Psoriasis: Proven Treatments & Why Early Care Matters
Psoriasis affects over 125 million people worldwide, impacting approximately 2-3% of the global population (World Health Organization). This chronic, immune-mediated condition triggers rapid skin cell growth, leading to red, scaly patches and inflammation. Beyond its visible effects, psoriasis can deeply influence quality of life. Unfortunately, many cases remain undiagnosed or diagnosed late, delaying effective care and increasing the risk of complications (National Psoriasis Foundation).
1. Understanding Psoriasis
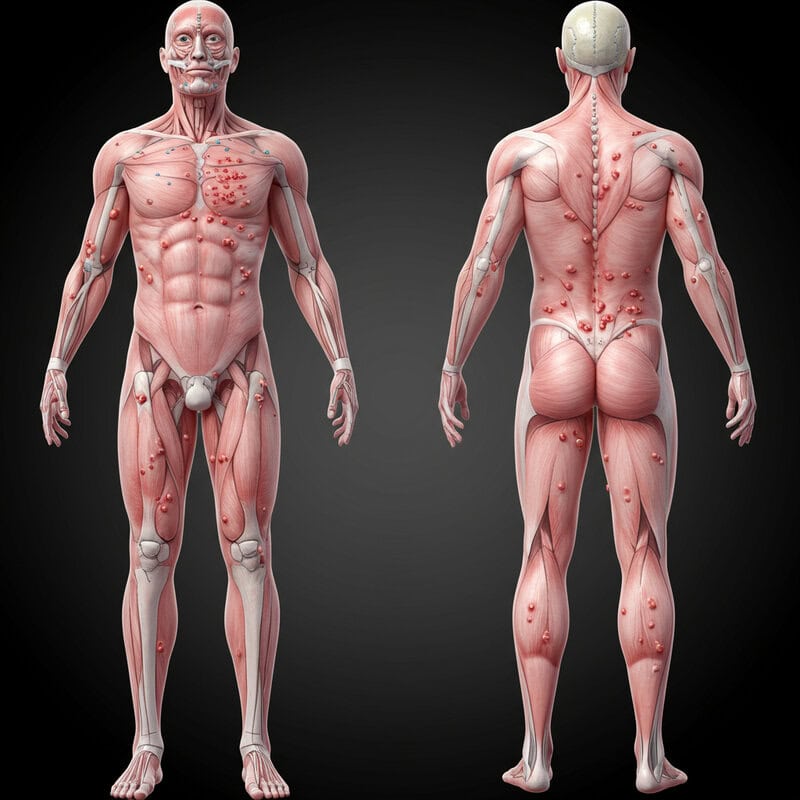
Psoriasis is a chronic, non-contagious skin disorder characterized by the rapid buildup of skin cells, resulting in thick, red, scaly patches that can cause discomfort and itching. The underlying cause is an overactive immune system, specifically involving T-cells that mistakenly attack healthy skin cells, triggering inflammation and accelerated cell turnover (American Academy of Dermatology). This immune dysfunction leads to the hallmark lesions that appear most commonly on the scalp, elbows, knees, and lower back, but can affect any area of the body.
Psoriasis is often confused with other dermatological conditions such as eczema, fungal infections, or dermatitis because of its similar symptoms—redness, flaking, and irritation. However, psoriasis has distinct characteristics like sharply defined plaques and silvery scales. Misidentification can lead to inappropriate treatments and unnecessary discomfort, emphasizing the importance of proper diagnosis (Mayo Clinic). Recognizing the unique immune system involvement in psoriasis is critical for choosing the right therapeutic approach and preventing potential complications. Due to these complexities, consulting a dermatologist is recommended for anyone experiencing persistent or unusual skin symptoms.
2. Early Signs and Symptoms

The earliest signs of psoriasis often appear as small, red, scaly patches on the skin, which may be mistaken for a rash or irritation. These lesions can develop anywhere but frequently emerge on the elbows, knees, or scalp. Some people may notice dry, cracked skin that can bleed, persistent itching, or a burning sensation (NHS). In certain cases, tiny pits or discoloration on the fingernails and toenails can be early indicators of nail psoriasis.
Psoriasis is frequently misdiagnosed, especially in its initial stages, as conditions like eczema, seborrheic dermatitis, or even fungal infections. For example, scalp psoriasis can look similar to dandruff, while guttate psoriasis in children may be mistaken for an allergic rash (Healthline). Delayed or incorrect identification can lead to inappropriate treatments and a worsening of symptoms. Prompt recognition is crucial, as early intervention may help prevent the spread and severity of the condition, improve quality of life, and reduce the risk of developing associated health issues, such as psoriatic arthritis or cardiovascular complications.
3. Triggers and Risk Factors
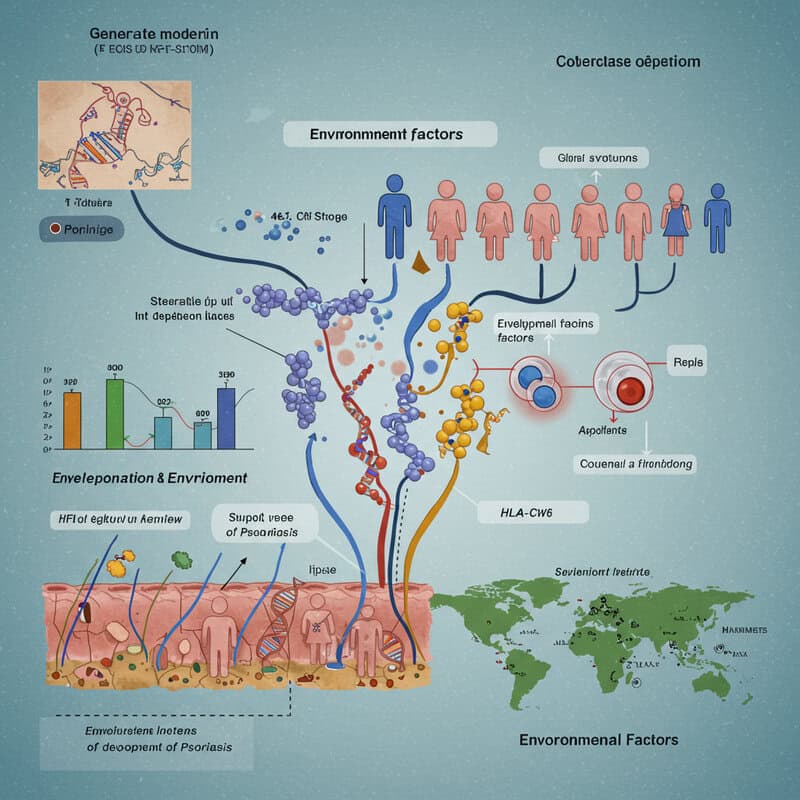
Psoriasis develops through a complex interaction between genetic predisposition and environmental triggers. A strong family history is one of the most significant risk factors—individuals with a parent or sibling affected by psoriasis have a higher likelihood of developing the condition themselves (NIAMS). Researchers have identified specific genes, such as HLA-Cw6, that are linked to increased risk, highlighting the inherited component of the disease.
Environmental factors can also spark or exacerbate psoriasis flare-ups. Common triggers include infections (especially streptococcal throat infections), skin injuries (cuts, scrapes, or sunburn), and certain medications like beta-blockers or lithium (National Psoriasis Foundation). Stress is a well-documented trigger, with emotional or physical stress often preceding flare-ups. Lifestyle choices such as smoking and excessive alcohol consumption can further worsen symptoms and increase disease severity. Additionally, environmental factors like cold, dry weather may aggravate skin irritation, while obesity is associated with increased risk and severity of psoriasis.
Understanding these triggers and risk factors is essential for effectively managing the disease and developing personalized treatment plans. Identifying and minimizing exposure to known triggers can help reduce flare-ups and improve long-term outcomes.
4. Plaque Psoriasis: The Most Common Type

Plaque psoriasis, also known as psoriasis vulgaris, is the most prevalent form of the disease, affecting about 80-90% of people diagnosed with psoriasis (National Psoriasis Foundation). It is characterized by raised, inflamed patches of skin covered with silvery-white scales. These plaques are often well-defined and can appear anywhere on the body, but they most commonly develop on the elbows, knees, lower back, and scalp. The plaques can be itchy, sore, and may crack or bleed, contributing to considerable discomfort and self-consciousness.
In contrast, less common types of psoriasis include guttate, inverse, pustular, and erythrodermic psoriasis. Guttate psoriasis presents as small, drop-shaped lesions and often follows a bacterial infection. Inverse psoriasis causes smooth, red patches in skin folds such as the armpits or groin. Pustular psoriasis is marked by pus-filled blisters, while erythrodermic psoriasis is a rare but severe form that leads to widespread redness and peeling of the skin (Mayo Clinic). Recognizing plaque psoriasis and distinguishing it from these less common types is crucial for determining the most effective treatment approach and managing symptoms appropriately.
5. Guttate Psoriasis
Guttate psoriasis is a distinct form of psoriasis that commonly develops in children and young adults. It is characterized by small, drop-shaped lesions distributed across the trunk, limbs, and sometimes the scalp (American Academy of Dermatology). Unlike the thick, scaly plaques seen in plaque psoriasis, guttate lesions are typically finer and less raised, but can still cause itching and discomfort.
This type of psoriasis is strongly associated with bacterial infections, especially those caused by streptococcus, such as strep throat. In fact, guttate psoriasis often appears suddenly two to three weeks after a bout of strep throat or an upper respiratory infection (National Psoriasis Foundation). The immune response to the infection appears to inadvertently trigger the rapid skin cell growth seen in psoriasis. While genetics play a role, the infectious trigger is a distinguishing feature of guttate psoriasis.
Guttate psoriasis sometimes resolves on its own, particularly when the underlying infection is treated, but it may also progress to chronic plaque psoriasis in some individuals. Prompt medical attention and treatment of infections can help manage symptoms and prevent potential complications.
6. Inverse Psoriasis

