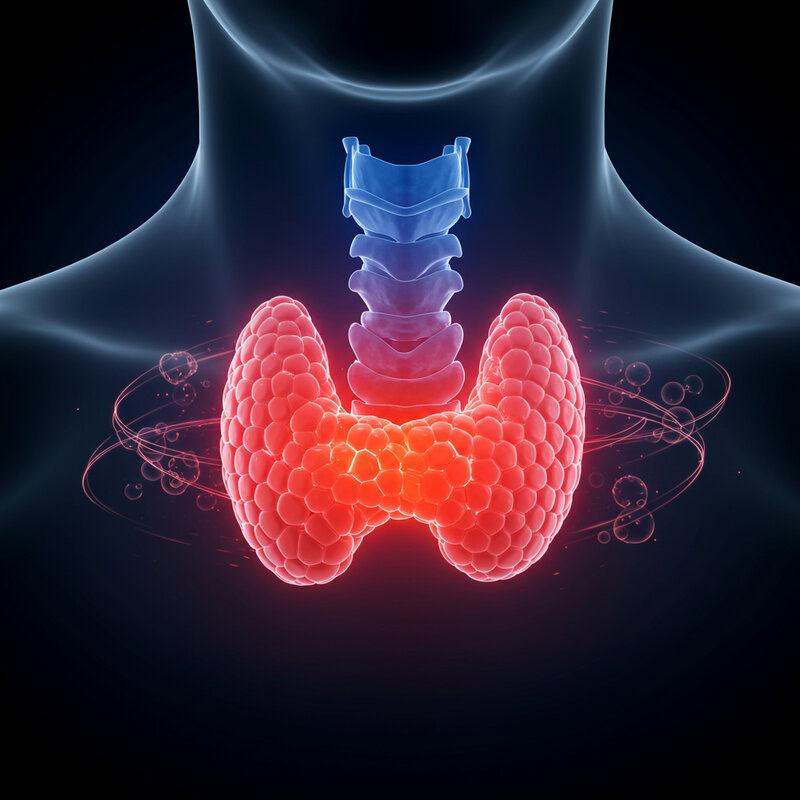
2. Hypothyroidism
Hypothyroidism is a condition where the thyroid gland produces insufficient thyroid hormones, leading to a generalized slowing of the body’s metabolism. Unlike the normal tiredness that follows exertion or poor sleep, the fatigue associated with hypothyroidism is persistent and often accompanied by other symptoms such as weight gain, dry skin, hair loss, constipation, and increased sensitivity to cold. The thyroid hormones play a crucial role in regulating energy production, so when levels are low, every cell in the body operates less efficiently (NIDDK).
This metabolic slowdown means people may feel sluggish throughout the day, regardless of rest or sleep quality. The fatigue can be profound and interfere with daily functioning, sometimes making even routine tasks feel overwhelming. Because hypothyroidism develops gradually, symptoms are often mistaken for normal aging or stress. If you notice persistent tiredness along with other signs—especially unexplained weight gain, changes in hair or skin, or feeling unusually cold—it is important to talk to your doctor. A simple blood test measuring thyroid-stimulating hormone (TSH) and thyroid hormones can confirm the diagnosis and guide appropriate treatment (Mayo Clinic).
3. Diabetes

Diabetes, particularly when blood sugar is poorly controlled, can significantly disrupt the body’s ability to use glucose for energy. Chronically high blood sugar leads to fatigue because, despite glucose being present in the bloodstream, cells are unable to absorb and utilize it efficiently. This results in persistent tiredness, regardless of sleep or activity level. Other related symptoms include increased thirst, frequent urination, blurred vision, and unexplained weight loss (CDC).
Consider the story of a patient named Maria, who began experiencing overwhelming fatigue that interfered with her daily routines. She initially attributed her exhaustion to working long hours, but when she also noticed excessive thirst and frequent bathroom trips, she saw her doctor. Blood tests revealed elevated blood glucose levels and a diagnosis of type 2 diabetes. With lifestyle changes and medication, Maria was able to regain her energy and improve her quality of life.
Monitoring blood glucose is crucial for anyone at risk or living with diabetes. Regular checks can help detect fluctuations early, allowing for timely intervention and better management. If you experience unexplained fatigue alongside other symptoms, ask your healthcare provider about screening for diabetes (American Diabetes Association).
4. Chronic Fatigue Syndrome (CFS/ME)

Chronic Fatigue Syndrome, also known as Myalgic Encephalomyelitis (CFS/ME), is a long-term, complex disorder characterized by profound, unexplained fatigue that does not improve with rest and is not caused by ongoing exertion. Unlike everyday tiredness, the fatigue in CFS/ME is severe enough to interfere significantly with daily activities and can worsen after physical or mental effort—a phenomenon known as post-exertional malaise. Other symptoms may include sleep disturbances, cognitive difficulties (“brain fog”), muscle or joint pain, and sore throat (CDC).
Diagnosing CFS/ME is challenging because there is no definitive test; instead, it is a diagnosis of exclusion, made after ruling out other medical conditions. The exact cause remains unknown, but it is believed to involve a combination of genetic, environmental, and immune factors. Red flags that warrant medical evaluation include fatigue lasting longer than six months, especially when accompanied by cognitive impairment, unrefreshing sleep, and worsening symptoms after exertion. If you experience these symptoms, it’s important to seek a healthcare provider familiar with CFS/ME for comprehensive assessment and support (National Institute of Neurological Disorders and Stroke).
5. Sleep Apnea

Sleep apnea is a common sleep disorder in which breathing repeatedly stops and starts during sleep, often due to airway obstruction (obstructive sleep apnea) or, less commonly, a failure of the brain to signal breathing muscles (central sleep apnea). These interruptions deprive the body and brain of adequate oxygen, causing frequent awakenings—many of which the person may not remember. As a result, individuals with sleep apnea often experience persistent daytime fatigue, even after what seems like a full night’s sleep (CDC).
Unlike insomnia, where people struggle to fall asleep or stay asleep, those with sleep apnea may fall asleep easily but awaken feeling unrefreshed. Loud snoring, gasping, or choking sounds at night are common signs, and bed partners often notice these episodes before the affected person does. Additional symptoms can include morning headaches, difficulty concentrating, mood disturbances, and increased risk of high blood pressure or heart disease.
If you or a loved one experiences excessive daytime sleepiness, loud snoring, or pauses in breathing during sleep, it’s essential to consult a healthcare provider. A sleep study, or polysomnography, is the gold standard for diagnosing sleep apnea and guiding effective treatment (Sleep Foundation).
6. Depression

Depression is a mood disorder that often manifests not only through emotional symptoms like sadness or hopelessness but also through persistent fatigue. This fatigue can be profound and may not improve with rest, making it difficult to perform everyday activities. Unlike the tiredness that follows physical exertion, depression-related fatigue is often accompanied by a sense of heaviness, lack of motivation, and difficulty concentrating. People may describe it as feeling “drained” or “weighed down,” affecting both mind and body (National Institute of Mental Health).
The distinction between mental and physical tiredness is important. While physical fatigue may respond to sleep or rest, mental fatigue in depression often persists regardless of lifestyle changes. Additional symptoms may include changes in appetite, sleep disturbances (too much or too little), irritability, and loss of interest in activities once enjoyed. It’s common for individuals to first seek help for ongoing tiredness, not realizing that it may be linked to their mental health.
If you experience persistent fatigue along with mood changes or loss of interest, it’s important to consider a mental health screening. Early recognition and treatment—through therapy, medication, or both—can make a significant difference (Mental Health America Depression Screening).
7. Heart Failure
Heart failure is a chronic condition in which the heart is unable to pump blood efficiently, leading to reduced delivery of oxygen and nutrients to the body’s tissues. This diminished circulation causes persistent fatigue and weakness, as the muscles and organs are deprived of the energy they need for normal function. Individuals may notice that even minor physical activity, such as climbing stairs or walking short distances, results in pronounced exhaustion (CDC).
Consider the story of John, a retiree who experienced increasing tiredness and found himself short of breath when doing simple chores around the house. He initially believed his fatigue was due to aging, but as his symptoms progressed to include swelling in his ankles and frequent nighttime urination, he sought medical help. John’s doctor diagnosed him with heart failure after a thorough evaluation and imaging studies. With proper treatment and lifestyle adjustments, John was able to better manage his energy levels and improve his quality of life.
It’s crucial to seek prompt medical attention if you experience fatigue alongside breathlessness, swelling, or chest discomfort. Early diagnosis and treatment can improve symptoms and outcomes (American Heart Association).
8. Cancer

