Skin Changes That Point to Cancer
Skin cancer remains the most commonly diagnosed cancer in the United States, with over 5 million cases treated each year according to the Centers for Disease Control and Prevention. As the body’s largest organ, the skin plays a vital protective role, but its vast surface also makes it vulnerable to malignancies. A major challenge in combating skin cancer is late detection, which often results from subtle or overlooked early changes in the skin’s appearance and texture.
1. New or Changing Moles

Moles, also known as nevi, are common skin growths that are usually harmless. However, some moles can evolve into melanoma, the deadliest form of skin cancer. It is important to monitor moles for any changes, as early detection greatly increases the chance of successful treatment. Warning signs include the emergence of a new mole in adulthood, or noticeable changes in an existing mole’s size, shape, or color. The American Cancer Society recommends using the “ABCDE” rule: watch for Asymmetry, irregular Borders, multiple or uneven Colors, a Diameter larger than a pencil eraser, and Evolving characteristics such as bleeding, itching, or rapid growth.
Not all changes mean cancer, but if you notice a mole that stands out from your other moles—sometimes called the “ugly duckling” sign—it’s wise to consult a dermatologist. According to the Skin Cancer Foundation, early evaluation and, if needed, a biopsy are essential. Prompt medical advice is especially important if the mole feels painful, bleeds, or develops a scab without healing. Regular self-exams and professional skin checks are key preventive steps.
2. Asymmetrical Lesions

Asymmetry in skin lesions is a significant warning sign for malignancy, particularly melanoma. A lesion is considered asymmetrical when one half does not match the other in shape, color, or texture. Healthy moles are usually symmetrical—if you drew a line through the middle, both sides would look similar. In contrast, cancerous lesions often develop irregular outlines or uneven distribution of color and structure. The American Cancer Society notes that asymmetry is a key component of the ABCDE rule for skin cancer detection.
During self-exams, pay close attention to any spot or mole that appears lopsided or different on one side. Use a mirror or ask someone for help to examine hard-to-see areas such as your back or scalp. Take note of lesions that change in symmetry over time, as this could suggest abnormal cell growth. According to the American Academy of Dermatology, regular monthly skin checks can help catch these changes early. If you notice a lesion that is not symmetrical, schedule an appointment with a dermatologist for further evaluation and possible biopsy.
3. Irregular Borders

The border or edge of a skin spot offers important clues about its nature. Non-cancerous moles typically have smooth, clearly defined borders, while cancerous lesions, especially melanomas, often exhibit irregular, jagged, or blurred edges. These uneven borders can make the spot appear notched or scalloped, setting them apart from benign growths. According to the American Cancer Society, irregular borders are a hallmark warning sign and form the “B” in the ABCDE detection rule for skin cancer.
The presence of indistinct or poorly defined borders may indicate that the abnormal cells are spreading into surrounding skin tissue, increasing the risk of malignancy. During self-examinations, closely inspect the edges of every mole or spot. Use good lighting and, if needed, a magnifying mirror to detect subtle border changes. The Skin Cancer Foundation emphasizes that jagged or fuzzy borders should never be ignored, as they often signal early melanoma or other serious skin cancers. If you notice a spot with an irregular outline, seek a dermatologist’s advice promptly for a professional assessment and possible biopsy.
4. Varied Colors

The appearance of multiple colors within a single mole or lesion is a significant warning sign for skin cancer, especially melanoma. Healthy moles tend to be uniformly tan, brown, or black. By contrast, cancerous lesions may display a mixture of hues, including different shades of brown, black, red, white, blue, or even pink. This uneven coloration occurs as cancer cells grow irregularly, leading to an unpredictable distribution of melanin and other pigments within the lesion.
The American Cancer Society highlights the presence of varied colors as the “C” in their ABCDE rule for evaluating suspicious moles. When performing self-checks, carefully observe each mole for any new colors or unusual combinations. Some melanomas may also develop lighter or darker patches over time, which should be closely monitored. The Skin Cancer Foundation recommends that people seek medical evaluation if they notice a lesion with multiple colors or areas of discoloration, as these can be early indicators of malignancy. Early intervention is critical, as color changes often precede other visible abnormalities.
5. Large Diameter
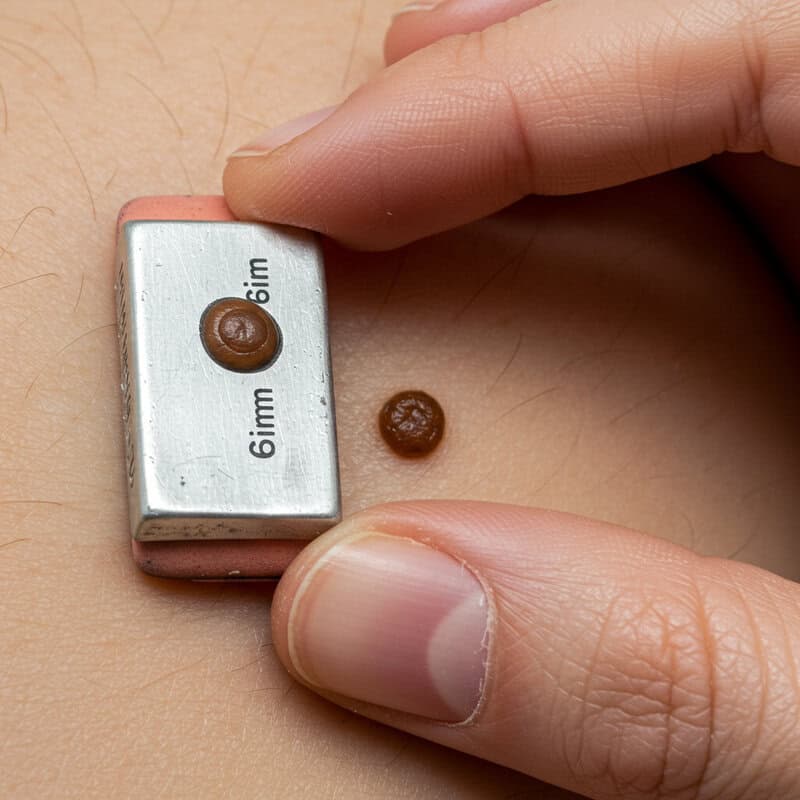
Moles that measure more than 6 millimeters (about the size of a pencil eraser) in diameter are generally considered higher risk for malignancy, particularly melanoma. While not all large moles are cancerous, studies show that size is an important factor in identifying potentially problematic lesions. The American Cancer Society includes “Diameter” as the “D” in the ABCDE rule for skin cancer detection, emphasizing that most melanomas are larger than 6mm when diagnosed, although they may be smaller in their early stages.
A larger diameter may indicate that the mole is growing due to abnormal cell proliferation, which is a key characteristic of cancerous change. During self-examinations, it is useful to compare the size of moles to a pencil eraser or use a ruler for accuracy. Be particularly cautious if a mole continues to enlarge over time or stands out as significantly larger than others. According to the American Academy of Dermatology, any mole exceeding 6mm should be evaluated by a dermatologist, especially if it also displays other warning signs such as asymmetry, irregular borders, or multiple colors.
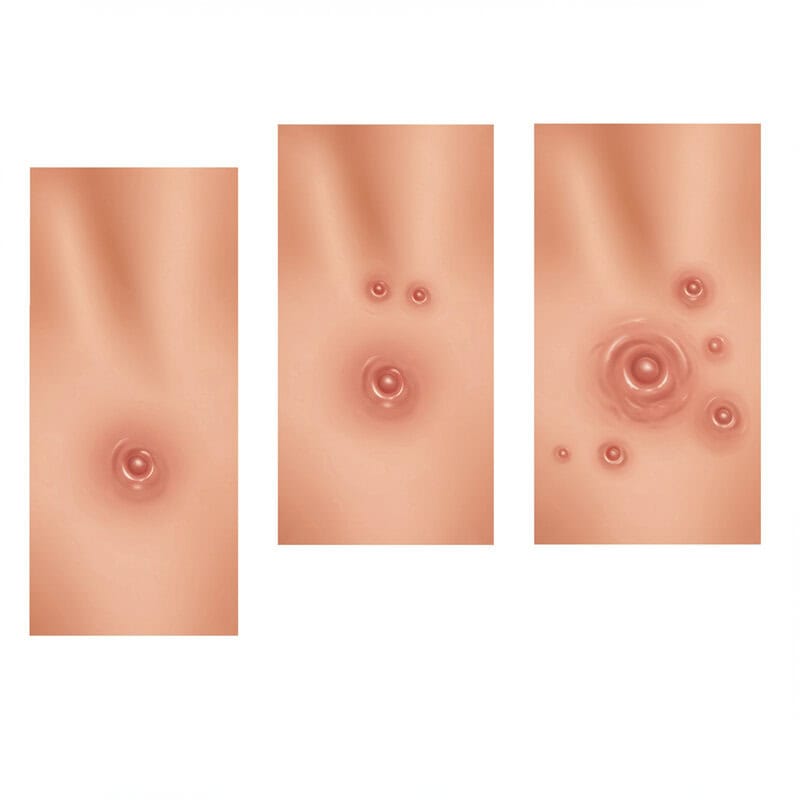
6. Evolving Appearance