Inverse psoriasis, also known as flexural psoriasis, manifests as smooth, red, and inflamed patches that primarily affect skin folds and areas where skin touches skin. Common sites include the armpits, under the breasts, groin, inner thighs, and around the genitals and buttocks (National Psoriasis Foundation). Unlike other types, inverse psoriasis does not typically present with the thick, scaly plaques characteristic of plaque psoriasis. Instead, the lesions appear shiny and lack scaling due to the moist environment of skin folds.
The unique challenge of inverse psoriasis lies in the constant moisture and friction within these areas, which can aggravate symptoms and make the skin more sensitive. Sweat and rubbing from skin-to-skin contact can worsen irritation, lead to increased redness, and even cause the skin to crack or become sore (Healthline). These conditions also make the affected areas more susceptible to secondary infections, such as yeast or fungal overgrowths, which can further complicate management.
Because of its location and appearance, inverse psoriasis is sometimes misdiagnosed as fungal or bacterial infections. Accurate diagnosis and tailored treatments are essential for controlling symptoms and maintaining skin integrity in these sensitive areas.
7. Pustular Psoriasis

Pustular psoriasis is a rare and severe form of psoriasis marked by the appearance of white, pus-filled blisters (pustules) surrounded by red, inflamed skin. Unlike infections, these pustules are sterile and not caused by bacteria. Pustular psoriasis can be localized—commonly affecting the hands and feet (palmoplantar pustulosis)—or generalized, spreading rapidly over large areas of the body (National Psoriasis Foundation).
The symptoms can develop suddenly and include intense redness, tenderness, and swelling in the affected areas. In cases of generalized pustular psoriasis, patients may also experience fever, chills, fatigue, rapid pulse, and muscle weakness. The aggressive nature of this form can lead to serious complications, such as dehydration, infection, and disturbances in blood chemistry (Mayo Clinic).
Because pustular psoriasis can escalate quickly and affect overall health, it requires urgent medical attention. Hospitalization may be necessary for severe outbreaks to stabilize symptoms and prevent life-threatening complications. Prompt, specialized care ensures effective management and can be lifesaving, especially during acute flares.
8. Erythrodermic Psoriasis
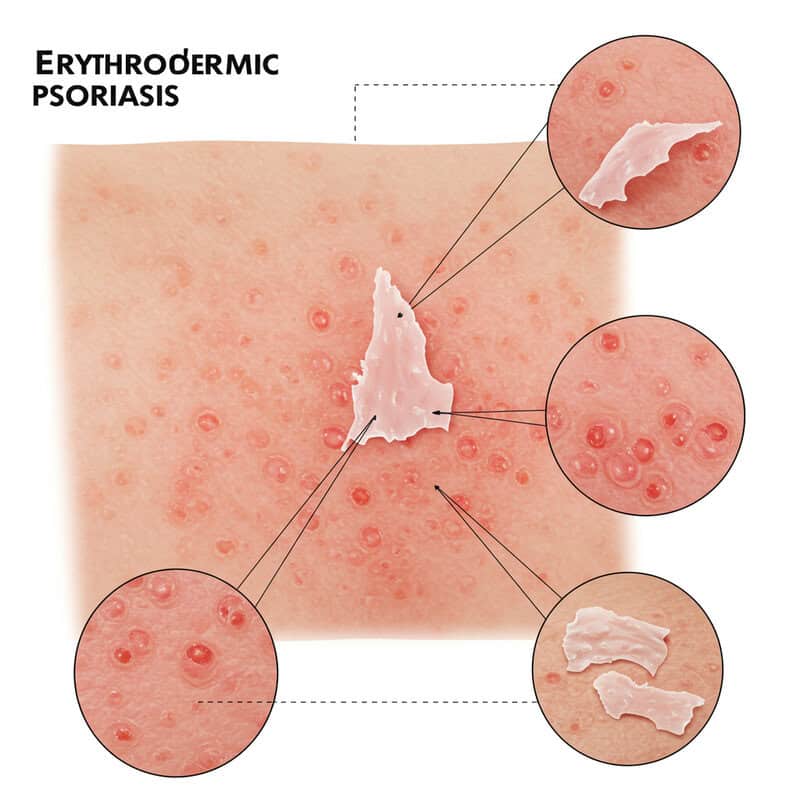
Erythrodermic psoriasis is an extremely rare and severe form of psoriasis that affects nearly the entire surface of the skin. It is characterized by widespread, fiery redness, intense itching, and shedding of skin in large sheets (National Psoriasis Foundation). Unlike localized plaque or guttate forms, erythrodermic psoriasis disrupts the skin’s barrier function, making it difficult for the body to regulate temperature and retain essential fluids.
This condition often develops suddenly, sometimes in people with unstable plaque psoriasis, after abruptly stopping systemic treatments or due to severe sunburn or infection. Symptoms can include severe pain, rapid heart rate, chills, and swelling from fluid retention. Because the skin is the body’s largest organ and serves as a crucial protective barrier, its extensive involvement can quickly lead to life-threatening complications such as dehydration, electrolyte imbalances, heart failure, and increased risk of infections (American Academy of Dermatology).
Erythrodermic psoriasis is a medical emergency. Immediate hospitalization is often necessary to stabilize the patient, manage symptoms, and prevent complications. Early recognition and intervention are vital to preserving health and preventing potentially fatal outcomes.
9. Nail Psoriasis

Nail psoriasis is a common manifestation of psoriasis, affecting up to 50% of people with the condition and as many as 80% of those with psoriatic arthritis (National Psoriasis Foundation). It occurs when the underlying inflammation of psoriasis targets the fingernails and toenails, leading to a range of visible changes. Symptoms may include pitting (small dents), discoloration (yellow-brown spots), thickening, crumbling, and separation of the nail from the nail bed (onycholysis).
Nail psoriasis is often mistaken for fungal infections due to overlapping features such as yellowing, brittleness, and debris under the nail (Healthline). Misdiagnosis can result in improper treatment and prolonged discomfort. Unlike fungal infections, nail psoriasis is an autoimmune condition and requires different therapies, such as topical steroids, systemic medications, or biologics.
These nail changes can significantly impact daily life, making tasks like typing, buttoning clothes, or even walking painful or difficult. The visible nature of nail psoriasis may also lead to embarrassment or social withdrawal. Early recognition and targeted treatment are crucial for improving function, appearance, and quality of life.
10. Scalp Psoriasis

Scalp psoriasis is a common form of psoriasis that affects the hair-bearing regions of the scalp, sometimes extending to the forehead, neck, and behind the ears. It appears as red, scaly patches that can be thick and crusted, often accompanied by intense itching and flaking (American Academy of Dermatology). The flakes produced by scalp psoriasis may closely resemble dandruff, making it difficult to distinguish between the two. However, scalp psoriasis tends to cause more pronounced redness, thicker scales, and sometimes even hair loss due to excessive scratching or inflammation.
Proper hair and scalp care is vital for managing symptoms and minimizing discomfort. Using medicated shampoos containing ingredients like coal tar, salicylic acid, or ketoconazole can help reduce scaling and inflammation (National Psoriasis Foundation). It is important to avoid overly vigorous scratching or picking at scales, as this can worsen irritation and potentially cause infection. Gentle brushing to loosen scales, maintaining a regular hair-washing routine, and using moisturizers or oils can provide relief. For severe cases, dermatologists may recommend topical corticosteroids or other prescription treatments to effectively control flare-ups.
11. Psoriatic Arthritis

