Silent Signs of Alopecia
According to the American Academy of Dermatology, alopecia impacts over 6.8 million people in the United States alone. This condition primarily affects the hair and skin, often leading to noticeable hair loss and changes in scalp health. However, early symptoms are frequently subtle and overlooked, resulting in many cases being detected only after significant hair loss has occurred. Recognizing these silent signs is crucial for early intervention and improved outcomes.
1. Subtle Widening of the Hair Part

One of the earliest and most easily overlooked indicators of alopecia is a gradual widening of the hair part. Many people notice that their central part appears slightly broader than before, but may dismiss this as a normal change due to styling, seasonal shedding, or aging. In reality, an expanding part is often a sign of diffuse hair thinning, which is most common in conditions like androgenetic alopecia and female pattern baldness.
This widening occurs as hair follicles miniaturize and produce thinner, weaker hairs before eventually ceasing growth. Over time, the density along the part line decreases, making the scalp more visible through the hair. It’s important to differentiate between occasional changes—such as those caused by tight hairstyles or temporary shedding—and persistent, progressive widening that does not resolve.
To monitor changes, experts recommend taking periodic photographs of your scalp or referencing previous images for comparison. If you notice a consistent pattern of widening, especially in conjunction with increased shedding, it may be worth consulting a dermatologist. For more information, visit the American Academy of Dermatology’s guide to female pattern hair loss.
2. Increased Hair Shedding in Shower or Brush

Noticing more hair than usual in your shower drain or brush can be an early silent sign of alopecia. Normally, most people lose between 50 to 100 hairs per day as part of the natural hair growth cycle, according to the Cleveland Clinic. However, when you begin to see clumps of hair or a sudden rise in shedding over several weeks, it may indicate a disruption in the hair growth cycle.
Excessive shedding can occur when a higher percentage of hairs enter the telogen (resting) phase simultaneously, a phenomenon known as telogen effluvium. This may be triggered by stress, hormonal changes, illness, or underlying autoimmune conditions like alopecia areata.
It’s important to monitor both the quantity and duration of increased hair loss. If shedding persists for more than a few weeks or you notice visible thinning, it’s advisable to seek medical evaluation. Early intervention can help determine the underlying cause and identify effective treatment options.
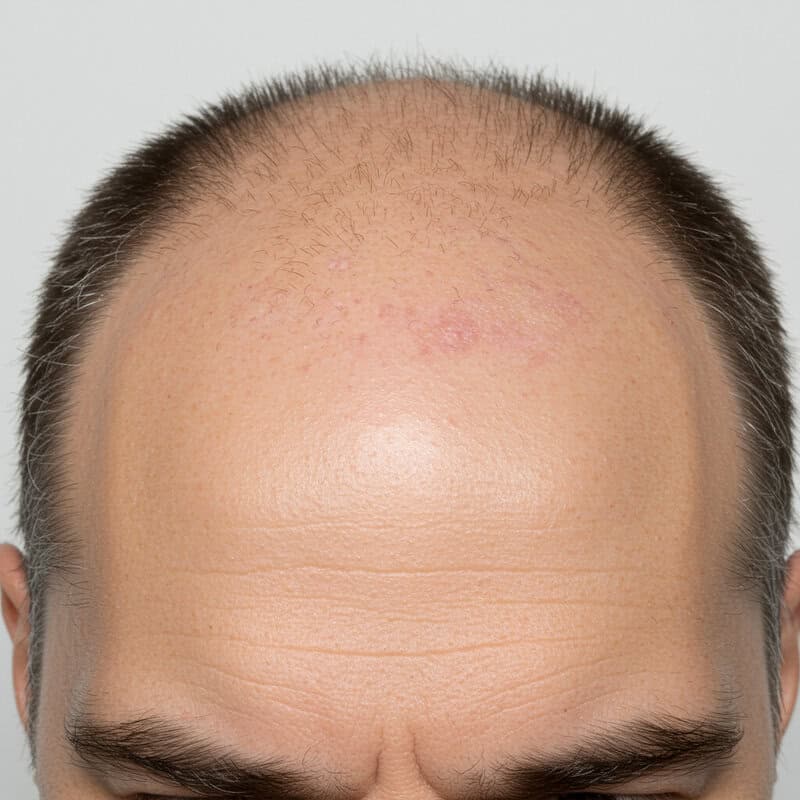
3. Receding Hairline at Temples

A gradual recession of the hairline at the temples is one of the defining early features of androgenetic alopecia, often referred to as male or female pattern hair loss. This process typically starts with subtle thinning and a slow retreat of the hairline on either side of the forehead, eventually forming a more pronounced “M” or “V” shape in men and a broader frontal area in women. Unlike a naturally high hairline, which remains stable throughout adulthood, a receding hairline caused by alopecia will progressively move backward and may be accompanied by thinning at the crown.
The recession occurs as hair follicles at the temples become increasingly sensitive to hormones such as dihydrotestosterone (DHT), leading to follicle miniaturization and shorter hair growth cycles. Over time, these follicles may stop producing hair entirely. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, early intervention is key to slowing progression and preserving existing hair.
If you notice that your hairline is changing shape at the temples or that it is receding more than in family photographs, it’s advisable to consult with a dermatologist for assessment and advice on management options.
4. Noticeably Thinner Ponytail

One of the most tangible ways many people detect early hair loss is by noticing a thinner ponytail. Over time, as diffuse thinning progresses, the volume of hair that can be gathered into a ponytail significantly decreases. This reduction is often subtle at first—hair ties may need to be wrapped an extra time, or the ponytail may feel less full to the touch. For many individuals, this physical change is more noticeable than visual thinning, especially when viewed in the mirror.
Diffuse thinning affects the entire scalp, not just the part or hairline, which is why ponytail volume is such a reliable indicator. Women experiencing female pattern hair loss or telogen effluvium may observe that their ponytail diameter is much less than it was just months or years before. Real-life examples frequently include needing to downsize hairbands or noticing that styles requiring thickness are harder to achieve.
If you find your ponytail is consistently thinner without obvious causes like recent haircuts, chemical treatments, or tight hairstyles, it could be a sign of underlying alopecia. Early recognition and intervention can improve treatment outcomes.
5. Sudden Appearance of Patchy Bald Spots

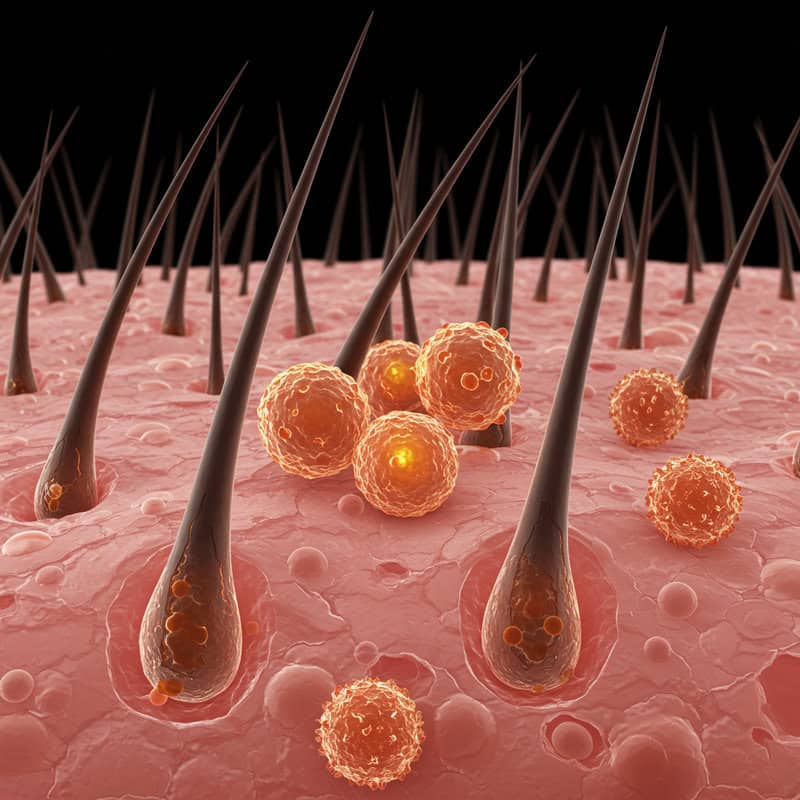
The sudden emergence of small, round bald spots on the scalp or other areas of the body is a hallmark of alopecia areata, a type of hair loss caused by an autoimmune reaction. In this condition, the immune system mistakenly targets healthy hair follicles, causing them to shrink and abruptly halt hair production. These bald patches are usually smooth, devoid of inflammation or scaling, and can appear in clusters or as isolated spots.
Early recognition is crucial, as alopecia areata can progress rapidly or even affect the entire scalp (alopecia totalis). Practical cues for spotting this form of hair loss include finding distinct, coin-sized areas of missing hair—often noticed by a hairdresser or when styling hair. Sometimes, tingling, mild discomfort, or itching may precede the visible loss.
If you observe patchy bald spots, it’s important to seek professional evaluation promptly. A dermatologist can confirm the diagnosis and discuss treatment options, which may include corticosteroid injections or topical immunotherapy. For more details on symptoms and management, visit the American Academy of Dermatology: Alopecia Areata.
6. Tingling or Itching Before Hair Loss
A subtle but telling sign that often precedes visible hair loss is the sensation of tingling, itching, or burning on the scalp. These sensations, sometimes referred to as “trichodynia” or “pruritus,” can indicate underlying inflammation or immune activity targeting the hair follicles. In conditions like alopecia areata or other inflammatory scalp disorders, the body’s immune response may attack the follicles, producing discomfort before any hair actually falls out.
Such scalp sensations tend to be mild and can easily be dismissed as dryness, product buildup, or a reaction to new shampoos. However, when tingling or itching is persistent and localized—especially if followed by increased hair shedding or patchy bald spots—it may signal the early phases of alopecia. According to the American Academy of Dermatology, inflammation around the follicles can disrupt the normal hair growth cycle, eventually leading to hair loss.
If you experience ongoing scalp sensations without an obvious cause, it is wise to monitor for other signs of hair thinning or loss and consult a dermatologist for evaluation and management.
7. Changes in Eyebrow or Eyelash Density