One of the most critical factors in identifying potentially cancerous skin lesions is their evolving appearance. This refers to any noticeable changes in a mole or spot’s size, shape, color, elevation, or overall look over time. Skin cancers, particularly melanoma, often undergo rapid and unpredictable transformations as malignant cells multiply. Tracking these changes is essential, as early detection of evolving lesions can significantly improve the prognosis and effectiveness of treatment.
The American Cancer Society highlights “Evolving” as the “E” in the ABCDE rule, underscoring its importance in skin self-exams. Individuals should regularly monitor their skin and document any changes, even subtle ones, to share with their healthcare provider. The American Academy of Dermatology recommends taking periodic photos of moles or lesions for comparison over time, which can help detect concerning shifts that might otherwise be overlooked. Any mole or spot that looks different from the rest, or has begun to itch, bleed, crust, or grow, warrants prompt medical evaluation. Awareness and vigilance are key to catching skin cancer in its earliest, most treatable stages.
7. Persistent Itching

Chronic itchiness confined to a specific area of the skin can sometimes be a warning sign of skin cancer, particularly when it occurs in a mole or new lesion. Unlike common rashes, which usually affect larger areas and are often associated with irritation, allergies, or dryness, cancer-related itching tends to be persistent and localized. This type of itch may not respond to typical over-the-counter creams or home remedies and can even worsen over time. According to the American Cancer Society, persistent itching, especially when paired with changes in the appearance of a mole or spot, should not be ignored.
Itching caused by skin cancer is believed to result from the abnormal growth of cancer cells that irritate surrounding nerve endings or from the body’s immune response to these cells. The Skin Cancer Foundation notes that although not every itchy spot is cancerous, itching that is persistent, unexplained, or associated with other signs such as bleeding or crusting warrants prompt medical attention. Identifying the difference between a fleeting itch and ongoing irritation is crucial for early detection, as lingering itchiness could signal an underlying malignancy needing professional evaluation.
8. Bleeding or Oozing Spots

Unexplained bleeding or oozing from a mole or skin spot is a potentially serious symptom that should never be overlooked. While minor injuries or irritation can occasionally cause skin lesions to bleed, spots that bleed, ooze, or form a crust without any obvious cause may indicate the presence of skin cancer. According to the American Cancer Society, both basal cell carcinoma and melanoma can present as lesions that bleed or discharge fluid, especially as the cancer advances and disrupts normal skin tissue.
Spontaneous bleeding is a result of abnormal blood vessel formation or ulceration within the cancerous lesion. The Skin Cancer Foundation advises that any spot that repeatedly bleeds, oozes, or does not heal after several weeks should be evaluated by a dermatologist. Unlike simple cuts or scrapes, cancerous lesions often fail to heal properly and may become progressively more irritated or tender. Prompt medical consultation is crucial, as persistent or recurrent bleeding could signify an underlying malignancy that requires diagnosis and timely intervention for the best possible outcome.
9. Non-Healing Sores

Sores or ulcers that fail to heal within a few weeks—especially those located on sun-exposed areas such as the face, ears, neck, hands, or arms—may be an early warning sign of skin cancer. While minor cuts and abrasions generally close up quickly, a persistent sore can indicate abnormal cell growth disrupting the skin’s natural healing process. According to the American Cancer Society, non-healing sores are most often linked to basal cell carcinoma and squamous cell carcinoma, the two most common forms of skin cancer.
Chronic sores may appear as small, open wounds that bleed, ooze, crust, or become tender, and are frequently mistaken for infections or harmless irritations. The Skin Cancer Foundation stresses that if a sore does not heal within four weeks, or repeatedly heals and then reopens, it should be evaluated by a dermatologist. Early identification is crucial—cancers detected in their initial stages are more easily treated, and outcomes are significantly improved. Regularly checking sun-exposed skin for non-healing sores can play a vital role in early detection and prevention of advanced skin cancer.
10. Scaly or Rough Patches

Rough, scaly patches on the skin, often referred to as actinic keratosis (AK), can signal an early, pre-cancerous change. These patches typically develop on sun-exposed areas such as the face, ears, scalp, hands, and forearms. Actinic keratoses are usually red, pink, or flesh-colored and may feel dry, sandpapery, or tender to the touch. While many AKs remain benign, a small percentage can progress to squamous cell carcinoma if left untreated. According to the American Cancer Society, recognizing and treating these lesions early can prevent the development of invasive skin cancers.
The Skin Cancer Foundation emphasizes that actinic keratosis is a warning sign of extensive sun damage and serves as a marker for increased skin cancer risk. People with multiple or recurring rough patches should have their skin evaluated by a dermatologist, as these lesions can be easily treated when caught early. Monitoring for new or changing scaly areas, especially in sun-exposed regions, is essential for proactive skin health and reducing the risk of progression to squamous cell carcinoma.
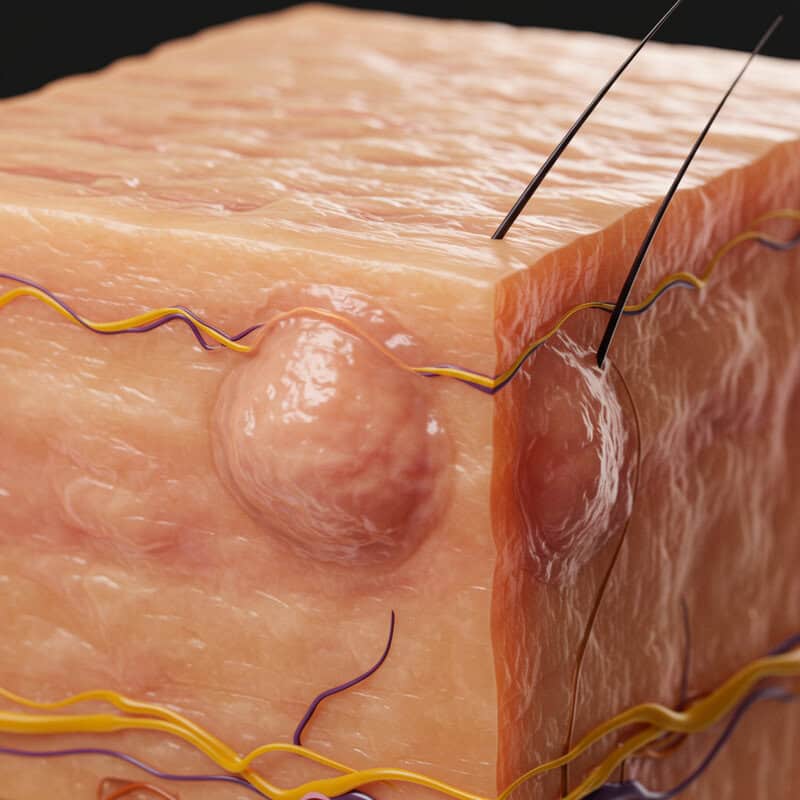
11. Pearly or Waxy Bumps