Cancer-related fatigue is a profound and persistent exhaustion that can develop before a cancer diagnosis is made. Unlike ordinary tiredness, this type of fatigue is not relieved by rest and often worsens over time. It may be due to the cancer itself, as tumors can interfere with normal body processes, secrete substances that disrupt metabolism, or cause chronic inflammation. In some cases, fatigue is the earliest and most prominent symptom, preceding other signs such as unexplained weight loss, pain, or fever (National Cancer Institute).
For example, a patient named Linda began experiencing overwhelming fatigue that made it difficult for her to keep up with her job and family responsibilities. She initially attributed her symptoms to stress, but when the fatigue persisted and she noticed new, unexplained bruising, she consulted her doctor. Blood tests and further investigations revealed leukemia. Early diagnosis allowed Linda to start treatment promptly, improving her prognosis and quality of life.
Persistent, unexplained fatigue—especially when accompanied by other warning signs—should never be ignored. Regular cancer screenings and timely evaluation of new symptoms can be life-saving (American Cancer Society: Screening Guidelines).
9. Rheumatoid Arthritis

Rheumatoid arthritis (RA) is an autoimmune condition in which the body’s immune system mistakenly attacks the lining of the joints, causing chronic inflammation. This inflammatory process not only damages joints but also releases chemicals that can lead to whole-body symptoms, including significant fatigue. The fatigue in RA is often described as overwhelming and can persist regardless of rest, making it distinct from the localized pain and stiffness seen in osteoarthritis (CDC).
Unlike osteoarthritis, which typically results from wear and tear and is confined to specific joints, RA is systemic. This means it can affect multiple joints symmetrically and cause generalized symptoms such as low-grade fever, malaise, and especially energy depletion. The combination of chronic pain, disrupted sleep, and the metabolic demands of ongoing inflammation amplifies fatigue, sometimes making daily activities a challenge even in the absence of severe joint pain.
People experiencing persistent joint pain, swelling, or stiffness—especially if it lasts more than six weeks or involves multiple joints—should seek medical evaluation. Early diagnosis and treatment of RA can help control inflammation, preserve joint function, and reduce fatigue (American College of Rheumatology).
10. Kidney Disease

Chronic kidney disease (CKD) occurs when the kidneys gradually lose their ability to filter waste and excess fluids from the blood. As kidney function declines, toxins and metabolic byproducts accumulate in the body, leading to a range of symptoms—most notably, persistent fatigue. This fatigue often develops slowly and is accompanied by other signs such as swelling in the ankles, muscle cramps, changes in urination, and difficulty concentrating (CDC).
When kidney function drops to a critical level, dialysis becomes necessary to artificially remove waste products from the bloodstream. Patients on dialysis frequently report feeling more energetic after treatment, underscoring how toxin buildup contributes to profound tiredness. However, even those with early-stage CKD can experience significant fatigue before dialysis is required. The fatigue associated with kidney disease often persists despite adequate sleep and may worsen as the condition progresses.
Anyone experiencing persistent, unexplained fatigue—especially if accompanied by swelling, changes in urination, or high blood pressure—should consider asking their healthcare provider about kidney function testing. Early detection through blood and urine tests can help manage CKD and prevent further complications (National Kidney Foundation).
11. Liver Disease

The liver is central to the body’s energy production and metabolism, processing nutrients, detoxifying blood, and storing glucose for use between meals. When the liver is damaged or inflamed, as in liver disease, these vital processes are disrupted, often resulting in persistent fatigue. Fatigue can be one of the earliest and most noticeable symptoms of liver dysfunction, even before more obvious signs such as jaundice or abdominal swelling appear (Mayo Clinic).
Common causes of liver disease include viral infections like hepatitis B and C, excessive alcohol consumption, nonalcoholic fatty liver disease, and autoimmune conditions. Hepatitis often presents with fatigue, mild abdominal discomfort, and loss of appetite, progressing to more severe symptoms if untreated. Cirrhosis, or advanced scarring of the liver, further impairs metabolic functions, intensifying fatigue and increasing the risk of complications like fluid buildup and confusion.
If you notice ongoing tiredness along with symptoms such as yellowing of the skin or eyes, dark urine, or unexplained abdominal pain, it is important to consult a healthcare provider. Early testing for liver enzymes and viral hepatitis can identify liver disease and guide timely treatment (U.S. Department of Veterans Affairs: How the Liver Works).
12. Multiple Sclerosis (MS)

Multiple sclerosis (MS) is a chronic autoimmune disorder in which the immune system attacks the protective covering of nerve fibers in the central nervous system. This damage disrupts the efficient transmission of electrical signals between the brain and body, leading to a wide variety of symptoms—including profound, often unpredictable fatigue. Unlike ordinary tiredness, MS-related fatigue can be overwhelming and may occur suddenly, even after minimal activity. It is frequently cited by patients as one of the most disabling aspects of the disease (National Multiple Sclerosis Society).
For example, one individual with MS may find that walking a short distance leaves them utterly exhausted, while another may be able to remain active but suddenly need to rest for hours without warning. This fatigue is distinct from muscle weakness or sleepiness and can persist even if other symptoms are well controlled. The unpredictable nature of fatigue in MS often interferes with work, family, and social life.
If you experience persistent, unexplained fatigue along with other neurological signs—such as numbness, vision changes, or coordination issues—it is important to consult a neurologist. Early neurologic evaluation and MRI scans can help confirm an MS diagnosis and guide treatment (Mayo Clinic).
13. Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a group of progressive lung diseases, including emphysema and chronic bronchitis, that make it increasingly difficult to breathe. As lung function deteriorates, less oxygen reaches the bloodstream and, consequently, the body’s tissues. This lack of adequate oxygen delivery results in persistent fatigue, often described as a sense of exhaustion that is not relieved by rest. Shortness of breath, coughing, and increased mucus production are also hallmark symptoms (CDC).
The fatigue experienced with COPD differs from that of asthma. While both conditions can cause tiredness, asthma-related fatigue is typically episodic and associated with acute attacks, whereas COPD fatigue is more persistent and gradually worsens over time. In COPD, the body is in a near-constant state of low oxygen, which can sap energy for even simple tasks. This ongoing energy drain can significantly impact daily life, making activities like walking or dressing challenging.
If you have a history of smoking, exposure to lung irritants, or notice persistent breathlessness and fatigue, it’s important to request a lung function test (spirometry) from your healthcare provider. Early detection and intervention can help slow disease progression and improve quality of life (American Lung Association).
14. Mononucleosis