Alopecia is not limited to scalp hair; it can also cause thinning or loss of eyebrows and eyelashes. This is particularly true in autoimmune forms like alopecia areata, where the immune system targets hair follicles anywhere on the body. Sometimes, the first sign of alopecia may be the gradual disappearance of the outer third of the eyebrows or noticeable gaps in eyelash rows. These changes are often subtle and can be mistaken for over-plucking, cosmetic irritation, or natural aging.
Real-world cases highlight how individuals may notice sparse brows when applying makeup or see excessive lashes on a pillow or makeup remover pad. In some instances, both brows and lashes thin simultaneously, while in others only one area is affected. According to the American Academy of Dermatology, alopecia areata can occur in “patches” on facial hair just as it does on the scalp.
To monitor for changes, pay attention to the shape and density of your brows and lashes over time. Documenting their appearance with photos can be helpful for noticing gradual thinning and discussing any concerns with a dermatologist.
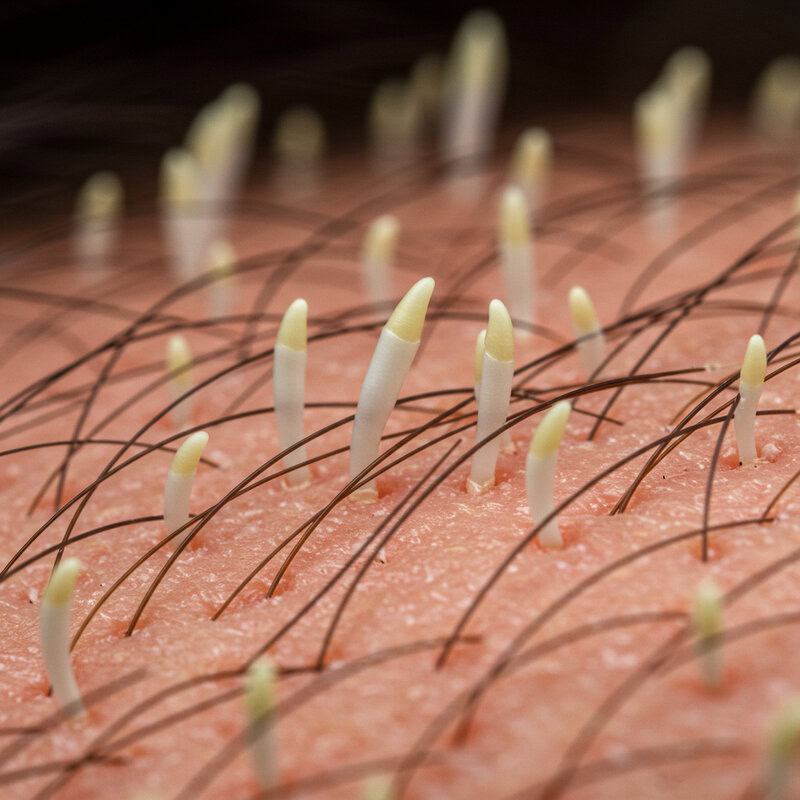
8. Short, Broken ‘Exclamation Mark’ Hairs
A distinctive but often overlooked sign of alopecia areata is the presence of short, broken hairs known as “exclamation mark” hairs. These hairs are so named because they are narrower and weaker at the base near the scalp, often appearing darker and thicker at the tip, resembling an exclamation mark. According to the DermNet NZ, these hairs are typically found at the edges of bald patches and are a key diagnostic clue for dermatologists.
Exclamation mark hairs form as the result of inflammation and immune attacks on the hair follicle, causing the growing hair shaft to narrow and break off easily. This weakening of the hair leads to stubble-like, tapered hairs that can be seen upon close inspection of the scalp. Their presence indicates active disease and ongoing follicular damage in alopecia areata.
To identify exclamation mark hairs, look closely at the border of bald or thinning areas for very short, broken hairs that are thinner at the scalp and thicker toward the ends. If you notice these unusual hairs, it’s important to bring them to the attention of a dermatologist for accurate diagnosis and timely treatment. For more information, visit American Academy of Dermatology: Alopecia Areata.
9. Increased Scalp Sunburn

An often-overlooked warning sign of hair thinning is an increase in scalp sunburn. As hair density decreases, the scalp becomes more exposed to ultraviolet (UV) rays, making it vulnerable to sunburn even after short periods outdoors. This heightened sensitivity is a direct result of hair’s natural function as a protective barrier for the skin on the head. People experiencing alopecia or diffuse thinning may find themselves unexpectedly dealing with redness, tenderness, or peeling on areas of the scalp that were previously covered by hair.
Examples include noticing a pink or tender scalp after spending time outside, even on cloudy days, or developing flaking and itching in areas where hair coverage has decreased. According to the Skin Cancer Foundation, the scalp is one of the most common sites for skin cancers caused by UV exposure, particularly when hair is thin or absent.
To prevent scalp sunburn, experts recommend wearing a hat, using a broad-spectrum sunscreen formulated for the scalp, and seeking shade during peak hours. Paying attention to increased scalp sunburn may be an early cue to underlying hair loss.
10. Slower Hair Regrowth After Shedding
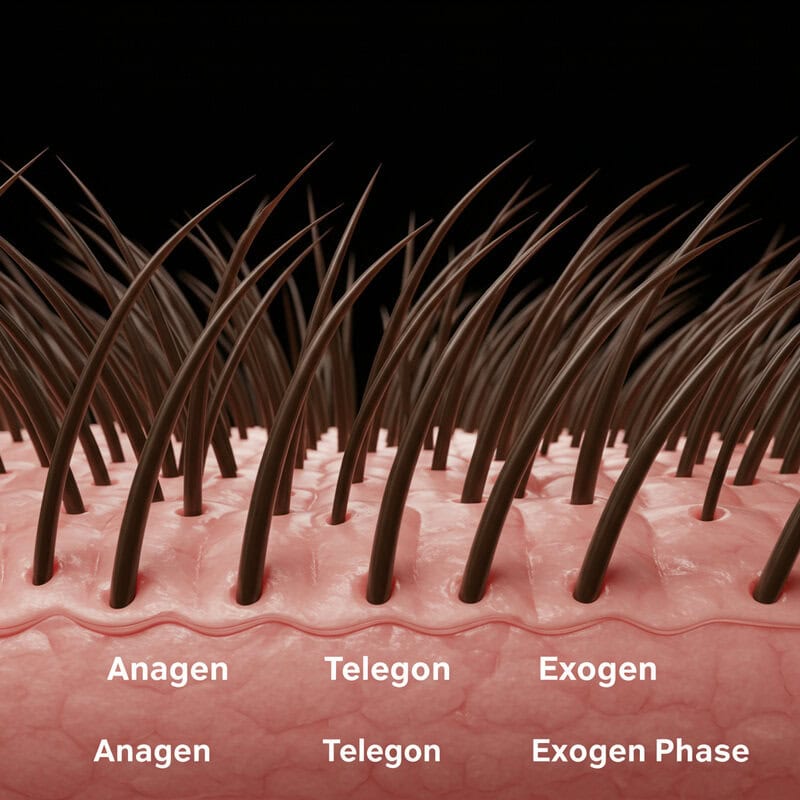
A subtle but significant sign of underlying alopecia is slower hair regrowth following a period of shedding. Normally, hair follows a cycle of growth (anagen), rest (telogen), and shedding (exogen), with most hair quickly regrowing after fallout. However, alopecia can disrupt this cycle, resulting in sparse or delayed regrowth. People may notice that areas affected by shedding remain thin or that new hairs appear finer and take much longer to reach their previous length.
Disruption of the hair growth cycle can occur in conditions such as alopecia areata or telogen effluvium, where inflammation or stress causes a greater proportion of follicles to enter the resting phase. This means fewer follicles are actively producing new hair, leading to prolonged periods of visible thinning. According to the American Academy of Dermatology, healthy regrowth should be noticeable within several months of increased shedding.
If you observe that your hair is not filling in as it once did, or that regrowth is patchy and slow, it may be time to consult a dermatologist. Early attention to these changes can help identify alopecia and guide effective treatment.
11. Excessive Hair on Pillow