Shiny, translucent bumps that appear pearly or waxy are characteristic warning signs of basal cell carcinoma (BCC), the most common type of skin cancer. These nodules often develop on sun-exposed areas such as the face, ears, neck, and scalp. Basal cell carcinomas typically present as flesh-colored, white, or pink bumps with a smooth, glossy surface. Over time, these lesions may develop tiny blood vessels (telangiectasia) or a central indentation, and they can bleed or form a crust if irritated.
According to the American Cancer Society, BCCs rarely spread to distant organs but can cause significant local damage if not treated promptly. The Skin Cancer Foundation advises that any persistent, pearly, or waxy bump that does not heal should be professionally evaluated. Early diagnosis and treatment are crucial to prevent further tissue destruction and minimize scarring. Because basal cell carcinomas often go unnoticed due to their subtle appearance and slow growth, regular skin checks and attention to new or unusual bumps are vital for early detection and effective management.
12. Reddish Patches or Irritated Areas

Persistent reddish patches or areas of irritated skin that do not resolve can sometimes be a sign of skin cancer, particularly basal cell carcinoma (BCC) or squamous cell carcinoma (SCC). These patches often appear on sun-exposed regions such as the face, chest, shoulders, arms, or legs. While they may resemble eczema, psoriasis, or dermatitis, cancer-related patches typically persist despite the use of moisturizers or topical steroid creams. According to the American Cancer Society, such patches might feel rough, crusty, or tender and can occasionally bleed or develop a scaly surface.
The Skin Cancer Foundation warns that reddish or inflamed areas are sometimes overlooked, especially if they do not cause pain or significant discomfort. It is important to monitor any patch that persists for several weeks or changes in size, color, or texture. If a red or irritated area fails to improve with typical skin care or becomes more pronounced, it should be checked by a dermatologist. Early intervention is key, as prompt diagnosis and treatment of skin cancers greatly improve outcomes and reduce the risk of complications.
13. Open Sores that Return
Sores that seem to heal but then reappear in the same spot are a cause for concern and may signal an underlying skin cancer. Unlike typical wounds that close and remain healed, cancerous lesions—especially basal cell carcinoma and squamous cell carcinoma—can cycle through periods of apparent healing followed by recurrence. This pattern occurs because the abnormal cells persist beneath the skin surface, enabling the sore to reopen repeatedly. According to the American Cancer Society, this is a classic warning sign that should not be ignored.
Recurrent open sores often occur in sun-exposed areas such as the face, scalp, hands, or arms, and may bleed, ooze, or become crusty. The Skin Cancer Foundation emphasizes that if a sore reopens more than once in the same location or never fully heals, it should be evaluated by a dermatologist. Such lesions may look harmless or be mistaken for minor irritations, but persistent recurrence is a hallmark of skin cancer. Early diagnosis is critical, as ongoing tissue breakdown can lead to deeper damage if left untreated.
14. Dark Streaks Under Nails

Melanoma, one of the most aggressive forms of skin cancer, can sometimes manifest as dark streaks or lines beneath the fingernails or toenails—a condition known as subungual melanoma. These streaks typically appear as brown, black, or even bluish lines running the length of the nail, and they may gradually widen or darken over time. Unlike bruises or injuries, which usually fade as the nail grows out, melanoma-related streaks persist and may be accompanied by changes in the nail’s appearance, such as splitting, lifting, or distortion.
The American Cancer Society notes that while dark streaks can sometimes result from harmless causes like trauma or certain medications, persistent or expanding lines should be promptly evaluated—especially in individuals with no history of nail injury. According to the Skin Cancer Foundation, subungual melanoma is more common in people with darker skin, but it can affect anyone. Early detection is crucial, as this type of melanoma can quickly become invasive. Any unexplained dark line under the nail that does not grow out or is associated with nail changes deserves urgent medical attention.
15. Lump or Thickening in the Skin

The presence of an unexplained lump or area of thickened skin can sometimes indicate a malignant process. While many skin lumps are benign, such as cysts or lipomas, skin cancers—including melanoma, squamous cell carcinoma, and rare soft tissue sarcomas—can also present as firm, painless nodules or patches that gradually increase in size. Unlike normal skin, these areas may feel unusually hard, immobile, or be accompanied by other changes such as discoloration, ulceration, or tenderness.
According to the American Cancer Society, new growths or thickened areas that persist for more than a few weeks, especially in sun-exposed regions, should be evaluated by a healthcare professional. The Skin Cancer Foundation notes that squamous cell carcinoma often manifests as a firm, red nodule or a scaly, thickened patch. Any lump that rapidly grows, becomes ulcerated, or is resistant to healing deserves prompt medical assessment. Early intervention can help determine the cause and, if necessary, allow for timely treatment of skin cancer, reducing the risk of spread or complications.
16. New Growths on the Skin

The sudden appearance of new growths on the skin—particularly in adulthood—warrants close attention, as it can be an early warning sign of skin cancer. While many skin growths are harmless, such as seborrheic keratoses or benign moles, new lesions that develop later in life are more likely to be abnormal. According to the American Cancer Society, melanoma and non-melanoma skin cancers often present as new spots or growths that look different from existing moles or marks.
The Skin Cancer Foundation emphasizes that adults should monitor their skin for any new, unexplained lumps, bumps, or patches—especially those that change rapidly, look unusual, or stand out from other marks. Growths that are shiny, pearly, waxy, or have a rough or scaly surface should be professionally evaluated, as these are common features of basal cell carcinoma and squamous cell carcinoma. The appearance of a new growth is particularly concerning if accompanied by symptoms such as itching, bleeding, or failure to heal. Early assessment by a dermatologist is crucial for prompt diagnosis and effective management.
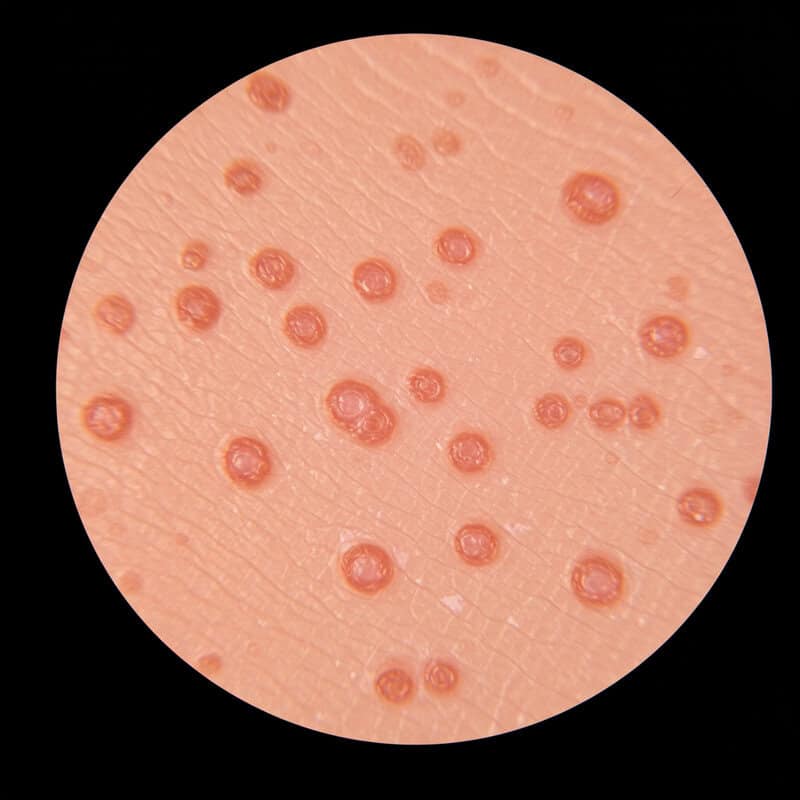
17. Wart-like Lesions

Certain skin cancers, particularly squamous cell carcinoma (SCC), can sometimes resemble common warts. These cancerous lesions often appear as rough, raised, or thickened growths with a surface that may be scaly or crusted. Unlike typical viral warts, which are usually painless and remain stable in size, wart-like cancer lesions may grow rapidly, become tender, bleed, or develop an ulcerated surface. The American Cancer Society notes that SCC can present as a persistent, wart-like sore or nodule, particularly in areas exposed to the sun.
The Skin Cancer Foundation advises that any wart-like lesion that fails to resolve after several weeks, changes in appearance, or develops symptoms such as pain, bleeding, or crusting should be examined by a dermatologist. Unlike benign warts, cancerous lesions do not respond to standard wart treatments and may continue to enlarge or become more irregular. Early evaluation is essential, as distinguishing between common warts and skin cancer often requires a professional assessment and, in some cases, a biopsy to confirm the diagnosis and guide treatment.
18. Painful Lesions

