Questions Cancer Patients Regret Not Asking
According to the American Cancer Society, over 1.9 million new cancer cases are expected to be diagnosed in the United States in 2024. The most commonly affected organs include the breast, lung, prostate, and colon. Despite advances in early detection, many patients still face diagnoses at later stages, limiting treatment options and survival rates. Frequently, individuals realize too late that there were crucial questions they should have asked their healthcare providers, potentially impacting their understanding, choices, and overall outcomes during their cancer journey.
1. What Are My Exact Diagnosis and Cancer Subtype?
Understanding your precise cancer diagnosis—including the specific subtype—is a critical first step in managing your treatment journey. Different cancers, even within the same organ, can have distinct molecular and genetic features that affect their growth rate, response to therapies, and overall prognosis. For example, breast cancer includes subtypes such as hormone receptor-positive, HER2-positive, and triple-negative, each requiring tailored treatment approaches (National Cancer Institute). Without clarity on these details, patients may miss out on targeted therapies, clinical trials, or important lifestyle adjustments.
Failing to ask about the exact diagnosis can also lead to confusion, anxiety, and uninformed decisions. Some patients later regret not knowing their cancer’s stage, grade, or genetic markers early on, which can influence everything from surgical options to systemic treatments such as chemotherapy or immunotherapy. Detailed information empowers patients to seek second opinions, research their condition, and participate actively in shared decision-making alongside their healthcare team. Always request a copy of your pathology report and ask your oncologist to explain the diagnosis in clear, understandable terms. For more on why knowing your subtype matters, visit the American Cancer Society.
2. What Stage Is My Cancer, and What Does It Mean?
Cancer staging describes how far the disease has progressed and is essential for developing an effective treatment plan. Staging typically considers tumor size, lymph node involvement, and whether cancer has spread (metastasized) to other organs. The numeric system—ranging from stage 0 (in situ) to stage IV (advanced/metastatic)—provides critical context for prognosis and available treatment options. According to the National Cancer Institute, accurate staging is foundational for determining eligibility for surgery, chemotherapy, radiation, or clinical trials.
Many patients later regret not asking for a thorough explanation of their cancer stage at diagnosis. Without this understanding, it can be difficult to grasp the urgency of starting treatment, the likelihood of cure, or the importance of certain interventions. For example, early-stage cancers may be curable with surgery alone, while later stages might require more aggressive or combined approaches. Details such as the TNM (Tumor, Node, Metastasis) classification can be complex but are critical for making informed choices. Always ask your doctor to clarify your stage, what it means for your prognosis, and how it affects the treatment roadmap. Learn more about cancer staging at the American Cancer Society.
3. What Are My Treatment Options—Including Clinical Trials?

Understanding all available treatment options is essential for cancer patients to make choices aligned with their values and goals. Standard treatments may include surgery, chemotherapy, radiation, immunotherapy, targeted therapy, or combinations thereof. However, for many cancers, especially rare or advanced types, clinical trials may offer access to cutting-edge therapies not yet widely available. Asking about clinical trials early in the process is crucial, as eligibility often depends on specific disease characteristics and prior treatments (National Cancer Institute).
Patients who overlook this question may later regret not exploring all possibilities, especially if standard treatments are ineffective or carry significant side effects. Sometimes, clinical trials provide not just hope but better outcomes or improved quality of life. Moreover, treatment recommendations can vary between institutions and specialists, making it wise to ask about second opinions and alternative approaches. Always request a comprehensive discussion of every available option, including the risks, benefits, and potential side effects. Additionally, inquire about the process for enrolling in a clinical trial and seek information from reputable sources such as the ClinicalTrials.gov database, which lists ongoing studies worldwide. This approach ensures no opportunity is inadvertently missed.
4. What Are the Expected Side Effects?
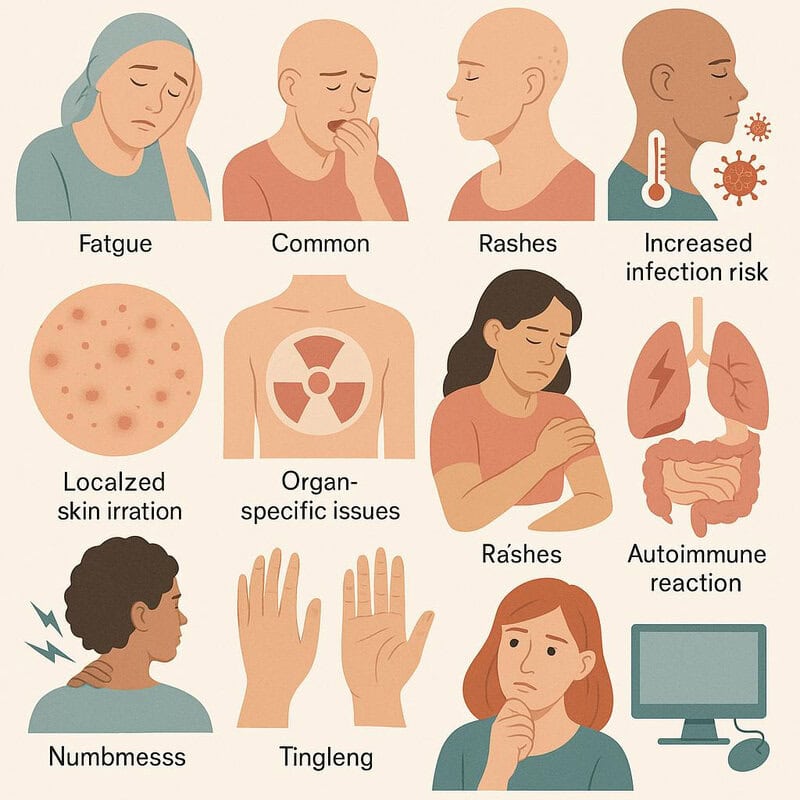
Every cancer treatment comes with the possibility of side effects—some common, others rare but serious. Chemotherapy, for instance, may cause fatigue, nausea, hair loss, and increased infection risk, while radiation can lead to localized skin irritation or organ-specific issues. Targeted therapies and immunotherapies may have unique side effects, such as rashes or autoimmune reactions (National Cancer Institute). Real-life accounts abound of patients who wish they had received more detailed information about potential complications, such as neuropathy or long-term organ damage, before starting treatment.
Anticipating side effects allows patients to make informed decisions and prepare practical strategies for managing symptoms. For example, knowing that certain chemotherapy regimens can cause severe nausea may prompt a patient to ask for anti-nausea medication in advance. Others, like numbness and tingling in the hands and feet, can be more subtle and may require early intervention to avoid lasting problems. Open conversations about side effects also help patients weigh the risks and benefits of each treatment option. For more tips on managing side effects, visit the American Cancer Society.
5. How Will Treatment Affect My Daily Life?

Cancer treatment can significantly impact daily routines, work responsibilities, and family dynamics. Side effects such as fatigue, nausea, pain, and immune suppression may limit a patient’s ability to maintain regular activities or employment. Many individuals find it challenging to predict how treatment cycles will interfere with their schedules, leading to issues like missed workdays, childcare concerns, or difficulty fulfilling household duties (American Cancer Society).
Common scenarios include needing to adjust work hours, arranging transportation to and from appointments, or seeking temporary help at home. For parents, managing fatigue while caring for young children can be especially demanding. Patients may also need to adapt their diets, exercise routines, and social calendars to accommodate treatment-related limitations. Missing this question can lead to stress, frustration, and disruptions that could have been better managed with advance planning.
Practical considerations include discussing flexible work arrangements with employers, delegating household tasks, and establishing a support network of friends and family. For more guidance, resources such as Cancer.Net offer tips for balancing treatment and daily life. Open conversations with healthcare providers can help anticipate these challenges and develop proactive solutions.
6. What Are My Chances of Recovery or Remission?