Waking up to find an unusual amount of hair on your pillow can be an unsettling experience and may signal an early stage of alopecia. While it is normal to shed some hair overnight as part of the natural hair growth cycle, the amount typically remains minimal—usually just a few strands. Noticing clumps or a noticeably greater number of hairs, however, can indicate that more hair is entering the shedding (telogen) phase or that follicles are no longer anchoring hair as securely as before.
This type of overnight shedding is commonly seen in conditions such as telogen effluvium or alopecia areata, where hair may shed rapidly and unexpectedly. It’s important to distinguish between normal hair loss and excessive shedding: if you consistently find more than a dozen hairs on your pillow each morning or observe a sudden spike following illness, stress, or medication changes, this should not be ignored.
Persistent overnight shedding that results in visible thinning or bald spots warrants a visit to a dermatologist. Early evaluation can help uncover the underlying cause and allow for timely management. For more information, see the American Academy of Dermatology’s guide to hair shedding.
12. Loss of Body Hair

Alopecia doesn’t just affect the scalp—it can also lead to loss of body hair, including on the arms, legs, underarms, chest, and even pubic area. This is most commonly seen in advanced cases of alopecia areata, particularly in its more extensive forms: alopecia totalis (loss of all scalp hair) and alopecia universalis (loss of all body hair). The immune system’s attack on hair follicles can cause smooth, hairless patches or complete absence of hair in areas that previously had normal growth.
Real-life stories often highlight the emotional and practical challenges faced by those experiencing widespread hair loss. For example, some individuals notice the sudden disappearance of arm or leg hair, while others report losing eyelashes, eyebrows, or even nasal hair—sometimes realizing it only after increased sensitivity or dryness. According to the American Academy of Dermatology, these patterns can help differentiate alopecia areata from other types of hair loss.
If you observe unexplained or rapid loss of body hair, it’s important to document which areas are affected and consult a dermatologist. Early recognition can guide diagnosis and inform the best treatment approach.
13. Brittle or Fragile Hair Texture

A noticeable shift toward brittle or fragile hair texture can serve as an early warning sign of underlying scalp health issues, including alopecia. Healthy hair shafts are resilient, flexible, and have a smooth cuticle layer that protects against breakage. When the scalp or hair follicles experience inflammation, reduced blood flow, or autoimmune attack—as seen in various forms of alopecia—the quality of hair produced can deteriorate, resulting in hair that is dry, breaks easily, or appears frizzy and lifeless.
Examples include increased hair breakage during brushing or styling, a rough or straw-like feel to individual strands, and split ends that occur even with regular trims. According to the American Academy of Dermatology, hair affected by alopecia may not only be thinner but also more prone to snapping due to weakened structure at the root. Conditions such as alopecia areata or scarring alopecias can lead to these texture changes long before significant hair loss becomes visible.
If you notice your hair is suddenly more fragile, breaking off with minimal tension, or has lost its usual shine, it’s important to assess your scalp health and consider seeking advice from a dermatologist.
14. Visible Scalp Through Hair

A common yet often subtle sign of progressive hair thinning is the increased visibility of the scalp through the hair. This phenomenon occurs when the density of hair follicles decreases, allowing more of the underlying scalp skin to be seen beneath what appears to be a full head of hair. While some scalp visibility is normal—especially under bright lights or with certain hairstyles—an increase over time may indicate the onset of alopecia or diffuse thinning.
Comparisons with old photographs can be particularly helpful for tracking changes. For example, you might notice that your part line appears wider, the crown is more exposed, or the overall hair coverage looks less dense in recent images. According to the American Academy of Dermatology, this sign is especially common in female pattern hair loss, where thinning is most pronounced at the top of the scalp.
To monitor for increased scalp visibility, use consistent lighting and angles when taking pictures of your hair, and compare them periodically. If you observe persistent or worsening scalp show-through, consult a dermatologist to explore potential causes and discuss early intervention strategies.
15. Unusual Hair Patterns or Growth Directions
Changes in the usual direction or pattern of hair growth can be a subtle but telling sign of underlying alopecia. Normally, hair follows consistent growth patterns determined by the orientation of follicles. However, when hair follicles are affected by inflammation, scarring, or autoimmune processes, as seen in various forms of alopecia, the regrowth may emerge at odd angles or in unexpected directions. This can result in cowlicks appearing in new places, hair standing up in areas that were previously flat, or an inconsistent texture when styling.
Patient experiences often include noticing that hair near a thinning patch starts to swirl, lay differently, or become unruly despite using the same grooming habits and products. In some cases, regrowing hair in a patch of alopecia areata may come in finer, lighter, or curlier than the surrounding hair, further highlighting the change. According to the DermNet NZ, these altered growth patterns can be among the earliest signs of follicular disruption.
If you observe new or persistent changes in the way your hair grows or lies, consider documenting the changes and seeking advice from a dermatologist to determine if they may be linked to early-stage alopecia.
16. Persistent Flaking or Scalp Inflammation
Persistent flaking, redness, or inflammation of the scalp can be more than just a cosmetic nuisance—it may signal underlying conditions that increase the risk of hair loss. Chronic scalp irritation, often due to seborrheic dermatitis, psoriasis, or inflammatory disorders, can disrupt the hair growth cycle and damage follicles over time. The ongoing inflammation weakens the environment needed for healthy hair, potentially leading to scarring alopecia or accelerating other types of hair thinning.
According to the American Academy of Dermatology, untreated or persistent scalp inflammation can manifest as excessive dandruff, itching, burning, or patchy redness. In severe cases, it can create an inhospitable environment for hair regrowth, causing irreversible follicle damage.
To monitor your scalp health, periodically check for flaking that doesn’t respond to over-the-counter shampoos, redness that persists beyond a few days, or areas of tenderness. Take clear photos under natural light to track changes and bring them to your dermatologist if symptoms persist. Early intervention with medicated treatments or lifestyle adjustments can help control inflammation and reduce the risk of associated hair loss.
17. Changes in Hair Color or Pigmentation