Psoriatic arthritis is an inflammatory type of arthritis that affects up to 30% of people with psoriasis (National Psoriasis Foundation). This condition occurs when the immune system not only targets the skin but also attacks the joints and connective tissues, leading to pain, swelling, and stiffness. The fingers, toes, knees, ankles, and spine are commonly involved, and the disease can affect one or multiple joints.
Early warning signs include joint pain, morning stiffness lasting more than 30 minutes, swelling of entire fingers or toes (dactylitis), and changes to the nails such as pitting or separation from the nail bed. Fatigue and reduced range of motion are also frequent complaints (Mayo Clinic). In some cases, joint symptoms may develop before or at the same time as skin lesions, making early diagnosis challenging.
Ignoring joint pain can lead to permanent joint damage and disability. Prompt medical attention and specialized treatment, such as disease-modifying antirheumatic drugs (DMARDs) or biologics, are essential for preserving joint function, reducing inflammation, and improving long-term outcomes.
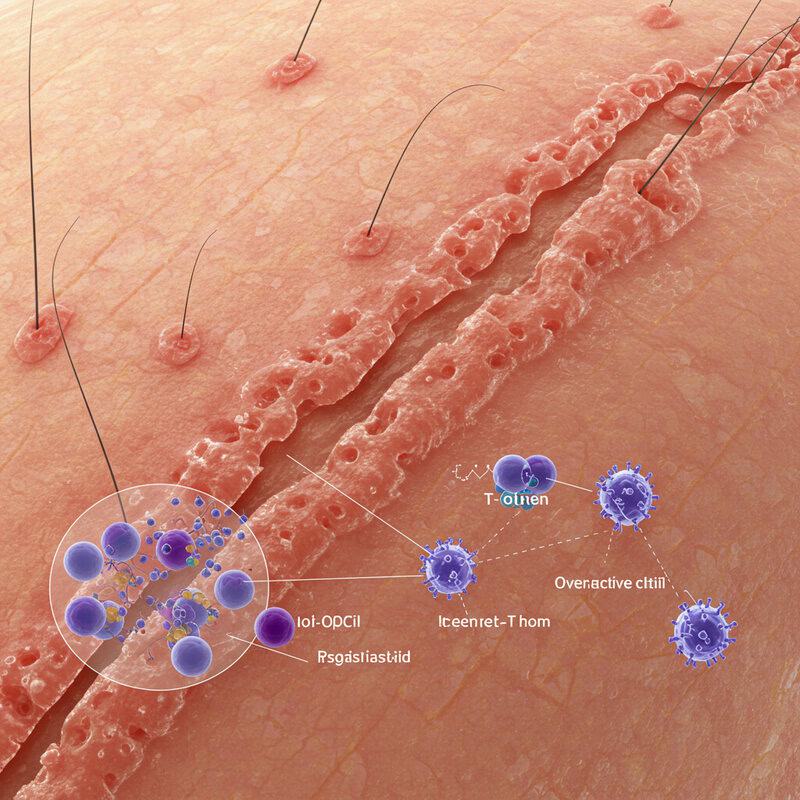
12. The Role of the Immune System
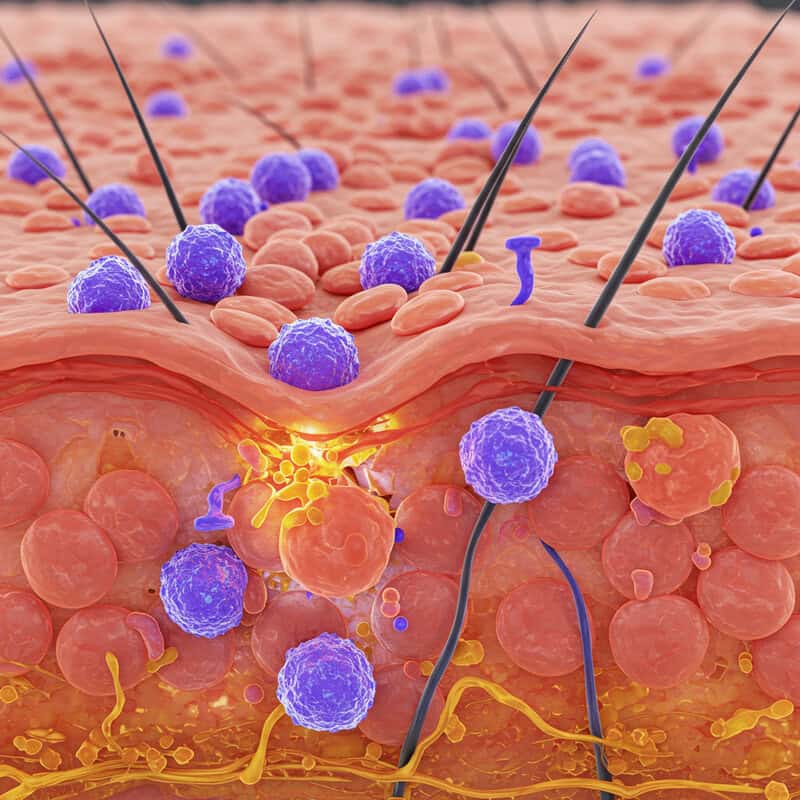
Psoriasis is fundamentally an immune-mediated condition, meaning it arises from a malfunction in the immune system. In healthy individuals, the immune system protects against infections and repairs damaged tissue. However, in people with psoriasis, immune cells—particularly T-cells—become overactive and mistakenly attack healthy skin cells. This triggers a cascade of inflammation, causing the rapid production and accumulation of new skin cells, which leads to the formation of the characteristic red, scaly plaques (NIAMS).
The immune dysfunction observed in psoriasis shares similarities with other autoimmune diseases, such as rheumatoid arthritis, lupus, and inflammatory bowel disease. In all these conditions, the body’s immune system loses the ability to distinguish between its own tissues and foreign invaders, resulting in chronic inflammation and tissue damage (National Psoriasis Foundation). These parallels help explain why some individuals with psoriasis also develop related conditions like psoriatic arthritis or have a higher risk for other autoimmune disorders.
Understanding the central role of immune dysregulation in psoriasis has paved the way for targeted therapies—such as biologics—that specifically address these immune pathways, offering more effective and personalized treatment options.
13. The Impact of Stress
Stress is a well-recognized trigger for both the onset and exacerbation of psoriasis symptoms. The body’s response to stress involves the release of hormones such as cortisol, which can disrupt immune function and amplify inflammation—key drivers of psoriasis flare-ups (National Psoriasis Foundation). Many individuals report that periods of emotional or physical stress coincide with worsening symptoms, making stress management a crucial component of disease control.
Chronic stress not only aggravates psoriasis but can also impact mental health, increasing the risk of anxiety and depression. This creates a cycle where stress worsens psoriasis, and the visible symptoms of psoriasis contribute to further stress (NIH).
Real-world stress management strategies include practicing mindfulness techniques such as meditation or deep-breathing exercises, engaging regularly in physical activity, and ensuring adequate sleep. Setting aside time for hobbies, connecting with supportive friends or family, and, if needed, seeking professional counseling can also help. Participation in support groups—either in person or online—can provide community and reduce feelings of isolation. Consistent self-care and stress reduction can make a meaningful difference in managing psoriasis symptoms.
14. The Importance of Moisturization
Daily moisturization is a cornerstone of psoriasis management, helping to reduce dryness, flaking, and itching while supporting the skin’s natural barrier. Psoriatic skin loses moisture more quickly than healthy skin, making it prone to cracking and irritation. Applying moisturizers regularly can soothe symptoms, enhance comfort, and improve the effectiveness of other topical treatments (National Psoriasis Foundation).
There are various types of moisturizers to consider. Ointments (such as petroleum jelly) provide the heaviest barrier, locking in moisture and offering significant relief for very dry or thickened plaques. Creams are lighter than ointments but still substantial, making them a good choice for daily use. Lotions, being the lightest, are easy to apply but may require more frequent reapplication and are best for mild dryness or use in warm climates (Healthline).
Consistency is key—moisturizers should be applied at least once or twice daily, ideally after bathing or hand washing to lock in moisture. Regular use not only eases discomfort but also helps prevent flare-ups, maintain skin health, and enhance the overall effectiveness of psoriasis treatment regimens.
15. Topical Steroids