Pain is not a typical feature of most benign skin lesions, so the presence of discomfort, tenderness, or outright pain in a mole or spot may be a red flag for skin cancer. Cancerous lesions, particularly those associated with squamous cell carcinoma or advanced melanoma, can invade deeper layers of the skin, irritate nerve endings, or trigger inflammation, resulting in persistent or worsening pain. According to the American Cancer Society, a skin spot that becomes painful, especially in the absence of trauma or infection, should prompt a medical evaluation.
The Skin Cancer Foundation notes that while benign growths are usually painless, cancerous lesions may be accompanied by other concerning symptoms such as bleeding, non-healing, or rapid changes in appearance. Painful lesions may be mistaken for infected cysts or insect bites, but unlike those conditions, cancer pain often persists or worsens over time and does not respond to typical first-aid measures. If a mole, bump, or patch of skin becomes tender or sore without a clear cause, it is vital to seek a dermatologist’s opinion for a thorough assessment, as early diagnosis can be lifesaving.
19. Ulcerated Areas

Ulcerated areas, which are open sores that fail to heal, are a serious sign that may indicate the presence of aggressive skin cancers such as squamous cell carcinoma or advanced basal cell carcinoma. These ulcers typically develop when the cancerous growth destroys the overlying skin, resulting in a persistent wound with a raw or crater-like appearance. According to the American Cancer Society, ulceration is often associated with more advanced or rapidly growing tumors, and is particularly concerning when found on sun-exposed areas like the face, scalp, and hands.
The Skin Cancer Foundation highlights that ulcerated skin cancers may ooze, bleed, or form a hard crust, and frequently recur even after partial healing. Unlike typical cuts or sores, these lesions do not close up with conventional wound care and may gradually enlarge or deepen. Prompt evaluation by a dermatologist is essential for any non-healing ulcer, as aggressive skin cancers can invade deeper tissues and spread if not treated early. Early diagnosis and intervention significantly improve the chances of successful treatment and recovery.
20. Red, Firm Nodules

Firm, red nodules on the skin can be an indicator of squamous cell carcinoma (SCC) or other types of skin cancer. These nodules typically appear as raised, solid, and often dome-shaped lumps that may be tender or painless. Unlike benign bumps, cancerous nodules tend to persist, gradually increase in size, and may develop a rough or scaly surface. According to the American Cancer Society, SCC commonly manifests as red, firm nodules on sun-exposed areas such as the face, ears, neck, hands, or arms.
The Skin Cancer Foundation notes that these nodules can sometimes ulcerate, bleed, or become crusty if the cancer advances. Unlike common cysts or benign skin growths, cancerous nodules do not resolve on their own and may invade deeper layers of skin or underlying tissues. Early recognition and evaluation by a dermatologist are crucial, as prompt treatment of SCC or other skin cancers greatly reduces the risk of spread and improves long-term outcomes. Any persistent, rapidly growing, or unusual red lump should be examined without delay.
21. Shiny, Translucent Bumps

Shiny, translucent bumps—often pink, pearly, or nearly see-through—are classic signs of basal cell carcinoma (BCC), the most common form of skin cancer. These bumps frequently appear on sun-exposed areas such as the nose, cheeks, forehead, and ears, and may initially be mistaken for harmless pimples or cysts. Over time, the bump’s surface may become more pronounced, develop a rolled edge, or reveal tiny blood vessels (telangiectasia) within the nodule. According to the American Cancer Society, these shiny lesions are a hallmark feature of BCC and should not be ignored.
The Skin Cancer Foundation emphasizes that while BCC rarely spreads to distant organs, it can cause significant local tissue destruction if left untreated. Unlike typical pimples, shiny cancerous bumps do not resolve and may slowly enlarge, sometimes ulcerating or bleeding with minor trauma. If you notice a persistent, shiny, or translucent bump that fails to heal, especially on sun-exposed skin, it is essential to seek a dermatologist’s evaluation. Early detection and intervention prevent further skin damage and reduce the risk of more extensive treatments.
22. Scar-like Areas Without Injury

Patches of skin that resemble scars—appearing as flat, firm, or waxy areas that develop without any history of trauma—can be an early warning sign of skin cancer, particularly a subtype of basal cell carcinoma known as morpheaform or sclerosing BCC. These areas often look pale, white, yellow, or slightly shiny and may feel taut or thickened compared to the surrounding skin. Unlike true scars that follow injury or surgery, these cancer-associated patches emerge spontaneously and tend to expand slowly over time. The American Cancer Society highlights that such scar-like changes, especially on sun-exposed areas, warrant prompt attention.
The Skin Cancer Foundation notes that these lesions are often mistaken for harmless scars or areas of dermatitis, leading to delayed diagnosis. Scar-like basal cell carcinoma can invade deeper skin layers, nerves, and even underlying tissues, making early identification crucial. If you observe a patch of skin that resembles a scar but have no memory of an injury in that area—or if the “scar” seems to be growing or changing—schedule a dermatologist evaluation as soon as possible for accurate diagnosis and care.
23. Pigmented Patches on Palms or Soles

Dark or pigmented patches that appear on the palms of the hands or the soles of the feet can be an indication of acral lentiginous melanoma, a rare but serious form of melanoma. Unlike other types of melanoma that are more linked to sun exposure, acral lentiginous melanoma often develops in areas not typically exposed to the sun. These patches may appear as flat, dark brown, black, or even bluish areas with irregular borders and may gradually enlarge or change in appearance over time. According to the American Cancer Society, this type of melanoma is more common in people with darker skin but can affect anyone.
The Skin Cancer Foundation warns that pigmented patches on the palms or soles are frequently overlooked or mistaken for bruises, warts, or fungal infections. Any new, evolving, or unusual dark spot in these areas should prompt a dermatologist evaluation, especially if the patch expands, changes color, or develops irregular edges. Early detection of acral lentiginous melanoma is critical for successful treatment and improved survival rates.
24. Rapidly Growing Lesions

Spots or bumps on the skin that grow rapidly—sometimes within weeks or a few months—are a serious concern and should be evaluated by a dermatologist without delay. Rapid growth is uncommon for benign skin lesions, which tend to remain stable or change very slowly. When a lesion expands quickly, it may signal an aggressive form of skin cancer such as melanoma, squamous cell carcinoma, or Merkel cell carcinoma. According to the American Cancer Society, the rate of change and growth is a critical warning sign, especially if the lesion also changes color, shape, or texture.
The Skin Cancer Foundation emphasizes that rapidly enlarging skin lesions—whether they are nodules, patches, or moles—require prompt professional assessment to rule out malignancy. Early detection is essential, as aggressive skin cancers can invade surrounding tissues and spread to other parts of the body if not caught in time. If you notice any spot or bump on your skin that appears to be growing quickly or changing dramatically, seek medical attention as soon as possible for an accurate diagnosis and timely treatment.
25. Skin Lesions with Raised Edges

Skin lesions with raised, rolled edges are a distinctive warning sign frequently associated with basal cell carcinoma (BCC). These lesions often present as shiny, pearly, or translucent bumps with a central depression surrounded by a thickened, elevated border. The raised edges may appear waxy or firm, and tiny blood vessels (telangiectasia) can sometimes be seen within the lesion or along its margin. According to the American Cancer Society, this rolled border appearance is typical of BCC and helps distinguish it from benign skin growths.
The Skin Cancer Foundation notes that these lesions may ulcerate or develop a crust in the center, while the edges remain elevated and smooth. This growth pattern results from the cancerous cells spreading outward while the center of the lesion breaks down. If you notice a spot with a raised, rolled edge—especially on sun-exposed areas such as the face, ears, or neck—it is important to have it evaluated by a dermatologist. Early detection and treatment of BCC prevent further local tissue damage and reduce the risk of more invasive procedures.
26. Unusual Texture Changes