Unexpected changes in hair color or pigmentation can sometimes serve as a subtle indicator of underlying follicle health issues, including early stages of alopecia. Healthy hair follicles produce pigment (melanin), which gives hair its color. When follicles are affected by inflammation, autoimmune activity, or other scalp disorders, pigment production may diminish, resulting in hair that grows back lighter, gray, or even white in affected areas. This is particularly noticeable in conditions such as alopecia areata, where regrowth after a bald patch may appear colorless or significantly lighter than surrounding hair.
Real-world examples include individuals who notice white or gray hairs sprouting within a newly regrown patch of hair, or sections of hair that suddenly lack pigment after a period of shedding or scalp irritation. According to the American Academy of Dermatology, these pigment changes are not just cosmetic—they can indicate disrupted follicle function and ongoing immune response at the hair root.
If you observe areas of hair regrowth that are lighter, gray, or white and these changes do not fit your normal aging process, it may be wise to consult with a dermatologist for further evaluation and monitoring.
18. Slower Nail Growth or Nail Pitting

An often overlooked but telling sign of underlying alopecia is a change in the condition of the nails, particularly slower nail growth or nail pitting. Nails and hair both originate from similar types of cells—keratinocytes—so disruptions in the body’s immune system or inflammation can impact both structures. In conditions such as alopecia areata, up to 20% of patients may experience nail symptoms, including tiny depressions (pitting), ridges, thinning, or white spots.
Real-world examples include individuals noticing that their nails are growing more slowly than usual, developing a rough, sandpaper-like texture, or becoming brittle and prone to splitting. According to the American Academy of Dermatology, nail pitting can even precede visible hair loss, serving as an early warning sign of autoimmune activity.
If you observe persistent nail changes such as pitting, slower growth, or unusual brittleness—particularly in combination with hair thinning—it is recommended to consult a dermatologist. Early detection can help guide a comprehensive approach to diagnosing and managing alopecia and related autoimmune conditions.
19. Increased Sensitivity to Hair Products

An often subtle sign of changing scalp health—and potential underlying alopecia—is increased sensitivity or irritation when using routine hair products. Scalp inflammation, thinning hair, and disrupted follicle health can compromise the skin’s natural barrier, making it more reactive to ingredients found in shampoos, conditioners, dyes, or styling agents. People may experience itching, burning, redness, or flaking after using products that previously caused no issues.
Consumer experiences often include suddenly developing allergic-like reactions, noticing stinging with hair dyes, or finding that mild products now trigger discomfort or dryness. According to the American Academy of Dermatology, this heightened reactivity can result from the scalp’s increased vulnerability as hair density decreases and protective oils are reduced.
If you find yourself needing to switch hair products frequently due to irritation, or if your scalp reacts to gentle formulas, it may be a sign of underlying inflammation or early alopecia. Monitoring which products trigger symptoms and noting new or worsening sensitivities can help guide conversations with a dermatologist, who can assess for scalp disorders or recommend suitable hair care routines.
20. Pain or Burning Sensation in Scalp
Experiencing a painful or burning sensation in the scalp—sometimes referred to as “scalp dysesthesia” or “trichodynia”—can be an early indicator of underlying inflammation that may precede visible hair loss. This discomfort is usually due to the activation of nerve endings in the scalp as a result of inflammatory processes targeting the hair follicles. In conditions such as alopecia areata or certain scarring alopecias, the immune system’s attack can produce localized pain, sensitivity, or a burning feeling even before hair begins to shed.
Patients often describe this sensation as persistent tenderness, tingling, or a “sunburned” feeling without any obvious external cause. According to the American Academy of Dermatology, these symptoms may be overlooked or mistaken for unrelated scalp conditions such as dermatitis.
If you notice unexplained scalp pain or burning, especially if it coincides with other silent signs like increased shedding or redness, it’s important to document your symptoms and seek medical evaluation. Early recognition of these sensations can help identify inflammation and prompt timely intervention before significant hair loss occurs.
21. Unexplained Hair Loss After Illness

Experiencing unexplained hair loss following an illness is a well-documented phenomenon, often linked to a condition known as telogen effluvium. After physical or emotional stress—such as high fever, surgery, or severe infection—the body can shift a large number of hair follicles from the growth (anagen) phase into the shedding (telogen) phase, resulting in noticeable hair loss two to three months later. This process is temporary but can be distressing, especially when large clumps of hair are lost with no obvious cause.
The COVID-19 pandemic provided numerous real-world examples, with many individuals reporting significant hair shedding weeks to months after recovering from the virus. According to the American Academy of Dermatology, this type of hair loss is usually reversible, and normal growth typically resumes within six to nine months.
If you notice sudden, diffuse hair shedding after recovering from illness, it’s important to avoid panic. Monitor the amount and duration of loss, and consult a dermatologist if shedding persists beyond several months or is accompanied by other concerning symptoms.
22. Increased Hair Loss During Stressful Periods
Heightened hair loss during times of significant stress is a common but frequently misunderstood sign that can indicate the onset of telogen effluvium or other forms of alopecia. Stressful events—such as job changes, bereavement, exams, or personal upheaval—can disrupt the normal hair growth cycle, prompting more follicles to enter the shedding (telogen) phase. According to the American Academy of Dermatology, this process typically results in noticeable hair loss two to three months after the stressful event, making the connection less obvious.
Real-world examples include increased hair on pillows, in the shower, or when brushing, often with no other changes to diet or health. Some people may notice their hair thinning uniformly rather than in patches, which can make detection challenging. Stress-induced hair loss is generally temporary, but chronic or severe stress can prolong or worsen the condition.
To detect patterns, keep a journal of significant life events and any changes in hair shedding. If you consistently observe increased hair loss following periods of stress, consider discussing your symptoms with a dermatologist or healthcare provider for guidance on management and prevention strategies. For more on stress and hair loss, visit Harvard Health Publishing.
23. Hair Loss Along Scalp Margins

Hair loss along the scalp margins, particularly at the hairline, temples, and nape of the neck, is a distinct sign often associated with conditions like traction alopecia. This type of alopecia is caused by prolonged tension on hair follicles due to tight hairstyles such as braids, ponytails, weaves, or extensions. Over time, the constant pulling weakens the follicles, leading to thinning and, eventually, permanent loss of hair along the edges if not addressed early.
Individuals may notice a gradual recession of the hairline, thinning edges, or even small bumps or redness along the affected areas. According to the American Academy of Dermatology, early intervention is crucial for halting and potentially reversing this type of hair loss.
To prevent edge hair loss, alternate hairstyles frequently, avoid excessive tension, and give your scalp breaks between protective styles. If you detect thinning or irritation along your scalp margins, consider loosening hairstyles and seeking advice from a dermatologist. Early recognition and gentle care can help protect the delicate follicles along your hairline and nape.
24. Sudden Loss of Hair After Styling Changes

A sudden increase in hair loss following changes in hairstyling routines can be a warning sign of mechanical or chemical trauma to the hair and scalp. New hairstyles that place increased tension on the hair—such as tight ponytails, braids, buns, or extensions—can cause traction alopecia, where persistent pulling leads to follicle damage and shedding. Similarly, chemical treatments like coloring, straightening, or perming may weaken the hair shaft and contribute to breakage and fallout.
Practical examples include noticing excessive hair left on brushes, in the shower, or on clothing shortly after adopting a new style or treatment. Some individuals report that their hair feels more fragile or appears thinner at the roots and along parts where styling was most intense. According to the American Academy of Dermatology, repeated exposure to harsh styling practices can result in both temporary and permanent hair loss if not addressed.
To minimize risk, avoid overly tight hairstyles, limit the frequency of chemical treatments, and ensure proper scalp care after any styling changes. If sudden hair loss occurs, promptly discontinue the new practice and consult a dermatologist to prevent further damage and discuss restorative options.
25. Delayed Hair Growth After Chemotherapy