Topical steroids are the most commonly prescribed medications for controlling mild to moderate psoriasis. These anti-inflammatory creams or ointments work by suppressing the overactive immune response in the skin, reducing redness, swelling, itching, and scaling (American Academy of Dermatology). They are available in a range of strengths, from mild (hydrocortisone) to very potent (clobetasol propionate, betamethasone dipropionate), and can be tailored to the severity and location of symptoms.
Commonly used topical steroid brands include Cortizone-10 (hydrocortisone), Temovate (clobetasol), and Diprolene (betamethasone). These medications are often applied once or twice daily directly to affected areas. High-potency steroids are typically reserved for thick plaques on the elbows, knees, or scalp, while milder steroids are used for sensitive areas like the face, groin, or underarms (National Psoriasis Foundation).
Safe usage is essential to avoid side effects such as skin thinning, stretch marks, or systemic absorption. Patients should use the lowest effective strength for the shortest duration possible and follow their healthcare provider’s instructions. Periodic breaks from steroid use and alternating with other treatments can help maintain skin health and effectiveness over time.
16. Vitamin D Analogues
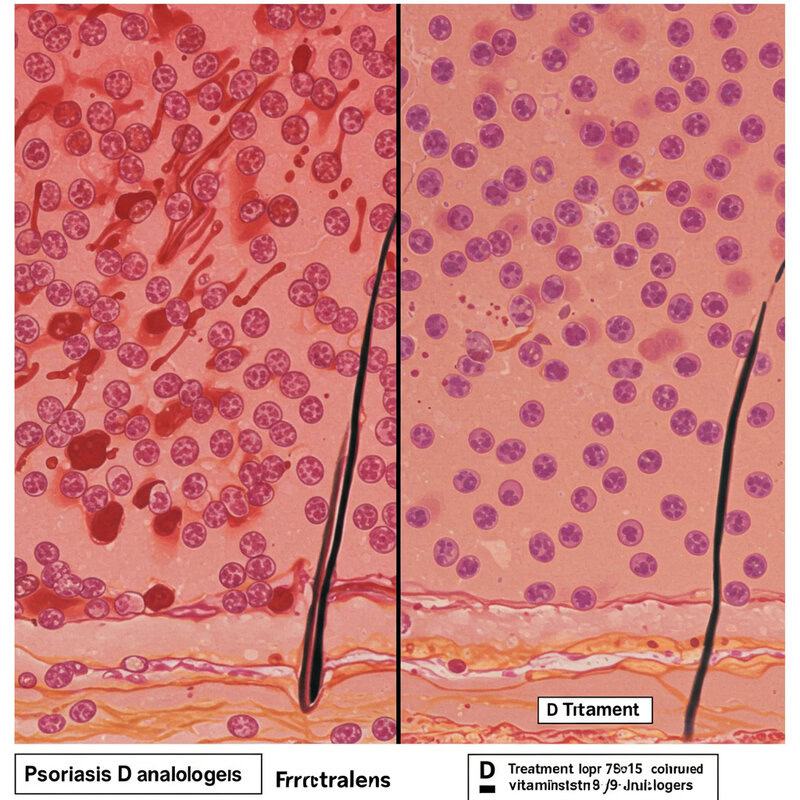
Vitamin D analogues are a class of topical medications widely used in the treatment of mild to moderate psoriasis. These agents, such as calcipotriene (brand name Dovonex) and calcitriol, work by slowing down the rapid growth and turnover of skin cells, which is a hallmark of psoriasis (American Academy of Dermatology). By normalizing cell production, these medications help reduce scaling, thickness, and redness of psoriatic plaques.
Vitamin D analogues are most effective in cases with limited skin involvement and are often prescribed as a first-line therapy for mild to moderate psoriasis. They can be used alone or in combination with topical corticosteroids to enhance their effects and minimize potential side effects (National Psoriasis Foundation). These medications are typically applied once or twice daily to affected areas.
Vitamin D analogues are generally well tolerated, with minimal side effects compared to long-term steroid use. Mild irritation or a burning sensation may occur at the application site, but serious adverse effects are rare. Consistent use, as directed by a healthcare provider, can help control symptoms and maintain clearer skin in mild cases of psoriasis.
17. Topical Calcineurin Inhibitors

Topical calcineurin inhibitors, such as tacrolimus (Protopic) and pimecrolimus (Elidel), are non-steroidal creams used to manage psoriasis in sensitive areas where prolonged steroid use may carry higher risks. These medications work by inhibiting the activity of calcineurin, a protein involved in activating T-cells that drive inflammation in psoriasis (American Academy of Dermatology). By reducing immune overactivity, calcineurin inhibitors help control redness, swelling, and itching without causing skin thinning.
These creams are particularly beneficial for treating psoriasis on the face, around the eyes, in skin folds, and in the genital region—areas prone to adverse effects from long-term topical steroid use. Compared to corticosteroids, calcineurin inhibitors do not cause atrophy (skin thinning), stretch marks, or visible blood vessels, making them safer for delicate skin (National Psoriasis Foundation).
Common side effects include a mild burning or stinging sensation at the application site, usually resolving within the first week of use. While long-term safety is generally favorable, these medications should be used under the guidance of a healthcare professional, especially for extended periods or over large skin areas.
18. Coal Tar Preparations

Coal tar has a long history as a treatment for psoriasis, with its use dating back over a century. Derived from coal, coal tar preparations are available as shampoos, creams, ointments, and bath solutions. Coal tar works by slowing the rapid growth of skin cells, reducing scaling, itching, and inflammation associated with psoriasis (American Academy of Dermatology). It is especially effective for mild to moderate cases, including scalp psoriasis and plaques on the body.
Coal tar is often used in combination with other therapies, such as topical corticosteroids or phototherapy, to enhance its effectiveness. Products like Neutrogena T/Gel and Psoriasin contain varying concentrations of coal tar and are available over-the-counter (National Psoriasis Foundation). While coal tar can help manage symptoms and improve skin appearance, results may be gradual and require consistent use.
Despite its benefits, coal tar has some drawbacks. It can stain clothing and bedding, has a strong odor, and may cause skin irritation or sensitivity to sunlight. Nonetheless, it remains a safe and cost-effective option for many, particularly when used as directed by a healthcare provider.
19. Salicylic Acid

Salicylic acid is a common over-the-counter treatment for psoriasis, particularly valued for its ability to soften and remove the thick, scaly buildup characteristic of the condition. As a keratolytic agent, salicylic acid works by dissolving the bonds between dead skin cells, making it easier to shed excess scales and allowing other topical treatments to penetrate more effectively (American Academy of Dermatology).
Salicylic acid is available in a variety of formulations, including creams, ointments, lotions, and medicated shampoos. It is particularly useful for treating scalp psoriasis, as regular use can help lift scales and reduce flaking (National Psoriasis Foundation). When using salicylic acid products, gentle application is important—rubbing too vigorously or using high concentrations can irritate the skin or even trigger additional flare-ups.
To maximize benefits, apply salicylic acid to wet skin after bathing, and follow up with a moisturizer to combat dryness. Avoid using salicylic acid on large areas or for extended periods, especially in children, as excessive absorption may cause side effects. Always consult a healthcare provider for personalized advice on safe and effective use.
20. Phototherapy (Light Therapy)

Phototherapy, also known as light therapy, is a well-established treatment for moderate to severe psoriasis. The most common type is narrowband ultraviolet B (UVB) phototherapy, which uses a specific wavelength of light to slow the growth of affected skin cells and reduce inflammation (National Psoriasis Foundation). UVB phototherapy is effective in clearing plaques, reducing itching, and improving overall skin appearance.
There are two primary options for phototherapy: in-clinic treatments and at-home phototherapy units. Clinic-based phototherapy is administered under medical supervision, usually two to three times a week, ensuring precise dosing and monitoring (American Academy of Dermatology). At-home units provide greater convenience and flexibility, but require careful instruction and regular follow-up with a dermatologist to ensure safety and effectiveness.
Safety is paramount with phototherapy. Overexposure to UV light can increase the risk of sunburn, premature skin aging, and, with long-term use, skin cancer. Protective measures, such as shielding sensitive areas and wearing eye protection, are essential. Phototherapy is not suitable for everyone, so a thorough evaluation by a healthcare provider is necessary to determine if this treatment is appropriate.
21. Excimer Laser Therapy

Excimer laser therapy is an advanced form of light treatment designed to target small, localized areas of psoriasis. The excimer laser emits a concentrated beam of ultraviolet B (UVB) light at a wavelength of 308 nanometers, which is highly effective at reducing inflammation and slowing the rapid skin cell turnover seen in psoriasis (National Psoriasis Foundation). This precision allows dermatologists to deliver high doses of UVB directly to plaques without affecting the surrounding healthy skin.
Excimer laser therapy is particularly useful for treating stubborn plaques on the elbows, knees, scalp, and other hard-to-treat areas. Sessions are typically brief and may be needed once or twice weekly, with noticeable improvement often seen within a few weeks (American Academy of Dermatology). Compared to traditional whole-body phototherapy, the excimer laser minimizes UV exposure to unaffected skin and can achieve faster results in small, resistant patches.
This therapy is generally well tolerated, though some patients may experience redness or blistering at the treatment site. Excimer laser therapy is not suitable for widespread psoriasis but offers an excellent option for localized, persistent lesions unresponsive to other treatments.
22. Systemic Medications: Methotrexate
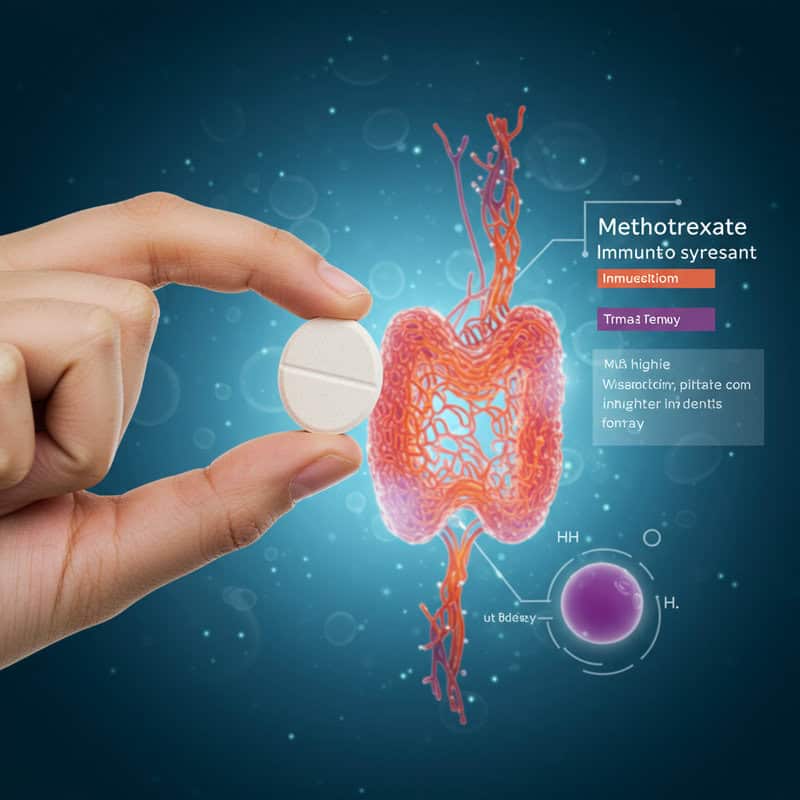
Methotrexate is a well-established systemic medication used to treat moderate to severe psoriasis and psoriatic arthritis. As an immunosuppressant, methotrexate works by inhibiting the activity of specific immune cells and enzymes involved in inflammation and rapid skin cell production (National Psoriasis Foundation). By dampening the overactive immune response, methotrexate helps reduce scaling, redness, swelling, and joint pain associated with psoriasis.
Methotrexate is typically reserved for cases that do not respond to topical treatments or phototherapy, or for those with extensive skin involvement or significant joint symptoms. It is taken orally once a week, or in some cases, administered by injection. Because methotrexate affects the entire immune system, close monitoring is essential to minimize potential side effects (American Academy of Dermatology).
Regular blood tests are required to check liver function, blood cell counts, and kidney health, as methotrexate can cause liver toxicity, bone marrow suppression, and other complications. Folic acid supplementation is often recommended to reduce side effects. Methotrexate is not suitable for everyone, especially pregnant women or those with liver disease, making medical supervision crucial throughout treatment.
23. Systemic Medications: Cyclosporine