Alterations in the texture of your skin—such as areas becoming excessively rough, leathery, or thickened—can be an important clue to underlying skin cancer or precancerous conditions. These changes are often most noticeable in regions that receive frequent sun exposure, including the face, neck, hands, and forearms. Chronic sun damage can lead to actinic keratosis, which may feel like sandpaper or appear as dry, gritty patches. While many texture changes are benign, persistent roughness or a leathery feel that does not improve with moisturizers should not be ignored.
The American Cancer Society points out that actinic keratosis can progress to squamous cell carcinoma if left untreated. The Skin Cancer Foundation also emphasizes that any patch of skin that becomes unusually thick or tough, develops scale or crust, or feels markedly different from surrounding skin should be evaluated by a dermatologist. These texture changes may signal abnormal cell growth, and prompt assessment allows for early intervention. Monitoring your skin for unusual textural changes is a key part of maintaining skin health and catching potential cancers early.
27. Inflamed Hair Follicles That Don’t Heal
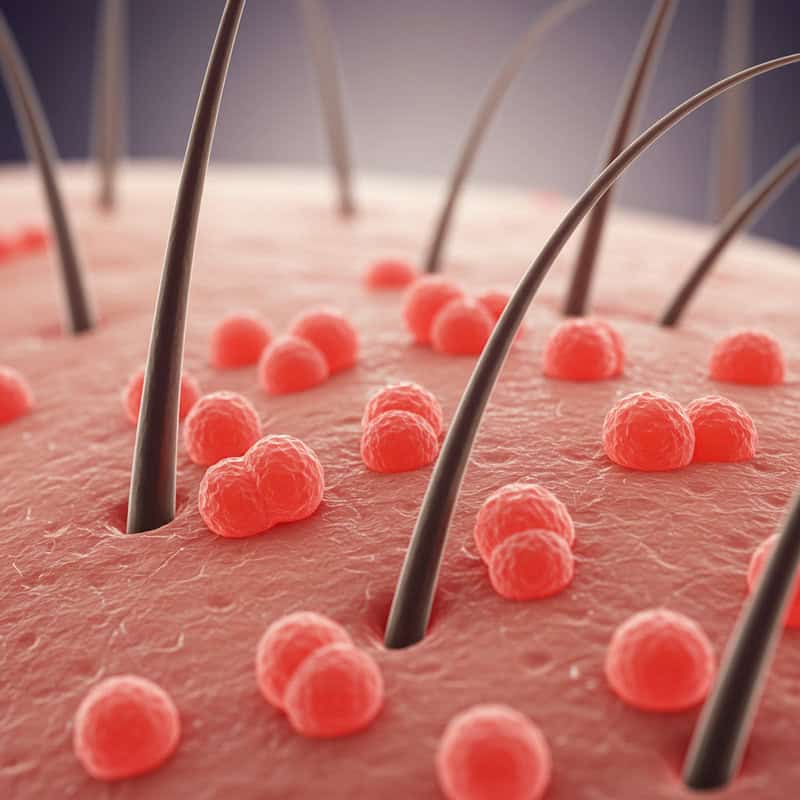
Persistent inflammation or infection around hair follicles—often appearing as red, swollen, or sore bumps that fail to heal—can be a lesser-known sign of skin cancer. While most folliculitis cases are benign and resolve with routine care or antibiotics, chronic or recurring areas of inflammation, particularly on sun-exposed skin, may point to an underlying malignancy such as squamous cell carcinoma or, less commonly, basal cell carcinoma. The American Cancer Society warns that non-healing lesions, especially those that bleed, crust, or increase in size, should always be evaluated by a healthcare provider.
The Skin Cancer Foundation notes that skin cancers can mimic common inflammatory conditions, making diagnosis challenging without professional assessment. If you notice an area that repeatedly becomes inflamed, tender, or develops a persistent sore near a hair follicle—and does not respond to typical treatments—it’s important to seek a dermatologist’s opinion. Early recognition is vital, as skin cancers disguised as chronic folliculitis may progress if left unchecked. Ongoing inflammation despite standard care warrants timely medical attention to rule out malignancy and ensure appropriate treatment.
28. White, Waxy Patches

The appearance of white, waxy patches on the skin—often smooth, firm, and slightly shiny—can be a warning sign of certain skin cancers, particularly basal cell carcinoma (BCC). These lesions may look similar to scars or areas of hypopigmentation but typically develop without any prior injury. According to the American Cancer Society, morpheaform or sclerosing BCC can manifest as flat, white, or yellowish patches that slowly expand over time and may feel tougher than the surrounding skin.
The Skin Cancer Foundation emphasizes that these white, waxy areas are particularly dangerous because they often go unnoticed or are mistaken for benign scars or simple discoloration. Left untreated, these patches can infiltrate deeper layers of the skin and underlying tissue, making treatment more complex. If you observe a white, waxy, or scar-like area that is growing, changing in texture, or appearing without a clear history of trauma, it is crucial to seek evaluation by a dermatologist. Early detection and treatment greatly reduce the risk of extensive tissue damage and improve overall outcomes.
29. Patches That Feel Like Sandpaper

Rough, sandpaper-like spots on the skin—especially in areas with significant sun exposure—are often a sign of actinic keratoses (AKs). These patches are usually small, dry, and may be pink, red, or flesh-colored, often feeling gritty or coarse to the touch. According to the American Cancer Society, actinic keratoses are considered pre-cancerous lesions, caused by long-term ultraviolet (UV) damage, and can progress to squamous cell carcinoma if left untreated.
The Skin Cancer Foundation stresses the importance of recognizing and treating AKs early to prevent malignant transformation. These rough patches most commonly appear on the face, scalp, ears, neck, forearms, and backs of the hands—areas frequently exposed to sunlight. While AKs themselves are not cancer, their presence is a clear indicator of extensive sun damage and increased risk for developing skin cancer. If you notice persistent, rough, sandpaper-like areas that do not improve with moisturizers or over-the-counter remedies, consult a dermatologist for evaluation and possible treatment to protect your long-term skin health.
30. Chronic Soreness or Tenderness

Long-lasting tenderness or soreness in a specific area of the skin can be a subtle but important warning sign of skin cancer. Unlike temporary discomfort caused by minor injuries, insect bites, or irritation, chronic soreness often persists for weeks or months without apparent cause. According to the American Cancer Society, persistent tenderness—especially when associated with a visible lesion, patch, or lump—may indicate an underlying malignancy such as squamous cell carcinoma, basal cell carcinoma, or even melanoma.
The Skin Cancer Foundation notes that cancerous lesions can invade local tissues and irritate nerve endings, resulting in ongoing pain or sensitivity. This symptom is often underestimated, as many benign skin conditions can also cause mild discomfort. However, if you experience localized soreness or tenderness that does not resolve and cannot be explained by injury or infection, it is vital to seek a dermatologist’s evaluation. Early consultation can help distinguish between benign causes and more serious conditions, enabling timely diagnosis and treatment if skin cancer is present.
31. Patches That Bleed Easily