For many individuals, hair regrowth after chemotherapy begins within a few weeks to months of completing treatment. However, a subset of patients experience prolonged or incomplete hair regrowth, a condition known as persistent chemotherapy-induced alopecia. According to studies cited by the American Cancer Society, while 65%-85% of patients see full regrowth within six months, up to 10% may face ongoing thinning or patchy hair loss a year or more after therapy.
Delayed regrowth can be particularly distressing for cancer survivors, as it may affect self-esteem and signal lingering follicular damage. The risk of persistent alopecia is higher with certain chemotherapy drugs such as taxanes or anthracyclines. Real-world reports include individuals noting that their hair comes back finer, sparser, or fails to return to its previous density and texture.
If you experience delayed or minimal hair regrowth after chemotherapy, consult your oncology team or a dermatologist. They may recommend topical treatments or supportive therapies to stimulate follicles. For more on managing hair loss after cancer treatment, visit the American Society of Clinical Oncology.
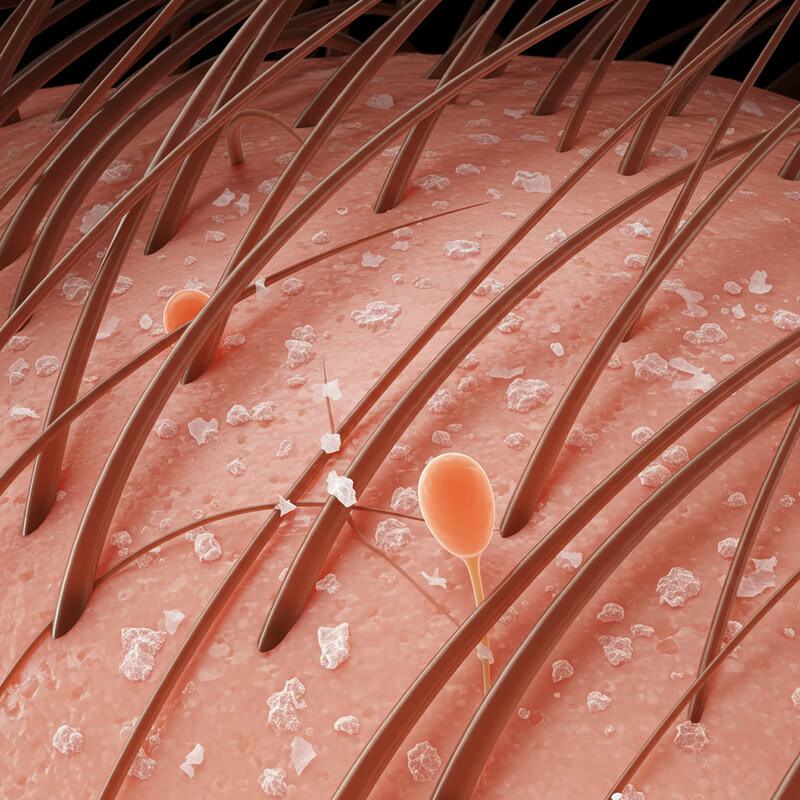
26. Miniaturization of Hair Shafts

Miniaturization of hair shafts refers to the process by which individual hairs become progressively thinner and shorter over time, a hallmark of androgenetic alopecia and other chronic hair loss conditions. Under magnification, miniaturized hairs appear much finer than surrounding healthy hairs, often resembling “peach fuzz.” This occurs as hair follicles shrink due to the effects of hormones (such as dihydrotestosterone, or DHT) or ongoing inflammation, shortening the growth phase (anagen) and producing weaker, less pigmented strands.
According to the American Academy of Dermatology, miniaturization is a key diagnostic feature in pattern hair loss. Patients may notice their hair feels less dense, and scalp visibility increases even though shedding rates appear unchanged. Dermatologists often use a dermatoscope to assess miniaturization, noting a mix of thick and thin hairs in the affected area—a pattern called “anisotrichosis.”
If you suspect your hair is becoming finer or patchier, or notice a high proportion of thin, wispy hairs, consider scheduling an evaluation. Early recognition of miniaturization can help guide treatment choices and improve the chances of preserving healthy follicles. Learn more from DermNet NZ.
27. Loss of ‘Baby Hairs’ Along Hairline

The gradual loss of fine ‘baby hairs’ along the hairline is an often-overlooked sign of early alopecia. These delicate, wispy hairs—technically known as vellus hairs—normally frame the edges of the scalp and help create a natural, soft border. Their disappearance may signal that hair follicles at the frontal margins are becoming inactive or miniaturized, which can be an early indicator of conditions like androgenetic alopecia or traction alopecia.
According to the American Academy of Dermatology, the loss of vellus hairs is often one of the first visible changes in the progression of pattern hair loss, preceding noticeable thinning or receding hairlines. People may observe that their hairline appears sharper or more defined, with fewer soft hairs to mask the transition from scalp to terminal hair. This change can be particularly apparent when styling hair or applying makeup.
Monitoring the presence of baby hairs over time—using photos, mirrors, or input from a stylist—can aid in early detection of alopecia. If you notice a reduction in fine hairs or a more pronounced hairline, consult a dermatologist for assessment and potential early intervention. For more information, visit DermNet NZ.
28. Increased Sensitivity to Temperature on Scalp

An often overlooked yet telling sign of hair thinning or early alopecia is increased sensitivity to temperature changes on the scalp. As hair density decreases, the insulating barrier provided by the hair is diminished, leaving the scalp more exposed to heat, cold, wind, and sunlight. Many individuals report feeling chilly on the scalp during colder months or experiencing discomfort and heat more acutely in the sun—sensations they may not have noticed before hair loss began.
Practical cues include feeling a cold draft on the scalp indoors, needing to wear hats more frequently, or experiencing mild scalp burns after only brief sun exposure. According to the Skin Cancer Foundation, an exposed scalp is at increased risk for sunburn, which can further damage sensitive follicles and skin. These temperature sensations may be most prominent in areas where thinning is greatest, such as the crown, part line, or hairline.
If you notice new or heightened sensitivity to temperature on your scalp—especially in conjunction with visible thinning or other silent signs—it may be an early indicator of alopecia. Monitoring these sensations can help prompt timely evaluation and protective measures.
29. Moth-Eaten or Irregular Bald Patches
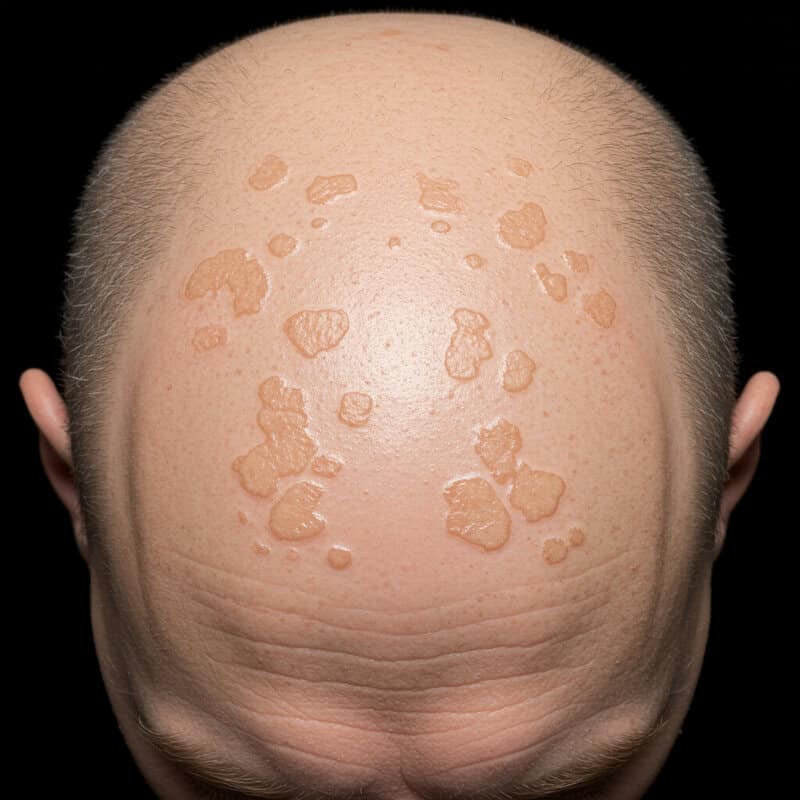
The appearance of moth-eaten or irregular bald patches on the scalp is a distinctive sign of certain types of alopecia, particularly syphilitic alopecia and advanced cases of alopecia areata. Unlike the smooth, round bald spots typically seen in classic alopecia areata, these patches are uneven, scattered, and may vary significantly in size and shape, giving the scalp a “moth-eaten” appearance. This pattern of hair loss can make the scalp look as if it has been randomly dotted with bare areas, some merging together while others remain isolated.
Such irregular patches may develop rapidly or gradually, sometimes accompanied by other symptoms such as redness, inflammation, or mild scaling. According to the American Academy of Dermatology, moth-eaten alopecia requires prompt evaluation, as it may point to underlying systemic disease, such as secondary syphilis, or signal a severe autoimmune process.
If you observe patchy, irregular bald areas rather than uniform thinning or round spots, seek medical attention for proper diagnosis. Early intervention can help identify the cause and guide the best treatment approach. Regular scalp checks and photographs can assist in tracking the development of these patches.
30. Loss of Hair in Circular Patterns