Cyclosporine is a potent immunosuppressive medication used to manage severe, treatment-resistant psoriasis, particularly during acute flares or in cases where rapid symptom control is required (National Psoriasis Foundation). It works by inhibiting the activity of specific immune cells (T-cells) responsible for triggering inflammation and the rapid overproduction of skin cells characteristic of psoriasis.
Due to its powerful effects, cyclosporine is generally prescribed for short-term use, typically up to one year, to avoid the risk of long-term side effects. It is administered orally in capsule or liquid form, and dosing is carefully tailored to the patient’s weight and disease severity (American Academy of Dermatology).
One of the most significant risks associated with cyclosporine is kidney toxicity. Regular monitoring of kidney function and blood pressure is essential throughout treatment, as cyclosporine can cause hypertension and potentially irreversible kidney damage. Other possible side effects include increased susceptibility to infections, tremors, and gum overgrowth. Because of these risks, cyclosporine is typically reserved for patients who have not responded to other therapies and is used under strict medical supervision to ensure safety and effectiveness.
24. Systemic Medications: Acitretin
Acitretin is an oral retinoid, a derivative of vitamin A, primarily used to treat severe or resistant forms of psoriasis, such as pustular or erythrodermic psoriasis (National Psoriasis Foundation). Acitretin works by normalizing the growth and differentiation of skin cells, helping to reduce scaling and promote the shedding of thickened plaques. Unlike immunosuppressants, acitretin does not directly suppress the immune system, making it a valuable option for patients who cannot tolerate or are not candidates for other systemic therapies.
Acitretin is often used in combination with phototherapy or other topical treatments to enhance its effectiveness (American Academy of Dermatology). However, it comes with unique precautions. The most notable is its strong teratogenic effect—women of childbearing potential must use effective birth control during treatment and for at least three years after stopping the medication, as acitretin can cause severe birth defects. Other common side effects include dry skin, chapped lips, hair thinning, and elevated blood lipid levels.
Regular monitoring of liver function and cholesterol is required during treatment. Acitretin is generally reserved for adults with severe, unresponsive psoriasis, and its use requires careful discussion of risks and benefits with a healthcare provider.
25. Biologic Therapies: TNF-Alpha Inhibitors
TNF-alpha inhibitors are a class of biologic medications that target and block tumor necrosis factor-alpha (TNF-alpha), a key inflammatory cytokine involved in the overactive immune response seen in psoriasis and psoriatic arthritis (National Psoriasis Foundation). By inhibiting TNF-alpha, these therapies help reduce inflammation, slow down the excessive production of skin cells, and alleviate both skin and joint symptoms.
Common TNF-alpha inhibitors used in moderate-to-severe psoriasis include etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade). These medications are administered by injection or intravenous infusion and are typically prescribed for patients who have not responded to traditional systemic treatments or phototherapy (American Academy of Dermatology).
TNF-alpha inhibitors have revolutionized psoriasis care by providing rapid and sustained symptom relief, as well as improving quality of life. However, because they suppress part of the immune system, they may increase the risk of infections, particularly tuberculosis and other serious infections. Patients require screening and ongoing monitoring while on these therapies. Careful selection and supervision by a healthcare provider are essential for safety and effectiveness.
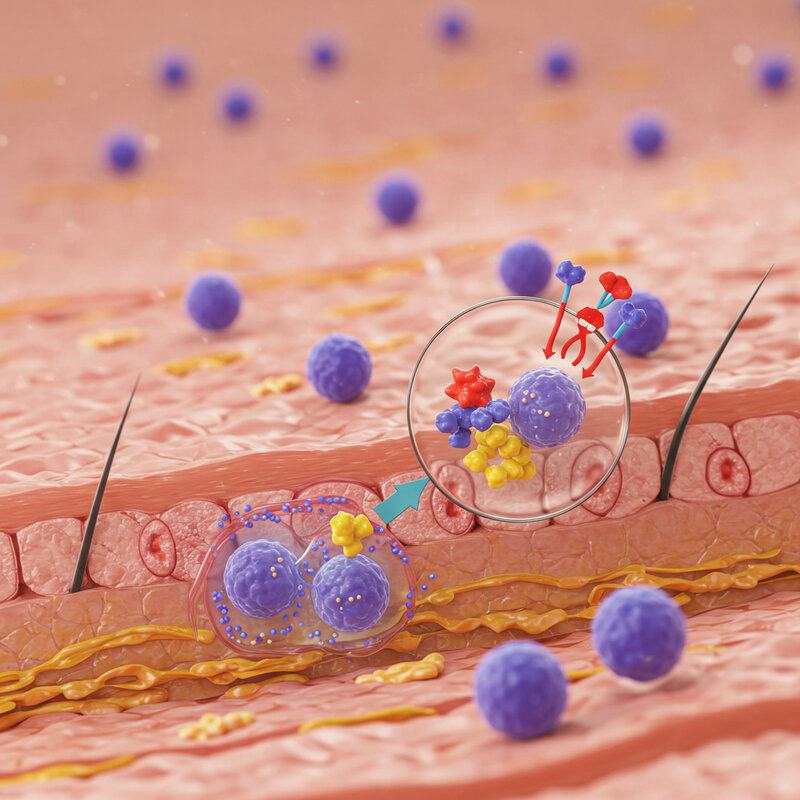
26. Biologic Therapies: IL-17 Inhibitors
IL-17 inhibitors represent a newer generation of biologic treatments designed to target interleukin-17 (IL-17), a cytokine that plays a central role in the inflammatory cascade driving psoriasis. By specifically blocking IL-17, these medications interrupt the immune signals responsible for the rapid growth and accumulation of skin cells, leading to swift improvement in psoriatic symptoms (National Psoriasis Foundation).
Common IL-17 inhibitors include secukinumab (Cosentyx), ixekizumab (Taltz), and brodalumab (Siliq). These drugs are administered via subcutaneous injection and are typically prescribed for individuals with moderate-to-severe plaque psoriasis who have not responded adequately to conventional systemic therapies or other biologics (American Academy of Dermatology).
One of the standout benefits of IL-17 inhibitors is their rapid onset of action—many patients experience significant clearing of skin lesions within weeks of starting treatment. While generally well-tolerated, these medications can increase the risk of certain infections, particularly those affecting the upper respiratory tract. Regular follow-up and monitoring are essential to ensure optimal safety and therapeutic results.
27. Biologic Therapies: IL-23 Inhibitors
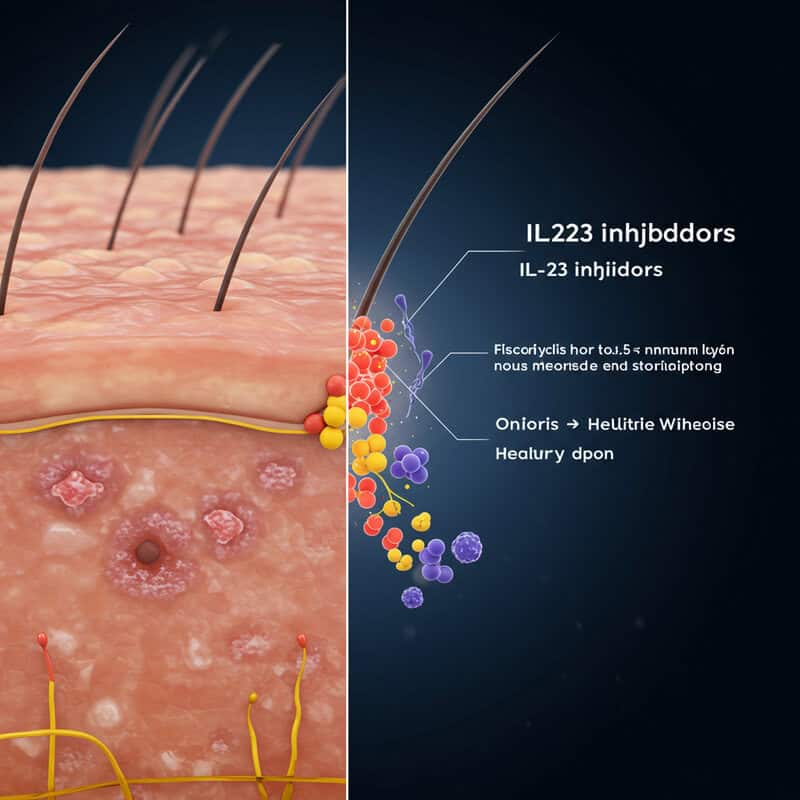
IL-23 inhibitors are a cutting-edge class of biologic drugs that target interleukin-23 (IL-23), a cytokine intimately involved in the chronic inflammation and abnormal skin cell growth characteristic of psoriasis. By selectively blocking IL-23, these medications disrupt a key pathway in the immune response, leading to substantial reductions in plaque formation and symptom severity (National Psoriasis Foundation).
Prominent IL-23 inhibitors include guselkumab (Tremfya), tildrakizumab (Ilumya), and risankizumab (Skyrizi). These agents are administered by subcutaneous injection, usually every 8 to 12 weeks after initial loading doses, making them convenient options for long-term management. IL-23 inhibitors are indicated for adults with moderate-to-severe plaque psoriasis, especially those who have not responded to traditional systemic treatments or other biologics (American Academy of Dermatology).
Clinical studies have demonstrated that IL-23 inhibitors offer long-lasting skin clearance, sustained symptom relief, and a favorable safety profile. Their advanced targeting of a specific immune pathway results in fewer systemic side effects and less frequent dosing compared to older therapies. Regular medical supervision ensures continued effectiveness and early detection of rare but potential side effects.
28. Oral Small Molecule Drugs (e.g., Apremilast)
Oral small molecule drugs, such as apremilast (brand name Otezla), represent a newer approach to managing moderate psoriasis and psoriatic arthritis. Unlike biologics, which are injected and target specific cytokines, these medications are taken by mouth and work by modulating intracellular signaling pathways that influence the immune response (National Psoriasis Foundation). Apremilast specifically inhibits phosphodiesterase 4 (PDE4), an enzyme that increases inflammatory activity in immune cells.
By blocking PDE4, apremilast helps reduce the production of pro-inflammatory cytokines and increases anti-inflammatory signals, leading to improvements in both skin and joint symptoms. Apremilast is often prescribed for patients who prefer oral therapy or are unable to use biologics or traditional systemic drugs due to contraindications (American Academy of Dermatology).
Apremilast has a favorable safety profile, with the most common side effects being gastrointestinal (such as diarrhea and nausea), headache, and mild weight loss. Routine blood monitoring is not typically required, making it a convenient option for long-term management. As with all therapies, regular follow-up with a healthcare provider is important to monitor response and manage any side effects.
29. Combination Therapy