Mononucleosis, often called “mono” or the “kissing disease,” is a viral infection most commonly caused by the Epstein-Barr virus (EBV). One of its hallmark symptoms is a profound and lingering fatigue that can last for weeks or even months, long after the initial fever and sore throat have resolved. This viral fatigue is different from ordinary tiredness, leaving individuals feeling drained regardless of sleep and rest. Other symptoms include swollen lymph nodes, enlarged spleen, and body aches (CDC).
Unlike the flu, which tends to cause intense symptoms that resolve within a few days to a week, mononucleosis leads to a more gradual onset of fatigue and malaise. While both illnesses can feature fever and body aches, mono’s fatigue is typically more persistent and debilitating. In addition, the sore throat in mono is often severe and accompanied by notably swollen tonsils and lymph nodes.
If you experience ongoing fatigue, sore throat, and swollen glands—especially if these symptoms persist longer than two weeks—it may be time to seek medical evaluation. A monospot test or other blood tests can confirm the diagnosis and help guide supportive care (Mayo Clinic).
15. Addison’s Disease
Addison’s disease is a rare but serious disorder where the adrenal glands fail to produce sufficient levels of crucial hormones, primarily cortisol and aldosterone. These hormones are vital for regulating metabolism, blood pressure, and the body’s response to stress. When hormone levels are chronically low, individuals experience a unique kind of fatigue that is far more intense and persistent than general tiredness. This exhaustion does not improve with rest and may worsen throughout the day, often accompanied by muscle weakness, weight loss, low blood pressure, and darkening of the skin (NIDDK).
Unlike ordinary fatigue, which typically resolves with sleep or lifestyle adjustments, the fatigue of Addison’s disease can be profound and disabling. Patients may also develop salt cravings, nausea, abdominal pain, and dizziness upon standing. Because these symptoms overlap with many other conditions, Addison’s disease can be difficult to diagnose in its early stages and is sometimes mistaken for chronic stress or depression.
If you have persistent, unexplained fatigue—especially when combined with unexplained weight loss, low blood pressure, or skin changes—prompt hormone testing is essential. Blood tests measuring cortisol and ACTH levels can help diagnose Addison’s disease and guide lifesaving treatment (Endocrine Society).
16. Lyme Disease

Lyme disease is an infectious illness caused by the bacterium Borrelia burgdorferi, transmitted through the bite of infected black-legged ticks. One of the most persistent symptoms, even after initial treatment, is post-infectious fatigue—an overwhelming sense of tiredness that can linger for weeks or months. This fatigue is often accompanied by joint pain, headaches, and sometimes cognitive difficulties, collectively known as “Lyme brain” (CDC).
Consider the case of a hiker who develops a circular rash and flu-like symptoms a few days after removing a tick. Although the initial fever resolves with antibiotics, the individual continues to feel exhausted and struggles with concentration and memory. This lingering fatigue distinguishes Lyme from typical viral illnesses and may signal ongoing immune activity or inflammation, even when the infection itself is no longer active.
If you have a history of possible tick exposure—especially in wooded or grassy areas—and develop persistent fatigue, joint pain, or a characteristic bull’s-eye rash, prompt medical evaluation is crucial. Early Lyme disease testing and treatment can prevent complications and reduce the risk of chronic symptoms (Mayo Clinic).
17. Lupus
Lupus, or systemic lupus erythematosus (SLE), is an autoimmune disease in which the immune system mistakenly attacks healthy tissues throughout the body. One of the most common and disabling symptoms is profound, immune-related fatigue that can persist even when other symptoms are mild or absent. Lupus fatigue is often described as “bone-deep” exhaustion, making it difficult for patients to get through daily activities regardless of how much they rest (Lupus Foundation of America).
Unlike the tiredness experienced with allergies, which is usually triggered by exposure to specific allergens and often accompanied by classic symptoms like sneezing and itching, lupus fatigue is more generalized and persistent. It may fluctuate with disease activity, often worsening during flares that can also bring joint pain, rashes (such as the signature butterfly rash), fever, and sensitivity to sunlight. The chronic inflammation associated with lupus is thought to be a major contributor to this unrelenting tiredness.
If you have ongoing fatigue along with joint pain, rashes, or unexplained fevers, it’s important to consult your healthcare provider. Blood tests for lupus markers, such as antinuclear antibodies (ANA), can help confirm a diagnosis and guide treatment (CDC).
18. Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain and persistent, debilitating fatigue. Unlike arthritis, which involves inflammation and damage to the joints, fibromyalgia does not cause visible swelling or joint destruction. Instead, the pain in fibromyalgia is thought to originate from abnormal processing of pain signals within the nervous system, leading to heightened sensitivity and discomfort throughout the body (CDC).
The fatigue experienced by those with fibromyalgia is often described as “fibro fog”—a deep, unrelenting tiredness that goes beyond normal exhaustion and frequently coexists with sleep disturbances, memory issues, and difficulty concentrating. This fatigue is not relieved by rest and can make daily activities, work, and social engagement challenging. Unlike arthritis, which is typically limited to affected joints, fibromyalgia symptoms are more diffuse and can affect muscles, tendons, and soft tissues across the body.
Because fibromyalgia can impact multiple aspects of health, a multi-disciplinary approach is often recommended. This might include medical management, physical therapy, psychological support, and lifestyle modifications. If you experience persistent, unexplained pain and fatigue, consulting a rheumatologist or pain specialist can help guide diagnosis and tailor an effective treatment plan (Mayo Clinic).
19. Vitamin D Deficiency

Vitamin D plays a crucial role in maintaining bone health, immune function, and energy levels. When vitamin D levels are low, individuals may experience persistent fatigue, muscle weakness, and general malaise. This deficiency can subtly sap energy and has been linked to mood changes and increased susceptibility to infections. Vitamin D is synthesized in the skin through exposure to sunlight, so deficiency is especially common in regions with long, dark winters or in people with limited sun exposure (NIH Office of Dietary Supplements).
A common seasonal example is the increased fatigue and “winter blues” that some people experience during colder months, when sunlight is scarce. This phenomenon, known as seasonal affective disorder (SAD), may be partly due to decreased vitamin D synthesis. Other risk factors for deficiency include darker skin pigmentation, older age, obesity, and certain chronic illnesses that affect nutrient absorption.
If you have ongoing tiredness, muscle aches, or are at risk due to lifestyle or geography, it’s a good idea to request a blood test for vitamin D levels from your healthcare provider. Early detection and appropriate supplementation can restore energy and support overall health (Mayo Clinic).
20. Heart Arrhythmias
Heart arrhythmias are disorders characterized by abnormal heart rhythms—either beating too fast, too slow, or irregularly. These disruptions interfere with the heart’s ability to pump blood efficiently, resulting in reduced oxygen delivery to vital organs and tissues. As a consequence, people with arrhythmias often experience unexplained fatigue, lightheadedness, or even episodes of fainting. The fatigue may be sudden or persistent, depending on the frequency and severity of the abnormal rhythm (CDC).
Unlike the occasional palpitations (the sensation of a racing or pounding heart) that many people experience during stress, caffeine intake, or exercise, arrhythmia-related fatigue is typically accompanied by other symptoms such as dizziness, shortness of breath, or chest discomfort. In some cases, arrhythmias may be “silent,” with fatigue being the only noticeable sign. Certain arrhythmias, like atrial fibrillation, can increase the risk of stroke and other serious complications if left untreated.
If you notice persistent fatigue along with palpitations, irregular heartbeat, or fainting episodes, it’s important to seek medical evaluation. An electrocardiogram (ECG or EKG) is a simple, non-invasive test that can detect abnormal heart rhythms and guide further management (American Heart Association).
21. Chronic Stress

Chronic stress occurs when the body’s stress response is activated over a prolonged period, causing the continuous release of stress hormones such as cortisol and adrenaline. While these hormones are beneficial in acute situations—helping us react quickly to danger—persistent exposure wears down the body’s systems, leading to exhaustion, weakened immunity, and increased risk of chronic illness. This state of ongoing arousal can drain energy reserves, resulting in persistent fatigue that rest alone does not relieve (American Psychological Association).
The difference between acute and chronic stress is significant. Acute stress is a short-lived reaction to immediate threats or challenges and typically resolves once the situation passes. In contrast, chronic stress stems from ongoing pressures such as work demands, financial difficulties, or caregiving responsibilities. Over time, chronic stress can disrupt sleep, appetite, memory, and mood, further compounding feelings of tiredness and overwhelm.
Warning signs of chronic stress include constant fatigue, irritability, headaches, digestive problems, and trouble concentrating. If you notice these symptoms persisting despite attempts at relaxation, it may be time to seek professional help or adopt structured stress management techniques (National Institute of Mental Health).
22. Celiac Disease