Understanding one’s prognosis is a fundamental aspect of cancer care, yet many patients hesitate to ask about their chances of recovery or remission. Prognosis refers to the likely course and outcome of a disease, often expressed as survival or remission rates. These statistics can vary greatly depending on the cancer type, stage at diagnosis, overall health, and response to treatment. For example, early-stage cancers like localized breast or prostate cancer may have high five-year survival rates, while advanced pancreatic or lung cancers are generally associated with poorer outcomes (SEER Cancer Statistics).
While numbers like “five-year survival rates” provide a general framework, each patient’s situation is unique. Knowing these odds can help individuals make informed choices about aggressive therapies, palliative care, financial planning, and personal priorities. Some patients regret not asking about prognosis early on, as it limits their ability to prepare emotionally, practically, and financially. It’s important to request a candid discussion about individualized prognosis, including factors that could improve or worsen outcomes. Reliable information empowers patients and families to balance hope with realistic expectations. For further reading, the Cancer.Net: Understanding Cancer Prognosis page offers in-depth guidance.
7. What Is the Goal of My Treatment?
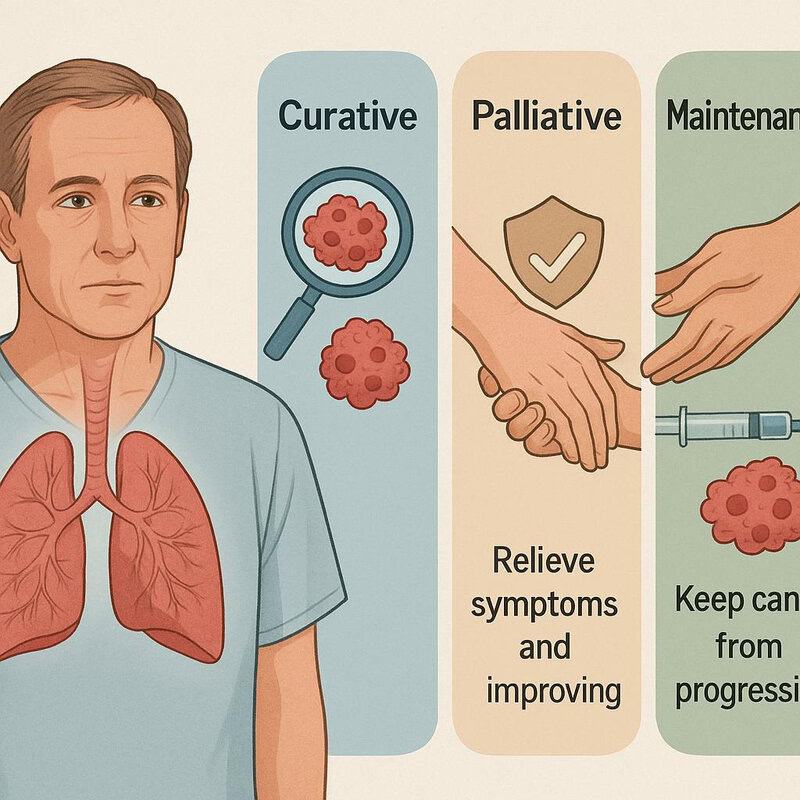
Clarifying the goal of treatment is vital for every cancer patient, as it helps set realistic expectations and guides decision-making. Treatments generally fall into three broad categories: curative, palliative, and maintenance. Curative treatments aim to eradicate the cancer and achieve long-term remission or cure, which is often possible in early-stage cancers. Palliative therapies, on the other hand, focus on relieving symptoms and improving quality of life when a cure is not feasible, particularly in advanced or metastatic cases. Maintenance therapy strives to keep cancer from progressing after initial treatments have controlled the disease (American Cancer Society).
Many patients later regret not asking about the intent of their recommended therapy. Without this understanding, individuals may undergo aggressive treatments with unrealistic hopes of cure or, conversely, may not realize that certain therapies are designed to prolong life or manage symptoms rather than eliminate cancer. Knowing the treatment goal enables better communication with healthcare teams, supports informed consent, and helps patients weigh the benefits and burdens of therapy. For an in-depth explanation of treatment goals and how they are determined, visit the National Cancer Institute.
8. What Will Happen If I Do Nothing?

While it may seem counterintuitive, asking about the possible outcomes of declining treatment is a critical question for cancer patients. The natural progression of untreated cancer varies by type, stage, and individual health factors. In some cases, such as certain slow-growing prostate cancers, a strategy called “watchful waiting” or “active surveillance” might be appropriate, allowing patients to avoid treatment side effects while closely monitoring for any changes (American Cancer Society). However, for most aggressive or advanced cancers, foregoing treatment can lead to rapid progression, worsening symptoms, and reduced survival.
Some patients later wish they had asked this question, as it provides a clearer understanding of the urgency or flexibility in decision-making. Real-life stories highlight individuals who chose observation due to advanced age, coexisting health problems, or personal values, sometimes experiencing a better quality of life for a period. Others, unaware of the consequences, delayed treatment and faced more limited options later. This conversation helps patients weigh the risks and benefits of intervention versus observation and ensures their choices align with their values. For further insight, the Cancer.Net: Choosing Not to Have Treatment resource offers valuable guidance.
9. How Will This Affect My Fertility?

Cancer treatments such as chemotherapy, radiation, and certain surgeries can significantly impact fertility in both men and women. Chemotherapy may damage eggs or sperm, while radiation to the pelvic area can harm reproductive organs. Some treatments cause temporary infertility, while others result in permanent loss of fertility (National Cancer Institute: Fertility in Women with Cancer). This is a crucial question for patients of childbearing age, yet many later regret not discussing it before starting therapy.
Comparisons between patients who explored fertility preservation and those who did not reveal stark contrasts in options and outcomes. Techniques such as egg or embryo freezing, sperm banking, and ovarian tissue preservation can safeguard the possibility of having biological children in the future. Early consultation with a reproductive endocrinologist is often necessary, as fertility preservation procedures must typically occur before cancer treatment begins. Patients who overlook this question may face unexpected grief and loss later, sometimes when they are already coping with the emotional toll of cancer survivorship. For more information and detailed options, visit the American Cancer Society: Fertility and Women With Cancer.
10. Should I Get a Second Opinion?

Seeking a second opinion is a step many cancer patients later wish they had taken, as it can significantly influence both diagnosis and treatment choices. A second opinion can confirm your diagnosis, suggest alternative treatments, or provide access to specialists who are familiar with the latest advances in cancer care. Multidisciplinary teams—often available at major cancer centers—bring together oncologists, surgeons, radiologists, and other specialists to review and discuss complex cases, ensuring that recommendations are comprehensive and personalized (American Cancer Society: Getting a Second Opinion).
Real-life examples abound where patients, after consulting another expert or team, discovered additional treatment options, eligibility for clinical trials, or even a modified diagnosis that changed their entire care plan. Second opinions are especially valuable for rare cancers, unusual presentations, or when the proposed treatment involves significant risks or life changes. Asking about this early can help ensure that all avenues are explored, and it can provide peace of mind for both patients and families. For guidance on how to request a second opinion and what to expect, consult the National Cancer Institute: Getting a Second Opinion resource.
11. What Are the Costs and Insurance Implications?