Combination therapy is a strategic approach in psoriasis management, often employed when a single treatment fails to provide sufficient control or when minimizing side effects is a priority. By using two or more therapies with different mechanisms of action, doctors can achieve better symptom relief and reduce the risk of medication resistance (National Psoriasis Foundation). Common combinations include topical steroids with vitamin D analogues, phototherapy with systemic medications, or oral drugs with biologics to maximize efficacy.
Real-world scenarios highlight the value of combination therapy. For example, a patient with moderate scalp psoriasis may use a medicated shampoo (such as coal tar or salicylic acid) alongside topical corticosteroids for faster relief. Another scenario involves a person with extensive, stubborn plaques who receives both phototherapy and methotrexate, allowing for lower doses of each treatment and minimizing side effects (American Academy of Dermatology).
Combination therapy is highly individualized, taking into account disease severity, patient preferences, and potential drug interactions. Regular monitoring by a healthcare provider ensures optimal results while minimizing the risks of adverse effects, making this a versatile and effective strategy for managing complex or treatment-resistant cases of psoriasis.
30. Lifestyle: Smoking and Alcohol

Lifestyle choices, particularly smoking and alcohol consumption, have a significant impact on the severity and progression of psoriasis. Numerous studies have shown that smoking not only increases the risk of developing psoriasis but also exacerbates existing symptoms, making flare-ups more frequent and severe (National Psoriasis Foundation). The chemicals in tobacco can trigger inflammation, compromise immune function, and interfere with the effectiveness of certain treatments. Additionally, smokers with psoriasis are at heightened risk for associated conditions such as cardiovascular disease and psoriatic arthritis.
Alcohol consumption is another well-established trigger. Heavy or frequent drinking has been linked to more persistent and treatment-resistant psoriasis, as well as a higher likelihood of relapse (National Institutes of Health). Alcohol can increase inflammation, weaken the immune system, and interact negatively with medications, particularly systemic drugs and biologics, increasing the risk of liver toxicity and other complications.
Reducing or eliminating smoking and moderating alcohol intake are strongly recommended as part of a comprehensive psoriasis management plan. These lifestyle modifications can lead to fewer flare-ups, improved treatment response, and a lower risk of long-term health complications.
31. Weight Management

Obesity is a well-established risk factor for both the development and worsening of psoriasis. Excess body fat promotes chronic inflammation, which can intensify immune system overactivity and increase the severity of psoriatic lesions (National Psoriasis Foundation). Obesity is also linked to a higher risk of developing related conditions such as psoriatic arthritis, cardiovascular disease, and metabolic syndrome, all of which can further complicate psoriasis management.
Research has shown that weight loss can lead to significant improvements in psoriasis symptoms and treatment responsiveness. Even modest reductions in body weight may decrease the frequency and intensity of flare-ups, enhance the effectiveness of systemic and biologic therapies, and reduce the risk of associated health problems (National Institutes of Health). Weight loss can also lower dosages required for some medications, minimizing potential side effects.
Effective weight management strategies include adopting a balanced, anti-inflammatory diet, increasing physical activity, and seeking support from healthcare professionals or nutritionists. These lifestyle changes not only improve psoriasis outcomes but also contribute to overall health and well-being, making them an integral part of comprehensive care.
32. Diet and Nutrition

Diet and nutrition play a supportive role in managing psoriasis, with emerging research suggesting that anti-inflammatory dietary patterns may help reduce symptom severity. Diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats—such as the Mediterranean diet—are believed to decrease systemic inflammation and support skin health (National Psoriasis Foundation). Omega-3 fatty acids, found in fatty fish, flaxseed, and walnuts, have shown potential for easing psoriatic inflammation due to their anti-inflammatory properties.
Some individuals with psoriasis also explore dietary supplements such as fish oil, vitamin D, and turmeric. While evidence is mixed, small studies suggest these supplements may provide mild symptom relief for certain patients (Healthline). It is important to consult a healthcare provider before starting any supplement, as interactions with medications or other conditions may occur.
Other nutritional strategies include avoiding or minimizing processed foods, refined sugars, and excessive alcohol, all of which can trigger inflammation and worsen flares. While no single diet is universally effective for all psoriasis patients, adopting an anti-inflammatory eating plan and maintaining a healthy weight can be beneficial in overall symptom management and health.
33. Managing Comorbidities

Psoriasis is increasingly recognized as a systemic condition with far-reaching effects beyond the skin. People with psoriasis are at higher risk for developing several serious comorbidities, most notably cardiovascular disease and type 2 diabetes (National Psoriasis Foundation). Chronic inflammation associated with psoriasis contributes to the development of atherosclerosis, high blood pressure, and metabolic syndrome, all of which significantly increase the risk of heart attack and stroke.
Diabetes risk is also elevated in individuals with psoriasis, likely due to overlapping inflammatory pathways and the impact of shared risk factors such as obesity and sedentary lifestyle (National Institutes of Health). Other common comorbidities include depression, anxiety, inflammatory bowel disease, and nonalcoholic fatty liver disease. These overlapping conditions can complicate psoriasis management and negatively affect overall health and quality of life.
Effective management requires a holistic approach, including regular screening for comorbidities, early intervention, and close collaboration between dermatologists, primary care physicians, and specialists. Addressing these associated conditions through lifestyle changes, appropriate medications, and mental health support is essential for optimizing both skin and systemic health outcomes in people with psoriasis.
34. The Importance of Sleep