Skin spots or patches that bleed with only minor trauma—such as gentle scratching, washing, or even light contact—may be a sign of underlying skin cancer rather than a simple superficial injury. Cancerous lesions, particularly basal cell carcinoma and squamous cell carcinoma, can cause the skin to become fragile and prone to bleeding because they disrupt the normal structure and integrity of the skin. According to the American Cancer Society, frequent or recurrent bleeding from a skin lesion, especially if persistent or unexplained, should be taken seriously.
The Skin Cancer Foundation emphasizes that patches that bleed easily—even with minimal provocation—often fail to heal properly and may develop crusts or scabs that repeatedly break open. Unlike minor cuts or abrasions, these lesions typically do not resolve with standard wound care and may gradually enlarge or change in appearance. If you notice a spot that bleeds with little or no reason, especially if it recurs in the same area, consult a dermatologist for evaluation. Early assessment can help identify skin cancer at an early, more treatable stage.
32. Blue or Black Nodules
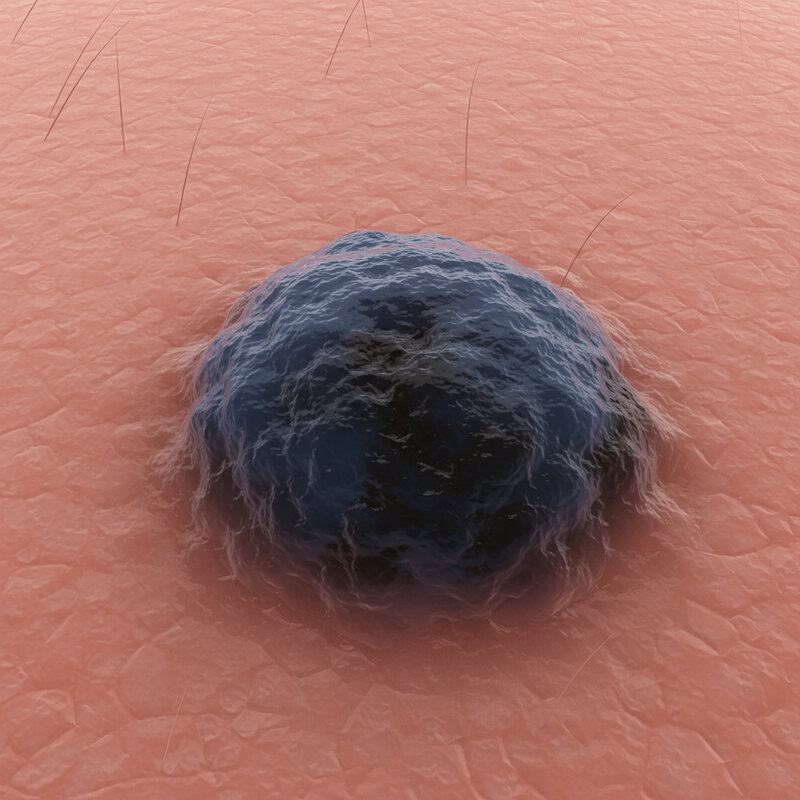
Certain types of skin cancer, most notably melanoma and sometimes basal cell carcinoma, can present as blue or black nodules beneath or on the surface of the skin. These nodules are often firm, dome-shaped, and may appear suddenly or grow rapidly. The pigmentation results from the accumulation of melanin or other pigments produced by cancerous cells, giving the lesion a distinctive dark blue, black, or even bluish-gray color. According to the American Cancer Society, any new or changing blue or black nodule—especially if it is asymmetric, has irregular borders, or is larger than a pencil eraser—should be evaluated as a potential melanoma.
The Skin Cancer Foundation advises that blue or black nodules are often mistaken for bruises or benign moles. However, unlike harmless spots, cancerous nodules persist, may increase in size, and can become ulcerated or bleed over time. Prompt evaluation by a dermatologist is essential, as pigmented nodules can indicate aggressive skin cancers that require early intervention for the best prognosis. Any unexplained, dark lump on your skin should be checked as soon as possible.
33. Skin Discoloration Not Fading

Patches of skin that change color—becoming darker, redder, or otherwise discolored—and do not fade or return to their normal appearance may be cause for concern. While temporary discoloration can result from bruising, rashes, or irritation, persistent changes that last for weeks or months may indicate abnormal cell growth beneath the surface. According to the American Cancer Society, changes in skin color that are not associated with injury or that do not resolve should be evaluated for possible skin cancer, particularly melanoma, which is known for its varied pigmentation.
The Skin Cancer Foundation notes that non-fading discoloration can present as brown, black, reddish, or even bluish patches, and may be flat or slightly raised. Persistent discoloration, especially if it is accompanied by other warning signs like irregular borders, evolving shape, or changes in texture, should prompt a dermatologist’s assessment. Early detection is key, as color changes may be one of the first visible signs of malignancy. Monitoring your skin for patches of discoloration that do not improve is an important part of skin cancer prevention and early intervention.
34. Discoloration Around a Mole

Color changes in the skin surrounding an existing mole are a potentially serious warning sign of malignant transformation. While healthy moles typically maintain a consistent, well-defined color and border, the appearance of redness, darkening, or new pigmentation around the perimeter can indicate the mole is becoming atypical or cancerous. According to the American Cancer Society, spreading color or a “halo” effect around a mole may signify early melanoma, especially if the color is uneven or extends into the adjacent normal skin.
The Skin Cancer Foundation emphasizes that any new discoloration—whether it appears as brown, black, red, or blue—around a mole should be evaluated promptly. Such changes can suggest that cancerous cells are spreading beyond the original borders of the mole, increasing the risk for invasive melanoma. Self-checks should include not only the mole itself but also the skin around it, noting any changes in color, texture, or border clarity. Immediate medical evaluation of these changes is critical for early diagnosis and effective treatment of potential skin cancer.
35. Unusually Swollen Skin
Persistent swelling or puffiness in a particular area of the skin—especially when not linked to an obvious injury, allergic reaction, or infection—can be an atypical but noteworthy indicator of skin cancer. While swelling is more often associated with trauma or inflammation, cancers such as melanoma, squamous cell carcinoma, or rare skin lymphomas can cause localized edema as they invade deeper tissues, disrupt lymphatic drainage, or trigger an inflammatory response. According to the American Cancer Society, swelling around a skin lesion or in the absence of other explanations should not be overlooked.
The Skin Cancer Foundation advises that unusually swollen or puffy skin, particularly if it is persistent, tender, or associated with a visible lump, discoloration, or non-healing sore, should prompt a dermatological evaluation. Swelling that does not improve with standard care or is accompanied by other changes—such as pain, warmth, or altered skin texture—deserves special attention. Early diagnosis and intervention can help identify serious conditions like skin cancer and improve the chances of successful treatment and recovery.
36. Pitted or Dimpled Areas

The development of pitted or dimpled skin—often described as having an orange-peel (peau d’orange) texture—can be a concerning sign, occasionally linked to underlying malignancies such as skin cancer or cutaneous metastases from internal cancers like breast carcinoma. This texture arises when abnormal cell growth or cancerous infiltration causes swelling and fibrosis, pulling on hair follicles and sweat glands to create small indentations or dimples. While peau d’orange is most famously associated with inflammatory breast cancer, it can also appear on other parts of the body as a result of local cancer invasion or lymphatic obstruction.
According to the American Cancer Society, skin dimpling or pitting without a clear cause should always be considered suspicious, especially if it is persistent, spreading, or associated with a mass, discoloration, or tenderness. The Skin Cancer Foundation also recommends that any newly dimpled or pitted skin—particularly if it appears alongside other warning signs of cancer—be evaluated promptly by a healthcare professional for further investigation, as early detection is critical for optimal outcomes.
37. Spreading Redness Beyond a Lesion
Redness that radiates outward from a central skin lesion—sometimes forming a halo or streaks—can be a sign of invasive skin cancer. This spreading erythema may result from the extension of cancerous cells into surrounding tissues, causing local inflammation, increased blood flow, and sometimes lymphatic involvement. While mild redness can occur with benign irritation or infection, persistent or expanding redness that cannot be explained by trauma or dermatitis is more concerning. According to the American Cancer Society, squamous cell carcinoma and aggressive forms of melanoma can both present with redness extending beyond the visible borders of the tumor.
The Skin Cancer Foundation emphasizes that this symptom is particularly worrisome if accompanied by other warning signs such as swelling, pain, non-healing sores, or changes in the lesion’s color or texture. Spreading redness may indicate local invasion or even early metastasis, making prompt evaluation by a dermatologist essential. If you observe a red zone that seems to grow outward from a mole, bump, or patch, seek medical advice immediately to rule out invasive skin cancer and ensure timely treatment.
38. Hard, Immovable Lumps