Celiac disease is an autoimmune disorder in which ingestion of gluten—a protein found in wheat, barley, and rye—triggers an immune response that damages the lining of the small intestine. This immune attack leads to poor absorption of nutrients and releases inflammatory chemicals, both of which can cause profound and persistent fatigue. Unlike simple food intolerance, which may only cause digestive discomfort, celiac disease can result in systemic symptoms such as anemia, joint pain, headaches, and skin rashes, in addition to chronic tiredness (National Institutes of Health).
Fatigue related to celiac disease often remains even after adequate rest and is a direct result of both chronic inflammation and nutritional deficiencies, particularly iron, folate, and vitamin B12. While food intolerance may lead to temporary bloating or discomfort, celiac disease can produce lasting symptoms that impact daily functioning and overall well-being. Children and adults alike may experience irritability, difficulty concentrating, or delayed growth (in children).
If you have unexplained fatigue, digestive issues, or other persistent symptoms after eating gluten-containing foods, it’s important to speak with your healthcare provider. Blood tests for celiac-specific antibodies, such as tTG-IgA, can help confirm a diagnosis and guide dietary treatment (Mayo Clinic).
23. Inflammatory Bowel Disease (IBD)

Inflammatory Bowel Disease (IBD), which includes Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the digestive tract. This ongoing immune response not only causes symptoms like abdominal pain, diarrhea, and weight loss but also leads to persistent fatigue. The fatigue in IBD is driven by a combination of factors: nutrient malabsorption, blood loss from the intestines, medication effects, and the body’s constant battle against inflammation. Many people with IBD report exhaustion that does not improve with rest and can significantly impact quality of life (Crohn’s & Colitis Foundation).
It is important to distinguish IBD from Irritable Bowel Syndrome (IBS). While IBS can cause abdominal discomfort and changes in bowel habits, it does not involve chronic inflammation or increase the risk of intestinal damage or nutritional deficiencies. Fatigue in IBS is usually less severe and more closely tied to symptoms like bloating and cramping, whereas IBD-related fatigue often persists independently of digestive flare-ups.
If you experience ongoing tiredness, blood in your stool, unintentional weight loss, or frequent digestive issues, you should consult a gastroenterologist. Specialized testing and endoscopy can help diagnose IBD and guide effective management (Mayo Clinic).
24. Heart Attack Recovery

Recovery from a heart attack (myocardial infarction) often involves persistent fatigue that can last for weeks or even months after the initial event. This lingering tiredness results from both the physical stress of heart tissue damage and the emotional impact of experiencing a major cardiac event. The heart must work harder to compensate for areas with reduced function, and medications prescribed during recovery—such as beta-blockers—can also contribute to feelings of exhaustion (CDC).
While both heart attack and stroke recovery can feature significant fatigue, the underlying causes may differ. Stroke recovery fatigue is often compounded by neurological deficits, cognitive impairment, and the brain’s healing process, whereas heart attack fatigue is more closely related to limited cardiac output and physical deconditioning. Both conditions, however, require patience, gradual increases in activity, and attention to emotional well-being.
Cardiac rehabilitation, which involves supervised exercise, education, and psychological support, is vital for regaining strength and energy after a heart attack. If fatigue persists or worsens during recovery, it’s important to communicate with your healthcare team. Early intervention can address underlying issues and optimize recovery (American Heart Association).
25. Obstructive Sleep Disorders

Obstructive sleep disorders encompass a range of conditions beyond just sleep apnea that can significantly impair the quality of rest and lead to chronic fatigue. These disorders interfere with normal breathing or movement during sleep, disrupting the restorative cycles needed for daytime alertness and energy. Restless leg syndrome (RLS), for example, is a neurological condition characterized by uncomfortable sensations and an urge to move the legs, most often at night. This can lead to frequent awakenings and unrefreshing sleep, much like obstructive sleep apnea (Sleep Foundation).
Other disorders in this category include upper airway resistance syndrome and periodic limb movement disorder, both of which can fragment sleep without the classic snoring or breathing pauses seen in apnea. The resulting fatigue is often misattributed to stress, aging, or lifestyle factors, delaying proper diagnosis and treatment.
If you experience persistent tiredness, difficulty staying asleep, or unusual sensations in your limbs at night, it’s important to consider a referral to a sleep clinic. Sleep specialists can conduct overnight studies to identify specific disorders and recommend targeted treatments, such as CPAP therapy, medications, or behavioral interventions (Mayo Clinic).
26. Medication Side Effects

Many commonly used medications can cause fatigue as a side effect, either by directly affecting the central nervous system or by altering the body’s normal physiological processes. Antihistamines, used to treat allergies, are well-known for causing drowsiness and lethargy, particularly first-generation types such as diphenhydramine. Beta-blockers, frequently prescribed for high blood pressure or heart conditions, can slow the heart rate and lower blood pressure, sometimes resulting in persistent tiredness or a lack of energy (FDA).
There is often a difference in the fatigue-inducing potential of prescribed versus over-the-counter medications. Prescription drugs like certain antidepressants, muscle relaxants, or anti-seizure agents may have significant sedative effects, while even widely available over-the-counter remedies—such as cold medicines or sleep aids—can cause notable drowsiness or grogginess. Sometimes, multiple medications taken together can have an additive effect, making fatigue worse.
If you experience new or worsening fatigue after starting a medication, it is important to review your current drug list with a healthcare provider or pharmacist. Adjusting dosages, changing medications, or altering the timing of doses can often alleviate fatigue without sacrificing treatment effectiveness (Mayo Clinic).
27. Menopause

Menopause marks the end of a woman’s reproductive years and is characterized by a natural decline in estrogen and progesterone levels. These hormonal changes can lead to a range of symptoms, with new-onset fatigue being one of the most common complaints. Unlike the cyclical tiredness associated with premenstrual syndrome (PMS), which typically resolves with the start of menstruation, menopausal fatigue can be more persistent and is often accompanied by hot flashes, night sweats, sleep disturbances, and mood changes (U.S. Department of Health & Human Services).
While PMS fatigue is usually predictable and short-lived, menopausal tiredness may fluctuate with hormone levels and can feel overwhelming, especially when compounded by sleep disruption from night sweats or insomnia. Additionally, menopause may bring muscle aches, cognitive changes (“brain fog”), and increased sensitivity to stress, all of which can intensify feelings of exhaustion.
If you are experiencing persistent fatigue along with other menopausal symptoms, it’s important to discuss them with your healthcare provider. They can help identify contributing factors, rule out other medical conditions, and recommend strategies such as lifestyle modifications, hormone therapy, or non-hormonal treatments to improve energy and quality of life (Mayo Clinic).
28. Chronic Infection (e.g., Hepatitis C, HIV)
Chronic viral infections, such as hepatitis C and HIV, can cause persistent and sometimes debilitating fatigue. These viruses remain in the body for years, triggering ongoing immune activation and low-level inflammation that depletes energy reserves and disrupts normal metabolism. Fatigue from chronic infection often develops gradually and can be one of the earliest symptoms, even before more recognizable signs like jaundice (in hepatitis C) or weight loss (in HIV) appear (CDC: Hepatitis C).
For instance, a person with untreated HIV may notice a gradual loss of stamina, increased need for rest, and trouble completing daily activities. This fatigue is due not only to the direct effects of the virus but also to the body’s constant effort to fight infection. As HIV progresses, fatigue can intensify and may be compounded by anemia, sleep disturbances, medication side effects, or other infections.
Because the symptoms of chronic infection are often vague or attributed to other causes, many individuals remain undiagnosed for years. If you experience ongoing, unexplained fatigue—especially if you have risk factors for hepatitis C or HIV—timely testing is crucial. Early diagnosis allows for effective treatment that can reduce fatigue and improve long-term outcomes (HIV.gov: HIV Testing).
29. Dehydration