Quality sleep is vital for overall health and particularly crucial for individuals with psoriasis. Research shows that poor sleep can trigger or worsen psoriasis flare-ups due to its impact on immune function and inflammation (National Psoriasis Foundation). People with psoriasis often report disrupted sleep from itching, discomfort, or associated conditions such as anxiety and depression. Chronic sleep deprivation can heighten inflammation, compromise the skin barrier, and increase the risk for comorbidities like obesity and cardiovascular disease.
Improving sleep quality can help manage symptoms and enhance quality of life. Practical strategies include establishing a consistent sleep schedule, creating a relaxing bedtime routine, and keeping the bedroom cool, dark, and comfortable. Moisturizing before bed, using soft bedding, and wearing breathable pajamas can reduce nighttime itching. Limiting screen time before sleep and avoiding caffeine or heavy meals late in the evening may also promote better rest (Sleep Foundation).
If sleep disturbances persist, it is important to discuss them with a healthcare provider, who can address underlying causes and recommend tailored interventions. Prioritizing sleep is a powerful, often overlooked, tool for improving psoriasis control and overall well-being.
35. Itch Management Strategies

Itching, or pruritus, is one of the most distressing symptoms of psoriasis and can significantly impair sleep, concentration, and overall quality of life. Managing itch requires a multifaceted approach that combines topical treatments, lifestyle adaptations, and non-drug remedies (National Psoriasis Foundation).
Topical treatments are a mainstay for itch relief. Moisturizers and emollients, applied generously and frequently, help lock in moisture and reduce dryness—one of the primary causes of itch. Topical corticosteroids and calcineurin inhibitors can also decrease inflammation and associated itching. Over-the-counter products containing menthol, pramoxine, or camphor provide a cooling or numbing effect and may deliver temporary relief (American Academy of Dermatology).
Non-drug strategies include using cool compresses, taking lukewarm oatmeal baths, and avoiding hot water or harsh soaps that can irritate the skin. Wearing loose, breathable clothing and keeping nails trimmed short can help prevent skin damage from scratching. Stress management and mindfulness techniques, such as deep breathing or meditation, may reduce the perception of itch. If itching remains severe or persistent, consulting a healthcare provider for additional therapies is recommended.
36. Sun Exposure: Risks and Benefits

Sunlight, particularly its ultraviolet B (UVB) rays, can be beneficial for many people with psoriasis. Controlled exposure to natural sunlight helps slow the rapid growth of skin cells, reduce inflammation, and clear psoriatic plaques (National Psoriasis Foundation). For some, moderate sun exposure has effects similar to clinical phototherapy and can result in noticeable symptom relief. However, excessive or unprotected sun exposure poses significant risks, including sunburn, which can worsen psoriasis through the Koebner phenomenon—where new lesions form at sites of skin injury (American Academy of Dermatology).
Repeated sunburns also increase the long-term risk of skin cancer and premature skin aging. To maximize benefits and minimize harm, it’s important to gradually build up sun exposure, starting with 5-10 minutes a day and increasing as tolerated. Always protect unaffected skin with broad-spectrum sunscreen (SPF 30 or higher), and avoid peak sunlight hours between 10 a.m. and 4 p.m. Individuals with a history of skin cancer or photosensitivity disorders should consult their healthcare provider before increasing sun exposure. Safe, mindful sun habits can support psoriasis management while preserving overall skin health.
37. Bathing and Skin Care Routines

Gentle bathing and proper skin care are essential components of psoriasis management, as they help soothe irritated skin and prevent flare-ups. Optimal bathing habits include using lukewarm—not hot—water, as excessive heat can strip the skin of natural oils and worsen dryness (National Psoriasis Foundation). Limiting baths or showers to 10-15 minutes and avoiding harsh scrubbing protect the skin’s barrier and reduce irritation.
Mild, fragrance-free, and dye-free cleansers are recommended for sensitive psoriatic skin. Products containing colloidal oatmeal or moisturizers can further ease itching and dryness. After bathing, gently blot the skin dry with a soft towel instead of rubbing. Immediately applying a thick moisturizer or emollient while the skin is still damp helps lock in hydration and improves comfort (American Academy of Dermatology).
Bath additives such as Epsom salts, Dead Sea salts, or oatmeal can provide additional relief, but bubble baths and products with alcohol or strong fragrances should be avoided. Regular, gentle skin care routines reduce inflammation, promote healing, and support the overall effectiveness of other psoriasis treatments.
38. Over-the-Counter Options

Over-the-counter (OTC) treatments can provide relief for mild psoriasis symptoms or serve as adjuncts to prescription therapies. Common OTC options include moisturizers, coal tar products, and salicylic acid preparations. Thick creams and ointments, such as petroleum jelly or fragrance-free emollients, help combat dryness and alleviate scaling (National Psoriasis Foundation). Coal tar shampoos and creams, like Neutrogena T/Gel, are effective for reducing itching, scaling, and inflammation, especially on the scalp. Salicylic acid-based products, available in shampoos and creams, help soften and remove scales, improving the absorption of other treatments.
Other OTC ingredients that may provide symptom relief include aloe vera, colloidal oatmeal, and menthol, which can soothe itching and irritation. While these products are generally safe, their effectiveness varies, and they may not provide sufficient control for moderate to severe cases (American Academy of Dermatology).
It is important to consult a doctor if symptoms persist, worsen, or are widespread, as stronger prescription medications or specialized therapies may be necessary. Medical advice is also essential when using OTC products in sensitive areas, on children, or in combination with other treatments to avoid adverse reactions.
39. The Role of Dermatologists

Dermatologists play a central role in the diagnosis and management of psoriasis, ensuring that patients receive accurate identification of their condition and tailored treatment plans. Diagnosis typically begins with a thorough skin examination and a detailed medical history. In some cases, a skin biopsy may be performed to distinguish psoriasis from other skin disorders (American Academy of Dermatology).
Once diagnosed, dermatologists assess the severity, type, and extent of psoriasis, as well as any associated symptoms such as joint pain or nail changes. They consider individual factors such as age, comorbidities, previous treatment responses, and patient preferences when crafting a treatment plan (National Psoriasis Foundation). Options may range from topical therapies and phototherapy to advanced systemic medications and biologics. Dermatologists also provide guidance on skin care routines, lifestyle modifications, and strategies for managing triggers.
Regular follow-up visits allow dermatologists to monitor progress, adjust treatments as needed, and address emerging issues such as side effects or new symptoms. Their expertise is crucial for optimizing outcomes, minimizing risks, and empowering patients to achieve long-term control over their psoriasis.
40. Telemedicine and Digital Tools

Telemedicine and digital tools have revolutionized psoriasis care, offering patients greater convenience, access, and continuity in disease management. Through virtual visits, individuals can consult with dermatologists from the comfort of their homes, making follow-up appointments and treatment adjustments more accessible—especially for those in rural areas or with limited mobility (National Psoriasis Foundation). Telehealth also facilitates quicker responses to new symptoms or treatment side effects, helping to prevent complications and optimize outcomes.
Mobile apps and digital platforms further empower patients to track symptoms, medication use, and triggers. For example, apps like MyPsoriasis or Imagine Skin Tracker allow users to document flare-ups, upload photos of affected areas, and monitor progress over time (American Academy of Dermatology). These digital records can be shared with healthcare providers, enabling more informed and personalized care decisions.
Telemedicine is also useful for patient education, as dermatologists can review skin care routines, discuss lifestyle modifications, and provide guidance on managing stress or comorbidities remotely. As digital health tools continue to evolve, they hold great promise for improving outcomes and supporting proactive, patient-centered psoriasis care.
41. Patient Support Groups

Patient support groups offer a vital resource for individuals living with psoriasis, providing a safe space for sharing experiences, challenges, and coping strategies. Connecting with others who face similar struggles can alleviate feelings of isolation, anxiety, and depression that often accompany chronic skin conditions (National Psoriasis Foundation). Support groups foster a sense of community, understanding, and encouragement, all of which are essential for emotional well-being.
These groups may meet in person or online, making them accessible regardless of location or mobility. Members often exchange practical advice on topics such as managing flares, navigating health insurance, and finding effective treatments. Support groups can also help patients stay informed about the latest research and therapies, empowering them to advocate for their own care (Healthline).
Participating in a support group has been shown to improve self-esteem, resilience, and treatment adherence. Many organizations, including the National Psoriasis Foundation, offer moderated forums, virtual events, and local chapters tailored to different age groups and needs. For many, these connections play a crucial role in maintaining hope, motivation, and a positive outlook while managing the challenges of psoriasis.
42. Pediatric Psoriasis

Pediatric psoriasis presents unique challenges distinct from adult cases, as children often face additional physical, emotional, and social hurdles. The condition can appear as early as infancy and is frequently misdiagnosed due to its resemblance to common pediatric skin ailments such as eczema or diaper rash (National Psoriasis Foundation). Symptoms in children may include smaller, less scaly patches, but the itching and discomfort can be equally intense, affecting sleep, concentration, and participation in activities.
Children with psoriasis may experience bullying, low self-esteem, and social isolation, making emotional support as important as medical management. Treatment options for pediatric patients are more limited, and therapies must be carefully tailored to balance effectiveness and safety. Mild cases are typically managed with moisturizers and low-potency topical steroids, while more severe forms may require systemic medications or phototherapy under close supervision (American Academy of Dermatology).
Family-centered care is crucial for pediatric psoriasis. Involving parents and caregivers in education, skin care routines, and emotional support helps ensure adherence and fosters coping skills. Collaboration among dermatologists, pediatricians, and mental health professionals can provide comprehensive care, supporting the child’s overall well-being and development.
43. Psoriasis in Older Adults