Lumps beneath the skin that are hard and immovable—meaning they do not shift when pressed—are generally more concerning than soft, mobile lumps. While many benign growths such as cysts or lipomas are soft and can be moved under the skin, hard lumps that are fixed in place may signal that the mass is anchored to deeper tissues, which is characteristic of malignant tumors. According to the American Cancer Society, squamous cell carcinoma and rare soft tissue sarcomas may present as firm, immobile nodules that gradually increase in size and can invade underlying structures.
The Skin Cancer Foundation advises that any persistent, hard lump—especially if it is growing, associated with skin changes, or accompanied by pain or ulceration—should be evaluated by a dermatologist. Immobility suggests possible invasion into surrounding tissue, a hallmark of cancerous growth. Early detection and intervention are crucial, as hard, immovable lumps are more likely to require prompt medical management to prevent further spread or complications. If you encounter such a lump anywhere on your skin, schedule an assessment as soon as possible.
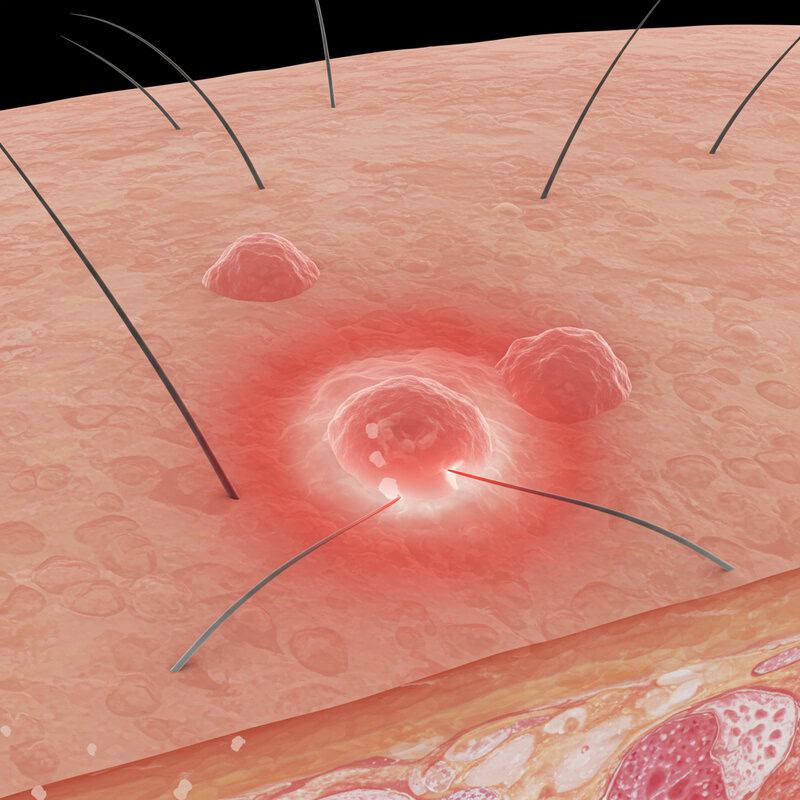
39. Satellite Lesions Near a Primary Spot

The emergence of small new spots, or “satellite lesions,” near an existing or previously diagnosed skin cancer lesion is a significant warning sign of local spread or recurrence. These satellite lesions appear as tiny nodules, bumps, or patches within a few centimeters of the primary tumor and may mimic benign skin changes. According to the American Cancer Society, satellite lesions are most commonly associated with advanced melanoma but can also occur with other invasive skin cancers if malignant cells spread through lymphatic channels or local tissue planes.
The Skin Cancer Foundation warns that the appearance of satellite lesions often indicates a higher risk of metastasis and requires urgent medical evaluation. These spots may be pigmented or flesh-colored and can sometimes ulcerate or bleed, just like the original cancer. If you notice new, unexplained spots developing close to a known or treated skin cancer, it is crucial to notify your dermatologist immediately. Early intervention can prevent further spread, guide effective treatment planning, and significantly improve long-term outcomes for patients with skin cancer.
40. Unexplained Hair Loss in a Patch

Patches of skin where hair falls out and does not regrow—known as localized alopecia—can sometimes be a subtle but important sign of underlying skin cancer. While hair loss is often caused by benign conditions such as alopecia areata, fungal infections, or trauma, persistent bald patches that do not improve may result from cancerous infiltration of hair follicles. According to the American Cancer Society, skin cancers such as basal cell carcinoma, squamous cell carcinoma, and even melanoma can invade the skin’s deeper layers and destroy hair follicles, leading to permanent hair loss in the affected area.
The Skin Cancer Foundation emphasizes that unexplained, persistent patches of hair loss—especially if accompanied by other warning signs like redness, scaling, non-healing sores, or changes in skin color or texture—should be evaluated by a dermatologist. Cancer-related hair loss may also be associated with a firm lump, ulceration, or altered sensation in the patch. Early recognition and assessment are essential to rule out malignancy and initiate timely treatment, improving the chances of a successful outcome.
41. Open Crusty Lesions

Persistent crusting on open skin spots is a significant warning sign of potential skin cancer, particularly basal cell carcinoma and squamous cell carcinoma. These lesions often start as small, red or flesh-colored bumps or patches that break open, ooze, and then form a crust or scab. Unlike minor scrapes or sores, cancerous lesions frequently fail to heal and may repeatedly crust over after minimal trauma or without any injury at all. According to the American Cancer Society, non-healing, crusty sores are a hallmark of both common and more aggressive skin cancers.
The Skin Cancer Foundation notes that open crusty lesions can be mistaken for eczema, psoriasis, or chronic wounds, leading to delays in diagnosis. Key features to watch for include persistent crusting, recurrent bleeding, a sore that enlarges, or a lesion that does not respond to standard treatments. If you notice a skin spot that remains open, forms a crust, and does not heal within several weeks, seek evaluation by a dermatologist. Early intervention is essential to prevent further tissue damage and to improve treatment outcomes for skin cancer.
42. Sudden Appearance of Multiple Lesions
The rapid development of several new skin lesions—especially in a short period—is a red flag that warrants immediate medical attention. While a single new mole or spot may be benign, the sudden appearance of multiple lesions can signal a serious underlying condition, including aggressive forms of skin cancer or metastasis from another cancer site. According to the American Cancer Society, melanoma and other skin cancers can sometimes manifest as multiple new growths, particularly if the disease is advancing or spreading through the lymphatic or vascular system.
The Skin Cancer Foundation highlights that while benign conditions like seborrheic keratoses or viral warts can present with multiple lesions, these usually have a distinctive, non-cancerous appearance and do not emerge rapidly. If you notice several new spots, bumps, or patches developing over days or weeks—especially if they are pigmented, irregular, or symptomatic (such as itching, bleeding, or pain)—contact a dermatologist promptly. Early evaluation is necessary to determine the cause, identify any malignancy, and initiate treatment as soon as possible for the best possible outcome.
43. Flat Brown or Black Patches

Flat brown or black patches on the skin, particularly those with irregular or poorly defined edges, are a classic warning sign of melanoma, the most dangerous form of skin cancer. These patches are often asymmetrical and may display multiple shades of brown, black, or even blue, red, or white within the same lesion. Unlike benign freckles or age spots, melanomas tend to have uneven borders and may gradually expand or change in color and texture over time. According to the American Cancer Society, the presence of a new or changing flat, pigmented patch is a key indicator for early melanoma detection.
The Skin Cancer Foundation recommends paying close attention to the ABCDEs of melanoma: Asymmetry, Border irregularity, Color variation, Diameter greater than 6mm, and Evolution over time. If you notice a flat, dark patch that stands out from other moles or spots—especially if it is growing or changing—consult a dermatologist promptly. Early identification and intervention are essential, as melanoma can quickly become invasive and life-threatening if not treated at an early stage.
44. Painful or Tender Nail Beds

Pain or tenderness in the nail bed is a rare but significant symptom that can indicate subungual melanoma, a dangerous form of skin cancer that develops beneath the fingernails or toenails. Unlike common nail injuries or fungal infections, pain from subungual melanoma is often persistent and may not be linked to any known trauma. This form of melanoma may also present with other warning signs, such as dark streaks under the nail, nail splitting, or changes in nail color and thickness. According to the American Cancer Society, nail bed melanoma can be overlooked, leading to delayed diagnosis and poorer outcomes.
The Skin Cancer Foundation stresses that persistent pain or soreness in the nail bed—especially if associated with discoloration or a noticeable mass—should be promptly evaluated by a dermatologist. Subungual melanoma can occur in any individual but is more common in people with darker skin tones and often affects the thumb or big toe. Early recognition is crucial, as this cancer can quickly become invasive. Any unexplained nail bed tenderness warrants professional assessment to rule out malignancy.
45. Skin That Becomes Fragile or Tears Easily