Dehydration occurs when the body loses more fluids than it takes in, disrupting the balance necessary for normal physiological function. Even mild dehydration can significantly impair energy levels, as fluids are critical for maintaining blood volume, regulating body temperature, and ensuring that nutrients and oxygen are efficiently transported to cells. As dehydration progresses, symptoms such as fatigue, dizziness, headache, dry mouth, and decreased urine output become more pronounced (CDC: Hydration).
It is important to differentiate dehydration from overhydration, a less common but potentially serious condition in which excessive water intake dilutes the body’s electrolytes, especially sodium. While dehydration leads to concentrated urine and thirst, overhydration often presents with symptoms like nausea, confusion, and swollen hands or feet. Both extremes can impact energy and well-being, but dehydration is far more likely to cause persistent tiredness in everyday life.
Warning signs of dehydration include dark yellow urine, infrequent urination, dry skin, rapid heartbeat, and persistent fatigue. If you notice these symptoms, increasing fluid intake—preferably water—can help restore balance. Severe dehydration, especially if accompanied by confusion or rapid heartbeat, warrants prompt medical attention (Mayo Clinic).
30. Poor Nutrition

Poor nutrition can have a profound impact on energy levels, as the body depends on a steady supply of calories and essential nutrients to fuel every cellular process. When nutrition is lacking—whether due to insufficient calorie intake, vitamin and mineral deficiencies, or unbalanced macronutrient consumption—fatigue often follows. This can happen with restrictive fad diets, eating disorders, or chronic illnesses that affect nutrient absorption. Symptoms of poor nutrition-related fatigue may also include hair loss, brittle nails, pale skin, and frequent illness (CDC: Why It Matters).
Fad diets that severely limit certain food groups or calories can lead to quick weight loss but often result in low energy, irritability, and long-term nutrient deficiencies. In contrast, balanced eating—focused on a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats—supports sustained energy, stable mood, and overall health. Nutritional fatigue is often gradual and may be overlooked until it begins to interfere with daily activities or exercise tolerance.
If you experience persistent tiredness, consider asking your healthcare provider for a nutritional screening, which might include blood tests for anemia, vitamin D, B12, iron, and other key nutrients. Early detection and dietary adjustments can restore vitality and prevent more serious complications (Harvard T.H. Chan School of Public Health: Healthy Eating Plate).
31. Post-COVID Syndrome (Long COVID)
Post-COVID syndrome, commonly known as Long COVID, refers to lingering symptoms that persist for weeks or months after the initial COVID-19 infection has resolved. Among the most frequently reported and debilitating symptoms is persistent fatigue—often described as overwhelming and unrelenting, regardless of rest. This fatigue can occur even after mild or asymptomatic cases of COVID-19 and may be accompanied by brain fog, muscle aches, shortness of breath, and sleep disturbances (CDC: Post-COVID Conditions).
Long COVID shares similarities with other post-viral syndromes, such as those occurring after mononucleosis or influenza, where the body’s immune and nervous systems remain in a heightened state long after the infection subsides. However, the scale and duration of fatigue in Long COVID have made it a significant public health concern, impacting people of all ages and activity levels. Unlike typical recovery from viral illnesses, the fatigue associated with Long COVID can be severe enough to interfere with work, school, and daily life.
If you continue to experience significant fatigue or other symptoms more than four weeks after recovering from COVID-19, it’s important to seek specialty care. Post-COVID clinics and multidisciplinary teams can offer targeted evaluation and rehabilitation (Yale Medicine: Long COVID).
32. Congestive Heart Failure
Congestive heart failure (CHF) is a chronic condition where the heart’s ability to pump blood effectively is compromised, resulting in poor circulation and a buildup of fluid in the lungs and tissues. This weak heart pump means that less oxygen and nutrients reach the body’s organs and muscles, leading to persistent fatigue and reduced exercise tolerance. Fluid accumulation can cause swelling in the legs, ankles, and abdomen, as well as shortness of breath, especially when lying down (CDC: Heart Failure).
Unlike hypertension (high blood pressure), which is often silent until complications arise, CHF produces noticeable symptoms that worsen over time. While both conditions affect the cardiovascular system, hypertension usually does not cause fatigue directly unless it has led to heart failure or organ damage. In CHF, everyday activities like walking or climbing stairs may become exhausting, and individuals may awaken at night gasping for air.
Warning signs that should prompt immediate medical attention include sudden weight gain, severe shortness of breath, swelling, or rapid heartbeat. If you have risk factors for heart disease or notice these symptoms, consult your healthcare provider promptly for evaluation and management (American Heart Association: Heart Failure Symptoms).
33. Sleep Deprivation

Sleep deprivation is a leading cause of fatigue and can have immediate and long-term effects on physical and mental health. Insufficient sleep disrupts the body’s natural repair processes, impairs cognitive function, weakens the immune system, and increases the risk of chronic diseases. Acute sleep deprivation—such as pulling an all-nighter—can result in noticeable sluggishness, poor concentration, and irritability the next day. Chronic sleep deprivation, however, accumulates over time and can lead to persistent exhaustion, mood disturbances, memory problems, and even increased risk of accidents (CDC: Sleep and Sleep Disorders).
The difference between acute and chronic lack of sleep is significant. While a single night of poor sleep can be “recovered” with rest, ongoing insufficient sleep creates a sleep debt that is harder to resolve and may have lasting consequences on overall well-being. People often underestimate the impact of missing just an hour or two of recommended sleep each night.
Improving sleep hygiene can help prevent and address sleep deprivation. Tips include maintaining a consistent bedtime routine, avoiding screens and caffeine before bed, keeping the bedroom cool and dark, and prioritizing 7-9 hours of sleep each night. Persistent sleep issues may require professional evaluation (Sleep Foundation: Sleep Hygiene).
34. Chronic Pain

Chronic pain is defined as pain that lasts for weeks, months, or even years, and it can have a profound impact on daily energy levels. The constant strain of living with pain disrupts sleep, increases stress hormone production, and saps both physical and emotional resources. As a result, people with chronic pain often experience persistent fatigue, difficulty concentrating, and reduced motivation for daily tasks. This stands in contrast to acute pain, such as that from a recent injury or surgery, which typically resolves as the underlying issue heals and is less likely to cause long-term exhaustion (CDC: Chronic Pain).
Acute pain is usually sharp, short-lived, and serves as a protective signal that prompts us to rest and recover. Chronic pain, on the other hand, can become a disease in itself, involving ongoing nerve signaling and psychological effects that perpetuate tiredness and distress. The constant need to adapt to pain can also lead to social withdrawal and depression, further compounding fatigue.
If you experience pain that persists for more than three months and notice it impacting your energy, mood, or daily functioning, seeking help from a pain management specialist can be beneficial. A comprehensive approach may include medication, therapy, physical rehabilitation, and lifestyle adjustments (Mayo Clinic: Chronic Pain).
35. Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting people of reproductive age, characterized by irregular menstrual cycles, elevated androgen levels, and multiple cysts on the ovaries. The hormonal imbalances in PCOS—especially insulin resistance and disruptions in estrogen, progesterone, and testosterone—can lead to persistent fatigue. This tiredness is often compounded by weight gain, mood changes, and sleep disturbances such as sleep apnea, which are more prevalent in women with PCOS (CDC: PCOS).
Unlike endometriosis, which primarily causes chronic pelvic pain and heavy menstrual bleeding due to tissue similar to the uterine lining growing outside the uterus, PCOS-related fatigue is more closely linked to metabolic and endocrine dysfunction. While both conditions can cause irregular periods and infertility, their underlying mechanisms and primary symptoms differ. Fatigue in PCOS may also be exacerbated by mood disorders, such as depression or anxiety, which are more common in those with the syndrome.
Signs that should prompt referral to a gynecologist include persistent fatigue alongside irregular periods, unwanted hair growth, acne, weight changes, or difficulty conceiving. Early diagnosis and management can improve symptoms, reduce complications, and enhance overall well-being (Women’s Health.gov: PCOS).
36. Vitamin B12 Deficiency