The financial impact of cancer care—often referred to as “financial toxicity”—can be as overwhelming as the disease itself. Treatments may involve not only hospital bills and medications but also expenses for travel, lodging, childcare, and lost income. Patients who do not ask detailed questions about costs and insurance coverage often encounter surprise bills or discover too late that certain treatments, scans, or medications are not fully covered by their plan (Cancer.Net: Managing the Cost of Cancer Care).
It is essential to clarify what is covered by your insurance, what your out-of-pocket responsibilities might be, and whether prior authorizations are needed for any procedures. Some patients later regret not seeking out a financial counselor or social worker—resources often available at cancer centers—to help navigate the complexities of insurance policies and financial aid. Inquiring about generic drug options, assistance programs, and payment plans can also prevent undue stress. For more information and helpful tools, the American Cancer Society: Financial Support and Resources provides guidance to avoid financial pitfalls and ensure you are fully informed before starting treatment.
12. Are There Support Services for Me and My Family?

Cancer is not only a medical challenge but also an emotional and practical one for both patients and their loved ones. Many regret not asking early about the array of support services available to help navigate the journey. Professional counseling, social work assistance, and support groups can address psychological distress, provide coping strategies, and offer guidance on practical matters such as transportation, legal issues, or advance directives (American Cancer Society: Support Programs and Services).
Patients who connect with support groups often report feeling less isolated and more empowered, sharing their experiences and learning from others who have faced similar challenges. Access to social workers can help families manage complex logistics, find financial assistance, and coordinate care. Emotional support—whether from professional counselors or peer groups—has been shown to improve quality of life and even treatment outcomes. Advice for accessing these resources includes asking your cancer care team for referrals, tapping into hospital-based programs, and exploring reputable online communities such as those listed by Cancer.Net: Support Groups. Early engagement with support services can make a meaningful difference throughout the cancer experience.
13. What Are My Nutritional Needs During Treatment?

Nutrition plays a vital role in supporting cancer patients through treatment and recovery. Adequate nutrition can help maintain strength, support the immune system, manage side effects, and improve overall treatment outcomes. However, nutritional needs can vary greatly depending on the type of cancer, treatment regimen, and individual factors such as weight loss, appetite changes, or gastrointestinal symptoms (National Cancer Institute: Nutrition in Cancer Care).
Some patients regret not asking about dietary support, only to struggle later with issues like malnutrition, dehydration, or difficulty eating. There is no universal diet for all cancer patients—dietary guidance might include increasing protein and calorie intake, addressing food aversions, or managing side effects like nausea and mouth sores. Consulting a registered dietitian with oncology experience can help tailor a plan to individual needs and preferences. Optimizing nutrition may also involve meal planning, using supplements, or incorporating small, frequent meals. For more information and practical tips, the American Cancer Society: Appetite Changes and Cancer.Net: Diet and Nutrition provide evidence-based resources to help patients stay nourished during treatment.
14. What Symptoms Should I Report Immediately?

Recognizing which symptoms warrant urgent medical attention is crucial for cancer patients, as prompt action can prevent complications and even save lives. Some symptoms—such as fever above 100.4°F (38°C), sudden shortness of breath, chest pain, uncontrolled bleeding, severe pain, confusion, or signs of infection—require immediate reporting to your healthcare team (Cancer.Net: When to Call the Doctor During Cancer Treatment).
Case studies highlight the importance of quick response: patients who developed neutropenic fever (a serious infection risk when white blood cells are low) and sought help promptly often avoided severe complications, while those who delayed care sometimes faced life-threatening situations. Similarly, reporting new neurological symptoms, such as weakness or confusion, can indicate urgent issues like blood clots or brain involvement that need rapid intervention.
To empower patients, healthcare teams often provide a checklist of symptoms to monitor. This should include:
High fever or chills
Sudden or severe pain
Unexplained bleeding or bruising
Shortness of breath or chest pain
Confusion, weakness, or severe headache
Persistent vomiting or diarrhea
For a comprehensive list and guidance, see the American Cancer Society: When to Call the Doctor.
15. How Will My Pain Be Managed?

Pain is a common and sometimes overwhelming symptom for many cancer patients, yet it remains under-treated when not discussed openly. An effective pain management plan should be tailored to each individual, taking into account the type and intensity of pain, as well as personal preferences and past experiences. Pain relief modalities can range from oral medications (like acetaminophen, NSAIDs, or opioids) to nerve blocks, physical therapy, acupuncture, and even integrative approaches such as relaxation techniques (National Cancer Institute: Pain in People With Cancer).
Proactive communication about pain is vital. Many patients later regret not asking more about what to expect, how to report pain, and what options are available if initial treatments are insufficient. Unmanaged pain can lead to decreased quality of life, sleep disturbances, and emotional distress. Regular assessment and adjustment of the pain plan ensure optimal relief and function. It’s important to discuss potential side effects of pain medications and to voice any concerns about dependency or tolerance. For more information on cancer pain management and available resources, visit the American Cancer Society: Pain Control.
16. How Will You Monitor My Progress?

Monitoring progress during and after cancer treatment is essential for assessing response, managing side effects, and detecting possible recurrences early. Follow-up typically involves a combination of physical exams, imaging studies (such as CT, MRI, or PET scans), and bloodwork to track tumor markers or organ function (National Cancer Institute: Follow-Up Care After Cancer Treatment). The frequency and type of monitoring depend on the cancer type, stage, and individual risk factors.
Patients who understand their follow-up plan are better prepared to recognize warning signs and adhere to scheduled appointments. Real-life accounts demonstrate the importance of regular monitoring: some survivors report that routine imaging caught early recurrences or new cancers, allowing for timely intervention and improved outcomes. Conversely, those unaware of what to expect may miss critical appointments or ignore subtle symptoms. Key questions to ask include how often tests will be done, what specific markers will be checked, and the implications of test results. For more on the importance of follow-up care and what to expect, refer to the American Cancer Society: Follow-Up Care After Cancer Treatment.
17. Are There Long-Term or Late Side Effects?

Many cancer treatments can cause side effects that appear months or even years after therapy has ended, known as long-term or late effects. Radiation therapy may lead to issues like fibrosis, lymphedema, or cardiovascular problems, while chemotherapy can cause neuropathy, heart or lung damage, cognitive changes (“chemo brain”), or secondary cancers (National Cancer Institute: Late Effects of Cancer Treatment). Hormonal therapies and targeted agents can also leave a lasting impact on bone health or metabolism.
Survivor stories often highlight unexpected challenges years after initial recovery. Some develop chronic fatigue, persistent pain, or infertility, while others experience emotional effects such as anxiety or depression triggered by ongoing health concerns. Being aware of these possibilities allows patients to watch for symptoms and seek timely intervention. Regular follow-up visits are critical for monitoring potential late effects. Patients should ask what signs or symptoms to report, what specific tests are recommended long-term, and how risks can be reduced through lifestyle changes or preventive care. For a comprehensive overview of late and long-term side effects, see the American Cancer Society: Late Effects of Cancer Treatment.
18. Can I Continue Working or Attending School?

Many cancer patients are concerned about maintaining their work or educational responsibilities during treatment. The ability to continue working or attending school depends on the type and intensity of treatment, side effects, and the flexibility of employers or institutions. Some people are able to keep working or studying with minor adjustments, while others may need extended leave or a reduced schedule (Cancer.Net: Working During Cancer Treatment).
Work and school accommodations can include remote work, flexible hours, reduced course loads, or time off for medical appointments. In the United States, legal protections such as the Americans with Disabilities Act (ADA) and the Family and Medical Leave Act (FMLA) offer rights to reasonable accommodations and extended leave (American Cancer Society: Working During and After Cancer Treatment). Patient stories often highlight the importance of open communication with supervisors, human resources, or school administrators, as well as the value of a supportive network. Some find empowerment in continuing their careers or studies, while others benefit from focusing on rest and recovery. Discussing these options early allows for better planning and less stress throughout the cancer journey.
19. Are There Genetic or Hereditary Components?