One of the most recognizable presentations of alopecia areata is the loss of hair in distinct circular or oval patches. These round bald spots are typically smooth and completely hairless, often appearing suddenly on the scalp or other hair-bearing areas. The immune system mistakenly attacks healthy hair follicles, leading to a sharply demarcated area of hair loss while the surrounding hair remains intact. This pattern is a hallmark of alopecia areata and helps distinguish it from other forms of diffuse or patterned hair loss.
Identification tips include looking for patches that are uniform in shape and size, usually ranging from the size of a coin to much larger areas as the condition progresses. These spots may be noticed by the individual, a hairdresser, or family members during styling or grooming. According to the American Academy of Dermatology, regrowth in these patches may initially appear as fine, light-colored “peach fuzz” before normal pigmentation returns.
If you detect sudden, round bald patches, it is important to seek evaluation from a dermatologist. Early diagnosis increases the likelihood of effective management and may help prevent further progression of hair loss.
31. Unusual Hair Loss in Children

While hair loss is often associated with adults, unusual hair loss in children can be an important indicator of pediatric alopecia or other underlying health conditions. Unlike adult patterns, hair loss in children commonly presents as sudden, patchy bald spots (often due to alopecia areata), diffuse thinning, or even broken hairs and scaling if fungal infections like tinea capitis are present. Children may also develop traction alopecia from tight hairstyles or trichotillomania, a compulsive hair-pulling disorder.
Pediatric alopecia often lacks the receding hairlines or gradual thinning seen in adults. Instead, parents might notice smooth, hairless patches that appear overnight or small areas where the hair breaks off close to the scalp. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, early intervention is crucial because untreated hair loss in children can affect self-esteem and social development.
If a child develops unusual hair loss, prompt medical evaluation is recommended. Pediatric cases may require different diagnostic tests and treatment strategies compared to adults. For more information, see the Cincinnati Children’s Hospital guide to alopecia areata.
32. Loss of Pubic or Axillary Hair

The loss of pubic or axillary (underarm) hair is a less-discussed but significant sign that can indicate systemic or advanced types of alopecia, such as alopecia universalis or other underlying medical conditions. Unlike scalp hair loss, which may be more readily noticed and discussed, changes in body hair—including the pubic and underarm regions—are often overlooked or attributed to normal aging or grooming habits. However, a sudden or progressive reduction in these areas can have important diagnostic implications.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, extensive forms of alopecia areata can result in hair loss across the entire body, including pubic and axillary regions. Real-world cases have shown that some individuals first notice thinning or patchy loss in these areas before or alongside scalp symptoms. In rare cases, loss in these regions may also point to hormonal imbalances, endocrine disorders, or autoimmune diseases.
If you observe unexplained loss of pubic or underarm hair—especially if accompanied by changes to scalp, eyebrow, or eyelash hair—it is important to seek medical advice. These changes can provide valuable clues for accurate diagnosis and tailored treatment. For further reading, visit American Academy of Dermatology: Alopecia Areata.
33. Hair Loss Following Rapid Weight Loss

A sudden or significant loss of hair following rapid weight loss is a well-documented manifestation of telogen effluvium, a condition where a large number of hair follicles enter the shedding phase simultaneously. This phenomenon is often triggered by nutritional deficiencies that can result from crash diets, extreme calorie restriction, or unbalanced eating patterns. Essential nutrients such as iron, protein, zinc, and biotin are all critical for healthy hair growth, and deficiencies can disrupt the natural hair cycle.
Real-life examples include individuals who pursue popular diet trends—such as very low-calorie ketogenic, juice cleanses, or fasting regimens—who then notice increased hair shedding two to three months after significant weight loss. According to the American Academy of Dermatology, telogen effluvium is typically reversible if normal nutrition is restored, but chronic deficiencies can lead to persistent thinning.
If you experience noticeable hair loss after rapid weight loss, review your diet to ensure it provides adequate nutrients. Consulting a healthcare provider or registered dietitian can help address deficiencies and restore hair health. For more information, visit the National Institutes of Health on diet and hair loss.
34. Loss of Hair Around Scars

Loss of hair around scars is a key feature of scarring alopecia, also known as cicatricial alopecia. This type of hair loss occurs when inflammation or injury destroys hair follicles and replaces them with scar tissue, resulting in permanent bald patches. Scarring alopecia can develop after trauma, burns, surgical incisions, or as a result of chronic inflammatory scalp conditions such as lichen planopilaris or discoid lupus erythematosus. The affected areas are often smooth, shiny, and may appear lighter or darker than the surrounding skin.
According to the American Academy of Dermatology, once a scar forms and follicles are replaced by fibrous tissue, regrowth in that region is not possible. Patients may first notice thinning or loss of hair bordering a scar, which gradually expands as the underlying condition progresses. In some cases, the skin may become tender, itchy, or show signs of redness and scaling before visible hair loss occurs.
If you observe progressive hair loss around old or new scars, seek prompt evaluation by a dermatologist. Early diagnosis and treatment of underlying inflammation can help limit further follicular destruction and preserve remaining hair. More on this topic is available at DermNet NZ: Cicatricial Alopecia.
35. Persistent Redness or Soreness of Scalp

Persistent redness or soreness of the scalp can be an important sign of underlying inflammatory alopecia, such as lichen planopilaris, discoid lupus erythematosus, or central centrifugal cicatricial alopecia. These chronic conditions trigger an inflammatory response in the scalp, damaging hair follicles and leading to progressive hair thinning or permanent loss. According to the American Academy of Dermatology, scalp redness, tenderness, and soreness often precede visible hair loss and are key warning signs that should not be ignored.
Self-check tips include gently parting your hair in several places under good lighting and looking for areas of persistent redness, swelling, or tenderness that do not resolve with regular washing or over-the-counter treatments. You may also notice a warm sensation, increased sensitivity to touch, or discomfort when brushing or styling.
If scalp redness or soreness is ongoing, especially when accompanied by flaking, pustules, or visible thinning, it is important to seek prompt evaluation by a dermatologist. Early intervention is crucial to reducing inflammation, preserving hair follicles, and preventing irreversible scarring alopecia. More information is available at DermNet NZ: Scarring Alopecia Overview.
36. Sudden Loss of Facial Hair in Men

A sudden and noticeable loss of facial hair in men, particularly in the beard area, is commonly referred to as alopecia barbae. This condition is a specific manifestation of alopecia areata, in which the immune system mistakenly targets hair follicles in the beard region, resulting in smooth, round, or oval bald patches. According to the American Academy of Dermatology, alopecia barbae can develop rapidly, sometimes over the course of just a few days or weeks.
The exact cause is not fully understood, but genetic predisposition, autoimmune factors, and emotional or physical stress are believed to play a role. Early signs include increased shedding when stroking the beard, finding bald spots after shaving, or noticing uneven beard growth. The affected skin is typically smooth and may be slightly lighter in color than surrounding areas, without signs of scarring or inflammation.
Early detection of alopecia barbae is important for effective management. Men who observe sudden patchy beard loss should consult a dermatologist promptly, as early intervention can sometimes encourage regrowth and help manage the underlying autoimmune response. For more information, visit DermNet NZ: Alopecia Barbae.
37. Development of Soft, White Downy Hairs
The development of soft, white downy hairs, also known as vellus hairs, is a notable sign in the progression and possible recovery from alopecia. Vellus hairs are fine, lightly pigmented or non-pigmented hairs that typically appear in areas where terminal (normal, thick) hairs have been lost. Their presence can represent the early stages of hair regrowth after conditions such as alopecia areata or telogen effluvium, but it may also indicate ongoing follicular miniaturization—a process where healthy hairs become progressively thinner and less pigmented.
According to the American Academy of Dermatology, the regrowth of vellus hairs is often observed before normal hair color and thickness return. This can be a positive sign, suggesting that follicles remain viable and may eventually produce healthy terminal hairs again. However, in chronic or untreated cases of alopecia, the persistence of vellus hairs without further thickening may indicate continued follicular distress or incomplete recovery.
Monitoring the transition of vellus hairs to thicker, pigmented terminal hairs can help track progress. If only fine, white downy hairs persist for several months, consult a dermatologist about additional treatment options or further evaluation. More details can be found at DermNet NZ: Alopecia Areata.
38. Asymmetrical Hair Loss Patterns
Asymmetrical hair loss patterns refer to uneven thinning or baldness that occurs more on one side of the scalp or body than the other. Unlike the symmetrical and predictable patterns seen in androgenetic alopecia or telogen effluvium, asymmetrical hair loss can be a warning sign that points to localized scalp disorders, physical trauma, or underlying medical issues. For example, conditions such as alopecia areata or scarring alopecias may produce patchy loss that is more pronounced on one side, while fungal infections and certain autoimmune diseases can also create irregular, asymmetrical patterns.
Clinically, asymmetrical loss may also result from repeated pressure or friction on one area of the scalp, such as sleeping on the same side or wearing headgear unevenly. According to the American Academy of Dermatology, this type of pattern warrants prompt evaluation, as it can sometimes signal conditions that require targeted treatment or further diagnostic testing.
If you notice that your hair loss is more severe or rapid on one side, or that the pattern is irregular and not following typical lines of recession, seek assessment from a dermatologist. Early identification of the underlying cause is key to effective management and prevention of permanent loss.
39. Loss of Sideburns or Edge Hair