Vitamin B12 is an essential nutrient that plays a vital role in red blood cell production, neurological function, and energy metabolism. When B12 levels are low, the body is unable to efficiently make healthy red blood cells or support proper nerve function, resulting in symptoms like persistent fatigue, weakness, numbness, and even cognitive changes. Individuals following a vegan or strict vegetarian diet are at higher risk, as vitamin B12 is naturally found almost exclusively in animal products such as meat, dairy, and eggs (NIH Office of Dietary Supplements).
For example, someone who adopts a vegan diet without adequate supplementation may gradually become more tired, pale, or experience tingling in their hands and feet. Over time, untreated B12 deficiency can lead to anemia and irreversible neurological damage. Other risk groups include older adults, people with digestive disorders affecting absorption (like Crohn’s or celiac disease), and those who have undergone gastric surgery.
If you notice ongoing tiredness, unexplained neurological symptoms, or follow a diet low in animal products, it’s wise to ask your healthcare provider about checking your B12 levels. Early detection through a simple blood test and appropriate supplementation can quickly restore energy and prevent complications (Mayo Clinic).
37. Sleep-Related Movement Disorders

Sleep-related movement disorders are conditions that disrupt sleep due to involuntary movements, significantly contributing to daytime fatigue. Two of the most common are restless leg syndrome (RLS) and periodic limb movement disorder (PLMD). RLS is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations that worsen at night or during periods of inactivity. PLMD, on the other hand, involves repetitive, involuntary jerking or twitching of the limbs during sleep, which can fragment the sleep cycle (Sleep Foundation).
Unlike insomnia, where the primary issue is difficulty falling or staying asleep due to racing thoughts or anxiety, sleep-related movement disorders disrupt rest due to physical sensations or movements. Individuals may not remember these nighttime movements but often wake feeling unrefreshed, experiencing persistent fatigue, mood changes, or trouble concentrating during the day.
If you have unexplained daytime tiredness, frequent nighttime awakenings, or bed partners who observe unusual limb movements, it’s important to consult a sleep specialist. Diagnosis often involves a detailed sleep history and may require an overnight sleep study (polysomnography) to capture and evaluate movement patterns (Mayo Clinic: RLS).
38. Hypopituitarism
Hypopituitarism is a rare condition in which the pituitary gland fails to produce adequate amounts of one or more of its essential hormones. The pituitary, often called the “master gland,” controls the function of other endocrine glands such as the thyroid, adrenals, and reproductive organs. Deficiencies in pituitary hormones can lead to a range of symptoms, with persistent fatigue being one of the most prominent. Depending on which hormones are lacking, individuals may also experience weight changes, low blood pressure, amenorrhea, infertility, or decreased libido (Mayo Clinic).
While thyroid disorders like hypothyroidism cause fatigue due to low levels of thyroid hormones, hypopituitarism can disrupt multiple hormonal pathways at once. The resulting fatigue is often more severe and may be accompanied by other signs such as weakness, poor stress tolerance, or dizziness. Unlike isolated thyroid disease, the symptoms of hypopituitarism are broader and may involve several organ systems.
If you experience unexplained fatigue along with other hormonal symptoms—especially after head trauma, brain surgery, or radiation—it’s important to request pituitary function tests. Blood tests measuring pituitary and target gland hormones can guide diagnosis and treatment, restoring energy and hormonal balance (Hormone Health Network).
39. Myasthenia Gravis
Myasthenia gravis is a chronic autoimmune disorder in which the immune system mistakenly attacks the communication between nerves and muscles, resulting in muscle weakness and rapid fatigue. The antibodies produced in this condition block or destroy acetylcholine receptors at the neuromuscular junction, making it difficult for nerves to stimulate muscle contraction. Symptoms often fluctuate, worsening with activity and improving with rest, and can affect any voluntary muscle group (National Institute of Neurological Disorders and Stroke).
A classic early sign of myasthenia gravis is ptosis, or drooping of one or both eyelids, particularly toward the end of the day or after prolonged use of the eyes. Other common symptoms include double vision, difficulty swallowing, slurred speech, and weakness in the arms or legs. Unlike general fatigue, the muscle weakness in myasthenia gravis is specific, often affecting the same muscle groups repeatedly and worsening with repeated use.
If you experience unexplained, fluctuating muscle weakness—especially with symptoms like droopy eyelids, double vision, or trouble swallowing—it’s important to consult a neurologist. Early diagnosis with specialized testing can help manage symptoms and prevent complications (Mayo Clinic).
40. Alcohol or Substance Use

Alcohol and substance use can significantly disrupt sleep patterns and deplete energy, resulting in persistent fatigue. Alcohol, although initially sedating, interferes with the deep, restorative phases of sleep and increases the likelihood of frequent nighttime awakenings. Over time, regular alcohol consumption can lead to insomnia, reduced sleep quality, and chronic tiredness the next day. Similarly, recreational drugs and certain prescription medications, such as stimulants or sedatives, can alter normal sleep architecture and leave individuals feeling physically and mentally drained (CDC: Alcohol Use).
Stimulants (such as cocaine or amphetamines) may temporarily boost alertness, but often result in a “crash” of exhaustion as their effects wear off. These substances can also contribute to anxiety, restlessness, and insomnia, further compounding the cycle of fatigue. In contrast, chronic alcohol use tends to cause more persistent sluggishness, mood swings, and memory problems. The interplay between substance use and fatigue is complex and can be further complicated by underlying mental health or medical conditions.
If you are struggling with ongoing fatigue and use alcohol or substances, it’s essential to have a candid conversation with your healthcare provider. Honest disclosure enables targeted support and treatment recommendations, which may include counseling, rehabilitation, or medication-assisted therapy (SAMHSA National Helpline).
41. Obesity
Obesity, defined as having a body mass index (BMI) of 30 or higher, can significantly contribute to persistent fatigue and low energy. Excess weight places additional strain on the heart, muscles, joints, and respiratory system, making physical activity more taxing and recovery slower. Obesity is also associated with chronic inflammation, insulin resistance, and an increased risk of conditions like sleep apnea, all of which can further sap energy and disrupt restorative sleep (CDC: Adult Obesity Causes & Consequences).
Fatigue in obesity is often compounded by difficulty breathing during activity, joint pain, and reduced physical endurance. In contrast, individuals who are underweight may experience tiredness due to insufficient calorie intake, nutrient deficiencies, or underlying health problems. Both extremes can lead to decreased stamina and a lower quality of life, but the mechanisms differ: obesity-related fatigue is often mechanical and metabolic, while underweight fatigue is more likely related to energy supply and nutritional status.
If you notice ongoing fatigue, shortness of breath, or new limitations in daily activities due to your weight, it’s important to seek help from a healthcare provider. They can assess for related conditions and offer a multidisciplinary approach—including nutrition counseling, exercise guidance, and medical management (National Heart, Lung, and Blood Institute: Aim for a Healthy Weight).
42. Chronic Allergies