Understanding whether a cancer has genetic or hereditary components is crucial for both patients and their families. Some cancers, such as breast, ovarian, colorectal, and prostate cancers, may be linked to inherited gene mutations like BRCA1, BRCA2, or Lynch syndrome (National Cancer Institute: Cancer Genetics Overview). Genetic testing can identify these mutations, offering valuable information about personal risk, guiding treatment decisions, and informing family members about their potential risks.
Patients who undergo genetic counseling and testing can sometimes access targeted therapies or join clinical trials tailored to their genetic profile. Moreover, discovering a hereditary risk allows relatives to consider early screening, preventive measures, or lifestyle adjustments, sometimes dramatically reducing cancer incidence in families. For example, knowledge of a BRCA mutation has led many women to opt for enhanced surveillance or preventive surgery, significantly improving outcomes. Those who didn’t ask about hereditary risks often express regret, particularly if other family members are later diagnosed with preventable or detectable cancers. For more details on genetic counseling and its benefits, visit the American Cancer Society: Family Cancer Syndromes.
20. What Should I Know About Complementary or Alternative Therapies?

The topic of complementary and alternative therapies is common among cancer patients seeking to manage symptoms, reduce stress, or improve overall well-being. Evidence-based complementary therapies—such as acupuncture, massage, yoga, and meditation—are often safely integrated with conventional treatment to help control pain, nausea, anxiety, and fatigue (National Cancer Institute: Complementary and Alternative Medicine). However, “alternative” therapies that claim to cure cancer in place of standard care can be dangerous, ineffective, or even interfere with proven treatments.
Many patients regret not discussing these options with their oncology team, sometimes resulting in harmful interactions or missed benefits. Openly asking about complementary methods helps ensure that choices are safe and supported by research. Oncology centers may offer integrative medicine consults to guide patients on which therapies are beneficial and which to avoid. Always ask about potential side effects, interactions with prescribed medications, and credentialing of practitioners. For more information on making informed decisions about complementary and alternative therapies, visit the American Cancer Society: Complementary and Integrative Medicine. Clear communication about these therapies ensures a holistic, effective, and safe approach to cancer care.
21. How Will My Mental Health Be Supported?

The psychological impact of a cancer diagnosis and treatment can be profound, often resulting in anxiety, depression, fear, or feelings of isolation. Yet, many patients do not realize the importance of proactively addressing mental health as part of their care plan. Mental health support may include counseling, psychotherapy, psychiatric care, or group therapy, all of which can help patients and families process emotions, develop coping strategies, and maintain hope (Cancer.Net: Managing Emotions).
Examples from cancer survivors highlight how access to mental health professionals or peer support groups can make a meaningful difference in quality of life and the ability to cope with challenges. Some treatment centers have dedicated psycho-oncology teams, while others can refer patients to external specialists experienced in cancer care. It is important to ask about the availability of psychologists, psychiatrists, or social workers, as well as programs for mindfulness, art therapy, or stress reduction. For additional support, organizations like the American Cancer Society offer resources tailored to emotional well-being. Addressing mental health is a vital component of holistic cancer care, and early intervention can greatly improve resilience and overall outcomes.
22. What Should I Tell My Children or Dependents?

Communicating a cancer diagnosis to children or dependents is one of the most challenging aspects for families. Age-appropriate communication is essential—young children may need simple, honest explanations, while teens or adult dependents can handle more complex conversations. Experts recommend using clear language, reassuring children about ongoing care, and allowing space for questions and emotional responses (American Cancer Society: Helping Children When a Family Member Has Cancer).
Real-life advice from parents and caregivers highlights the value of honesty and consistency. Many regret withholding information, finding that children often sense when something is wrong and may experience greater anxiety if left in the dark. Support services, including child life specialists, family counselors, and school-based resources, can help guide these conversations and provide ongoing emotional support. Some cancer centers offer workshops or family programs to help children process their feelings and adjust. For additional resources, the Cancer.Net: Talking With Children About Cancer page provides practical tips and downloadable guides. Seeking help early ensures that children and dependents feel supported and secure throughout the cancer journey.
23. How Do I Prepare for Surgeries or Procedures?

Preparation for surgery or invasive procedures is a critical step in the cancer care process. Patients who understand what to expect before, during, and after surgery often experience smoother recoveries and reduced anxiety. Pre-surgical preparation may include fasting, medication adjustments, preadmission testing, and arranging for post-operative transportation and support at home (American Cancer Society: Preparing for Surgery).
Comparisons among patients show that those who follow thorough preparation protocols and ask about details—such as pain management, potential complications, and expected hospital stay—tend to recover more quickly and with fewer surprises. Understanding the recovery timeline helps with planning for time off work, mobility aids, wound care, and physical therapy if needed. A patient checklist for surgical preparation might include confirming medication instructions, arranging childcare or help at home, preparing meals in advance, and gathering questions for the surgical team. For a comprehensive pre-surgery checklist and recovery guidance, see the Cancer.Net: Practical Tips for Surgery. Asking about each step ensures a confident approach and facilitates optimal outcomes.
24. Will My Appearance Change?

Many cancer treatments can lead to physical changes that affect appearance, such as hair loss, weight fluctuations, skin changes, and surgical scars. Chemotherapy is well-known for causing temporary hair loss, while radiation may result in localized hair shedding or skin discoloration. Weight changes—whether gain from steroids or loss due to appetite suppression—are also common, sometimes leading to significant body image concerns (American Cancer Society: Hair Loss).
Patients often regret not asking about these changes beforehand, which can intensify feelings of shock or loss when they occur. Openly discussing potential appearance-related side effects allows for proactive steps, such as obtaining wigs, scarves, or hats before hair loss begins, or receiving guidance on skin care and clothing adaptations. Support groups and counseling can help patients process emotional reactions and build self-confidence. Practical advice includes using gentle hair and skin products, exploring cosmetic solutions, and seeking support from organizations like Look Good Feel Better, which offers free programs to help manage appearance-related changes. Addressing body image concerns with healthcare teams ensures patients feel prepared and supported throughout their cancer journey.
25. Are There Risks of Infection or Immunosuppression?
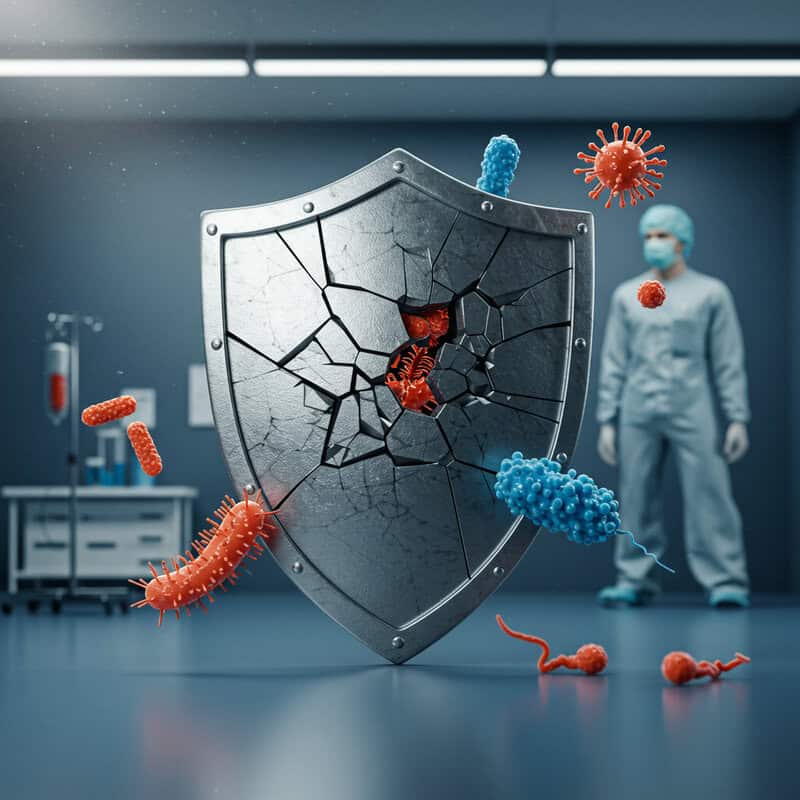
Cancer treatments such as chemotherapy, radiation, and certain targeted therapies can weaken the immune system, increasing the risk of infections. This immunosuppression may be temporary or, in some cases, longer-lasting, depending on the specific drugs or interventions used. Patients with low white blood cell counts (neutropenia) are particularly vulnerable to bacterial, viral, and fungal infections, which can become serious very quickly (National Cancer Institute: Infection and Neutropenia).
Prevention is paramount. Strategies include frequent hand-washing, avoiding crowds and sick contacts, maintaining good oral hygiene, and receiving recommended vaccines (when appropriate). Patients should also be aware of food safety guidelines to minimize the risk of foodborne illness. If exposed to potential sources of infection or experiencing symptoms such as fever, chills, or sore throat, immediate contact with the healthcare team is essential. Prompt reporting can lead to early intervention and prevent complications. Many regret not asking about infection risks, as awareness enables proactive behavior and rapid response to warning signs. For comprehensive infection prevention tips, see the American Cancer Society: Infections in People With Cancer.
26. How Will You Coordinate with My Other Doctors?