Psoriasis in older adults presents distinct challenges, as seniors often have additional health concerns, polypharmacy, and reduced mobility. Age-related changes in skin structure—such as thinning and decreased elasticity—can increase sensitivity to psoriasis treatments and elevate the risk of side effects from topical steroids or systemic medications (National Psoriasis Foundation). Medication safety is a major consideration; older patients may have comorbidities like cardiovascular disease, diabetes, or kidney dysfunction, which can complicate the use of immunosuppressants, biologics, or methotrexate.
Polypharmacy—taking multiple medications for various conditions—raises the risk of drug interactions and adverse events. Treatment plans for seniors must be carefully individualized, with regular monitoring of blood work and overall health. Lower-potency topicals, non-steroidal creams, and moisturizers are often preferred for sensitive skin, while newer biologic therapies may be considered for severe cases, provided the benefits outweigh the risks (American Academy of Dermatology).
Mobility limitations can make daily skin care and treatment application difficult. Support from caregivers, simplified routines, and assistive devices can improve adherence and comfort. Addressing the psychosocial impact of psoriasis, including loneliness and depression, is also important for promoting overall quality of life in older adults.
44. Pregnancy and Psoriasis

Pregnancy can have unpredictable effects on psoriasis, with some women experiencing improvement in symptoms and others noticing flare-ups or new onset of the disease. Hormonal changes during pregnancy are thought to play a significant role in these fluctuations (National Psoriasis Foundation). For about half of pregnant women with psoriasis, symptoms improve, possibly due to increased levels of certain pregnancy-related hormones that suppress immune activity. However, others may see their condition worsen, particularly after delivery when hormone levels shift again.
Treatment of psoriasis during pregnancy requires special consideration to ensure the safety of both mother and baby. Most topical therapies, such as moisturizers and low-potency corticosteroids, are considered safe when used as directed. Stronger topical steroids, systemic medications (like methotrexate and acitretin), and certain biologics are generally avoided due to potential risks to fetal development (American Academy of Dermatology). Light therapy (narrowband UVB) is often regarded as a safe and effective option for managing moderate symptoms during pregnancy.
Close collaboration with dermatologists and obstetricians ensures that treatment decisions are tailored to the individual’s needs, balancing the health of the mother with the safety of the developing baby.
45. Gender Differences in Psoriasis
Men and women experience psoriasis differently, both in terms of prevalence and disease expression. Research suggests that while the overall rates of psoriasis are similar between genders, women often report a greater impact on quality of life, particularly regarding emotional well-being and social interactions (National Psoriasis Foundation). Women may be more likely to experience psoriasis on sensitive areas such as the scalp, face, and skin folds, which can cause increased discomfort and self-consciousness.
Hormonal fluctuations unique to women, including those related to menstruation, pregnancy, and menopause, can significantly influence the severity and frequency of flares (National Institutes of Health). On the other hand, men are more likely to develop severe forms requiring systemic therapies. Gender also plays a role in treatment decisions; for example, considerations about pregnancy and breastfeeding may limit the use of certain medications in women, while men may have different risk profiles for comorbidities such as cardiovascular disease.
Understanding these gender differences enables healthcare providers to offer more personalized care, address psychosocial needs, and select treatments that align with each patient’s unique physiological and lifestyle factors.
46. The Role of Primary Care

Primary care physicians play a crucial role in the early detection and ongoing management of psoriasis. As the first point of medical contact for most patients, they are often responsible for recognizing initial symptoms, such as persistent red, scaly patches or unexplained joint pain, that may otherwise be mistaken for eczema, dermatitis, or other conditions (American Academy of Dermatology). Early identification by primary care doctors can lead to timely referrals to dermatologists, enabling patients to receive specialized care and avoid long-term complications.
In addition to diagnosis, primary care providers play a vital role in monitoring for comorbidities commonly associated with psoriasis, including cardiovascular disease, diabetes, and depression. They can provide counseling on lifestyle modifications, coordinate vaccinations, and monitor for medication side effects or interactions in patients on systemic treatments (National Psoriasis Foundation).
Effective communication and collaboration between primary care and specialist teams are essential for holistic, patient-centered care. This approach ensures that all aspects of the patient’s health are addressed, from managing skin symptoms to treating underlying conditions, ultimately improving long-term outcomes for individuals living with psoriasis.
47. Barriers to Early Care

Despite advances in diagnosis and treatment, many individuals with psoriasis experience significant barriers to early care. Stigma remains a major obstacle; visible skin symptoms can lead to embarrassment, social withdrawal, or even discrimination, causing some people to delay seeking medical attention (National Psoriasis Foundation). Misconceptions about psoriasis being contagious or “just a rash” further contribute to underreporting and delayed diagnosis.
Cost is another substantial barrier. The expenses associated with specialist visits, diagnostic tests, and long-term medications—especially advanced biologic therapies—can be prohibitive for uninsured or underinsured patients (National Institutes of Health). Even with insurance, high deductibles and copays may deter patients from pursuing necessary care or adhering to prescribed treatments.
Misinformation and lack of awareness complicate matters further. Patients may try ineffective home remedies or over-the-counter products, or they may not recognize the importance of early intervention. Limited access to dermatologists, particularly in rural or underserved areas, also contributes to delays. Addressing these barriers through education, advocacy, and expanded healthcare access is essential for ensuring that all individuals with psoriasis receive timely and effective care.
48. The Value of Patient Education

Patient education is a cornerstone of effective psoriasis management, empowering individuals and their families to make informed decisions and take an active role in their care. Understanding the chronic, immune-mediated nature of psoriasis helps patients recognize the importance of early intervention, adherence to treatment regimens, and regular follow-up with healthcare providers (National Psoriasis Foundation). Education reduces anxiety, dispels myths about contagion, and fosters realistic expectations about the course of the disease and available therapies.
Informed patients are better equipped to identify triggers, manage symptoms, and implement lifestyle modifications such as stress reduction, skin care routines, and diet changes. Education also extends to family members, who play a supportive role and can help monitor for complications or medication side effects. Family awareness can reduce stigma, improve communication, and encourage a supportive home environment (American Academy of Dermatology).
Resources such as brochures, reputable websites, support groups, and educational workshops offer valuable information. Ongoing education ensures that patients stay up-to-date with new treatments, research, and self-care strategies, ultimately leading to better disease control, improved quality of life, and more positive long-term outcomes.
49. Advances in Psoriasis Research

Recent years have witnessed remarkable progress in psoriasis research, leading to innovative therapies and a deeper understanding of disease mechanisms. Breakthroughs in immunology have identified new molecular targets, resulting in the development of highly specific biologic drugs such as IL-17 and IL-23 inhibitors, which offer rapid and sustained skin clearance with fewer side effects (National Psoriasis Foundation). Ongoing clinical trials are exploring next-generation biologics, oral small molecule drugs, and novel topical agents that promise even greater efficacy and safety.
Research is also focusing on the genetic and environmental factors that trigger psoriasis flares, as well as the microbiome’s role in disease progression and response to treatment (National Institutes of Health). Advances in digital health, including artificial intelligence and remote monitoring tools, are enhancing early diagnosis and personalized care approaches. Studies are underway to better understand the links between psoriasis and comorbidities, such as cardiovascular disease and mental health, with the goal of integrated, holistic management.
These scientific advances are rapidly expanding the treatment landscape, offering hope for improved outcomes, individualized therapies, and ultimately, a cure for psoriasis in the future.
50. Why Early Care Matters Most

Early intervention is critical in the management of psoriasis, with substantial evidence showing that prompt diagnosis and treatment lead to better long-term outcomes. Starting care soon after symptoms appear can significantly reduce the risk of complications such as psoriatic arthritis, cardiovascular disease, and mental health disorders (National Psoriasis Foundation). Early, effective therapy helps control inflammation before it causes irreversible skin or joint damage, preserving mobility and daily function.
Timely care also improves quality of life by reducing the physical and emotional burden of persistent symptoms. Studies demonstrate that patients who receive early and appropriate treatment experience fewer severe flares, better symptom management, and less impact on work, social activities, and self-esteem (National Institutes of Health). Early education and support further empower patients to adopt healthy lifestyle habits, avoid triggers, and adhere to treatment plans, which are all key to preventing relapses.
Ultimately, prioritizing early care not only minimizes the risk of long-term complications but also fosters a proactive approach to disease management—enabling individuals with psoriasis to lead healthier, more fulfilling lives.
Conclusion

Early recognition and prompt care are essential for minimizing the impact of psoriasis and preventing serious complications. Taking proactive steps—such as seeking medical evaluation for persistent skin changes, following recommended treatments, and adopting healthy lifestyle habits—can greatly enhance quality of life. If you suspect you may have psoriasis, consider using screening tools or scheduling an appointment with your healthcare provider. For additional support, resources like the National Psoriasis Foundation and American Academy of Dermatology offer education, patient communities, and guidance for managing psoriasis at every stage. Don’t wait—early action truly makes a difference.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