Chronic allergies, also known as perennial allergic rhinitis, occur when the body is continuously exposed to allergens such as dust mites, pet dander, or mold. Unlike seasonal allergies, which typically arise during certain times of the year due to pollen or specific plants, chronic allergies persist year-round. The immune system’s ongoing response leads to the release of histamines and other inflammatory chemicals, causing symptoms like nasal congestion, sneezing, itchy eyes, and—most notably—persistent fatigue. The constant battle against allergens can drain energy reserves, disrupt sleep, and make concentration difficult (American Academy of Allergy, Asthma & Immunology).
While seasonal allergies may cause short bursts of tiredness and discomfort, chronic allergies often result in long-term exhaustion, especially when sleep is disturbed by congestion or coughing. This ongoing fatigue can impact productivity, mood, and overall quality of life. Children and adults with chronic allergies may also be more prone to sinus infections, headaches, and irritability.
If you experience persistent fatigue along with allergy symptoms that do not improve with over-the-counter treatments, it may be time to consider allergy testing. Identifying and addressing specific triggers—either through medication, environmental controls, or immunotherapy—can greatly improve energy and daily functioning (Mayo Clinic).
43. Hyperthyroidism
Hyperthyroidism is a condition where the thyroid gland produces excessive amounts of thyroid hormones, accelerating the body’s metabolism. While hypothyroidism causes sluggishness and persistent tiredness due to a slow metabolism, hyperthyroidism can also result in significant fatigue—but for different reasons. The overactive metabolism leads to restlessness, difficulty sleeping, muscle weakness, and the rapid consumption of energy reserves. Despite feeling “wired,” individuals often experience profound exhaustion, especially after physical activity (Endocrine Society).
A common example is someone who notices a rapid or irregular heartbeat, excessive sweating, weight loss despite a normal or increased appetite, and feelings of anxiety or irritability. This constant state of metabolic overdrive can prevent restful sleep and quickly wear down the body, leaving people drained even though they may appear energetic or agitated on the surface. Muscle weakness, especially in the upper arms and thighs, is also common and can make everyday tasks more tiring.
If you notice persistent fatigue along with symptoms such as palpitations, tremors, unexplained weight loss, or heat intolerance, it’s important to seek thyroid function testing. Early diagnosis and treatment can restore hormonal balance and improve energy levels (Mayo Clinic).
44. Major Sleep Disorders (Narcolepsy, Insomnia)

Major sleep disorders such as narcolepsy and chronic insomnia are rare but can cause profound, life-altering fatigue. Narcolepsy is a neurological disorder that disrupts the regulation of sleep and wake cycles, leading to sudden episodes of overwhelming daytime sleepiness, “sleep attacks,” and sometimes cataplexy—sudden muscle weakness triggered by emotions. People with narcolepsy may fall asleep without warning during daily activities, regardless of how much sleep they’ve had at night. This differs from insomnia, which is characterized by difficulty falling or staying asleep, frequent nighttime awakenings, and unrefreshing rest. Insomnia leads to chronic tiredness, trouble concentrating, irritability, and increased risk for other health problems (Sleep Foundation: Narcolepsy, Sleep Foundation: Insomnia).
While both disorders result in persistent fatigue, the underlying causes and patterns are distinct. Narcolepsy’s symptoms can be more unpredictable and severe, often impacting safety and functioning, while insomnia’s effects are tied to the inability to achieve restful sleep at night. Both conditions can be mistaken for stress or depression, delaying appropriate treatment.
If you experience sudden sleep episodes, persistent unrefreshing sleep, or severe daytime drowsiness despite good sleep habits, consult a sleep medicine specialist. Accurate diagnosis and targeted therapies can greatly improve quality of life.
45. Chronic Sinusitis
Chronic sinusitis is a condition marked by inflammation and infection of the sinus cavities lasting for 12 weeks or longer, despite treatment attempts. This ongoing inflammation leads to symptoms such as nasal congestion, facial pain or pressure, postnasal drip, and a reduced sense of smell. One of the most overlooked but common consequences is persistent fatigue, as the body continuously fights infection and inflammation. The ongoing discomfort and difficulty breathing can also disrupt sleep, compounding the feeling of tiredness (CDC: Chronic Sinusitis).
Chronic sinusitis differs from acute sinusitis, which usually develops suddenly after a cold or respiratory infection and resolves within a few weeks. While acute sinusitis may cause temporary tiredness, the fatigue in chronic sinusitis is more prolonged and often interferes with work, social activities, and overall quality of life. Recurrent or persistent infections can also contribute to brain fog and irritability.
If you suffer from ongoing sinus symptoms and unexplained fatigue lasting several weeks or more, a referral to an ear, nose, and throat (ENT) specialist is recommended. ENT evaluation may include imaging, nasal endoscopy, or allergy testing to guide effective treatment and relieve both sinus and fatigue symptoms (ENT Health).
46. Medication Withdrawal

Medication withdrawal occurs when a person stops taking a drug that their body has become accustomed to, and fatigue is a frequent and often underestimated symptom of this process. Common culprits include antidepressants, corticosteroids, benzodiazepines, and some pain medications. When these drugs are discontinued—especially abruptly—the brain and body must readjust to the absence of substances that influenced neurotransmitters or hormone levels, resulting in tiredness, mood changes, sleep disturbances, and sometimes flu-like symptoms (FDA: Drug Withdrawal).
The fatigue from sudden withdrawal tends to be more intense and disruptive compared to symptoms that arise when medications are tapered gradually under medical supervision. For instance, stopping antidepressants “cold turkey” can lead to withdrawal syndrome, featuring exhaustion, dizziness, irritability, and headaches. Gradual dose reduction allows the body to adapt more comfortably, minimizing the severity of fatigue and other withdrawal effects.
If you are considering stopping or changing a regular medication and are concerned about fatigue or other withdrawal symptoms, always consult your healthcare provider first. Medical guidance ensures a safer, individualized tapering plan and helps manage side effects, supporting a smoother transition (Mayo Clinic: Antidepressant Withdrawal).
47. Chronic Inflammatory Response Syndrome (CIRS)
Chronic Inflammatory Response Syndrome (CIRS) is a complex, multi-system illness triggered by ongoing exposure to environmental toxins such as mold, water-damaged buildings, or certain bacteria. These triggers provoke an abnormal and persistent inflammatory response in genetically susceptible individuals, leading to a wide range of symptoms—most notably, profound fatigue that does not resolve with rest. Other common complaints include brain fog, muscle aches, headaches, sinus issues, and gastrointestinal disturbances (NCBI: CIRS and Mycotoxins).
Mold exposure is one of the best-known environmental causes of CIRS. People living or working in damp, water-damaged environments may inhale or absorb mold toxins, which can overwhelm the immune system and trigger chronic inflammation. Unlike simple allergies, the fatigue and cognitive issues in CIRS often persist long after leaving the contaminated space and may worsen over time if not properly addressed.
If you experience unrelenting fatigue, cognitive changes, or other unexplained symptoms—especially after known or suspected mold exposure—it is important to seek evaluation from a healthcare provider familiar with CIRS. Referral to a specialist, such as an environmental medicine or integrative physician, can help guide advanced testing and targeted therapy (Surviving Mold: Diagnosis Steps).
48. Post-Concussion Syndrome