Effective cancer care often requires a multidisciplinary approach involving oncologists, surgeons, primary care physicians, specialists, and allied health professionals. Coordination among these providers is essential for ensuring consistent care, avoiding drug interactions, and addressing the full spectrum of a patient’s needs. However, real-world challenges such as fragmented communication, delayed record sharing, or conflicting recommendations can occur, leading to confusion and potential gaps in care (Cancer.Net: Coordinating Your Care).
Patients who ask about care coordination can advocate for integrated treatment plans and clear communication between all members of their healthcare team. Practical tips include designating a primary physician or nurse navigator to oversee care, maintaining a personal health record, and ensuring all providers have up-to-date information about medications and treatments. Some cancer centers offer formal tumor boards or case conferences where multiple experts review and discuss complex cases together, resulting in more comprehensive and personalized recommendations. For more advice on managing multidisciplinary care and ensuring all providers are aligned, visit the American Cancer Society: Multidisciplinary Cancer Care. Proactive coordination helps prevent medical errors and optimizes outcomes for cancer patients.
27. Can I Travel During Treatment?

The possibility of travel during cancer treatment is a common concern. Whether for work, family commitments, or personal reasons, many patients wonder if travel is safe or feasible. The answer depends on the type and schedule of treatment, overall health, immune status, and potential side effects like fatigue or risk of infection. Some treatments may require frequent hospital visits or strict timing, making travel challenging, while others may allow for flexibility (American Cancer Society: Traveling During Cancer Treatment).
Patient experiences vary—some are able to travel with advance planning and support, while others find it best to postpone trips until after treatment. Key considerations include proximity to medical facilities, access to necessary medications, travel insurance that covers pre-existing conditions, and preparing for emergencies. Discussing travel plans with your oncology team is essential; they can help assess risks, adjust treatment schedules, and provide documentation or referrals if needed. Planning ahead may involve arranging for laboratory tests or infusions at another location or carrying a summary of your diagnosis and treatments. For detailed advice on safe travel during cancer care, visit the Cancer.Net: Planning for Travel.
28. What Happens If Treatment Stops Working?

When cancer treatment is no longer effective, it’s a pivotal moment that requires honest, compassionate conversations and careful consideration of next steps. Disease progression can happen gradually or suddenly, and it’s crucial for patients to understand what signs to watch for and how their care team will monitor changes. At this stage, new treatment options may include switching to different medications, enrolling in clinical trials, or considering palliative therapies designed to relieve symptoms and improve quality of life (Cancer.Net: When Cancer Treatment Stops Working).
Ongoing communication with healthcare providers is essential. Some patients regret not asking early about what to expect if the disease progresses, which can delay critical decisions about future care, advance directives, or hospice. Discussing the possibility of treatment resistance helps families prepare emotionally and practically, and it ensures that patient wishes remain at the center of care planning. For more information about dealing with treatment changes and exploring supportive care resources, visit the American Cancer Society: Palliative Care. Early, open discussions provide clarity and support, empowering patients to navigate the next chapter of their journey with dignity and informed choice.
29. How Will My Sexual Health Be Affected?

Cancer and its treatments can profoundly impact sexual health, yet many patients feel uncomfortable or embarrassed to broach the topic. Physical changes may include vaginal dryness, erectile dysfunction, decreased libido, changes in sensation, or pain during intercourse—effects that can result from surgery, chemotherapy, radiation, or hormone therapy (American Cancer Society: Sexual Side Effects). Emotional factors, such as body image concerns, fatigue, and anxiety, often further complicate intimacy and self-confidence.
Patient stories reveal the importance of honest conversations with healthcare providers about potential changes and strategies for adaptation. Some couples find that open communication and counseling help maintain or rebuild intimacy, while others benefit from medical interventions such as lubricants, medications, or pelvic floor therapy. Regret is common among those who did not ask about sexual health, as unexpected changes can lead to distress or relationship strain. Dedicated resources and support services—including sex therapists, support groups, and educational materials—are available through organizations such as Cancer.Net: Cancer and Sexuality. Addressing sexual health early helps empower patients to seek solutions and maintain quality of life throughout and after cancer treatment.
30. Are Vaccinations Safe During Treatment?

Vaccinations play a critical role in protecting cancer patients from infections, but not all vaccines are safe or recommended during active treatment. Generally, inactivated (non-live) vaccines such as the annual flu shot and COVID-19 vaccines are considered safe and are often encouraged to reduce the risk of serious illness. However, live vaccines—such as the measles, mumps, and rubella (MMR) or the varicella (chickenpox) vaccine—are typically avoided during chemotherapy or when the immune system is suppressed, as they can pose infection risks (National Cancer Institute: Vaccines and Cancer Treatment).
Cancer patients should consult their oncology team before receiving any vaccine. Timing is also important; some vaccines are best administered before treatment begins or during periods when immune function is stronger. Patients often regret not asking about immunizations, particularly during flu season or outbreaks of preventable diseases. Best practices include keeping an up-to-date vaccination record, coordinating with both oncologists and primary care providers, and ensuring close contacts are also immunized to provide “cocoon” protection. For detailed, evidence-based guidance on vaccines during cancer care, visit the American Cancer Society: Vaccines and Cancer Treatment.
31. Will I Need Rehabilitation or Physical Therapy?