A subtle but significant sign of certain types of alopecia is the loss of sideburns or edge hair along the hairline, particularly in conditions like frontal fibrosing alopecia (FFA). FFA is a form of scarring alopecia that predominantly affects postmenopausal women but can occur in men and younger women as well. It often begins with a gradual recession of the frontal hairline, accompanied by thinning or complete loss of hair at the temples and sideburns. This edge hair loss can extend to the eyebrows and, in some cases, the nape of the neck.
The changes are often subtle at first, with individuals noticing that their sideburns appear sparser or that the skin in these areas feels smoother than before. According to the American Academy of Dermatology, early symptoms may include redness, slight scaling, or discomfort along the affected edges.
Because edge hair loss can progress gradually, it is important to monitor the shape and density of the hairline and sideburns over time. If you observe persistent thinning or disappearance of hair along the edges, consult a dermatologist promptly for assessment and to discuss early intervention options.
40. Hair Loss in Eyebrow Tails

Loss of hair in the outer (lateral) third of the eyebrows—often called “eyebrow tail loss”—is a subtle but meaningful sign, especially in the context of autoimmune conditions such as alopecia areata or thyroid disease. This pattern of loss, known medically as “Queen Anne’s sign,” may be one of the earliest indicators of underlying systemic issues. In autoimmune conditions, the body’s immune response targets hair follicles, leading to thinning or complete loss of the eyebrow tails while the inner portions remain relatively intact.
According to the American Academy of Dermatology, lateral eyebrow thinning is particularly common in alopecia areata and can also be associated with hypothyroidism and other endocrine disorders. Real-world cases often involve individuals noticing their brows look shorter or that makeup application becomes more difficult at the ends. The change is frequently gradual, making it easy to overlook until there is a noticeable asymmetry or significant thinning.
If you observe consistent thinning or loss of hair at the outer ends of your eyebrows, especially alongside other symptoms such as scalp or eyelash loss, consult a dermatologist or endocrinologist. Early recognition can lead to prompt investigation and targeted treatment for underlying autoimmune or hormonal conditions. For more information, visit DermNet NZ: Eyebrow Loss.
41. Persistent Scalp Tenderness

Persistent scalp tenderness is a frequently overlooked symptom that can act as a warning sign for impending or concurrent hair loss. Chronic tenderness, soreness, or sensitivity of the scalp may be caused by underlying inflammation, increased blood flow, or nerve irritation—all of which are common in inflammatory forms of alopecia such as lichen planopilaris, discoid lupus erythematosus, or central centrifugal cicatricial alopecia. According to the American Academy of Dermatology, such discomfort often precedes visible scalp changes or accompanies early stages of hair thinning and loss.
Patients often describe the sensation as a dull ache, a feeling of pressure, or tenderness that becomes more noticeable when touching, brushing, or styling the hair. The discomfort may be intermittent or constant and can sometimes be accompanied by redness, swelling, or flaking.
To monitor for this symptom, gently press or massage different areas of your scalp and note any persistent tenderness or pain. If chronic sensitivity is present, especially in combination with shedding or visible thinning, consult a dermatologist. Early recognition and treatment of scalp tenderness can help manage inflammation and prevent irreversible hair loss. For more, visit DermNet NZ: Cicatricial Alopecia.
42. Frequent Hat or Headwear Imprints

Frequent and lasting imprints from hats or headwear can be a subtle sign of diminished hair volume and density. With healthy, thick hair, the scalp is cushioned and protected, so headwear tends to leave only faint or temporary marks. However, as hair thins and the scalp becomes less insulated, hats, headbands, and even headphones may leave more pronounced and longer-lasting impressions on the skin. This is because the scalp, now more exposed and less protected, is more susceptible to pressure and indentation.
Individuals may notice that after wearing a hat for only a short time, visible lines or creases persist on their scalp, or there is increased sensitivity in those areas. According to the American Academy of Dermatology, reduced hair density can lead to increased scalp exposure and reactivity to external forces, including pressure from headwear.
If you frequently observe noticeable headwear imprints, it may be an early cue that your hair volume is decreasing. Monitoring this subtle change, especially in conjunction with other signs of thinning, can prompt timely evaluation and intervention. For more on early detection and scalp changes, visit DermNet NZ: Alopecia Areata.
43. Noticeable Change in Hair Styling Hold

A noticeable change in hair styling hold—such as difficulty maintaining volume, shape, or grip in hairstyles—can serve as an early sign of reduced hair density or altered texture. Healthy, dense hair naturally provides structure and resilience for various styles, allowing products like gels, sprays, or mousses to keep hair in place throughout the day. As hair becomes thinner due to conditions like androgenetic alopecia, telogen effluvium, or other causes, it may no longer respond as expected to styling, falling flat or slipping out of clips and bands much more easily.
Individuals might observe that braids feel looser, ponytails require extra wraps with an elastic, or updos that once held firm now collapse quickly. The hair may also appear limp or fail to retain curl and body, despite using the same products and techniques. According to the American Academy of Dermatology, these shifts in manageability often reflect underlying changes in hair shaft diameter and follicle activity.
If you notice persistent changes in how your hair holds a style, consider it a subtle cue of possible thinning or texture alteration and consult a dermatologist. Early attention can help address underlying causes and maintain hair health. For more, see DermNet NZ: Alopecia Areata.
44. Increased Sensitivity to Wind or Touch

Increased sensitivity to wind or touch on the scalp can be a subtle yet telling sign of hair thinning or early alopecia. As the protective layer provided by dense hair diminishes, the scalp becomes more exposed to environmental stimuli. Individuals may notice that even a gentle breeze feels unusually cool or tingly on the scalp, or that light touches—such as running fingers through the hair or brushing—produce heightened sensations of tickling, discomfort, or even mild pain.
Practical cues include feeling drafts on areas of the scalp previously covered by thicker hair, or being more aware of the scalp’s surface during routine grooming. Some people report an increased awareness of temperature changes or even sunburn risk after hair thinning. According to the American Academy of Dermatology, these changes in sensory perception are often among the earliest noticed as the hair’s insulating properties are lost.
If you begin to experience new or increased sensitivity to wind, touch, or temperature on your scalp, especially alongside other silent signs of alopecia, it may be time for a professional evaluation. Early recognition can help address underlying causes and protect scalp health. Learn more at DermNet NZ: Alopecia Areata.
45. Darker Appearance of Scalp Under Lighting