Skin that suddenly becomes thin, fragile, or prone to tearing and injury may signal an underlying health issue, including the presence of skin cancer. While fragile skin is commonly associated with aging, chronic steroid use, or certain systemic diseases, the sudden onset of these symptoms—especially in a previously healthy area—warrants further investigation. According to the American Cancer Society, squamous cell carcinoma and advanced basal cell carcinoma can disrupt normal skin architecture, making affected areas more susceptible to splitting, tearing, or non-healing wounds.
The Skin Cancer Foundation notes that skin cancers can weaken local tissue integrity, resulting in increased fragility, recurrent minor injuries, and wounds that do not heal as expected. If you notice that a patch of skin suddenly becomes much thinner, tears easily, or develops frequent cuts and abrasions—especially in the absence of trauma or a clear cause—consult a dermatologist promptly. Early recognition and diagnosis are essential for determining the underlying cause and initiating timely treatment, particularly if skin cancer is present.
46. Chronic Inflammation Around Old Scars

Long-term or recurrent inflammation around old scars can be more than a simple nuisance—it may sometimes signal the development of cancerous changes, particularly a type known as Marjolin’s ulcer. Chronic inflammation can disrupt normal tissue repair, leading to abnormal cell growth and increasing the risk for squamous cell carcinoma in scarred or previously injured skin. According to the American Cancer Society, skin cancers arising in old scars, burns, or chronic wounds are often more aggressive and may invade deeper tissues.
The Skin Cancer Foundation notes that persistent redness, swelling, ulceration, or a new lump within or around a scar should not be ignored. These symptoms can sometimes be mistaken for infection or irritation, but if they do not resolve with usual care, prompt evaluation by a dermatologist is essential. Early detection is critical, as cancer arising in scar tissue can spread quickly. Monitoring old scars for new or persistent inflammation, pain, or changes in appearance is a vital part of skin cancer prevention and early intervention.
47. Unusual Skin Tag Growths

Skin tags are generally harmless, benign growths that appear as small, soft, flesh-colored projections on the skin. However, when a skin tag begins to grow rapidly, change color, develop an irregular shape, or becomes painful, it may be more than a simple nuisance. According to the American Cancer Society, rapid changes in skin tags or the sudden appearance of multiple abnormal growths should prompt further evaluation, as these can sometimes mimic or mask skin cancers such as melanoma or squamous cell carcinoma.
The Skin Cancer Foundation emphasizes that skin tags that bleed, ulcerate, develop multiple colors, or grow out of proportion to typical tags are especially concerning. While most skin tags remain stable, unusual changes in their appearance or behavior may indicate the presence of malignant cells or an underlying tumor. If you notice a skin tag that looks or feels different from the rest—particularly if it is growing quickly or changing in color or texture—consult a dermatologist for assessment. Early recognition and biopsy can help rule out or confirm skin cancer, supporting timely treatment if needed.
48. Persistent Burning Sensation

A persistent burning or stinging sensation in a specific area of the skin—especially if it is not linked to an obvious cause like sunburn, insect bites, or irritation—can be a subtle warning sign of skin cancer. Malignant lesions, particularly squamous cell carcinoma and melanoma, can invade nerve endings or trigger inflammatory responses that result in chronic discomfort or a sensation of burning pain. According to the American Cancer Society, unusual or long-lasting sensations in the skin, including burning or tingling, should not be ignored if they persist or are associated with a visible lesion.
The Skin Cancer Foundation notes that while benign skin conditions may occasionally cause burning or stinging, sensations that are localized, ongoing, or linked to a changing patch, sore, or lump are reason for concern. Cancer-related nerve involvement may also be accompanied by changes in color, texture, or the appearance of the affected skin. If you experience a persistent burning feeling in one spot, particularly if the area looks abnormal, seek evaluation by a dermatologist to rule out malignancy and ensure proper management.
49. Non-Sun-Exposed Lesions
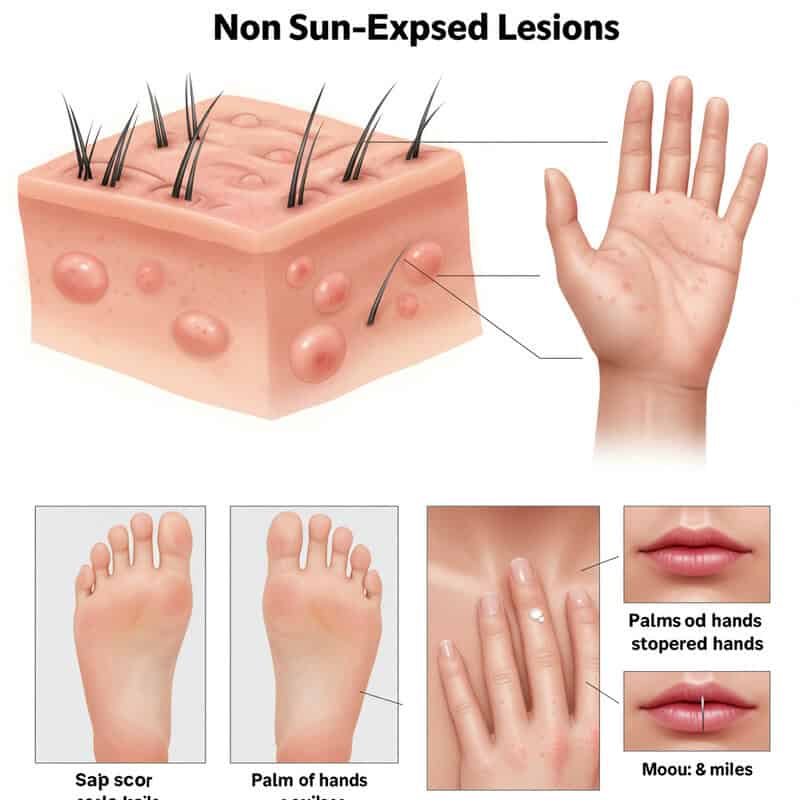
While most skin cancers develop on areas frequently exposed to the sun, such as the face, neck, arms, and legs, it is important to recognize that malignancies can also arise in regions not typically exposed to ultraviolet (UV) light. These include the scalp (beneath hair), the soles of the feet, palms of the hands, under the nails, genitals, and even within the mouth. According to the American Cancer Society, melanoma and rare types of skin cancer, such as mucosal melanoma, can occur anywhere on the body, regardless of sun exposure.
The Skin Cancer Foundation stresses that non-sun-exposed lesions are often overlooked or diagnosed late because people may not regularly check these areas. Warning signs include new or changing spots, persistent sores, dark streaks under nails, or unexplained lumps in these locations. It is essential to perform thorough skin self-exams, including hard-to-see areas, and to consult a dermatologist for any suspicious finding—regardless of its location. Early detection of skin cancer in non-sun-exposed areas is crucial for successful treatment and improved outcomes.
50. Swollen Lymph Nodes Near Skin Lesions

Swelling of lymph nodes near a suspicious skin lesion is a concerning sign that may indicate the spread of skin cancer to the lymphatic system. Lymph nodes, which are small, bean-shaped structures located throughout the body, act as filters for harmful substances and play a critical role in the immune response. According to the American Cancer Society, advanced melanoma and other aggressive skin cancers can metastasize to nearby lymph nodes, leading to noticeable swelling, firmness, or tenderness in these glands.
The Skin Cancer Foundation emphasizes that swollen lymph nodes, especially if they are painless, enlarging, and located near a new or changing skin lesion, should not be ignored. This symptom may signal that cancer cells have migrated from the primary tumor site and are beginning to spread to other parts of the body. Early medical evaluation is crucial for accurate staging, guiding treatment decisions, and improving prognosis. If you notice persistent swelling of lymph nodes—such as in the neck, armpit, or groin—near a skin spot or sore, consult a healthcare professional promptly.
Conclusion

Recognizing and promptly addressing skin changes is crucial for early detection and treatment of skin cancer. Regular self-examinations and awareness of new or evolving lesions can make a life-saving difference. If you notice any suspicious signs or persistent changes, consult a dermatologist for a thorough evaluation. Professional skin checks and, in some cases, formal screenings are highly recommended, especially for those at increased risk. For more guidance on skin cancer prevention and detection, visit the American Cancer Society and the Skin Cancer Foundation. Early intervention maximizes your chances for a healthy outcome.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