Rehabilitation and physical therapy are often essential components of cancer recovery, helping patients regain strength, mobility, and independence after treatment. The need for rehab may arise due to surgery, radiation, chemotherapy, or the cancer itself, especially if these cause muscle weakness, joint stiffness, balance issues, or lymphedema (American Cancer Society: Rehabilitation for Cancer Survivors).
Common types of therapy include physical therapy for restoring movement and strength, occupational therapy for daily living skills, and speech therapy for swallowing or speech difficulties. Some patients also require specialized interventions for lymphedema management or cognitive rehabilitation after “chemo brain.” Survivor experiences highlight the benefits of early and consistent rehab—many report faster recoveries, improved quality of life, and reduced risk of long-term disability. Those who did not ask about or pursue therapy often face prolonged challenges that could have been mitigated. Patients should discuss symptoms like fatigue, pain, or movement limitations with their care team to determine if a referral is appropriate. For more information about cancer rehabilitation and available services, visit the Cancer.Net: Rehabilitation for Cancer Survivors.
32. How Will You Address My Spiritual or Cultural Needs?

Spirituality and cultural beliefs play a significant role in how individuals experience illness, cope with stress, and make healthcare decisions. Many cancer centers recognize this and offer spiritual care services, such as access to chaplains, religious leaders, or meditation spaces, to help patients find comfort, meaning, and hope during treatment (National Cancer Institute: Spirituality in Cancer Care). Respect for cultural practices may involve accommodating dietary restrictions, language preferences, family involvement in decision-making, or specific rituals around healing and end-of-life care.
Patients who communicate their spiritual or cultural needs often report improved emotional well-being, a stronger sense of support, and greater satisfaction with their care. Real-world examples include integrating prayer, traditional healing practices, or cultural ceremonies alongside medical treatment. Healthcare teams can facilitate this by asking about preferences, connecting patients with spiritual advisors, and ensuring interpreters or culturally competent resources are available. For more on integrating spiritual and cultural care in the cancer setting, visit the American Cancer Society: Spirituality in Cancer Care. Open dialogue ensures holistic care that honors each patient’s values, beliefs, and identity, contributing to overall well-being and resilience.
33. What Palliative Care Options Are Available?

Palliative care is specialized medical care focused on providing relief from the symptoms, pain, and stress of cancer, regardless of the stage or expected outcome. It is appropriate at any point in the illness—not just at end-of-life—and can be provided alongside curative or life-prolonging treatments (National Cancer Institute: Palliative Care). Services may include pain and symptom management, psychological support, spiritual care, and assistance with complex decision-making.
Patients who receive early palliative care often experience better symptom control, improved emotional well-being, and enhanced quality of life. Real-life stories highlight individuals who, with the support of a palliative care team, achieved better pain management, found meaning in their experience, and maintained dignity throughout their cancer journey. Some regret not learning about palliative care sooner, mistakenly equating it with hospice or giving up. Asking about these options ensures a proactive approach to comfort and holistic well-being. For more information about what palliative care involves and how it can support both patients and families, visit the American Cancer Society: Palliative Care.
34. How Do I Handle Advance Directives and End-of-Life Planning?
Advance directives are legal documents that enable individuals to outline their preferences for medical care if they become unable to communicate or make decisions. Common forms include a living will, which details the types of life-sustaining treatments a person wants or does not want, and a durable power of attorney for healthcare, which designates a trusted individual to make decisions on their behalf (American Cancer Society: Advance Directives).
Early discussions about these topics are vital, as they ensure that care aligns with a patient’s values, reduce stress for family members, and prevent unwanted or unnecessary interventions. Many patients and families later regret delaying these conversations, finding themselves unprepared during a crisis. Initiating the conversation with your oncology team or a social worker can help clarify options and provide the necessary forms. For more detailed guidance and free downloadable resources, the Cancer.Net: Advance Directives page offers step-by-step support. Addressing advance directives and end-of-life planning early fosters peace of mind and empowers patients to make informed choices about their care journey.
35. Are My Medications Compatible with My Cancer Treatment?
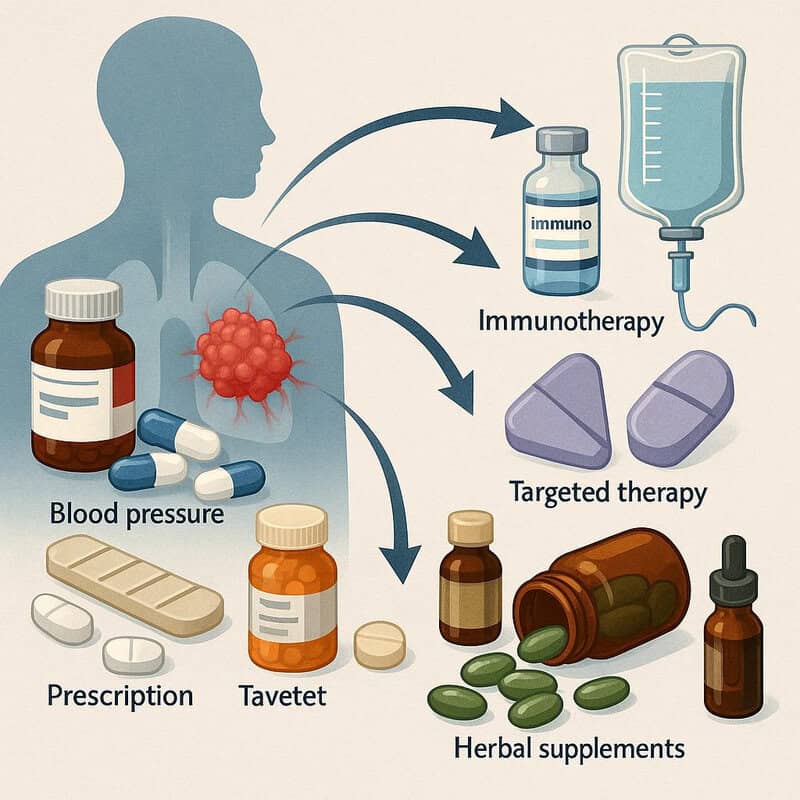
Drug interactions are a critical but sometimes overlooked aspect of cancer care. Many cancer patients take medications for other conditions—such as blood pressure, diabetes, depression, or pain—which can potentially interact with chemotherapy, immunotherapy, or targeted agents. These interactions can reduce the effectiveness of treatment, increase toxicity, or even lead to serious adverse events (National Cancer Institute: Drug Interactions in Cancer Treatment).
For example, some common medications, like certain antibiotics or blood thinners, may intensify side effects or require dose adjustments. Herbal supplements and over-the-counter drugs can also pose risks; St. John’s wort, for instance, can reduce the efficacy of some chemotherapy drugs. Real-life reports highlight patients who experienced unexpected complications because they did not disclose all their medications to their oncology team. Best practices include keeping an up-to-date list of all prescriptions, supplements, and vitamins, and sharing it with every healthcare provider. Pharmacists and oncology nurses can assist with medication reviews to identify and prevent harmful interactions. For more information and tools to manage medication safety, visit the American Cancer Society: Chemotherapy Safety.
36. What Should I Expect from Follow-Up Care?
Follow-up care is an essential phase for cancer survivors, encompassing ongoing monitoring, management of late effects, and support for overall well-being. A survivorship care plan typically includes a personalized schedule for physical exams, blood tests, imaging studies, and assessments for potential recurrence or secondary cancers (National Cancer Institute: Follow-Up Care After Cancer Treatment). These appointments may also address lingering side effects, emotional health, and preventive care recommendations.
Patients who ask about follow-up care tend to feel more confident and proactive, knowing what signs to watch for and when to seek help. Survivor stories often underscore the value of vigilant monitoring—early detection of recurrence through routine scans or bloodwork has enabled timely intervention and improved outcomes. Conversely, those without clear follow-up plans sometimes miss subtle symptoms or delay reporting changes, impacting their long-term health. It’s important to clarify who will coordinate your follow-up, the frequency of visits, and what symptoms should prompt immediate contact with your care team. For more on what to expect from survivorship care and how to develop a comprehensive plan, visit the American Cancer Society: Follow-Up Care.
37. How Will This Affect My Memory or Cognitive Function?