A darker appearance of the scalp under lighting is a subtle indicator that hair density may be decreasing. As hair thins and more scalp becomes exposed, the underlying skin—often slightly darker or with more visible pigmentation—shows through, especially under bright or direct lighting. Common scenarios include noticing the scalp looking more prominent or shadowy in photos, in bathroom mirrors, or beneath harsh fluorescent or overhead lights. This effect can be more pronounced in individuals with darker skin tones or naturally dark hair, where the contrast between scalp and hair accentuates the change.
According to the American Academy of Dermatology, increased scalp show-through is one of the earliest signs of female and male pattern hair loss. People may also observe that the scalp appears shiny or picks up more light reflections, making thinning areas more noticeable.
If you find your scalp appears darker or more visible under certain lighting conditions, consider taking periodic photos in similar settings to monitor changes over time. Early detection of these visual cues can prompt timely investigation and intervention. For more tips on early hair loss detection, visit DermNet NZ: Alopecia Areata.
46. Gradual Shortening of Hair Growth Cycle
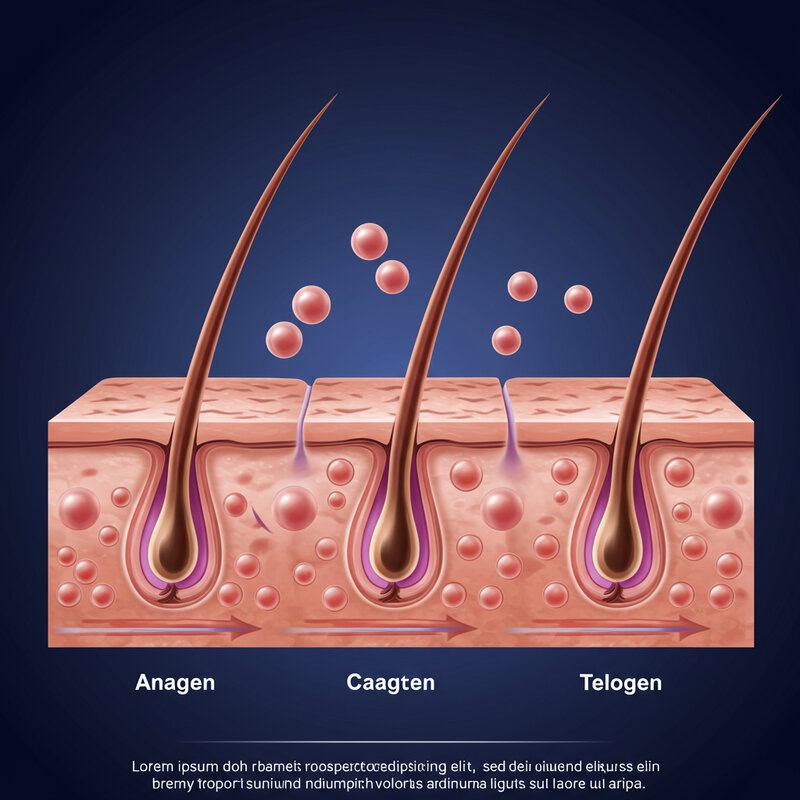
Gradual shortening of the hair growth cycle is a critical but often unnoticed process underlying many types of alopecia, particularly androgenetic alopecia. Normally, each hair follicle undergoes a cycle consisting of a long growth phase (anagen), a brief transitional phase (catagen), and a shedding phase (telogen). In healthy scalps, the anagen phase can last several years, allowing hairs to grow long and thick. However, in alopecia, hormonal changes or inflammation can progressively shorten the anagen phase, causing hairs to grow for much less time before entering the shedding stage.
As a result, new hairs become finer, shorter, and less pigmented with each cycle—a phenomenon known as follicular miniaturization. According to the American Academy of Dermatology, these changes may not be obvious at first but eventually lead to visible thinning and increased scalp show-through. People may notice that their hair never seems to grow past a certain length or becomes increasingly difficult to style.
If you observe that your hair growth has plateaued or your hair is becoming progressively shorter and finer, it may be a sign of an underlying disruption in the hair growth cycle. Early diagnosis can offer more treatment options and better long-term outcomes. For further reading, see DermNet NZ: Androgenetic Alopecia.
47. Painful Hair Pull Test

The hair pull test is a simple clinical tool used by dermatologists to assess active hair shedding and scalp sensitivity. During the test, a small bundle of hair (about 40-60 strands) is gently tugged at the roots. In healthy conditions, only a few hairs (typically fewer than six) will come out, and there should be minimal or no discomfort. However, if the test results in significant pain or an excessive number of hairs are shed, it may indicate an underlying hair disorder such as telogen effluvium, alopecia areata, or inflammatory scalp disease.
Pain during the hair pull test suggests that there may be inflammation or increased sensitivity of the scalp, often associated with conditions like scarring alopecia or active dermatitis. According to the American Academy of Dermatology, the combination of tenderness and excessive shedding warrants prompt evaluation, as ongoing inflammation can lead to permanent follicle damage if not addressed.
If you or your healthcare provider notice pain or significant hair loss during a hair pull test, seek further assessment by a dermatologist. Early diagnosis and intervention can prevent progression and help preserve remaining hair. For more information, visit DermNet NZ: Hair Loss.
48. Loss of Hair Shine or Luster

Dull, lackluster hair is more than just a cosmetic concern—it can be an early indicator of underlying follicle stress or the onset of hair loss. Healthy hair reflects light due to its smooth cuticle layer and natural oils, giving it a shiny, vibrant appearance. When hair follicles are stressed by inflammation, illness, nutritional deficiencies, or hormonal imbalances, they may produce hair that is dry, brittle, and lacking in shine. This loss of luster often precedes visible thinning or shedding, serving as a subtle sign that something is amiss with scalp or follicle health.
Individuals might notice that their hair appears matte, feels rough to the touch, or is difficult to style regardless of conditioner or hair products. According to the American Academy of Dermatology, telogen effluvium and other forms of alopecia often manifest with changes in hair texture and sheen before more obvious symptoms emerge.
If you detect a persistent dullness or loss of shine in your hair, consider reviewing your diet, overall health, and hair care practices. Persistent changes warrant consultation with a dermatologist, as early intervention can address underlying causes and potentially restore hair vitality. For further reading, visit DermNet NZ: Hair Loss.
49. Difficulty Growing Hair Out

Difficulty growing hair out to previous lengths can be a subtle but significant warning sign of underlying hair loss or disruption of the hair growth cycle. In healthy individuals, scalp hair in the anagen (growth) phase can grow several inches per year and maintain length for years before naturally shedding. However, with conditions such as androgenetic alopecia, telogen effluvium, or chronic follicular stress, the growth phase shortens, resulting in hair that falls out or breaks before reaching its former length.
People experiencing this change may notice that their hair “plateaus” at a certain length or becomes increasingly uneven, thin, or prone to breakage at the ends. According to the American Academy of Dermatology, shortened hair growth cycles are common in alopecia and may precede visible thinning or wider parts.
If you observe that your hair is no longer reaching lengths it once easily achieved—despite good hair care and overall health—it may be time to consult a dermatologist. Early recognition of this warning sign can lead to timely intervention and improve the odds of restoring healthier, longer hair. For more details, see DermNet NZ: Hair Loss.
50. Increased Hair Loss During Seasonal Changes

Increased hair loss during seasonal changes is a phenomenon experienced by many people, often most noticeable in the fall and spring. This process, known as “seasonal shedding,” is generally a natural part of the hair growth cycle, with more hairs entering the telogen (resting) phase in response to environmental cues such as changes in daylight or temperature. According to the American Academy of Dermatology, most individuals shed 50-100 hairs daily, but this number can rise temporarily during certain seasons.
However, when seasonal hair shedding becomes excessive—leading to noticeable thinning, patchy loss, or fails to resolve after a few months—it may indicate underlying alopecia rather than a simple seasonal fluctuation. People may observe more hair on their pillow, in the shower, or on clothing, with a slower return to normal density than in previous years.
To differentiate normal seasonal shedding from alopecia, monitor the amount, duration, and pattern of hair loss. If increased shedding is accompanied by other silent signs such as widening parts or visible scalp, consult a dermatologist to rule out underlying hair disorders. For more in-depth guidance, visit DermNet NZ: Telogen Effluvium.
Conclusion

Early detection of alopecia’s silent signs is crucial for preserving hair health and preventing irreversible loss. Subtle changes—such as increased shedding, altered hair texture, or scalp sensitivity—can be easy to overlook but may signal underlying conditions requiring prompt attention. Vigilance in monitoring your hair and scalp, along with proactive self-checks, can make a significant difference in outcomes. If you notice persistent or unusual changes, do not hesitate to seek guidance from a dermatologist. Timely intervention and accurate diagnosis can open the door to effective treatments and improved quality of life. For more information on recognizing and addressing hair loss concerns, visit the American Academy of Dermatology’s hair loss resource.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