Post-concussion syndrome (PCS) refers to a set of symptoms that persist for weeks or months after a mild traumatic brain injury, such as a concussion. One of the most common and debilitating symptoms is lingering fatigue, which can affect both physical and mental functioning. This tiredness may be accompanied by headaches, dizziness, memory problems, difficulty concentrating, irritability, and sleep disturbances. Unlike the acute recovery phase, where symptoms usually resolve in days, PCS-related fatigue can persist long after the initial injury (CDC: Concussion).
PCS is distinct from whiplash, though both can result from similar mechanisms, such as car accidents or sports injuries. Whiplash primarily affects the neck and soft tissues, leading to pain and stiffness but rarely causing the cognitive or emotional symptoms typical of PCS. In PCS, the brain’s ability to process information and maintain alertness is disrupted, leading to a deep and persistent sense of exhaustion that is not relieved by rest alone.
If you experience ongoing fatigue, confusion, mood changes, or concentration difficulties for more than two weeks after a head injury, it is important to seek a neurologic evaluation. Early assessment and rehabilitation can improve recovery and help manage persistent symptoms (Mayo Clinic: Post-Concussion Syndrome).
49. Chronic Viral Infections (EBV, CMV)
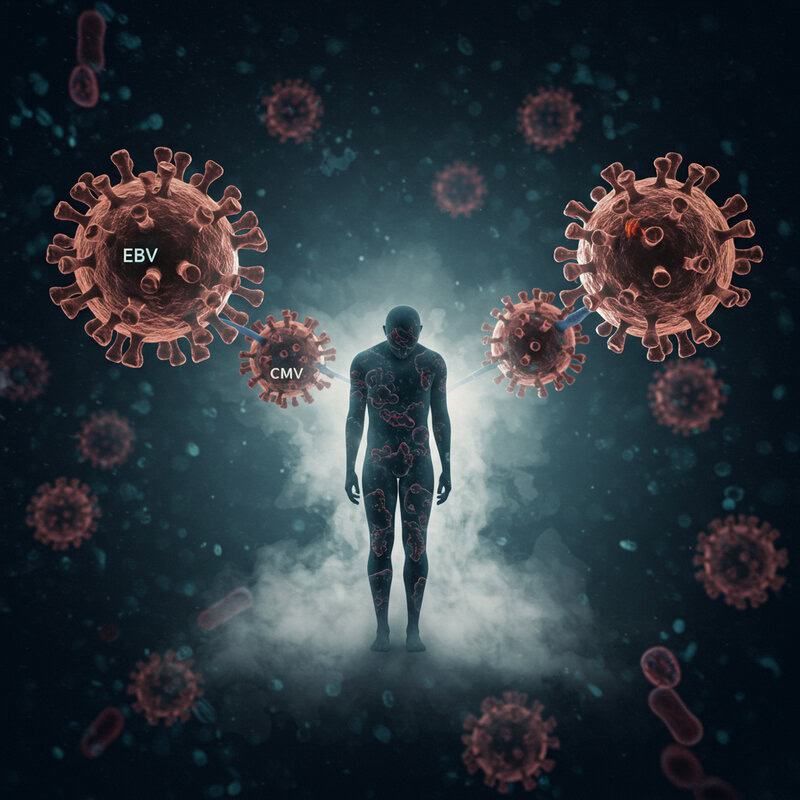
Chronic viral infections such as Epstein-Barr virus (EBV) and cytomegalovirus (CMV) are known for causing prolonged fatigue that can persist long after the initial illness has resolved. EBV, the virus responsible for mononucleosis (“mono”), and CMV, another common herpesvirus, both remain dormant in the body and can reactivate under certain conditions. This can result in low-grade inflammation, immune activation, and a deep, lingering tiredness that may last for months or even years (CDC: Epstein-Barr Virus, CDC: Cytomegalovirus).
Unlike acute viral infections, which typically cause intense but short-lived symptoms such as fever, sore throat, or body aches, chronic EBV and CMV infections manifest primarily as persistent fatigue, cognitive difficulties (“brain fog”), and sometimes mild muscle or joint pain. This form of fatigue is often resistant to rest and can significantly disrupt daily life, making it challenging to work, study, or maintain social activities.
If you have ongoing, unexplained tiredness—especially if it began after a viral illness or is accompanied by swollen lymph nodes or low-grade fevers—consider discussing viral testing with your healthcare provider. Blood tests can help identify chronic or reactivated infection and guide supportive care (Mayo Clinic: EBV).
50. Malignancy-Related Paraneoplastic Syndromes
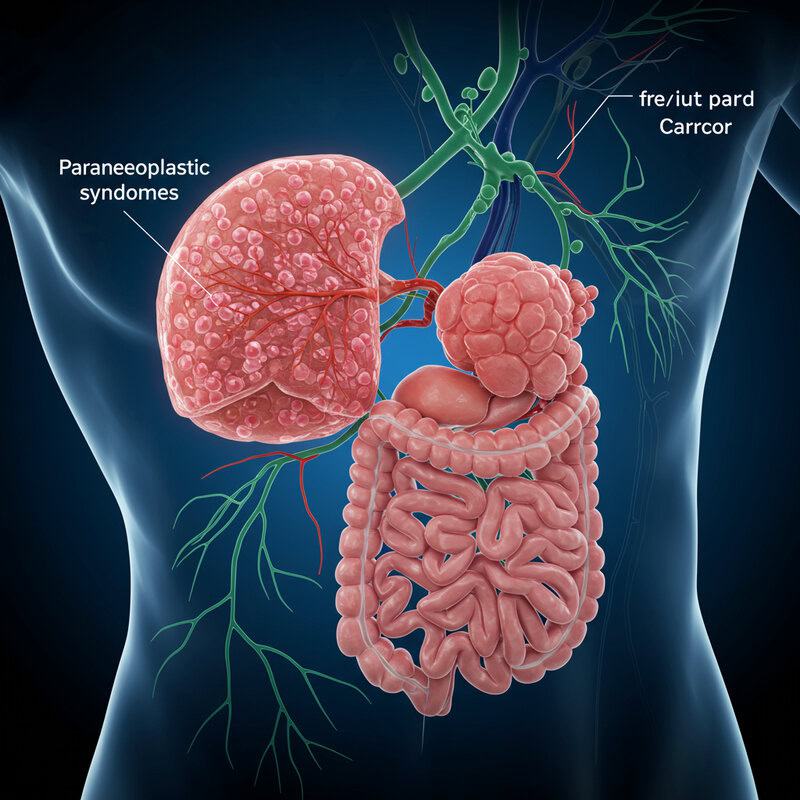
Paraneoplastic syndromes are rare disorders that occur when cancer triggers an immune response or releases substances affecting tissues far from the tumor site. One significant manifestation is profound, unexplained fatigue that may precede or accompany other cancer symptoms. These syndromes can affect the nervous system, endocrine glands, or muscles, and are most commonly associated with cancers like small-cell lung cancer, ovarian cancer, or lymphomas (American Cancer Society: Paraneoplastic Syndromes).
For example, small-cell lung cancer can cause a paraneoplastic neurologic syndrome, resulting in muscle weakness, difficulty walking, and deep fatigue, sometimes even before the cancer is diagnosed. Other paraneoplastic syndromes may cause hormonal imbalances, weight loss, or changes in mental status. These symptoms are not caused by the direct growth of the tumor, but by immune or chemical effects elsewhere in the body.
Red flags for urgent evaluation include rapid, unexplained weight loss, persistent fatigue despite rest, neurological changes (such as confusion or weakness), and new-onset symptoms in someone with a known cancer risk. If you experience these signs, prompt medical assessment is crucial for diagnosis and early cancer treatment (Mayo Clinic: Paraneoplastic Syndromes).
Conclusion

Persistent fatigue is more than just tiredness—it can be an early warning sign of a wide range of underlying health conditions. Recognizing when fatigue lingers, worsens, or is accompanied by other symptoms is crucial for early diagnosis and effective treatment. Timely evaluation by a healthcare provider can help uncover root causes, from hormonal imbalances to chronic infections or more serious illnesses. If you or someone you know continues to experience unexplained fatigue, consider seeking medical advice or appropriate screening tests (CDC: Chronic Disease and Aging). Taking fatigue seriously can lead to better outcomes and improved quality of life.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