Many cancer patients experience difficulties with memory, attention, and thinking during or after treatment—a phenomenon often called “chemo brain” or cancer-related cognitive impairment. Symptoms can include forgetfulness, trouble concentrating, slower processing speeds, and difficulty multitasking. These changes may be temporary or, in some cases, persist long after treatment ends (National Cancer Institute: Memory or Concentration Problems).
Patient experiences vary widely. Some report only mild disruptions, while others find cognitive challenges significantly impact their daily activities, work, or relationships. Those who are aware and prepared for these effects often manage better, utilizing coping strategies such as keeping detailed calendars, making to-do lists, breaking tasks into smaller steps, and allowing extra time for activities. Cognitive rehabilitation, occupational therapy, and brain-training exercises can also be beneficial. Patients frequently regret not asking about cognitive side effects, as early recognition enables more effective support and adaptation. For more information about chemo brain, coping strategies, and real-life survivor tips, visit the American Cancer Society: Cognitive Problems After Cancer Treatment.
38. Can I Take Part in Decision-Making About My Care?

Shared decision-making is a cornerstone of modern cancer care, empowering patients to actively participate in choices about their treatment and overall care plan. This collaborative approach involves open communication between patients, families, and healthcare providers, ensuring that individual values, preferences, and goals are considered alongside medical expertise (Cancer.Net: Shared Decision-Making).
Patients who engage in shared decision-making often report greater satisfaction with their care, a stronger sense of control, and improved quality of life. They feel empowered to ask questions, express concerns, and weigh the pros and cons of different options. In contrast, those who feel excluded or uninformed may experience frustration, confusion, or regret about their choices later on. Examples include patients who, after discussing options in depth, chose less aggressive therapies that aligned with their values, or others who pursued clinical trials after learning all available alternatives.
To facilitate shared decision-making, it is helpful to bring a list of questions to appointments, involve loved ones in discussions, and request clear explanations of risks and benefits. The National Cancer Institute: Making Decisions About Cancer Treatment offers tools and guidance for becoming an active partner in your care.
39. What Should I Bring Up If My Symptoms Change?
Reporting changes in symptoms promptly is essential for effective cancer management and ensuring the best possible outcomes. Keeping a symptom diary or using an app to track new or worsening issues—such as pain, fatigue, swelling, fever, or neurological changes—enables patients and their care teams to identify patterns and intervene early (American Cancer Society: When to Call the Doctor).
Patient anecdotes reveal that early reporting often leads to timely adjustments in treatment, prevention of complications, or even detection of recurrence. For example, a patient who noticed and reported new swelling was promptly evaluated for lymphedema and received interventions that prevented further progression. Conversely, those who delayed sharing symptoms sometimes faced avoidable hospitalizations or worsening side effects. Guidance includes notifying your care team about:
Persistent or severe pain
Sudden fatigue or weakness
Unexplained weight loss or gain
Changes in appetite or digestion
New lumps, swelling, or rashes
Any unusual mental or physical changes
For more advice on symptom tracking and when to seek help, visit the Cancer.Net: When to Call the Doctor.
40. How Will You Communicate With Me and My Family?

Clear, consistent communication between the healthcare team, patients, and families is critical throughout the cancer journey. Establishing a communication plan—such as how updates will be shared, who will be included in major discussions, and how to reach the team in emergencies—helps prevent misunderstandings and fosters trust (Cancer.Net: Communicating With Your Health Care Team).
Family meetings, regular check-ins, and the use of patient portals or secure messaging systems can ensure that everyone stays informed about changes in treatment, test results, or care needs. Real-world examples highlight the difference: patients who had scheduled team meetings and clear points of contact felt more supported and empowered to make decisions, while those who lacked structured communication often experienced confusion, delays, or conflicting information.
Best practices include designating a family spokesperson, requesting summaries after major appointments, and clarifying the preferred method of communication (phone, email, portal messages). It’s also important to ensure that language needs or hearing impairments are addressed. For more strategies on effective communication in cancer care, see the American Cancer Society: Support Programs and Services and the National Cancer Institute: Communicating With Your Health Care Team.
41. Are There Survivorship Programs I Can Join?

Survivorship programs are structured initiatives designed to support cancer patients as they transition from active treatment to life after cancer. These programs typically offer comprehensive services such as medical follow-up, symptom management, psychological counseling, nutrition guidance, and educational workshops (American Cancer Society: Survivorship Care Plans). Some are hospital-based, while others are available through community organizations or online platforms.
Patients who participate in survivorship programs often report improved quality of life, better management of late effects, and a stronger sense of community through support groups and educational sessions. Programs may also offer resources for navigating work or school reintegration, financial planning, and ongoing wellness initiatives such as exercise or mindfulness classes. Survivor experiences highlight the value of these services in addressing lingering challenges and fostering hope. Those who do not access survivorship programs sometimes feel isolated or unprepared for the unique issues that arise post-treatment. To find a program, ask your oncology team for referrals or visit the Cancer.Net: Survivorship page, which provides resources, directories, and guidance for optimizing life after cancer.
42. How Will I Know If I’m Having a Recurrence?

Recognizing the signs of cancer recurrence and understanding monitoring protocols are key concerns for many survivors. Recurrence can manifest as the return of original symptoms, new lumps or pain, unexplained weight loss, persistent fatigue, or other changes in health. Regular follow-up appointments, imaging scans, and blood tests are standard protocols for detecting recurrence early (National Cancer Institute: Follow-Up Care After Cancer Treatment).
Survivor advice emphasizes vigilance and self-advocacy. Many survivors keep detailed health diaries and promptly report any new or unusual symptoms to their healthcare team. Some recount how early detection of a recurrence—through careful monitoring and swift communication—led to successful second-line treatments or interventions. Others wish they had asked more about which symptoms to watch for, resulting in delayed care. Patients are encouraged to clarify with their care team which signs warrant immediate attention and to establish a clear follow-up schedule. For more on detecting recurrence and recommended monitoring, visit the American Cancer Society: Cancer Recurrence, which provides guidance on what to expect and how to stay proactive in survivorship.
43. What Are My Legal Rights as a Patient?
Cancer patients are protected by a range of legal rights designed to ensure autonomy, privacy, and fair treatment within the healthcare system. These rights include informed consent—meaning patients must receive clear explanations of their diagnosis, treatment options, and risks before agreeing to care. Privacy protections under the Health Insurance Portability and Accountability Act (HIPAA) ensure that medical records and personal information remain confidential (U.S. Department of Health & Human Services: HIPAA for Individuals).
Legal protections such as the Americans with Disabilities Act (ADA) and the Family and Medical Leave Act (FMLA) safeguard against discrimination at work or school and provide for reasonable accommodations and medical leave (American Cancer Society: Legal Rights of Cancer Patients). Patients also have the right to access their medical records, seek second opinions, and participate actively in care decisions. Understanding these rights helps patients advocate for themselves, resolve disputes, and address any mistreatment or denial of services. For further reading and legal resources specific to cancer care, visit Cancer.Net: Legal Resources.
44. Can I Participate in Advocacy or Research?

Many cancer patients and survivors find purpose and empowerment through advocacy and participation in research. Patient advocacy can include sharing your story, raising awareness about cancer issues, influencing healthcare policy, or supporting others through peer mentorship and community outreach. National organizations such as the American Cancer Society and National Coalition for Cancer Survivorship offer structured opportunities to get involved.
Research participation is another impactful avenue. Patients can contribute by enrolling in clinical trials, genetic studies, or patient-reported outcome projects, helping to advance scientific knowledge and improve future treatments. Many regret not asking about research opportunities earlier, as some studies have strict eligibility criteria or are only available at certain stages of care. For those interested, the Cancer.Net: Patient Advocacy and Involvement page outlines pathways to engagement. Meaningful participation not only benefits the broader cancer community but can also offer personal fulfillment and a sense of agency during and after treatment. Patients are encouraged to ask their care team about current advocacy and research initiatives relevant to their diagnosis and interests.
45. What Should I Know About Nutrition Supplements?

Nutrition supplements, including vitamins, minerals, herbs, and other dietary products, are commonly considered by cancer patients seeking to boost health or manage side effects. However, not all supplements are safe or effective, and some can interfere with cancer treatments. For example, antioxidant supplements like vitamins C and E may reduce the efficacy of chemotherapy or radiation, while certain herbal products such as St. John’s wort can alter the metabolism of cancer drugs, leading to harmful interactions (National Cancer Institute: Dietary Supplements in Cancer Care).
Evidence-based use of supplements means relying on recommendations from qualified healthcare professionals, such as oncology dietitians or pharmacists, rather than self-medicating or following unverified online advice. Patient cases have shown that unreported supplement use can result in unexpected side effects, drug interactions, or even reduced treatment effectiveness. Always inform your care team about any supplements you are considering or currently taking. For more guidance and safety information, visit the American Cancer Society: Dietary Supplements. Open discussion about supplements helps ensure your safety and the best possible outcomes during cancer treatment and recovery.
46. How Do I Manage Fatigue and Low Energy?

Cancer-related fatigue is a persistent, overwhelming sense of tiredness or exhaustion that is not relieved by rest and is distinct from normal tiredness. This fatigue can result from the cancer itself, treatments like chemotherapy or radiation, anemia, sleep disturbances, or emotional stress (National Cancer Institute: Fatigue in Cancer Patients). Unlike typical fatigue, cancer-related fatigue can interfere with daily activities, work, and quality of life, often lasting weeks or even months after treatment ends.
Effective management begins with identifying and addressing underlying causes, such as treating anemia or managing pain. Coping tips include pacing activities, prioritizing tasks, and allowing for regular rest breaks. Gentle exercise, such as walking or stretching, has been shown to help reduce fatigue for many patients. Adequate hydration, balanced nutrition, and maintaining good sleep hygiene also play important roles. Patients who openly discuss fatigue with their care team are more likely to receive supportive interventions, such as referrals to physical therapy or counseling. For additional information and self-care strategies, see the American Cancer Society: Fatigue. Proactive fatigue management improves both energy levels and overall well-being.
47. Will My Cancer Affect My Heart or Other Organs?

Some cancer treatments can have significant effects on vital organs, most notably the heart, liver, lungs, and kidneys. Certain chemotherapy agents and targeted therapies are associated with cardiotoxicity, which may manifest as heart failure, arrhythmias, or high blood pressure. Radiation aimed at the chest can also increase the risk of long-term cardiac complications (National Cancer Institute: Heart Health and Cancer Treatment).
Other organs may be impacted as well. For example, some drugs can cause kidney damage or lung inflammation, while liver toxicity is also a risk with specific medications. Patients with pre-existing conditions are at greater risk for these complications. Monitoring typically involves regular blood tests, imaging studies, and specialized assessments such as echocardiograms or pulmonary function tests. Early detection of organ problems allows for timely interventions, including medication adjustments, cardio-protective strategies, or referral to specialists.
Patients are encouraged to ask their healthcare team about organ-specific risks associated with their treatment plan and to report symptoms such as shortness of breath, chest pain, swelling, or jaundice. For more on protecting your heart and other organs during cancer care, visit the American Cancer Society: Heart Problems and Cancer Treatment.
48. Are There Lifestyle Changes That Could Help?

Evidence increasingly shows that certain lifestyle changes can support cancer treatment, improve recovery, and enhance long-term well-being. Interventions such as regular physical activity, a balanced diet rich in fruits and vegetables, maintaining a healthy weight, limiting alcohol, and quitting smoking are all associated with better outcomes during and after cancer care (American Cancer Society: Healthy Living During and After Cancer Treatment).
Real patient stories highlight remarkable transformations—some individuals report reduced fatigue, improved mood, and better tolerance of treatment after adopting exercise routines or making dietary changes. Others find that mindfulness practices and stress management techniques, such as yoga or meditation, help them cope with anxiety and improve sleep. Actionable changes include setting realistic, incremental goals; seeking guidance from oncology dietitians or physical therapists; and involving family members to create a supportive environment. Even small adjustments, like daily walks or swapping processed foods for whole grains, can make a meaningful difference. For more guidance on lifestyle modifications tailored to cancer patients, visit the Cancer.Net: Healthy Living After Cancer. Integrating healthy habits is a proactive way to regain control and foster resilience throughout the cancer journey.
49. What Should I Do If I Experience Financial Hardship?

Cancer treatment often brings substantial financial burdens, including costs for medications, hospital stays, transportation, childcare, and lost income. Many patients encounter “financial toxicity,” which can create stress and impact adherence to treatment. Fortunately, a variety of financial support options and assistance programs are available to help alleviate these pressures (American Cancer Society: Financial Support and Resources).
Patient experiences highlight the value of seeking help early—those who connect with hospital social workers or financial counselors often access grants, copay assistance, or charity care that significantly reduce out-of-pocket costs. Programs offered by national organizations, such as the Triage Cancer and CancerCare, provide direct financial aid, insurance guidance, and legal advocacy. Tips for accessing support include keeping thorough records, asking about payment plans, and researching prescription assistance for high-cost medications. For additional resources, the Cancer.Net: Financial Resources page offers a comprehensive directory. Being proactive about financial concerns ensures you can focus on healing without the added weight of undue financial stress.
50. What Resources Are Available for Survivors?

Survivorship brings its own set of challenges and opportunities, and a wide array of resources exists to support cancer survivors as they transition beyond treatment. Key resources include rehabilitation services to address lingering physical effects, mental health counseling for emotional recovery, nutritional guidance, and specialized clinics focused on long-term follow-up care (American Cancer Society: Survivorship).
Social reintegration support is also available, helping survivors return to work, school, or community activities. Many organizations offer peer mentoring, survivorship workshops, and online forums to foster connection and share advice. Access to these resources often begins with a survivorship care plan, developed in collaboration with your healthcare team, outlining recommended screenings, lifestyle strategies, and support services. Survivors can also explore local community groups, hospital-based programs, and national directories such as the Cancer.Net: Survivorship portal. Real-world experiences underscore the value of tapping into these networks—patients report improved confidence, reduced isolation, and greater empowerment in managing their health. Asking your care team about available resources ensures you receive comprehensive support for both your physical and emotional well-being as you move into survivorship.
Conclusion

Asking the right questions is critical for navigating a cancer diagnosis and ensuring the best possible outcomes. Many patients express regret over missed opportunities to understand their diagnosis, treatment options, side effects, and available support. Proactive communication with your healthcare team can help you advocate for your needs, reduce anxiety, and prevent avoidable complications. Regular screening and early intervention remain vital for improving prognosis and quality of life. For more guidance on empowering yourself as a patient, visit the Cancer.Net: Asking Your Health Care Team Questions and American Cancer Society: Cancer Screening Guidelines. Remember, no question is too small—your voice is essential to your care.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





